We are pleased to announce the following changes and additions to our core series of courses. These changes are being undertaken by our Curriculum Development Team based on evolving realities of our field and the body of evidence and literature. In keeping with the way the field has evolved, we will be making the following changes to our core coursework.
Two courses will be joining our Pelvic Function Series:
- Pelvic Function Modalities - This brand new course is an in-person two-day continuing education course targeted to pelvic health clinicians covering frequently used modalities in pelvic health, including biofeedback and EStim. Hands-on labs using a variety of equipment necessitate that this course be offered in-person, where participants can practice using the equipment.
- Pelvic Function Level 2C: the Male Pelvic Floor and Men’s Pelvic Health - formerly the stand-alone course, Male Pelvic Floor Function Dysfunction and Treatment, this course is now being adapted and reformatted to be a part of the Pelvic Floor Series, reflecting the inclusive stance of H&W core series instructing in the care of all patients. This course will be offered as satellite, self-hosted, and in-person options in order to provide the most flexible pathway for participants.
In addition to these two new offerings, you will see greater inclusion of all genders throughout the series, starting with PF1. The modified titles and topics will be as follows:
Pelvic Function Level 1: Introduction to Pelvic Health - this course will provide a thorough and comprehensive introduction to anatomy and physiology of the pelvis and surrounding structures in all genders. Includes an introduction to performing intra-vaginal exam. This course will be offered in satellite and in-person formats.
HW is excited to announce the addition of a brand-new course to our Pelvic Function (PF) Series!
Pelvic Function Level 2C (PF2C): the Male Pelvic Floor and Men’s Pelvic Health
Formerly the stand-alone course, Male Pelvic Floor Function Dysfunction and Treatment, this course is now being adapted and reformatted to be a part of the PF Series, reflecting the inclusive stance of H&W core series instructing in the care of all patients. This course is intended for the pelvic health clinician who treats patients with conditions including post-prostatectomy urinary incontinence, erectile dysfunction, and chronic pelvic pain (CPP).


Within the walls of the pelvic rehabilitation clinics, we often hear more intimate details than we ever imagined we would, could, or perhaps should. With increasing patient care experiences, most therapists demonstrate increased knowledge, awareness, and with some practice, increased skill at discussing sensitive issues such as sexuality. Every person and relationship is unique and we are sometimes asked questions by our patients such as "Should I be having more sex?" or "Am I normal?"
I have sometimes been surprised when a patient reports that he or she is "not having sex often enough" and for that patient it means that daily sexual activity is no longer happening. Other patients are quite satisfied with their sexual activity occurring 2-3x/month. We meet patients who have gone for years without engaging in sexual activity, perhaps because of pain, or lack of intimate partnership, or medical issues with a partner. It is very useful to avoid having expectations for what we as therapists think a patient should or should not be doing, whether that pertains to a particular sexual practice or to a level of involvement with a partner.
-Holly Tanner. Sexuality and the Older Patient. Tuesday, 13 September 2011.

The upcoming Modalities and Pelvic Function course is a collaboration of different faculty members working to bring participants the information they have been asking for about modalities, ever since COVID forced a shift in Herman & Wallace's course format. This is a two day, in-person, hands-on course, created to be a very research based and intervention heavy learning experience for participants.
The majority of the in-person learning is interactive or lab based with the lectures being primarily focused on how to apply these modalities to clinical experiences and practice. If you can think of a modality, it is probably mentioned, if not practiced or sampled during this class. You can check out the schedule for an extensive list of all of the modalities included in this class. If there was a modality that could not be experienced as a group, there are interspersed expert interviews reviewing those concepts.
This class is for all types of learners and will definitely meet the needs of people missing in person learning opportunities. Because this class is so lab focused, hands-on and has so much equipment involved, there will only be a few offerings with small in person class sizes.
Breast Cancer Awareness Month
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.

Special thanks to faculty member Mora Pluchino, PT, DPT, PRPC, and Carole High Gross, PT, DPT, PRPC taking time during HWConnect 2023 to sit down and do this interview. Carole earned her Doctorate of Physical Therapy from Arcadia University in 2015, and her Master of Science in Physical Therapy in 1992 from Thomas Jefferson University, and earned her Pelvic Rehabilitation Practitioner Certification and enjoys working as a Pelvic Clinical Rehabilitation Specialist for Lehigh Valley Health Network. She is a Lead Teaching Assistant and instructor with Herman & Wallace. You can meet Carole in her upcoming course Eating Disorders and Pelvic Health Rehabilitation: The Role of a Rehab Professional scheduled for October 28-29, 2023.

