Everyone experiences constipation, sometime! Maybe it was on vacation and you felt bloated and miserable; or when you were busy at work and had to rush to complete a task. In any event, you felt ‘awful’. Maybe you couldn’t zip your favorite jeans due to abdominal bloating, maybe you experienced lower abdominal discomfort or experienced a painful ‘movement’ once you went. There are many people who experience these symptoms and more on a daily basis. When someone finally gets the courage to see a specialist about this problem, they might be diagnosed with ‘pelvic floor dyssynergia’ or ‘muscle incoordination’.

Pelvic muscle dyssysnergia (incoordination) refers to the action that occurs in the pelvic floor musculature at the time of defecation. It can become a withholding pattern and in the case of vacation or a change in your work schedule, it can simply be tensing the muscle to avoid the bowel movement (due to inconvenience) rather than heeding the ‘call’. Over time, if this behavior is repeated, it becomes muscle memory; instead of relaxing the pelvic muscle to defecate, the patient tenses the muscle; thus the term dyssynergia or incoordination. The function of the pelvic floor for bowel function is to provide closure of the anal canal to maintain continence. The muscle should signal the rectum and the colon when to defecate and should provide opening of the anal canal by total relaxation to allow for complete and effortless elimination. A dyssynergic pattern shuts the opening of the canal by tensing the muscle to prevent elimination. Thus an incoordination.
The research by Heymen, Scarlett, Ringman, Drossman et al entitled “Randomized, Controlled Trial Shows Biofeedback to Be Superior to Alternative Treatments for Patients with Pelvic Floor Dyssynergia-Type Constipation” supports the value of biofeedback in the treatment of this withholding pattern associated with stool elimination. This study supports the benefit of biofeedback treatments using internal sensors to provide the feedback displayed on a computer screen for visualization. This study goes on to say, “We also have shown that the machines are necessary—instrumented biofeedback is an essential element of successful training; however, there is a shortage of practitioners who are trained to provide this form of biofeedback, and there are few clinics where biofeedback instruments are available and where this form of biofeedback can be obtained”.
Biofeedback provides visual and auditory feedback of muscle tension. It is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function, enabling the patient to learn how to alter the physiological process through verbal and visual cues. This mechanism allows the patient to assess muscle resting tone, creating an environment that teaches how to downtrain a tense pelvic floor while providing the means to teach co-ordination of muscle function.
In short, biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors associated with tensing the pelvic floor for defecation instead of the proper relaxation of the pelvic floor for release of stool from the anal canal.
The Herman Wallace Course on Biofeedback Training for Pelvic Muscle Dysfunction provides the clinician with the proper treatment technique to use in the clinic to rehabilitate patients with pelvic floor muscle dyssynergia. Learning the proper use of biofeedback equipment and understanding the components to treating these challenging patients successfully is an essential component to this course. The clinician will learn numerous ways to teach this challenging patient population how to make this muscle function as intended, providing the patient with successful strategies for improved patient outcomes.
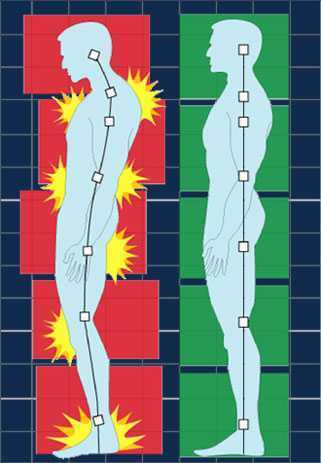
Posture is a concept that rehab clinicians have long hung our hats on, and yet updated models of evaluation and care take into account the truth that there are plenty of humans functioning in poor postures who do not complain of musculoskeletal pain or other dysfunctions. Is postural dysfunction always, or never, causative? As with many things in life, the answer is likely somewhere in between. If our patient arrives at the clinic with a dysfunctional posture and improving their alignment eases discomfort and improves function, we have provided help with addressing posture. It is also likely that we have spent a bit too much time lecturing on the elusive “ideal” posture, when in fact dynamic and adaptive postures are more often occurring throughout a person’s day. Certainly computer postures add to a patient’s movement challenge, and we continue to learn more about the best ways for patients to manage the otherwise potentially static and unhealthy positions that add to many of our patients’ issues.
