
One of my favorite things as the instructor of the Menopause Transitions course is when participants ask questions. Whether it is something about their own menopause journey or when a patient is struggling with symptoms, it thrills me to provide resources and clarity to help them make informed decisions.
The following are some of the questions that have come up in class or that have been brought to my attention via email after participants are back in the clinic:
Given the many benefits of hormone therapy, should every patient take it during or after perimenopause for the prevention of chronic disease?
This is an excellent question! Based on recommendations from The Menopause Society, hormone therapy is approved for the treatment of vasomotor symptoms, genitourinary symptoms, and the prevention of osteoporosis.

One of the most bothersome and common symptoms experienced by patients going through the menopausal transition is hot flashes (Freedman 2015). Vasomotor symptoms can vary in intensity from mild to debilitating (Gold et al., 2000), and patients can suffer from a flushed face up to a full sweat with the removal of clothing and a brisk fan required for relief. Hot flashes can affect a patient’s focus, sleep, and activity tolerance. These pesky flashes are also associated with several medical disorders including heart disease, dementia, and osteoporosis (Biglia et al, 2017).
What causes hot flashes isn’t entirely known. A variety of factors can be at play including genetics, personal experience, cultural influences, and medications (Biglia et.al, 2017), however, one of the predominant factors contributing to these flushes is decreasing or fluctuating estrogen levels. Declining estrogen is linked with the KnDy (kisspeptin-neurokinin B-dynorphin neurons) located in the hypothalamus. These neurons project to the thermoneutral zone also located in the hypothalamus. This zone regulates the temperature in the body. As estrogen levels diminish, these neurons hypertrophy. This causes an increase in activity to the thermoneutral zone making the patient more sensitive to temperature changes (Rance et al, 2013). A small shift in temperature causes a greater physiological response triggering the hot flash.
In their 2022 position statement on hormone therapy, the North American Menopause Society recommends estrogen as one of the most effective treatments for this symptom. It is cited as a safe and effective option which many choose for relief. For some patients, this is not an option due to either personal choice or contraindications from their medical history.

According to the International Menopause Society, “The purpose of the day is to raise awareness of menopause and the support options available for improving health and well-being.” While we have come a long way in bringing this issue into the spotlight, I still encounter patients on a daily basis who are unaware of what this transition can mean to their long-term health and quality of life. Some do not discuss their symptoms with their physician, and others, despite sharing their symptoms with their doctor, often leave the visit with “just live with it” as the recommended course of care due to fear of breast cancer (Barber and Charles 2023).
I have been teaching my menopause course, Menopause Transitions and Pelvic Rehab, for almost three years. A common question raised by participants during the course is whether discussing hormonal treatment options is outside the scope of pelvic rehabilitation. While I understand the concern, I do have some thoughts I would like you to consider. To elaborate, let me share a recent clinical experience I had when evaluating a patient for an orthopedic pathology.
This patient was a cis-female patient in her late 40s who presented to the clinic for mid-back pain. She had an extensive medical history of auto-immune conditions and work-related injury. She had been hospitalized due to her diagnosis and had lost a substantial amount of weight. As with any therapy evaluation, I asked how she was sleeping.
Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician who wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process. To learn more join Christine in her upcoming course scheduled for February 10-11, 2024.
Conversations about menopause are becoming more mainstream. What used to be a taboo subject has thundered into the media in triumphant fashion. Drew Barrymore, Oprah Winfrey, and Maria Shriver are just a few of the celebrities spreading the word about this transition that will affect all menstruating people at some point in their lives. Despite the headlines and increased coverage, most women feel uneducated and underprepared for how this transition will manifest itself in their bodies concerning symptoms and long-term health (Tariq et al., 2023). Pelvic health providers are the perfect people to educate their patients on these changes.
