Pelvic-Related Dysfunction in People with Eating Disorders

HW faculty member Carole High Gross, PT, MS, DPT, PRPC instructs her remote course, Eating Disorders and Pelvic Health Rehabilitation, on October 19-20, 2024 that takes a deep dive into the role of pelvic health rehabilitation with individuals with eating disorders.
The role of a pelvic health rehabilitation professional includes caring for individuals with dysfunction within the pelvis and abdominal canister. We treat individuals with constipation, fecal incontinence, pelvic organ prolapse, urinary dysfunction, pelvic pain, abdominal pain, and bloating (to name a few). Individuals with eating disorders often experience ALL of these symptoms. Numerous studies demonstrate bowel, bladder, and pelvic dysfunction in those with eating disorders (see reference list for some of these studies). We CAN help!
Eating disorders are mental health conditions with serious biopsychosocial implications that negatively impact the function of the body, social interactions, and psychological well-being. The American Psychiatric Association characterizes Eating Disorders (ED) as “behavioral conditions characterized by severe and persistent disturbance in eating behaviors and associated distressing thoughts and emotions.” Types of eating disorders include:
- anorexia nervosa (AN)
- bulimia nervosa (BN)
- binge eating disorder (BED)
- avoidant restrictive food intake disorder (ARFID)
- other specified feeding and eating disorders (OSFED)
- pica and rumination disorder
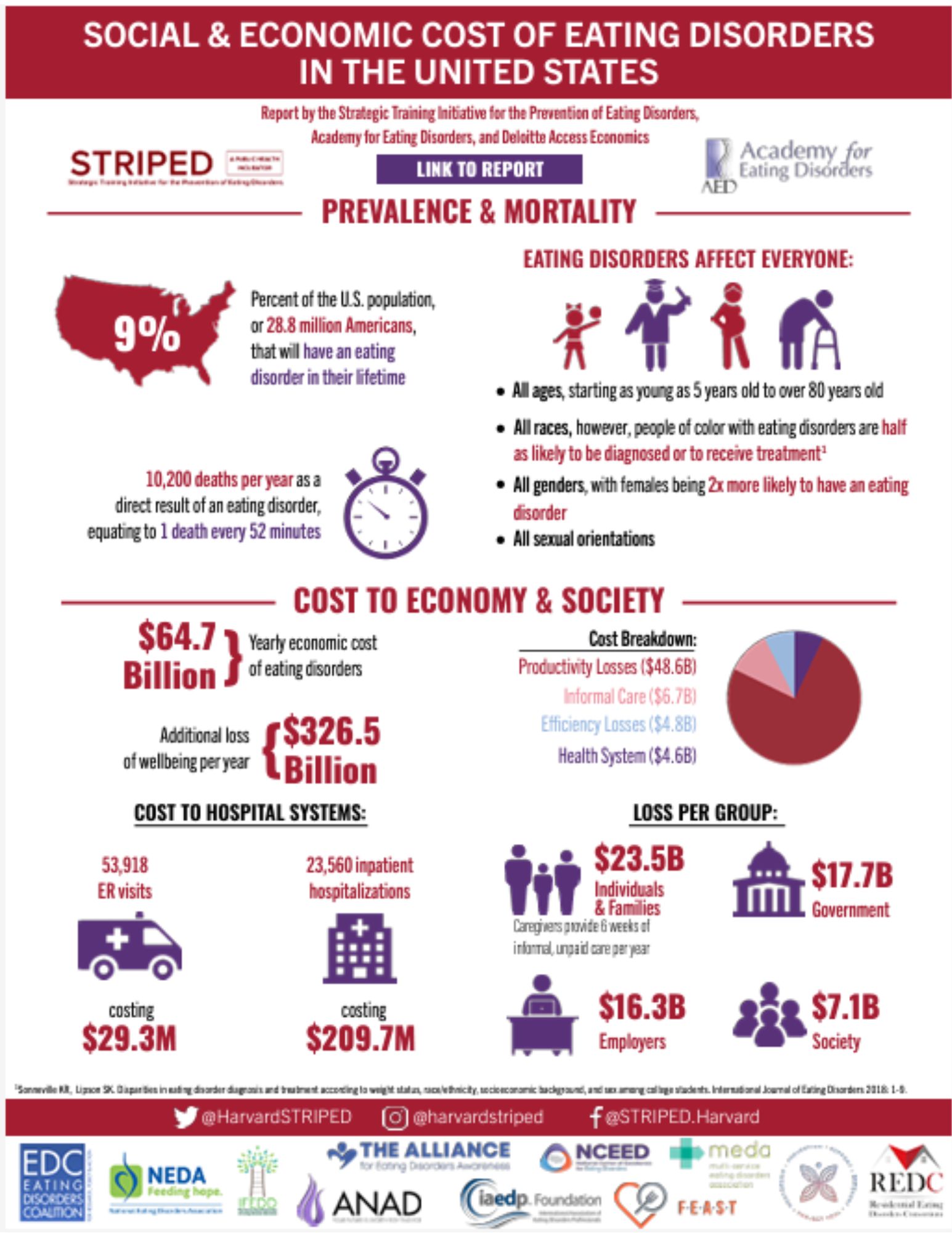
Eating disorders are estimated to affect roughly 5% of the population and are often under-reported and unidentified by the medical community. People of all genders often suffer in silence as eating disorders tend to be a very secretive and all-consuming mental illness that does not discriminate based on gender, culture, race, or nationality. Eating disorders can develop at any time in someone’s life, however, often signs develop in adolescence and early adulthood.