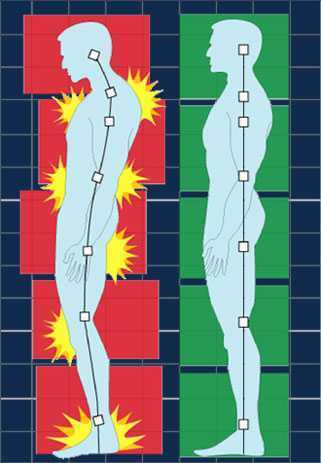 In regards to the pelvic floor, does changing standing lumbopelvic posture affect pelvic floor muscle (PFM) activation? This is the question asked by researchers from Queen’s University in Canada. (Capson et al., 2011) Sixteen women ages 22-41 who had never given birth and who were continent participated in the study. They were assessed completing five tasks in three different postures: normal lumbopelvic posture, hyperlordosis, and hypolordosis. The tasks included quiet standing, maximal effort cough, Valsalva maneuver, pelvic floor maximal voluntary contraction, and a load-catching activity. A vaginal sensor was to use to collect electromyographic activity of the pelvic floor, and sensors were placed on trunk muscles including the rectus abdominus, external and internal obliques, and erector spinae. A perineometer was utilized separately to record manometry measures, and 3D motion analysis was used to position women in the appropriate lumbopelvic angles. Key results of the investigation are summarized below:
In regards to the pelvic floor, does changing standing lumbopelvic posture affect pelvic floor muscle (PFM) activation? This is the question asked by researchers from Queen’s University in Canada. (Capson et al., 2011) Sixteen women ages 22-41 who had never given birth and who were continent participated in the study. They were assessed completing five tasks in three different postures: normal lumbopelvic posture, hyperlordosis, and hypolordosis. The tasks included quiet standing, maximal effort cough, Valsalva maneuver, pelvic floor maximal voluntary contraction, and a load-catching activity. A vaginal sensor was to use to collect electromyographic activity of the pelvic floor, and sensors were placed on trunk muscles including the rectus abdominus, external and internal obliques, and erector spinae. A perineometer was utilized separately to record manometry measures, and 3D motion analysis was used to position women in the appropriate lumbopelvic angles. Key results of the investigation are summarized below:
- Baseline EMG activity of the PFMs and the trunk muscles was significantly lower in supine versus standing
- PFM EMG activity in standing hypolordotic was higher than normal or typical posture
- Trunk muscle EMG activity did not significantly change during the 3 quiet standing postures
- For maximal PFM contraction and for cough, Valsalva, and load-catching, lower EMG activity was measured in standing in hyperlordotic or hypolordotic postures compared to “normal” or habitual posture
- With cough, all muscles except the erector muscles demonstrated increased activity
- In general, EMG activity was increased in trunk muscles when the subjects were in their habitual posture
- Related to timing of the rectus abdominus (RA) muscles, the RA were activated 106 ms before the PFM
- In standing, the intravaginal pressure was significantly higher in the hypolordotic posture compared to hyperlordotic posture
How can we put this valuable research to work in the clinic? This study validates a typical EMG activity finding of increased activity during standing versus lying, which makes sense given the pelvic tasks of working against gravity. In addition, it may be the case that our patients can generate an optimal amount of pelvic muscle contraction (when strengthening) in a more neutral posture. It may also be worth considering that for our patients who are chronically holding, perhaps a tendency for them to be in a hypolordotic posture is perpetuating their dysfunction. The data on timing of trunk and pelvic floor muscles was less consistent, although not less interesting. This research can also be implemented as an evaluation and intervention in the clinic- let’s be sure that we are using methods of feedback such as EMG, real-time ultrasound, or pressure biofeedback in various and functional positions. Then we can find out what seems to work best for our patient, whether the goal is to increase or decrease muscle activity and function.
Capson, A. C., Nashed, J., & Mclean, L. (2011). The role of lumbopelvic posture in pelvic floor muscle activation in continent women. Journal of Electromyography and Kinesiology21(1), 166-177.
