Prolapse and Rehabilitation Part III: Does Pelvic Rehabilitation Help Prolapse?
When considering rehabilitation of prolapse symptoms, therapists often implement an approach that addresses multiple factors related to pelvic health and function. Rehabilitation of prolapse symptoms may include bladder re-training, pelvic muscle strengthening, bowel health management, trunk and pelvic control strategies, avoidance of potential aggravating maneuvers such as bearing down, and education in management tools such as pessaries. As we have established in earlier posts in this 3-part series, each patient must be evaluated and treated with respect to her complaints and clinical findings. This post highlights a few of the many clinical research studies aimed at determining effectiveness of pelvic rehabilitation for prolapse symptoms.
In recent research, Hagen and colleagues completed a multi-center, randomized trial using parallel treatment groups to assess recovery from prolapse. Women with a stage I-III prolapse of any type confirmed by a physician using the POP-Q system and complaints of prolapse symptoms were the primary inclusion criteria. Women who had previously been treated by surgery for prolapse were excluded. The control group (n = 222) were given a prolapse lifestyle advice leaflet and no pelvic floor muscle training. The lifestyle advice included information about weight loss, constipation, avoidance of heavy lifting, coughing, and high-impact exercise. No information about pelvic floor muscle exercise was included.
The physiotherapy treatment group (n = 2250 received up to 5 individualized sessions of pelvic floor muscle training over 16 weeks. The first appointments were scheduled closer together to allow for proper training in muscle education, with the latter appointments being spread further apart. Rehabilitation began with instruction in pelvic muscle anatomy and function. Exercises were instructed based on results of a pelvic muscle assessment, and exercises were progressed with a goal of up to 10, 10-second holds, and up to 50 quick contractions completed three times per day. Women were also instructed in a pre-contraction of the pelvic floor muscles prior to increases in intra-abdominal pressure. (Electromyography, electrical stimulation, or pressure biofeedback were not allowed among the interventions.)
Outcomes tools included the pelvic organ prolapse symptom score (POP-SS) and several other tools to measure quality of life, level of bother from bowel and bladder symptoms, and a general health survey. Women in the physiotherapy treatment group reported more improvements in prolapse symptoms (POPP-SS). While degree of prolapse was also improved in the intervention group, the authors state that the differences were not significant when compared to the control group. Following are highlights from other research completed in prior years.
In this review of 5 randomized, controlled trials, Kari Bo describes the potential benefits demonstrated in the literature including improved pelvic organ prolapse (POP) stage, symptoms, and pelvic floor muscle morphology. The author summarizes that supervised and more intensive training is more effective than unsupervised training.
In this study the authors conducted 14 weeks of treatment with 7 clinic visits that included pelvic muscle awareness and proprioceptive training, education in home exercise program of strengthening.) Positive outcomes included improved anatomic measurements via POP-Q in anterior and posterior vaginal wall, and decreased prolapse symptoms. The intervention group demonstrated improved muscle strength, endurance, and surface EMG parameters. The study concluded that pelvic floor muscle training is effective in treating prolapse.
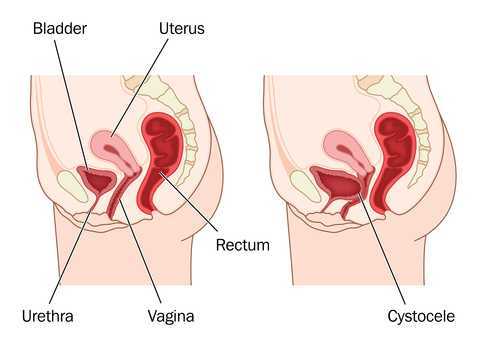
Compared with women in the control group, women in the pelvic floor muscle training group in this study demonstrated increased muscle thickness, decreased hiatal area, shortened muscle length, and elevated position of the bladder and rectum. Subjects also demonstrated decreased muscle length at maximum Valsalva, which the researchers indicated as a sign of increased muscle stiffness.
Following a 16 week physiotherapy program, women with stage I or II prolapse demonstrated significant improvement in stage of prolapse in this research. Women in the treatment group were more likely to report subjective improvement when compared to the control group.
The research indicates, although not consistently, that pelvic floor muscle training can improve the level of prolapse or descent in women with various types of prolapse. Many of the studies include not only pelvic muscle strengthening, but pelvic muscle awareness, protection, and training in functional activation to reduce the impact of straining when it does occur. Regardless of improvement in structural measures, women participating in pelvic muscle training consistently report decreased symptoms such as sense of heaviness when standing. In rehabilitation we are always concerned about function, level of bother, and quality of life of our patients. The bottom line appears to be that symptoms rule the day. We can tap into this fact by taking careful histories, by using outcomes tools, and by teaching our patients that over time they may benefit from continued rehabilitation efforts based on their home program. As with any home program, patients may benefit from a reevaluation and modification of a home program.
Although the research addressing perioperative pelvic rehabilitation is emerging, therapy in combination with surgical approaches may also help prepare women for successful management of prolapse symptoms. Evaluation and treatment of prolapse is instructed in the Institute's pelvic floor series, both in the Level 1 and in the Level 2B course. If you are interested in any series courses, please remember to plan ahead, as these courses fill up several months ahead of time! You can find all of our continuing education courses on the website by clicking here.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./








