Supporting Research
One noteworthy article, which was published in May of 2024, was written by Monica Williams and colleagues from ACUTE, an inpatient eating disorder treatment facility, in Denver, Colorado.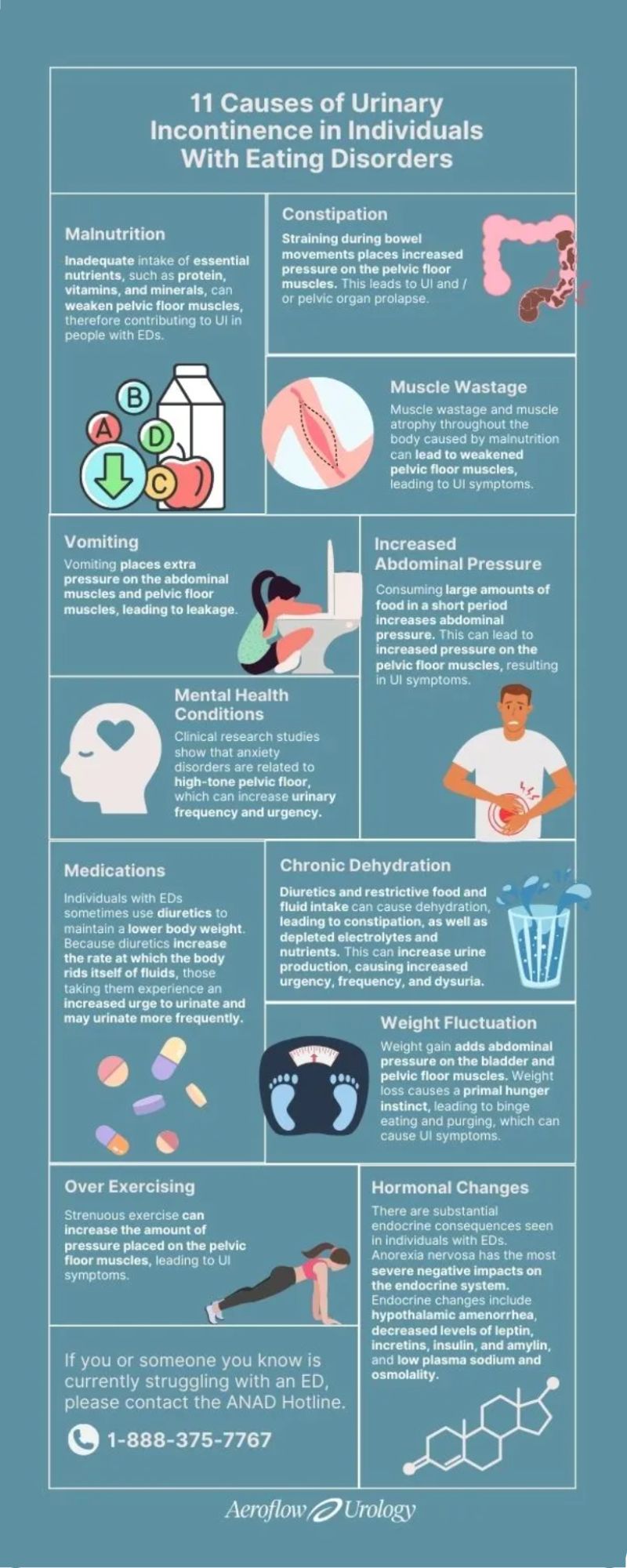 Williams et al. published a retrospective cohort study of 193 female women highlighting pelvic floor dysfunction in people with eating disorders. This study illustrated the positive effects of management (including education, pelvic floor muscle assessment, biofeedback, and active retraining of the pelvic muscle) on pelvic floor dysfunction (PFD) with the intervention group (n=84). Each of the patients in this study had only one to a few treatment sessions of selected appropriate interventions.
Williams et al. published a retrospective cohort study of 193 female women highlighting pelvic floor dysfunction in people with eating disorders. This study illustrated the positive effects of management (including education, pelvic floor muscle assessment, biofeedback, and active retraining of the pelvic muscle) on pelvic floor dysfunction (PFD) with the intervention group (n=84). Each of the patients in this study had only one to a few treatment sessions of selected appropriate interventions.
The control group received the standard of care education including mindfulness, relaxation techniques, and diaphragmatic breathing. All participants in the intervention group received a 30-minute education session which included the purpose of the pelvic floor, causes of pelvic floor dysfunction, the relationship between the pelvic floor and diaphragm, typical bladder norms, strategies to improve bowel/bladder emptying and urge suppression techniques. The Education Group (n=26) received education only without other