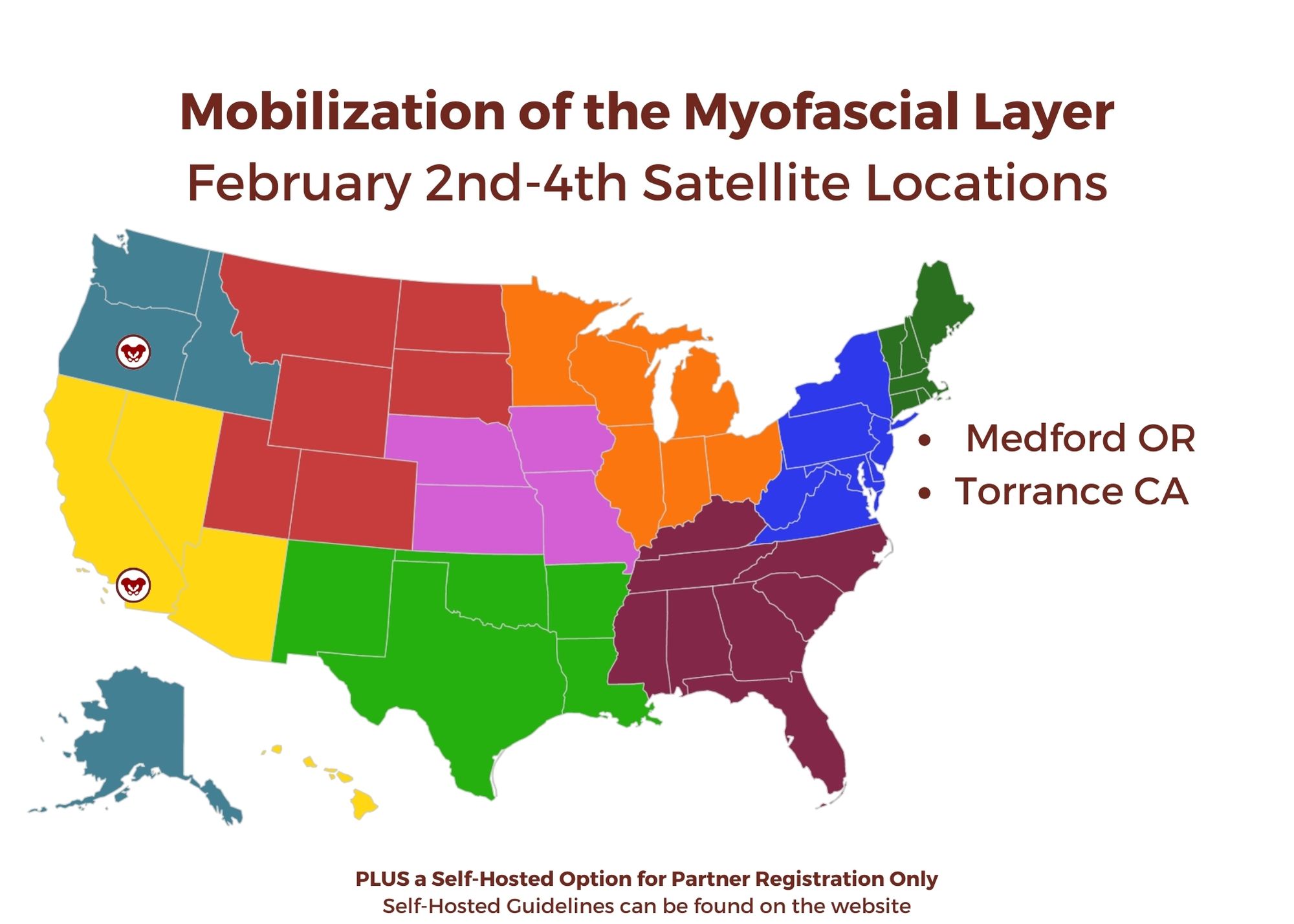
Ramona Horton, MPT, DPT developed and instructs the visceral and fascial mobilization courses for HW and presents frequently at local, national, and international venues – including International Pelvic Pain Society, CSM and HWConnect - on topics relating to women’s health, pelvic floor dysfunction, and manual therapy. Join Ramona in her upcoming course, Mobilization of the Myofascial Layer: Pelvis and Lower Extremity this February 2-4, 2024.
1. Learn from Ramona Horton!
Ramona C. Horton MPT, DPT serves as the lead therapist for her clinic’s pelvic dysfunction program in Medford, OR. Her practice focuses on treating adults and children with urological, gynecological, and colorectal issues. Her PT career began in the US Army, and she has taken the military “mission first” mentality into her approach to patient care. Simply said, “Diagnosis is just a label, perform a comprehensive musculoskeletal evaluation and treat what you find”. For her many contributions to the field of pelvic health, Ramona was awarded the prestigious Academy of Pelvic Health Elizabeth Noble Award in 2020.