One of the dilemmas for many clinicians new to pelvic rehab is trying to figure out which equipment to purchase, and how to convince their employer (or themselves) to purchase the equipment. A common question in relation to equipment for pelvic rehabilitation is “what do I really need?” In a perfect world, and based on both existing and emerging research as well as clinical practice recommendations, we would all have access to pressure biofeedback and real-time ultrasound to help us document and train our patients in best strategies. The truth, however, lies in the fact that when those devices are not available, clinical practice can gain meaningful information from our best tools: our eyes and our hands. Certainly when completing research about pelvic floor generated pressures we might choose pressure biofeedback, and when looking for muscle activation patterns, needle EMG is the right choice, but no one should deny patients the opportunity to learn how to increase or decrease muscle activity, focus on movement retraining, and learn strategies to decrease improve quality of life and function because the latest technology is unavailable.
 Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Vaginal pelvic muscle assessment via palpation has been shown to be more accurate when assessed by more experienced therapists, and use of multiple methods may be most valuable in gaining the most accurate data. In addition to validating the usefulness of pelvic muscle palpation as an evaluative tool, the authors point out that transperineal ultrasound may also be the most appropriate tool for pediatric patients or patients who are otherwise not appropriate for internal pelvic muscle assessment.
Pereira, V. S., Hirakawa, H. S., Oliveira, A. B., & Driusso, P. (2014). Relationship among vaginal palpation, vaginal squeeze pressure, electromyographic and ultrasonographic variables of female pelvic floor muscles. Brazilian journal of physical therapy, 18(5), 428-434.
 Sexual dysfunction is a common negative consequence of Multiple Sclerosis, and may be influenced by neurologic and physical changes, or by psychological changes associated with the disease progression. Because pelvic floor muscle health can contribute to sexual health, the relationship between the two has been the subject of research studies for patients with and without neurologic disease. Researchers in Brazil assessed the effects of treating sexual dysfunction with pelvic floor muscle training with or without electrical stimulation in women diagnosed with multiple sclerosis (MS.) Thirty women were allocated randomly into 3 treatment groups; 20 women completed the study. All participants were evaluated before and after treatment for pelvic floor muscle (PFM) function, PFM tone, flexibility of the vaginal opening, ability to relax the PFM’s, and with the Female Sexual Function Index (FSFI). Rehabilitation interventions included pelvic floor muscle training (PFMT) using surface electromyographic (EMG) biofeedback, neuromuscular electrostimulation (NMES), sham NMES, or transcutaneous tibial nerve stimulation (TTNS). The treatments offered to each group are shown below.
Sexual dysfunction is a common negative consequence of Multiple Sclerosis, and may be influenced by neurologic and physical changes, or by psychological changes associated with the disease progression. Because pelvic floor muscle health can contribute to sexual health, the relationship between the two has been the subject of research studies for patients with and without neurologic disease. Researchers in Brazil assessed the effects of treating sexual dysfunction with pelvic floor muscle training with or without electrical stimulation in women diagnosed with multiple sclerosis (MS.) Thirty women were allocated randomly into 3 treatment groups; 20 women completed the study. All participants were evaluated before and after treatment for pelvic floor muscle (PFM) function, PFM tone, flexibility of the vaginal opening, ability to relax the PFM’s, and with the Female Sexual Function Index (FSFI). Rehabilitation interventions included pelvic floor muscle training (PFMT) using surface electromyographic (EMG) biofeedback, neuromuscular electrostimulation (NMES), sham NMES, or transcutaneous tibial nerve stimulation (TTNS). The treatments offered to each group are shown below.
| sEMG biofeedback | Sham NMES | Intravaginal NMES | TTNS | |
| Group 1 (n=6) | X | X | ||
| Group 2 (n=7) | X | X | ||
| Group 3 (n=7) | X | X |
The following factors made up the inclusion criteria for the study: age at least 18 years, diagnosis of relapsing-remitting MS, and a 4 month history of stable symptoms. All of the participants were sexually active and were found to be able to contract pelvic floor muscles correctly. Group 1 patients were treated with “sham” electrical stimulation using surface electrodes placed over the sacrum at a pulse width of 50 ms and a frequency of 2 Hz. Patients in Group 2 used an internal (vaginal) electrode at 200 ms at 10 Hz. Group 3 were given transcutaneous tibial nerve stimulation at 200 ms and 10 Hz. All groups followed these treatments with pelvic floor muscle exercises using a vaginal sensor and biofeedback.