interventions. Although this group showed improvements in the PFDI score, the improvements did not meet statistically meaningful improvement in pelvic floor dysfunction symptoms. However, the other treatment subgroups within the intervention group showed statistically meaningful improvements in pelvic floor dysfunction. The Pelvic Floor Assessment group (n=13) included individuals who received the education (noted above) and internal assessment of pelvic floor musculature with the goal of improving coordination of PFM.
The Urinary Distress Inventory 6 (UDI-6) demonstrated statistically significant improvement in the Pelvic Floor Assessment Group. The UDI-6, the Colorectal-Anal Inventory 6 (CRAD-8), and the Pelvic Organ Prolapse Distress Inventory 6 (POPDI-6) improved with the Active Retraining (of the pelvic floor muscles) Group (n=67). The individuals in the Active Retraining group received: Education (mentioned above) and bladder training (improving time between voids) and pelvic floor stretches (deep squat, butterfly, child’s pose, happy baby including coordination of diaphragmatic breathing and movement of the pelvic floor). The Biofeedback Group (n=3) received Education (mentioned above) and biofeedback including visual feedback to instruct patients on how to effectively contract and relax PFM. The Biofeedback Group showed statistical improvement with the POPDI-6 score.
Overall, Williams et al. concluded that patients with eating disorders report an increased level of pelvic floor symptoms. The interventions provided in this study were found to be beneficial. Individuals with the anorexia binge-purge subtype also had higher scores on the PFDI than the anorexia nervosa restricting subtype. The authors recommended future studies to better describe the etiology of PFD in individuals with ED and how PFD contributes to both behaviors and GI symptoms of those with eating disorders.