There has been a bit of buzz on the various news outlets and social media feeds about the “new organ” the interstitium. On March 27th an article appeared in Scientific Reports, an online peer-reviewed journal from the publishers of Nature. This work was presented by a team of researchers that utilized a new in vivo laser endomicroscopy technique that demonstrated this tissue is a matrix of collagen bundles and elastic fibers surrounded by fluid rather than the tightly packed layers of connective tissue that was previously observed on fixed slides . This submucosal layer was observed in the entire gastrointestinal tract, the urinary bladder, bronchus, dermis, bronchus and peri-arterial soft tissue and fascia. The authors state, “In sum, we describe the anatomy and histology of a previously unrecognized, though widespread, macroscopic, fluid-filled space within and between tissues, a novel expansion and specification of the concept of the human interstitium” Benias et al., 2018.
The only thing ‘new’ is the way that this group of scientists observed the tissue that until now has primarily been studied ex vivo. I find it rather humorous to note that it is mainstream news that histologists in the 21st century just realized that there is a difference in the architecture of living versus dead tissue. They noted a significant change in the appearance of tissue slides that were chemically fixed in the traditional manner when compared to studies of in vivo structures as well as fresh frozen samples. The researchers noted this tissue in the dermis as well as urinary system, gastrointestinal system and respiratory system. This further supports one of my favorite talking points presented in the visceral mobilization courses “fascia is fascia is fascia is fascia.”
As an instructor that presents entire courses around the importance of the fascial system within all structures of the body including the dermis, epimysium, all organs, and the adventitia of vessels, I am thrilled to see this layer of the fascial system receive recognition and garner the attention it deserves. However, to refer to the interstitium as a new undiscovered organ is to ignore the work of the International Fascia Research Congress as well as many other notable scientists. These researchers see the fascial system as the dynamic mesenchymal tissue that unites every cell in the body and allows for fluid and tissue movement.
Today we get to hear from Ramona Horton, MPT, who teaches several courses with the Herman & Wallace Institute. Her upcoming course, Visceral Mobilization Level 1: Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction in the Urologic System, will be taking place November 6-8, 2015 in Salt Lake City, UT.
This spring I reached a milestone in my career. I have been working as a licensed physical therapist for 30 years, of which the past 22 have been in the field of pelvic dysfunction. Other than some waitressing stents and a job tending bar while in college this is the only profession I have known. When I entered the US Army-Baylor program in Physical Therapy in the fall of 1983 nowhere was it on my radar screen that I would be dealing with the nether regions of men, women and children, let alone teaching others to do so. As time marches on, I find myself visiting my hair dresser a bit more frequently to deal with that ever progressive grey hair that marks the passage of these years…translation: I am an old dog and I have been forced to learn some new tricks.
Like many aspects of our modern life, the profession of physical therapy is under a constant state of evolution. The best example of this is the way we look at pain and physical dysfunction. I was educated under the Cartesian model, one that believed pain is a response to tissue damage. Through quality research and better understanding of neuroscience we now know that this simplistic model is, in a word, too simple. We have come to recognize that pain is an output from the brain, which is acting as an early warning system in response to a threat real or perceived. I wholeheartedly embrace the concept that pain is a biopsychosocial phenomenon; however I am not willing to give up my treatment table for a counselors couch when dealing with persistent pain patients.
The following post was contributed by Herman & Wallace faculty member Ramona Horton. Ramona teaches three courses for the Institute; "Myofascial Release for Pelvic Dysfunction", "Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction - Level 1: The Urologic System", and "Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction - Level 2: The Reproductive System". Join her at Visceral Mobilization of the Urologic System - Madison, WI on June 5-7!
My physical therapy training and initial experience were in the US Army, so I had a strong bias toward utilization of manual therapy techniques based on a structural evaluation. When the birth of my 10 pound baby boy threw me head-long into the desire to become a pelvic dysfunction practitioner, I became plagued by the question: how do you treat the bowel and bladder, without treating the bowel and bladder? That, along with a mild obsession for the study of anatomy was the genesis of my desire to explore the technique of visceral mobilization.
The field of pelvic physical therapy has moved far beyond the rehabilitation of the pelvic floor muscles for the purpose of gaining continence, which was its origin. Now pelvic rehabilitation is a comprehensive specialty within the PT profession, treating a variety of populations and conditions (Haslam & Laycock 2015). Research has provided a greater understanding of the abdomino-pelvic canister as a functional and anatomical construct based on the somatic structures of the abdominal cavity and pelvic basin that work synergistically to support the midline of the body. The canister is bounded by the respiratory diaphragm and crura, along with the psoas muscle whose fascia intimately blends with the pelvic floor and the obturator internus and lastly the transversus abdominis muscle (Lee et al. 2008). The walls of this canister are occupied by and intimately connected to the visceral structures found within. These midline contents carry a significant mass within the body. In order for the canister to move, the viscera must be able to move as well, not only in relationship to one another, but with respect to their surrounding container. There are three primary mechanisms by which disruption of these sliding surfaces could contribute to pain and dysfunction: visceral referred pain, central sensitization and changes in local tissue dynamics.





































