Pelvic Floor: Does Posture Matter?
Posture is a concept that rehab clinicians have long hung our hats on, and yet updated models of evaluation and care take into account the truth that there are plenty of humans functioning in poor postures who do not complain of musculoskeletal pain or other dysfunctions. Is postural dysfunction always, or never, causative? As with many things in life, the answer is likely somewhere in between. If our patient arrives at the clinic with a dysfunctional posture and improving their alignment eases discomfort and improves function, we have provided help with addressing posture. It is also likely that we have spent a bit too much time lecturing on the elusive “ideal” posture, when in fact dynamic and adaptive postures are more often occurring throughout a person’s day. Certainly computer postures add to a patient’s movement challenge, and we continue to learn more about the best ways for patients to manage the otherwise potentially static and unhealthy positions that add to many of our patients’ issues.
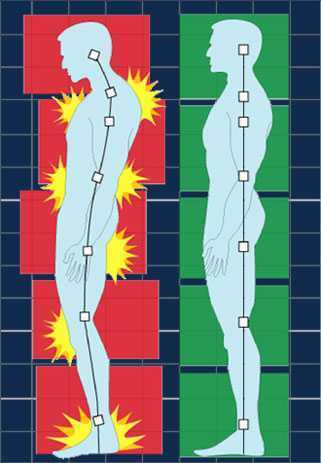 In regards to the pelvic floor, does changing standing lumbopelvic posture affect pelvic floor muscle (PFM) activation? This is the question asked by researchers from Queen’s University in Canada. (Capson et al., 2011) Sixteen women ages 22-41 who had never given birth and who were continent participated in the study. They were assessed completing five tasks in three different postures: normal lumbopelvic posture, hyperlordosis, and hypolordosis. The tasks included quiet standing, maximal effort cough, Valsalva maneuver, pelvic floor maximal voluntary contraction, and a load-catching activity. A vaginal sensor was to use to collect electromyographic activity of the pelvic floor, and sensors were placed on trunk muscles including the rectus abdominus, external and internal obliques, and erector spinae. A perineometer was utilized separately to record manometry measures, and 3D motion analysis was used to position women in the appropriate lumbopelvic angles. Key results of the investigation are summarized below:
In regards to the pelvic floor, does changing standing lumbopelvic posture affect pelvic floor muscle (PFM) activation? This is the question asked by researchers from Queen’s University in Canada. (Capson et al., 2011) Sixteen women ages 22-41 who had never given birth and who were continent participated in the study. They were assessed completing five tasks in three different postures: normal lumbopelvic posture, hyperlordosis, and hypolordosis. The tasks included quiet standing, maximal effort cough, Valsalva maneuver, pelvic floor maximal voluntary contraction, and a load-catching activity. A vaginal sensor was to use to collect electromyographic activity of the pelvic floor, and sensors were placed on trunk muscles including the rectus abdominus, external and internal obliques, and erector spinae. A perineometer was utilized separately to record manometry measures, and 3D motion analysis was used to position women in the appropriate lumbopelvic angles. Key results of the investigation are summarized below:
- Baseline EMG activity of the PFMs and the trunk muscles was significantly lower in supine versus standing
- PFM EMG activity in standing hypolordotic was higher than normal or typical posture
- Trunk muscle EMG activity did not significantly change during the 3 quiet standing postures
- For maximal PFM contraction and for cough, Valsalva, and load-catching, lower EMG activity was measured in standing in hyperlordotic or hypolordotic postures compared to “normal” or habitual posture
- With cough, all muscles except the erector muscles demonstrated increased activity
- In general, EMG activity was increased in trunk muscles when the subjects were in their habitual posture
- Related to timing of the rectus abdominus (RA) muscles, the RA were activated 106 ms before the PFM
- In standing, the intravaginal pressure was significantly higher in the hypolordotic posture compared to hyperlordotic posture
How can we put this valuable research to work in the clinic? This study validates a typical EMG activity finding of increased activity during standing versus lying, which makes sense given the pelvic tasks of working against gravity. In addition, it may be the case that our patients can generate an optimal amount of pelvic muscle contraction (when strengthening) in a more neutral posture. It may also be worth considering that for our patients who are chronically holding, perhaps a tendency for them to be in a hypolordotic posture is perpetuating their dysfunction. The data on timing of trunk and pelvic floor muscles was less consistent, although not less interesting. This research can also be implemented as an evaluation and intervention in the clinic- let’s be sure that we are using methods of feedback such as EMG, real-time ultrasound, or pressure biofeedback in various and functional positions. Then we can find out what seems to work best for our patient, whether the goal is to increase or decrease muscle activity and function.
Capson, A. C., Nashed, J., & Mclean, L. (2011). The role of lumbopelvic posture in pelvic floor muscle activation in continent women. Journal of Electromyography and Kinesiology21(1), 166-177.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./








