The authors concluded that pelvic floor muscle training alone or in combination with intravaginal neuromuscular electrostimulation or transcutaneous tibial nerve stimulation is effective in treating sexual dysfunction in women who have MS. Improvements were noted in these groups in sexual arousal, vaginal lubrication, satisfaction, and in the Female Sexual Function Index. While the numbers in the respective intervention groups is not large enough to determine the best option for patients who have multiple sclerosis, the research reminds us that neurostimulation in conjunction with pelvic muscle training may be very valuable.
Over the past 28 years, my pelvic floor has endured at least 20,000 miles of running, including racing on the collegiate level and then completing 10 marathons. Add to the high-impact sport two 8.1 pound natural childbirth deliveries 26 months apart, and you can imagine why I accepted the invitation to blog for this well-respected institute. One of my elderly patients once told me my uterus was going to drop out from so much running (which, thankfully, has NOT happened); however, I have to admit, urinary stress incontinence and frequent urination were unwelcome enough consequences! On the positive side, it all initiated my journey to understanding the pelvic floor.
![By Mike Baird [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons](/images/photos/Blog/Female_jogger.jpg)
In 2014, Poswiata et al used the Urogenital Distress Inventory (UDI-6) to assess how prevalent stress urinary incontinence may be among elite female skiers and runners. Of the 112 female athletes in the study, 50% reported leaking a small amount of urine. Coughing and sneezing provoked leakage for 45.54% of those women, indicating stress incontinence, and 58.04% of the women in the study reported frequent urination. Are those acceptable statistics? I would have to say no.
Research results can be comforting so athletes can be told they are not alone regarding a quite personal aspect of their lives. When I could supposedly empty my bladder, stand to wash my hands and have to go again, walk down the hall to put on my sneakers and go once again before heading out the door for a run, it was nice to know someone else was probably experiencing the same issue that morning. Just because it is common, though, does not make it “normal.” We are not meant to leak just because we stress our bodies beyond normal ADLs.
A very recent study by Luginbuehl et al (2015 July 21), just published online, attempted to explore the electromyography (EMG) activity of pelvic floor muscles with variable running speeds (7, 9, and 11km/h) over 10 steps. The highest pelvic floor muscle activity was recorded at 11km/h, which would sensibly suggest the muscles produce a greater contraction the faster someone runs. If a runner has developed a decreased ability to activate the pelvic floor muscles, stress urinary incontinence will likely become a highly irritating problem with fast running speeds over time. But how do they know, and where do they go?
Without health practitioners trained in rehabilitation of pelvic floor dysfunctions, consider how chronic an issue urinary stress incontinence would be for a large athletic population. So many women (and men) do not even recognize their leakage or frequent urination as treatable “issues” and never mention them to anyone. Often times, we are treating an athlete for a hip or lumbar injury and purposefully yet discretely have to ask the right questions and then educate the patient how some of their symptoms are secondary to pelvic floor deficits. Someone has to explain what is normal, and, better yet, someone HAS to make an effort to fix what is “broken” and restore the pelvic floor to a higher level of function. With the proper training, perhaps that someone can be you.
References:
1. Poświata, A., Socha, T., & Opara, J. (2014). Prevalence of Stress Urinary Incontinence in Elite Female Endurance Athletes. Journal of Human Kinetics,44, 91–96. doi:10.2478/hukin-2014-0114.
2. Helena Luginbuehl, Rebecca Naeff, Anna Zahnd, Jean-Pierre Baeyens, Annette Kuhn, Lorenz Radlinger (2015 July 21). Pelvic floor muscle electromyography during different running speeds: an exploratory and reliability study. Archives of Gynecology and Obstetrics. doi: 10.1007/s00404-015-3816-9.