Ng et al., 2022, discussed research that demonstrated the relationship between eating disorders and urinary incontinence through the lens of psychoanalysis.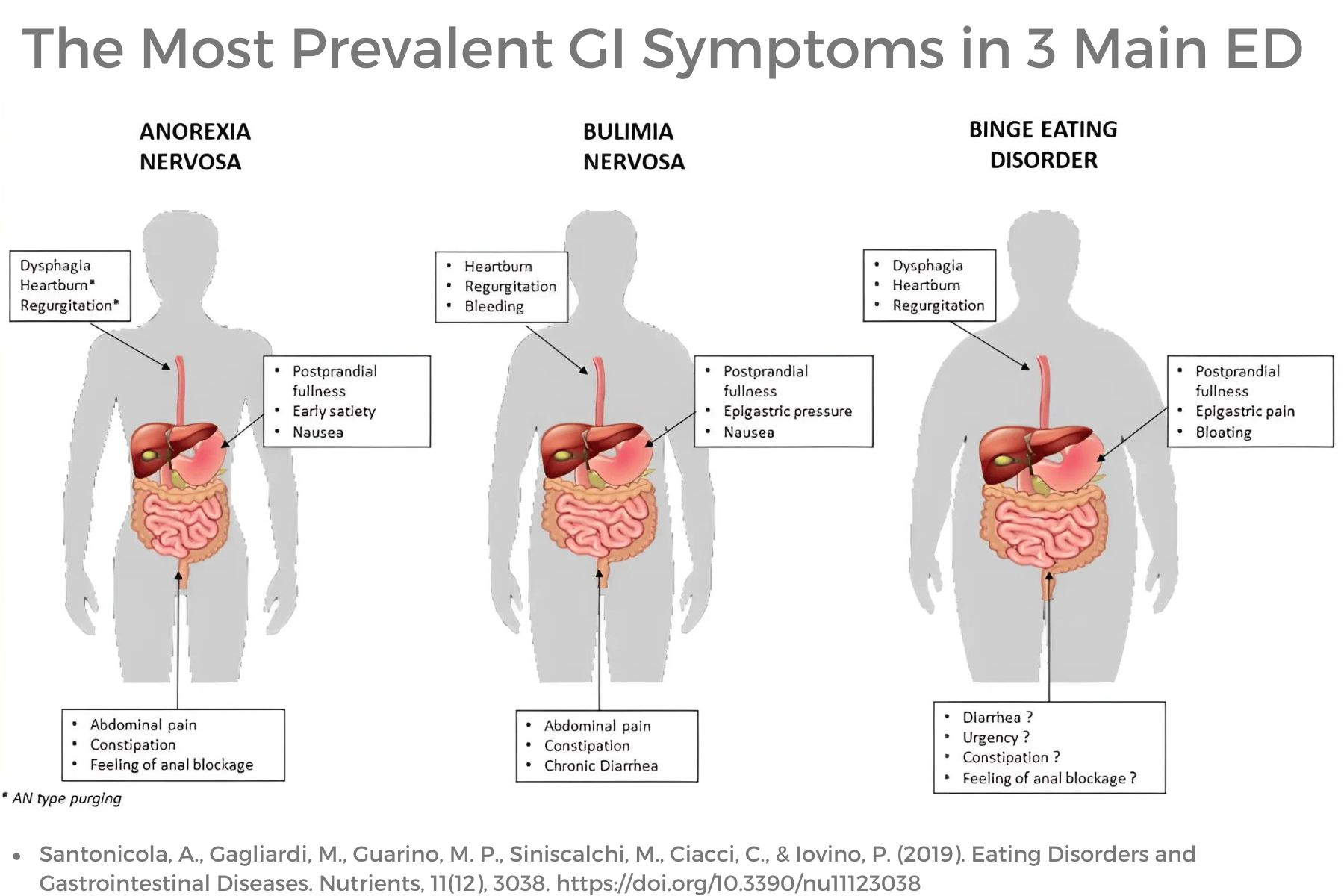 This article described mental health co-morbidities with eating disorders that contribute to urinary dysfunction. The authors also encouraged a good psychodynamic understanding of childhood relationships, personality traits, and the inner mental “landscape.” The authors reinforced mental co-morbidities contribute to increased urinary incontinence and dysfunction including poor interoceptive awareness, personality traits, decreased life satisfaction, need for control, and anxiety.
