Lymphedema following breast cancer treatment, characterized by limb pain, tightness, heaviness, and possible infections, can occur during or even years following treatments for cancer. Determining which patients are at risk for lymphedema after breast cancer may allow clinicians and researchers to provide appropriate follow-up care and education. In a recent study 190 women who underwent breast cancer treatment including level 3 axillary lymph node dissection (ALND) were followed to determine risk factors for development of lymphedema. Level 3 dissection refers to the surgical classification of the axillary lymph nodes into three compartments, defined in relationship to the pectorals minor muscle. Level 3 describes the nodes above and medial to the pectoralis minor. This page includes more information about breast anatomy and the levels of dissection.
To determine the presence of lymphedema, upper limb circumferential measurements were taken. Lymphedema was found to be present in 41.5% of the women. Of these women, 44 had stage 1, 25 had stage 2, and 10 had stage 3 lymphedema. Stage 1 lymphedema is described as pitting edema that is reversible, stage 2 as non-pitting and irreversible, and stage 3 is considered advanced lymphedema with enlarged limb volume and significant skin changes. The distribution of the lymphedema was measured as 15 cm proximal to the elbow in 94.9% of the patients, and in 73.4% it was located 10 cm distal to the elbow.
In this study, the identified risk factors for developing lymphedema included axillary radiotherapy, chemotherapy, the number of metastatic lymph nodes, age and body mass index (BMI). Because of the known increase in lymphedema prevalence in patients who experience axillary lymph node dissection versus sentinel lymph node dissection, the authors recommend that physicians should play a stronger role in identifying high-risk patients and working towards lymphedema prevention. The medical prevention of lymphedema can include more frequent and thorough follow-up after surgery, and education about modifiable risk factors such as obesity. To learn more about additional lymphedema prevention educational strategies, the Institute offers Rehabilitation for the Breast Cancer Patient with instructor Susannah Haarmann. You still have time to sign up for this course that takes place at the end of the month in the Chicago area!
According to the online resource www.celiac.org celiac disease (also called celiac sprue or gluten sensitive enteropathy) is an autoimmune disorder in which the ingestion of gluten can damage the small intestine. It is further described as an autoimmune disorder affecting 1 in 100 people worldwide and a disorder that can occur among "genetically predisposed people." Common signs and symptoms include abdominal bloating and pain, chronic diarrhea, vomiting, constipation, weight loss, fatigue, irritability and behavioral issues, dental enamel defects, delayed growth, failure to thrive, and ADHD. If not treated, long-term consequences may include developing other disorders such as Type I diabetes, multiple sclerosis, dermatitis herpetiformis (itchy rash), anemia, osteoporosis, infertility, epilepsy, migraines, and intestinal cancers.
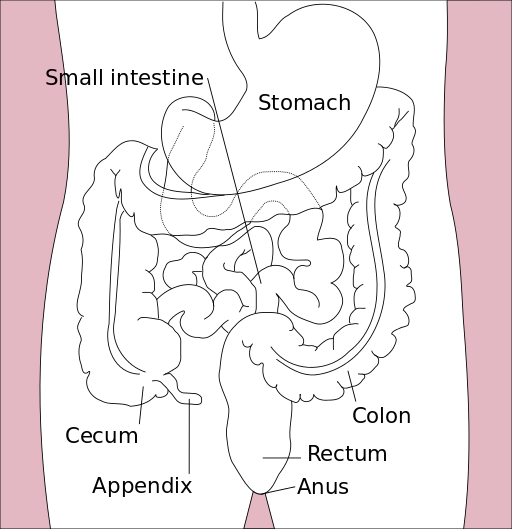
Last year, in the Journal of Family Practice, an article was published describing "Why celiac disease is so easy to miss" the authors point out that less than half of patients present with GI symptoms. An unexplained symptom, iron deficient anemia, may be a clue that a patient needs to be tested for celiac disease. Other conditions, such If a patient has a 1st degree relative with celiac disease, presents with autoimmune thyroid disease, peripheral neuropathy, recurrent migraine, chronic fatigue, osteopenia/osteoporosis, or elevated liver enzymes. (See the linked article for further considerations for testing.) Blood serum tests can help determine the presence of celiac disease, and other tests such as an intestinal biopsy or response to a gluten-free diet can be used to confirm the condition. Adherence to a gluten free diet is critical for a patient with celiac disease, and if you are currently (or have tried) eating a gluten free diet, you know how challenging that may be because gluten is in so many products including sources such as vitamins, medications, and lipsticks! If your patient has been diagnosed recently with celiac disease, referral to a nutritionist may be an excellent part of the patient's plan.
While we might imagine that a patient who has a genetic susceptibility for celiac disease would be diagnosed long before we first see them in the clinic, patients can have a "triggering event" such as a trauma, infection, or severe stress that triggers an onset of the disease. And because of the common gastrointestinal symptoms that are present, a patient with undiagnosed celiac disease may be found in our clinical practice. If you would like to learn more about how celiac disease can affect our patients, those diagnosed or undiagnosed, check out the Institute's new course on Nutrition Perspectives for the Pelvic Rehab Therapist, instructed by Megan Pribyl who earned degrees in both nutrition and exercise science. The course taking place in Seattle this weekend has a few last-minute spots for you to attend, and if you'd like to host this course, contact us at the Institute!