Herman & Wallace has more than 55 different courses with over 200 individual course events scheduled throughout the year to choose from. Our course catalog is growing all the time with new courses, new instructors, more course dates, and even more satellite locations!
In 2022 there are already six BRAND NEW courses available, with more to be planned. H&W is kicking off the new year strong with Dr. Michael Hibner on January 9th with Pudendal Dysfunction: The Physician's Perspective. Kristina Koch is back in 2022 with her newly updated and reformated course, Pharmacologic Considerations for the Pelvic Health Provider which is scheduled for April 10, July 9, and November 19th.
Do you live near Salt Lake City, Utah? Our first live, in-person course since the pandemic will be there on March 12-13, 2022: Dry Needling and Pelvic Health.
In an excerpt from a conversation with The Pelvic Rehab Report, Tara Sullivan discusses her course, Sexual Medicine in Pelvic Rehab. She imparts, "As rehab professionals, we are in a unique position to bridge the gap between disciplines with our extensive time for exams and differential diagnoses. Many causes of dyspareunia, vestibulodynia, and IC-type symptoms can be diagnosed by careful observation and testing of the vestibule. This is often the missing link in resolving the patient's symptoms of burning, itching, urgency, and pain."
Sexual Medicine in Pelvic Rehab covers lecture topics that are often taboo in Western cultures, such as hymen myths, female squirting, G-spot, sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, and orgasm. She also discusses vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, and post-prostatectomy issues.
So what is Vestibulodynia? Vestibulodynia is a localized form of vulvodynia. The Baylor College of Medicine defines vestibulodynia as "chronic pain or discomfort that occurs in the area around the opening of the vagina, inside the inner lips of the vulva. This area is known as the vestibule."
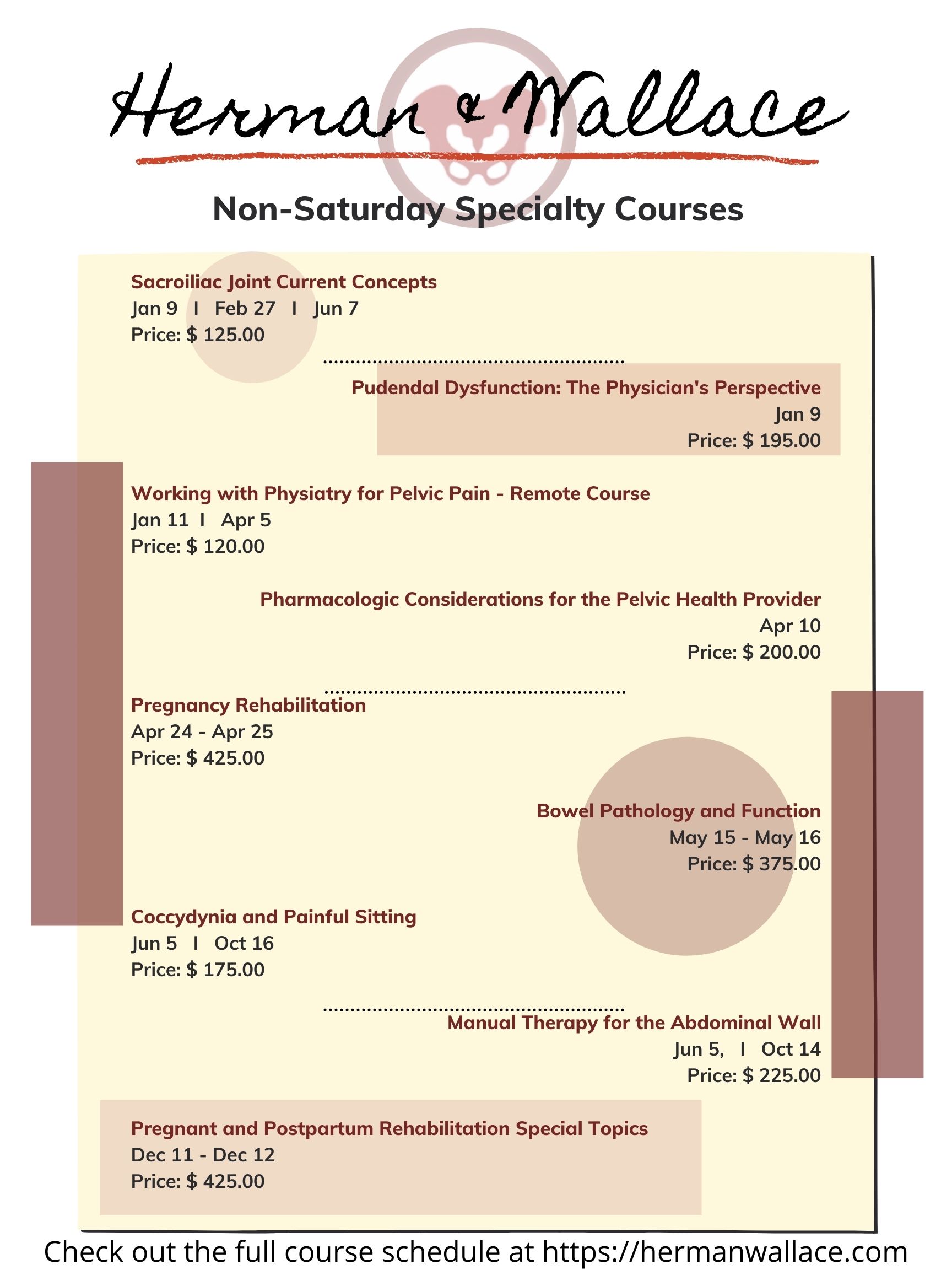
Did you know that Herman & Wallace provides continuing education courses for other weekdays than Saturday?