This article described mental health co-morbidities with eating disorders that contribute to urinary dysfunction. The authors also encouraged a good psychodynamic understanding of childhood relationships, personality traits, and the inner mental “landscape.” The authors reinforced mental co-morbidities contribute to increased urinary incontinence and dysfunction including poor interoceptive awareness, personality traits, decreased life satisfaction, need for control, and anxiety.
Ng and colleagues described the prominence of poor interoceptive awareness among individuals with eating disorders. Interoceptive awareness refers to awareness of one’s feelings or emotions. This may also affect a person’s perception of stimuli arising in the body, such as to perform bodily functions such as urination. Poor interoceptive awareness would likely also play a factor in awareness of the body’s need to evacuate stool however, this was not within the scope of this article. Bowel dysfunction with ED is well documented in the research.
Ng et al’s article also discusses common personality traits among individuals with some eating disorders including perfectionism and asceticism. Asceticism refers to the self-denial of physical or psychological desires or needs and can also be viewed as a ritualization of life. Often this refers to spirituality or religious practices, however, denial of bodily urges and the need for control is a common characteristic with some eating disorders which include restriction (AN, BN, OSFED). Denial of basic needs, such as urination, would reasonably reinforce the need for control. Often those with restrictive eating disorders excessively control what goes into the body and may also be restricting what is coming out of the body including feces and urine.
Anxiety and other mental health comorbidities are common in individuals with ED and can contribute to increased tone and tension in the pelvic floor contributing to urinary dysfunction. Additional research supports that this increased pelvic tone and tension also contributes to sexual dysfunction, pelvic pain, and bowel dysfunction in individuals with and without eating disorders. Mental health challenges may also lead to closed posturing, tightness in the back, hip, and shoulder musculature as well as upper chest breathing, and poor excursion of the diaphragm.
As pelvic health rehabilitation providers, we need to look at the whole person as so many factors influence pelvic-related dysfunction. Numerous factors affect bowel, bladder, and pelvic function including muscle wasting and atrophy, slow GI motility, medications, hormonal changes, weight fluctuations, purging behaviors, poor pressure management, increased intra-abdominal pressure, mental wellness comorbidities, excessive exercise, water loading, dehydration, malnutrition, poor postural alignment, length and tension of muscular and fascial systems, diaphragmatic/lower costal excursion and diversity of microbiome to name a few.
Septak posted a blog in February 2024 for the aeroflowurology.com website that discussed factors that negatively impact bladder control in individuals with anorexia nervosa and bulimia nervosa based on research.
The author discussed research implying muscle wasting and atrophy caused by malnutrition can lead to weakness in pelvic floor musculature and support structures. This contributes to urinary symptoms, however, also contributes to bowel dysfunction. The musculature around the colon when not used will atrophy and weaken.
Purging behaviors have numerous negative and potentially dangerous effects on the body function of individuals with eating disorders. Vomiting will increase pressure on PFM, pelvic organs, and abdominal musculature. Laxative use will lead to fecal issues such as fecal incontinence and can contribute to increased pressure and trauma on pelvic organs/musculature. Purging will also lead to serious electrolyte imbalances which can lead to organ system dysfunction or failure.
Other medications also influence bowel and bladder function such as diuretics, which are often mis-utilized to lower body weight through the rapid loss of body fluids. Individuals with DM Type 1 may also withhold insulin to result in a diuretic effect. This not only disrupts essential body electrolytes, but it will also lead to dehydration contributing to bowel dysfunction such as constipation. Diuresis of fluids will also increase urinary urgency, frequency, and risk for incontinence.