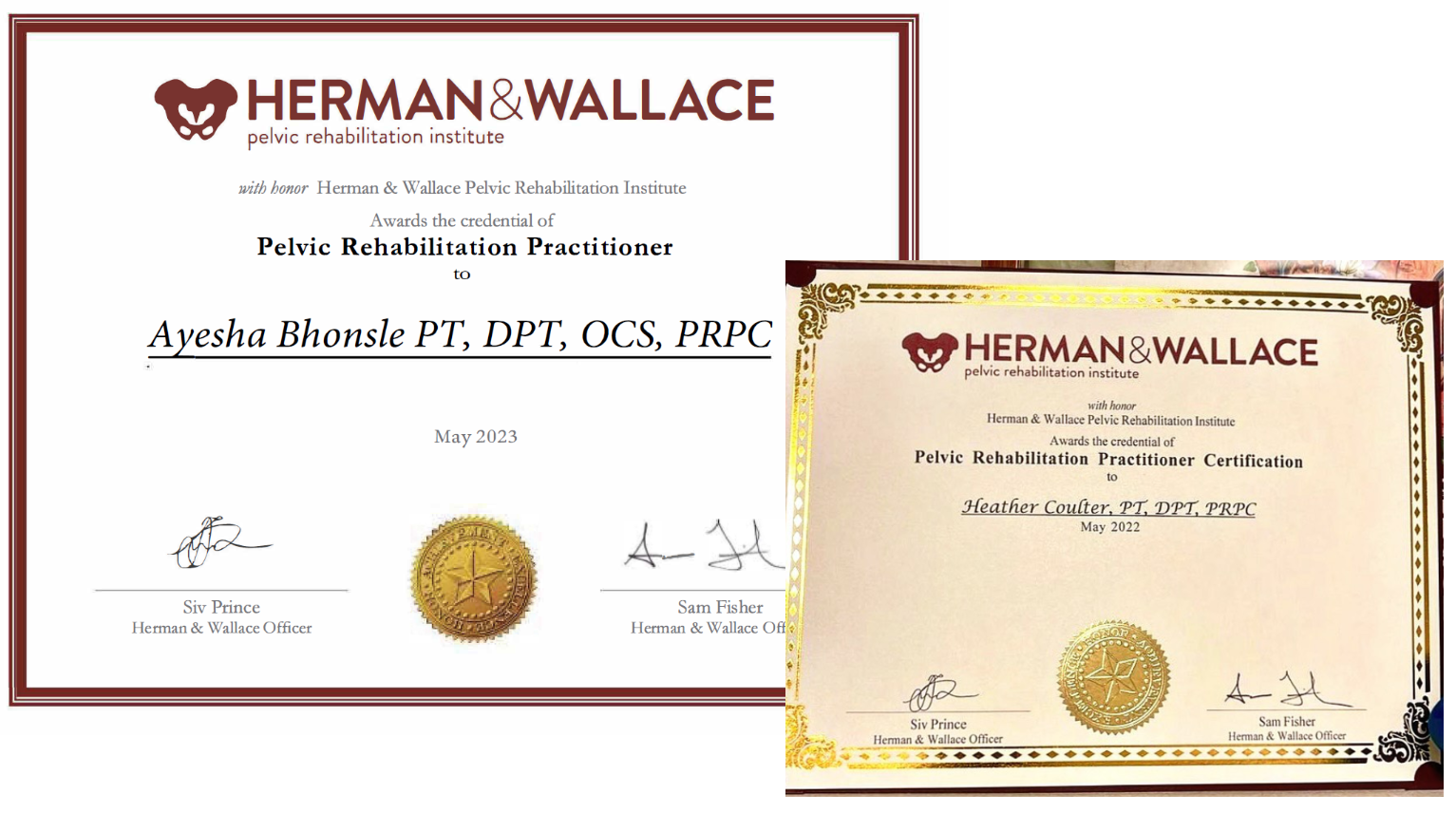
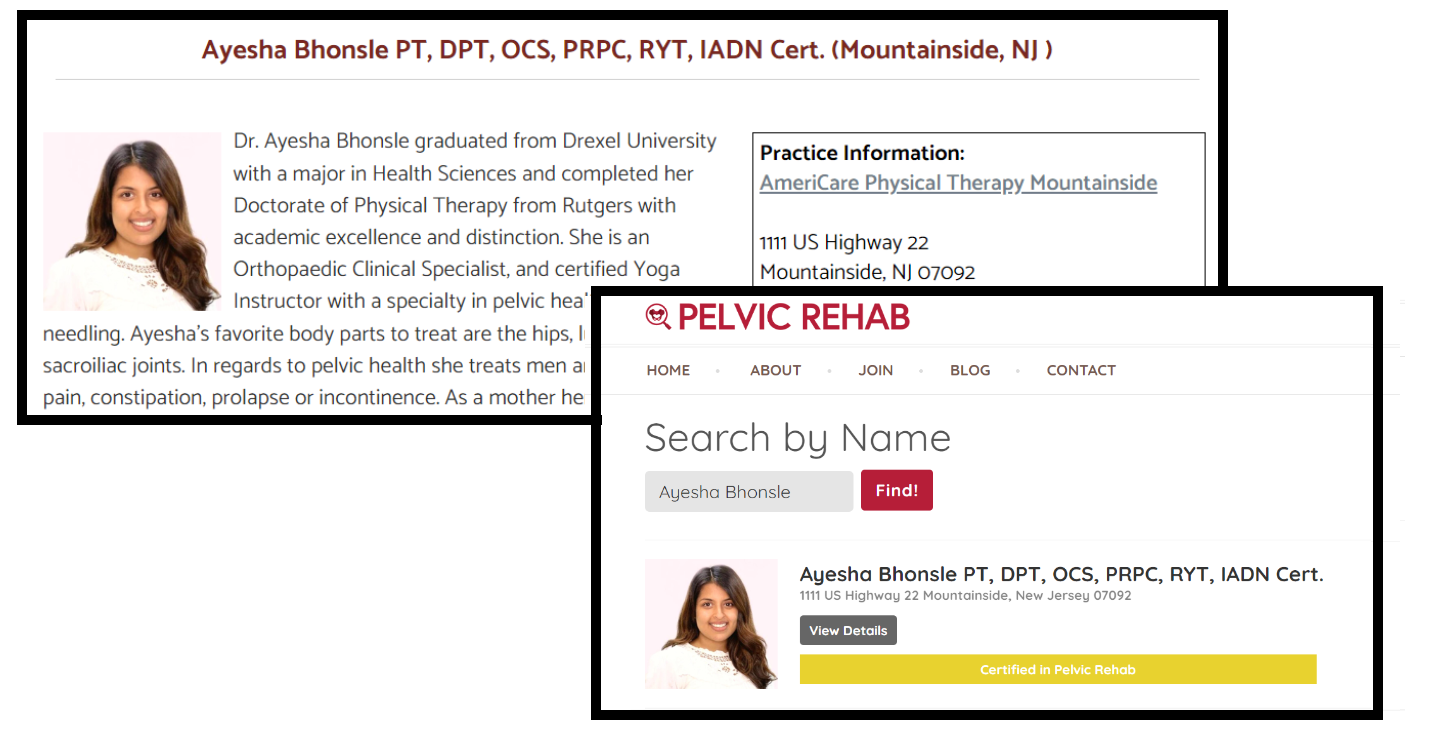
It is important that the PRPC remains current and reflects the knowledge and skills of the pelvic rehab practitioner working in the field today. The best practice for professional certification examinations like the PRPC is for them to be evaluated every 7-10 years to ensure that they continue to reflect the most current knowledge and evidence in the field.
As the PRPC will become 10 years old in 2024, HW is excited to announce that we have gathered a dedicated team of Subject Matter Experts, to analyze and update the PRPC items (multiple choice questions and answers) where needed. The Subject Matter Experts have been chosen from HW Senior Faculty and have been teaching for the Institute for over a decade. They live and work all around the United States, come from diverse backgrounds, and treat different regional patient populations all of which are important for an exam that is administered worldwide. They will be deciding which items need to be thrown out, reworked, or kept. Expected changes to the exam include updated terminology and case studies to be more inclusive of patients across the gender spectrum. The result of this process will be an exam that does not change significantly - items will still cover knowledge and skills for treating pelvic rehab patients throughout the life cycle - but that keeps up with the newest research in that field.
By going through this process, HW ensures that the PRPC remains a valid and legally defensible distinction of competence in the field.
Sarah Hughes PT, DPT, OCS, CF - L2 has been a practicing physical therapist since 2007 and opened her private practice Arrow Physical Therapy in 2016. She now owns and operates Arrow remotely while residing in the Chicago area and practicing at Outlier Physical Therapy. Her specialties include dance medicine, the CrossFit and weightlifting athlete, and conditions of the hip and pelvis such as femoroacetabular impingement and labral tears. Dr. Hughes earned a BS in exercise science from Gonzaga University and a DPT from the University of Washington, she wrote and instructs Weightlifting and Functional Fitness Athletes.
Modifying exercise, particularly CrossFit and weightlifting exercises, when pregnant is critical to reducing your risk for injury. It’s hard to do for sure. We all want to maintain our fitness and remain competitive. But, the priority during and after pregnancy is the safety and health of both baby and the birthing person.
Remember, just because you aren’t in pain or you are still capable of performing in the way you did pre-pregnancy, you may be doing yourself a disservice by setting yourself up for problems down the line, or at the very least some bad habits as you change your technique with various movements.