There is a wide selection of courses that fall on other weekdays. From Pelvic Floor Level 1 scheduled March 20-21, 2022 on Sunday and Monday to our specialty courses such as Working with Physiatry for Pelvic Pain scheduled for Tuesday, January 11, 2022.
Are you interested in attending a satellite lab course, but don't see a satellite available? Do you know a clinic that would be able to host? Feel free to reach out to us through the Host A Course form online.
Generally, H&W is looking for locations to host that have the following:
Dr. Michael Hibner is an international expert on pudendal neuralgia and chronic pelvic pain. Dr. Hibner joins Holly Tanner to discuss his new exclusive course with H&W titled Pudendal Dysfunction: The Physician's Perspective.
This blog includes portions of an interview with Ramona Horton. Ramona serves as the lead therapist for her clinic's pelvic dysfunction program in Medford, OR. Her practice focuses on patients with urological, gynecological, and colorectal issues. Ramona has completed advanced studies in manual therapy with an emphasis on spinal manipulation, and visceral and fascial mobilization. She developed and instructs her visceral and fascial mobilization courses for the Herman & Wallace Pelvic Rehabilitation Institute, and presents frequently at local, national, and international venues on topics relating to women’s health, pelvic floor dysfunction, and manual therapy.
How did you start in pelvic rehabilitation and visceral mobilization?
My PT training was through the Army-Baylor program, I was all in for orthopedics and sports medicine until October of 1990. I gave birth to my second child, an adorable, but behemoth, 9lb 9oz baby boy. His delivery, a VBAC (vaginal birth after cesarean) was very traumatic on my pelvis, I sustained pudendal nerve injury and muscular avulsion. When I queried the attending OB-GYN about my complete lack of bladder control his response and I quote “do a thousand Kegels a day, and when you’re 40 and want a hysterectomy, we’ll fix your bladder then.” As for the desire to study visceral mobilization, that reflects back to my PT training through the US Army which was 30 years ago, when the MPT was just getting started. It was an accelerated program, to say the least. We received a master's in physical therapy with 15 months of schooling. Given the very limited timeline, which included affiliations and thesis, the emphasis in our training was on critical thinking and problem solving, not memorization and protocols which in 1985 was not the norm. I can still hear the words of our instructors “You have to figure it out, I am not going to give you a cookbook."
Erika Vitek is kicking off the new year with her remote course Parkinson Disease and Pelvic Rehabilitationscheduled for January 14-15, 2022. In this course, she explains that akinesia is a term to describe the movement dysfunction observed in people with Parkinson Disease (PD). Akinesia is defined as poverty of movement, impairment or loss of the power to move, and slowness in movement initiation. This is observable in the loss of facial expression, associated nonverbal communicative movements, arm swing with gait, and overall small amplitude movements throughout all skeletal muscles in the body.
The cause of this characteristic profile of movement is due to loss of dopamine production in the brain, which causes a lack of cortical stimulation for movement(1). If the loss of dopamine production in the brain causes this poverty of movement in all skeletal muscles of the body, how does the pelvic floor function in people with PD, and what should the pelvic floor rehabilitation professional know about treating the pelvic floor in this population of patients?
Common pelvic floor dysfunctions often involve functions controlled through reflexes and voluntary actions such as bladder, bowel, and sexual functions. PD-related pelvic floor dysfunctions impact the non-motor portion of the bladder, bowel, and sexual functions. A recent study by Gupta et al. showed that “urinary dysfunction and constipation, manifestations of pelvic floor dysfunction are common sources of disability and impaired quality of life in women with PD(2).” This study concluded that pelvic floor dysfunction is underreported and undertreated in people with Parkinson's Disease.
Holly Tanner Short Interview Series - Episode 2 featuring Deb Gulbrandson
Holly Tanner and Deb Gulbrandson sat down to discuss the Osteoporosis Management Remote Course and why it is important for practitioners to recognize and know how to safely treat and manage osteoporosis patients in their practices.
Deb Gulbrandson shares the goal of the Osteoporosis Management remote course: "This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS...we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients."
Join H&W at the Osteoporosis Management remote course, scheduled for September 18-19, 2021, to learn more about treating patients with osteoporosis.








