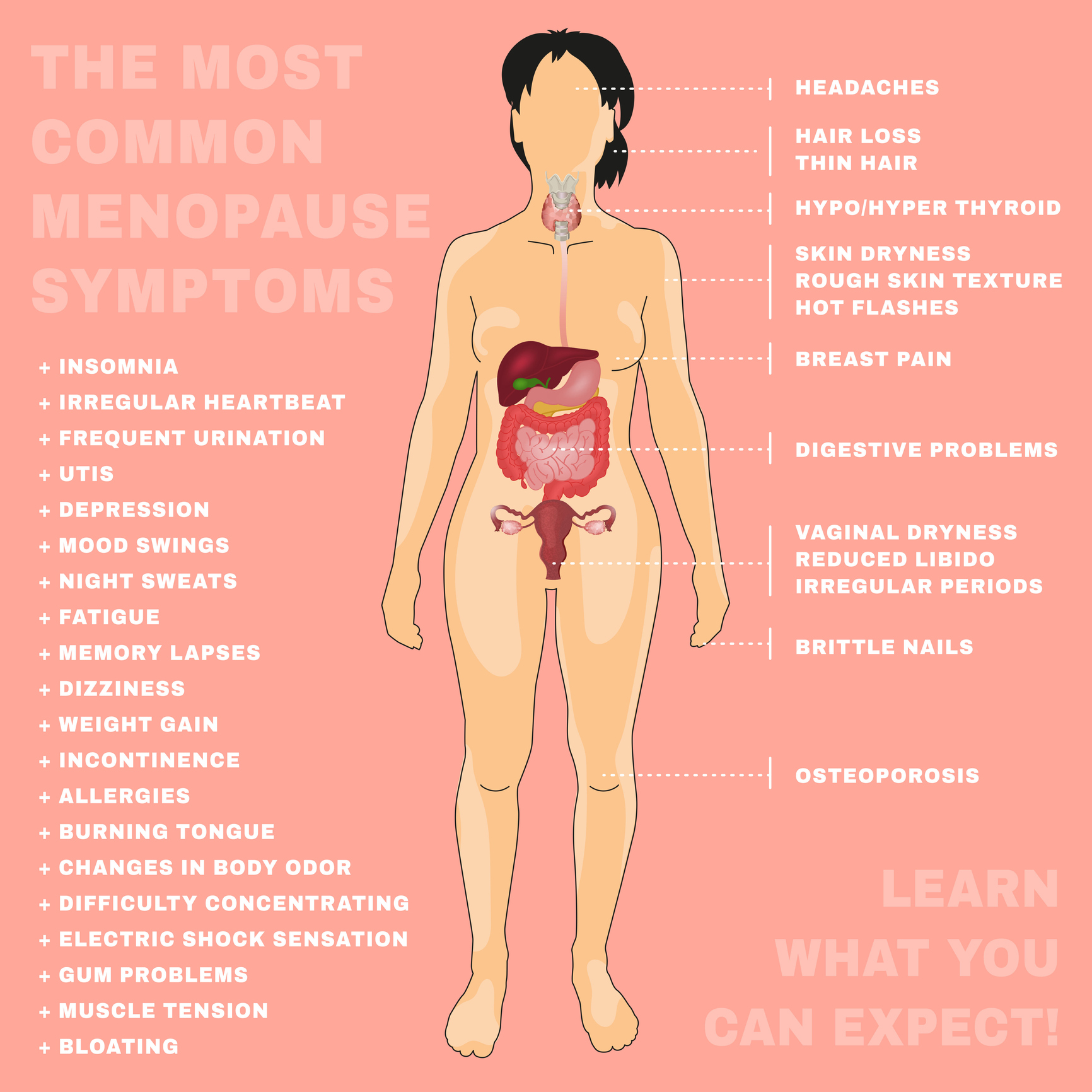
Menopause is defined as twelve months with no menstrual cycle. Once this has occurred, a patient has then entered a post-menopausal state. However, the process of reaching this twelve-month milestone will begin long before menopause is achieved (Lewis 2021). Symptoms are often experienced in the transitional process leading up to menopause, years before it finally occurs. Perimenopause is the precursor to menopause and represents a time when the ovary begins to change. Hormone levels begin to fluctuate which can affect cycle regularity and intensity. Cycles can now occur every three weeks, ovulation can become irregular, and periods can become heavier. When hormones and cycles change, symptoms can begin. Sleeplessness and night sweats before the onset of menstruation can be an early indicator of perimenopause as well as increased anxiety, brain fog, and irritability (Aninye et al., 2021). These changes can begin in patients as early as their late teens but most commonly will occur in the late 30’s and early 40’s. Knowing how to recognize symptoms that can occur during the perimenopause transition can help to educate patients on what is occurring and what they can anticipate as the ovary continues to age.
Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Christine joined Olathe Health in 2010 to further focus on women’s health and obtain her CMPT from the North American Institute of Manual Therapy. She also went through Diane Lee's integrated systems model in 2018. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician that wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process.
Menopause. The M-word, the second puberty, is the final frontier of a hormonal roller coaster when there are twelve consecutive months with no menstruation. A time of celebration, right? No more cramps, hygiene products, menstrual cups, or moodiness – FREEDOM! Not so fast my fellow clinician!
The body goes through some serious, hormonal loop-the-loops leading up to the cessation of ovulation. Perimenopause is the stretch leading up to the final cycle and this stretch can feel like yoga on steroids. It can last TEN years, not including symptoms experienced after the transition takes place. Changes in cycle length, flow, anovulation, and yes, even ovulating twice are all stages of perimenopause. (Hale et al., 2009). These changes translate into symptoms: sleeplessness, brain fog, anxiety, palpitations, fatigue, painful intercourse, and joint stiffness are just a few things that can be experienced during this time (Lewis, 2021).





































