Why you should learn about Pudendal Neuralgia
Herman & Wallace are pleased to announce a new course! Pudendal Neuralgia and Nerve Entrapment will be presented by Michelle Lyons in Freehold, NJ on June 17/18, 2017. We chatted with Michelle about this new course to hear her thoughts and get an overview of the contents
 There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
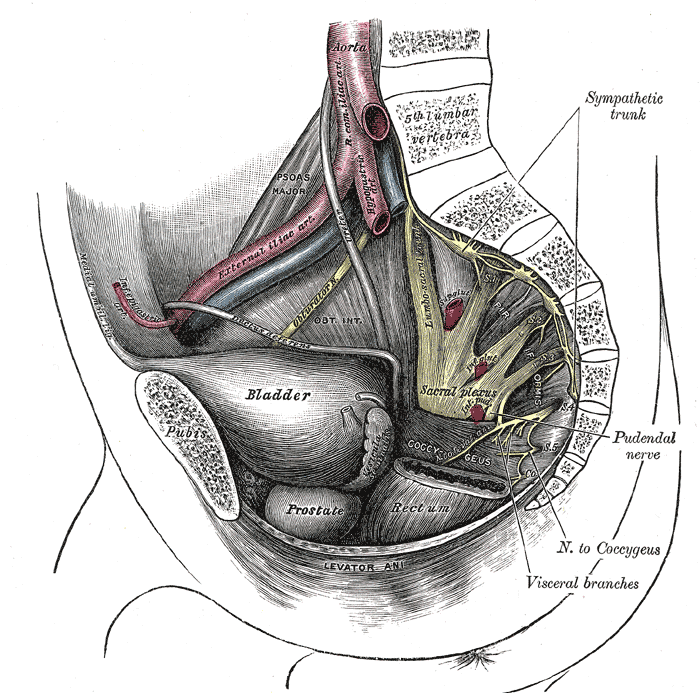
When I was approached about developing this course for the Institute, I jumped at the opportunity. For those who don’t know me, I really like to bring an integrative approach to my work, both clinically and educationally. I have experience and training in nutrition, coaching, yoga, Pilates and mindfulness as a therapeutic intervention and I think these fit really well alongside traditional pelvic rehab approaches. Manual therapy and bespoke exercise prescription will always be the bedrock of my approach, but sometimes our patients, especially those with chronic pain, need some extra support. I’m also a bit of an anatomy nerd, so the chance to delve deep into pelvic neuroanatomy and neurodynamics was too much to resist!
I think this is a Golden Age in pelvic health – there are so many great learning opportunities and resources available to us to help serve our patients better. Another area that I find fascinating to explore is the huge leap we have made in understanding neuroscience and the role of pain education when it comes to chronic pelvic pain. I’m a big fan of the work done by Moseley and Butler in Australia, and I love how authors like Hilton, Vandyken and Louw have transferred that to the world of pelvic pain in their book "Why Pelvic Pain Hurts". The language that we use is very important when discussing how the brain responds to chronic pain and the changes that occur with central sensitization. We never want our patients to feel as if we think their pain is ‘all in their heads’ but at the same time, we need to be able to incorporate strategies such as motor imagery and graded exposure and to demonstrate to our patients that"…it is important to acknowledge that chronic pain need not involve any structural pathology" (Aronoff 2016).
Those are some of the discussions we’ll be having in Freehold, NJ next June – I hope you’ll come and join the conversation!
"What Do We Know About the Pathophysiology of Chronic Pain? Implications for Treatment Considerations" Aronoff, GM Med Clin North Am. 2016 Jan;100(1):31-42
"Why Pelvic Pain Hurts: Neuroscience Education for Patients with Pelvic Pain" Hilton, Vandyken, Louw, International Spine and Pain Institute (May 28, 2014)
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./



































