"We Are Desperate"
Male Pelvic Pain: What Therapists Can Do to Help End the Desperation
Recently, a note was left at my doorstep by the wife of an older gentleman who had chronic male pelvic pain. His pain was so severe, he could not sit, and he lay in the back seat of their idling car as his wife, having exhausted all other medical channels available to her, walked this note up to the home of a rumored pelvic floor physical therapist who also treated men. The note opened with how she had heard of me. She then asked me to contact her about her husband’s medical problem. It ended with three words that have vexed me ever since…we are desperate.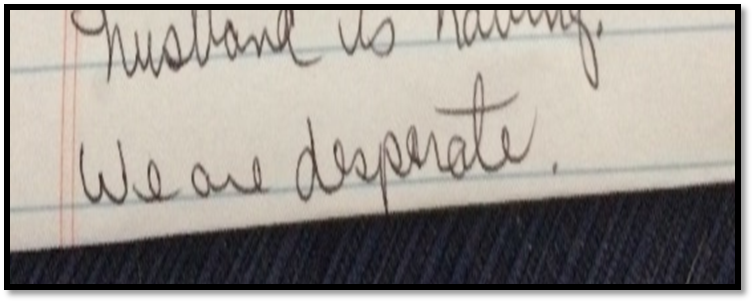
Unlike so many men with chronic pelvic pain, he had at least been given a diagnostic cause of his pain, pelvic floor muscle dysfunction, rather than vaguely being told it was just a prostate issue. However, the therapists that had been recommended by his doctor only treated female pelvic dysfunction.
“We are desperate”: A Call to Action for All Therapists to become Pelvic Floor Inclusive
My first thought after reading the note was, “I bet shoulder or knee therapists don’t get notes like this on their doorstep.” My next thought, complete with facepalm, “THIS HAS TO STOP! Pelvic floor rehab has got to become more accessible”.
Pelvic floor therapists see men and women and even transgenders. They treat in the pediatric, adult, and geriatric population. They treat pelvic floor disorders in the outpatient, home health and SNF settings. They treat elite athletes and those with multiple co-morbidities using walkers. They can develop preventative pelvic wellness programs and teach caregivers how to better manage their loved one’s incontinence. This is due to one simple fact: No matter the age, gender, level of health or practice setting, every patient has a pelvic floor.
The pelvic floor should not be regarded as some rare zebra in clinical practice when it is the workhorse upon which so many health conditions ride. It interacts with the spine, the hip, the diaphragm, and vital organs. It is composed of skin, nerves, muscles, tendons, bones, ligaments, lymph glands, and vessels. It is as complex and as vital to function and health as the shoulder or knee is, and yet students are lucky if they get a “pelvic floor day” in their PT or OT school coursework.
I call for every therapist, specialist, and educator to learn more about the pelvic floor. Here are some steps you can take today toward eliminating the need for such a note to be written.
If you are a pelvic floor therapist who treats men, shout it from the rooftops!
Contact every PT clinic, every SNF, every doctor, every nurse, every chiropractor, every acupuncturist, every massage therapist, every personal trainer, every community group and let them know! If you have already told them, tell them again. Send a one page case study with your business card. Host a free community health lecture at the library or VFW hall. Keep the conversation going. Reach out to your local rehab or nursing school programs and volunteer to speak to the students. Feature pelvic health topics in your clinic’s social media stream. Get on every single therapist locator that you can so people can find you. Click here to go to the Herman and Wallace Find a Practitioner site.
If you only treat pelvic dysfunction in women, please consider expanding your specialty to include men.
The guys really need your help. You literally may be the only practitioner around that has the skills to treat these types of problems. Yes, the concerns you have about privacy and feeling comfortable are valid. But, you are not alone in this. Smart people like Holly Tanner have figured all that stuff out for you and can guide you on how to expertly treat in the men’s health arena. Sign up for Male Pelvic Floor or take an introductory course online at Medbridge. If you have only taken PF1, it’s time to sign up for Pelvic Floor Level 2A: Function, Dysfunction and Treatment: Colorectal and Coccyx Conditions, Male Pelvic Floor, Pudendal Nerve Dysfunction. Reach out to other pelvic floor therapists that treat men and ask for mentorship.
If you are general population therapist, consider taking a pelvic floor course.
Good news! Not every pelvic floor course requires you to glove up and donate your pelvis to science, so to speak. Yes, there are several external only courses you can take that do not have an internal examination lab. Click here and look under “course format” to see a list of external only courses. If you treat in the outpatient, ortho, or sports medicine arena, consider taking Biomechanical Assessment of the Hip & Pelvis: Manual Movement Therapy and the Myofascial Sling System or the Athlete and the Pelvic Floor .
If you treat in the Medicare age population, work in skilled nursing, or home health, join me in New York on May 21-22 for Geriatric Pelvic Floor. It is an external course and we cover documentation and self-care strategies extensively for incontinence and pelvic pain in older adults across multiple settings. Older adults with pelvic pain, like the man in the back seat, are at risk for being diagnostically ignored. We will address biases, such as “prostato-centric” thinking, ageism, and the ever-present “no fracture no problem” prognosis given to seniors who sustain a fall, but are left with disabling soft tissue dysfunction.
If you are a PT or OT school educator, eliminate “Pelvic Floor Day”.
Sorry, but it sounds silly. It’s like saying you offer a “Knee Day” in your program. Replace it by including the pelvic floor into Every. Single. Class…anatomy, ther ex, neuro, peds, geriatrics, and even cardiopulmonary!
As the baby boomer population grows, pelvic floor disorders are expected to rise significantly (download a free white paper on pelvic floor trends here). Are you preparing your doctorate students to be competent screeners of pelvic floor dysfunction? Pelvic floor rehab is becoming the gold standard of first line treatments for pelvic dysfunction. Are you giving your students the skills to be competitive in a job market that recognizes pelvic floor rehabilitation as standard of care? Bias is learned. Excluding the pelvic floor in your student’s coursework or presenting it as a niche specialty subtly reinforces this bias.
Reach out and ask your local pelvic floor therapists to guest lecturer throughout the program. Send your instructors to pelvic floor courses. Encourage your students to take Pelvic Floor Level 1 in their last 6 months of coursework. Offer a clinical rotation in pelvic floor rehabilitation. Include case studies and patient perspectives on pelvic dysfunction, such as A Patient’s Pelvic Rehab Journey.
The Silver Lining
Thanks to the champions of pelvic floor rehab education, we’ve come a long way. The good news in this story is that this man’s doctor recognized early that he had pelvic floor muscle dysfunction and recommended that he see a pelvic floor physical therapist. The bad news-it took 2 years before he could find one. The ball is in our court, therapists. Let’s do better. Until there are no more men in the back seat, we still need to #LearnMoreAboutThePelvicFloor.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./








