Constipation may be caused by numerous factors including dehydration, muscle wasting, slow motility, decreased gastric emptying, and poor nutritional intake. Upregulation of the sympathetic nervous system with trauma history, personality traits, and numerous mental health comorbidities such as anxiety, OCD, and depression, play a significant role in constipation. Bowel movement straining places excessive stress on pelvic organs, pelvic musculature, fascia, and suspension structures, as well as the abdominal wall musculature and fascia. Constipation also contributes to urinary dysfunction due to the proximity of pelvic organs and can lead to pelvic organ prolapse.
Hormonal changes due to endocrine dysfunction with eating disorders, such as with AN, BN, and OSFED, can lead to disruptions in body system function. Hormonal disruptions often lead to hypothalamic amenorrhea, reduced levels of important levels of leptin (regulates appetite, energy balance, and metabolism), insulin (regulates blood sugar and is responsible for storage of incoming food as fat/ fuel), incretins (regulates blood sugar by stimulating pancreas to produce insulin), amylin (may contribute to low bone density with AN), plasma sodium and altered osmolarity (may result in nausea, vomiting, energy loss, confusion, seizures, heart, liver, kidney dysfunction). In addition, there are disruptions with other essential electrolytes that can contribute to body organ system malfunction and failure.
As pelvic health rehabilitation providers, we know how to treat pelvic and abdominal dysfunction.
We may, in fact, be the first healthcare professional who asks the important questions or makes insightful observations that illuminate a person’s secret struggle in the darkness. We may be able to lead these individuals to healthcare providers who are skilled in diagnosing, managing, and guiding that individual into the light of recovery. While we do not treat eating disorders, we DO treat the dysfunction caused by eating disorders. So many individuals with eating disorders will benefit from our education and interventions to assist them on their recovery journey.
Join Carole High Gross, PT, MS, DPT, PRPC in Eating Disorders and Pelvic Health Rehabilitation on October 19-20 for a deep dive into the role of pelvic health rehabilitation with individuals with eating disorders. We will discuss the different eating disorders, medical complications, signs and symptoms, screening and observations, interventions, and treatment approaches.
References:
- Abbate-Daga, G., Delsedime, N., Nicotra, B., Giovannone, C., Marzola, E., Amianto, F., & Fassino, S. (2013). Psychosomatic syndromes and anorexia nervosa. BMC psychiatry, 13, 14. https://doi.org/10.1186/1471-244X-13-14[31]
- Abraham, S., Luscombe, G. M., & Kellow, J. E. (2012). Pelvic floor dysfunction predicts abdominal bloating and distension in eating disorder patients. Scandinavian journal of gastroenterology, 47(6), 625–631. https://doi.org/10.3109/00365521.2012.661762
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision DSM- 5TR. Fifth Edition. American Psychiatric Press. 2022.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders.Fifth Edition. American Psychiatric Press. 2013.
