Effects of Exercise on Polycystic Ovary Syndrome
Few patients discuss polycystic ovary syndrome (PCOS) in orthopedic manual therapy, but one lady left a lasting impression. She was adopted and did not know her family’s medical history or her genetics. At 18, she had a baby as a result of rape. At 34, she was married and diagnosed with POCS. She struggled with infertility, anxiety, obesity, and hypertension. Although I saw her for cervicalgia, the exercise aspect of her therapy had potential to impact her overall well-being and possibly improve her PCOS symptoms.
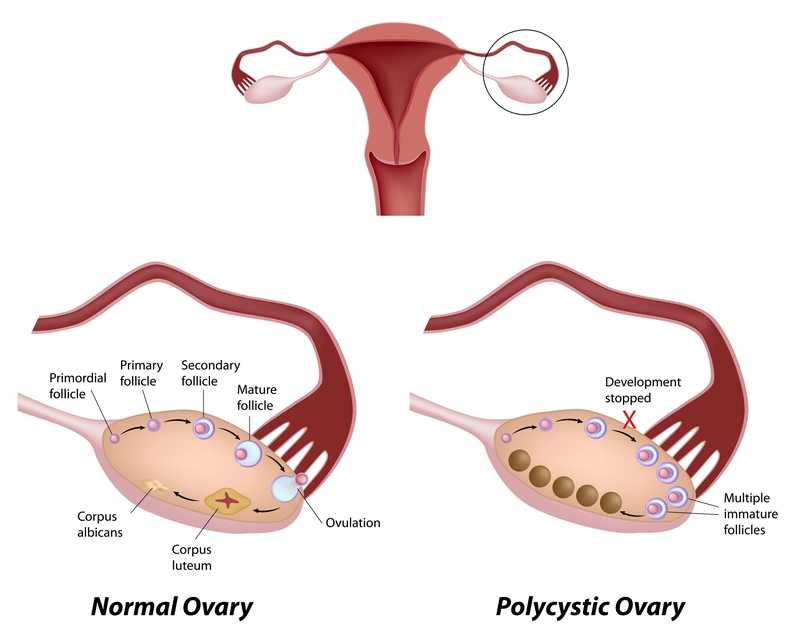 Pericleous & Stephanides (2018) reviewed 10 studies that considered the effects of resistance training on PCOS symptoms. Some of these symptoms include the absence of or a significant decrease in ovulation and menstruation, which can lead to infertility; obesity, which in turn can affect cardiovascular health and increase the risk of diabetes, insulin resistance, and metabolic syndrome; and, mental health problems. Research has shown resistance training benefits include lowering body fat, improving insulin resistance and glucose metabolism, and increasing insulin sensitivity in type II diabetes. Although it has been documented that obesity and insulin resistance can exacerbate PCOS symptoms, resistance training is not a common recommendation in healthcare settings for patients with PCOS . Studies have shown diet and exercise are essential to improve cardiac and respiratory health and body makeup in patients with PCOS, as the combination improves the Follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), ovulation, testosterone levels, and weight loss. One systematic review found that weight loss can improve PCOS symptoms without consideration of diet; however, most other studies find intake of various macronutrients (protein, fat, carbohydrates) may lead to different results, and the effects of resistance training can only be optimized with appropriate dietary changes. These authors concluded caloric consumption and macronutrient habits must be considered in conjunction with resistance training to determine the greatest impact on improving PCOS symptoms.
Pericleous & Stephanides (2018) reviewed 10 studies that considered the effects of resistance training on PCOS symptoms. Some of these symptoms include the absence of or a significant decrease in ovulation and menstruation, which can lead to infertility; obesity, which in turn can affect cardiovascular health and increase the risk of diabetes, insulin resistance, and metabolic syndrome; and, mental health problems. Research has shown resistance training benefits include lowering body fat, improving insulin resistance and glucose metabolism, and increasing insulin sensitivity in type II diabetes. Although it has been documented that obesity and insulin resistance can exacerbate PCOS symptoms, resistance training is not a common recommendation in healthcare settings for patients with PCOS . Studies have shown diet and exercise are essential to improve cardiac and respiratory health and body makeup in patients with PCOS, as the combination improves the Follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), ovulation, testosterone levels, and weight loss. One systematic review found that weight loss can improve PCOS symptoms without consideration of diet; however, most other studies find intake of various macronutrients (protein, fat, carbohydrates) may lead to different results, and the effects of resistance training can only be optimized with appropriate dietary changes. These authors concluded caloric consumption and macronutrient habits must be considered in conjunction with resistance training to determine the greatest impact on improving PCOS symptoms.
Benham et al., (2018) also performed a recent systematic review to assess the role exercise can have on PCOS. Fourteen trials involving 617 females of reproductive age with PCOS evaluated the effect of exercise training on reproductive outcomes. The data published did not allow the authors to quantitatively assess the impact of exercise of reproductive in PCOS patients; however, their semi-quantitative analysis allowed them to propose exercise may improve regularity of menstruation, the rate of ovulation, and pregnancy rates in these women. Via meta-analysis, secondary outcomes of body measurement and metabolic parameters significantly improved after women with PCOS underwent exercise training; however, symptoms such as acne and hirsutism (excessive, abnormal body hair growth) were not changed with exercise. The authors concluded exercise does improve the metabolic health (ie, insulin resistance) in women with PCOS, but evidence is insufficient to measure the exact impact on the function of the reproductive system.
Increasing our knowledge about comorbidities such as PCOS, regardless of our practice setting, can help us provide better education to the patients we treat. Perhaps exercise compliance can increase when patients are told multiple long-term benefits, not just immediate symptom relief. More often than not, a patient’s 4-6 week interaction with us could motivate and promote healthy lifestyle changes.
Pericleous, P., & Stephanides, S. (2018). Can resistance training improve the symptoms of polycystic ovary syndrome? BMJ Open Sport — Exercise Medicine, 4(1), e000372. http://doi.org/10.1136/bmjsem-2018-000372
Benham, J. L., Yamamoto, J. M., Friedenreich, C. M., Rabi, D. M. and Sigal, R. J. (2018), Role of exercise training in polycystic ovary syndrome: a systematic review and meta‐analysis. Clin Obes, 8: 275-284. doi:10.1111/cob.12258
Suggested newly published resource for readers…
Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., … Yildiz, B. O. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction (Oxford, England), 33(9), 1602–1618. http://doi.org/10.1093/humrep/dey256
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./








