The message below is written by HW Senior Faculty Member Jennafer Vandevegte and Elizabeth Akincilar, the Co-Program Directors of the Pelvic Health Physical Therapy Program.
I am writing to introduce an exciting new initiative that will create scholarship opportunities for Kenyan physical therapists pursuing a degree specializing in pelvic health physical therapy.
The Jackson Clinics Foundation was formed in 2012 to fund educational efforts in East Africa. To date, the foundation has sent over 100 faculty members from their clinics and from around the country to teach in East and Central Africa. Some of the best and brightest physical therapists in the United States have volunteered their time to travel to Africa to teach these students and upgrade their education.
In 2019 the Pelvic Health Physical Therapy program in Kenya was launched by the Jackson Clinics Foundation and the Kenya Medical Training College with educational content and instructor support from the Herman and Wallace Pelvic Rehabilitation Institute and Pelvic Health and Rehabilitation Center. As you may be aware, pelvic health issues have become increasingly common in Kenya, with millions of people suffering from conditions like urinary incontinence, pelvic organ prolapse, and sexual dysfunction secondary to untreated medical conditions such as vaginal fistulas and the deleterious effects of female genital mutilation and prostate cancer. Unfortunately, there is a lack of trained professionals in this field to provide the necessary care and treatment to those affected. In fact, this program trained the first group of pelvic health physical therapists in all of East Africa.
Due to the enormous success of the initial Pelvic Health Physical Therapy program and the growing need for specialized physical therapists, The Jackson Clinics Foundation has created a two-year degree specializing in Pelvic Health. This program will become available to Kenyan physical therapists in 2024. This advanced degree will provide extensive training in assessing and treating various pelvic health conditions for adults and children. Additionally, graduates of this program will also learn how to teach their medical colleagues about pelvic health issues, bringing much-needed attention to the grossly untreated pelvic health conditions in East and Sub-Saharan Africa.
The tuition costs for this program are the primary obstacle preventing therapists from pursuing this advanced degree; therefore, we have established the Pelvic Health Physical Therapy Scholarship Fund. The fund will provide financial assistance to physical therapists in Kenya who are interested in pursuing their specialized training in Pelvic Health.
The scholarship fund seeks to raise $36,000 over the next year. We would be honored if you could contribute any amount towards this goal. Your tax-deductible contribution will go directly to the scholarship fund and will be used exclusively for pelvic health program scholarships.
Please visit our website to donate to this fund. Click on the dropdown menu to select Pelvic Heath. We appreciate any support you can offer us.
Thank you for considering this request. The infrastructure is in place, and the programs are ever-expanding and improving. These initiatives have one purpose: To improve human lives. We function under one premise, "Teach One - Treat Many." Together, we can create a healthier and more vibrant future for Kenyan communities.
Sincerely,
Elizabeth Akincilar Jennafer Vandevegte
Co-Program Director Co-Program Director
Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Christine joined Olathe Health in 2010 to further focus on women’s health and obtain her CMPT from the North American Institute of Manual Therapy. She also went through Diane Lee's integrated systems model in 2018. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician that wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process.
What was your motivation for creating this course?
As I was entering my mid-40s, I started to experience some physiological symptoms that were a bit unnerving. My sleep was inconsistent. My menstrual cycle which used to be every 35 days now was every 21 – and it changed. It lasted longer and was much heavier than before. I also started to experience heart palpitations. I sought out care from my primary care doctor, who ran labs and referred me to a cardiologist. I was placed on a halter monitor and underwent a cardiac ultrasound. The tests all came back..... normal. But I didn’t feel normal. What was happening with my body and why didn’t any of the health professionals that I consulted seem to have any answers? That was where my journey began. I started reading and researching. What I soon learned was that these symptoms, while bothersome and a little unnerving, were common. They often begin as the ovary is changing in its ability to produce hormones. I learned there are ways to manage symptoms through lifestyle choices and treatments that can help in a stage of life that can last for over 20 years. I then started to listen, really listen, to what my patients were telling me about their bodies. I had answers for them about what they were experiencing and could offer some solutions and referrals to the appropriate healthcare providers. While they were all very grateful, I kept hearing the same frustrations. Why don’t more healthcare providers know about perimenopause and menopause? Why am I being told that I must live with my symptoms? Why aren’t more providers well-versed in treatment options? That was my “aha” moment. If more healthcare providers knew about these changes and the symptoms that manifest as a result, hundreds if not thousands of patients could get the care that they need. I wrote Menopausal Transitions and Pelvic Rehab in an effort to bridge the gap in knowledge that currently exists for many of the health care providers treating this patient population. It is a culmination of hours of research into hormones, physiology, health impacts, and treatment options during this time.








