- Andersen AE, Ryan GL. Eating disorders in the obstetric and gynecologic patient population [published correction appears in Obstet Gynecol. 2010 Nov;116(5):1224]. Obstet Gynecol. 2009;114(6):1353-1367. doi:10.1097/AOG.0b013e3181c070f9
- Bodner-Adler, B., Alarab, M., Ruiz-Zapata, A. M., & Latthe, P. (2020). Effectiveness of hormones in postmenopausal pelvic floor dysfunction-International Urogynecological Association research and development-committee opinion. International urogynecology journal, 31(8), 1577–1582. https://doi.org/10.1007/s00192-019-04070-0
- Bulik CM, Reba L, Siega-Riz AM, Reichborn-Kjennerud T. Anorexia nervosa: definition, epidemiology, and cycle of risk. Int J Eat Disord. 2005;37 Suppl:S2-S21. doi:10.1002/eat.20107
- Carvalhais A, Araújo J, Natal Jorge R, Bø K. Urinary incontinence and disordered eating in female elite athletes. J Sci Med Sport. 2019;22(2):140-144. doi:10.1016/j.jsams.2018.07.008
- Castellini, G., Lelli, L., Ricca, V., & Maggi, M. (2016). Sexuality in eating disorders patients: etiological factors, sexual dysfunction and identity issues. A systematic review. Hormone molecular biology and clinical investigation, 25(2), 71–90. https://doi.org/10.1515/hmbci-2015-0055
- Chiarioni, G., Bassotti, G., Monsignori, A., Menegotti, M., Salandini, L., Di Matteo, G., Vantini, I., & Whitehead, W. E. (2000). Anorectal dysfunction in constipated women with anorexia nervosa. Mayo Clinic Proceedings, 75(10), 1015–1019. https://doi.org/10.4065/75.10.1015
- Cortes, E., Singh, K., & Reid, W. M. (2003). Anorexia nervosa and pelvic floor dysfunction. International urogynecology journal and pelvic floor dysfunction, 14(4), 254–255. https://doi.org/10.1007/s00192-003-1082-z
- Dobinson A, Cooper M, Quesnel D. Safe Exercise at Every Stage: A Guideline for Managing Exericse in Eating Disorder Treatment. https://www.safeexerciseateverystage.com/sees-guidelines
- Dreznik, Z., Vishne, T. H., Kristt, D., Alper, D., & Ramadan, E. (2001). Rectal prolapse: a possibly underrecognized complication of anorexia nervosa amenable to surgical correction. International journal of psychiatry in medicine, 31(3), 347–352. https://doi.org/10.2190/3987-2N5A-FJDG-M89F
- Dunkley CR, Gorzalka BB, Brotto LA. Associations Between Sexual Function and Disordered Eating Among Undergraduate Women: An Emphasis on Sexual Pain and Distress. J Sex Marital Ther. 2020;46(1):18-34. doi:10.1080/0092623X.2019.1626307
- Durnea, C. M., Khashan, A. S., Kenny, L. C., Tabirca, S. S., & O'Reilly, B. A. (2014). An insight into pelvic floor status in nulliparous women. International urogynecology journal, 25(3), 337–345. https://doi.org/10.1007/s00192-013-2225-5
- Emerich Gordon, K., & Reed, O. (2020). The Role of the Pelvic Floor in Respiration: A Multidisciplinary Literature Review. Journal of voice : official journal of the Voice Foundation, 34(2), 243–249. https://doi.org/10.1016/j.jvoice.2018.09.024
- Gaudiani, J. L. (2019). Sick enough: a guide to the medical complications of eating disorders. Routledge.
- Gibson, D., Watters, A., & Mehler, P. S. (2021). The intersect of gastrointestinal symptoms and malnutrition associated with anorexia nervosa and avoidant/restrictive food intake disorder: Functional or pathophysiologic?-A systematic review. The International journal of eating disorders, 54(6), 1019–1054. https://doi.org/10.1002/eat.23553
- Gibson, D., Workman, C., & Mehler, P. S. (2019). Medical Complications of Anorexia Nervosa and Bulimia Nervosa. The Psychiatric clinics of North America, 42(2), 263–274. https://doi.org/10.1016/j.psc.2019.01.009Gong, R., & Xia, Z. (2019). Collagen changes in pelvic support tissues in women with pelvic organ prolapse. European journal of obstetrics, gynecology, and reproductive biology, 234, 185–189. https://doi.org/10.1016/j.ejogrb.2019.01.012
- Guarda A. (2023, February). What are Eating Disorders? . American Psychiatric Association. https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders
- Harm-Ernandes, I., Boyle, V., Hartmann, D., Fitzgerald, C. M., Lowder, J. L., Kotarinos, R., & Whitcomb, E. (2021). Assessment of the Pelvic Floor and Associated Musculoskeletal System: Guide for Medical Practitioners. Female pelvic medicine & reconstructive surgery, 27(12), 711–718. https://doi.org/10.1097/SPV.0000000000001121
- Imgart H, Zanko A, Lorek S, Schlichterle PS, Zeiler M. Exploring the link between eating disorders and persistent genital arousal disorder/genito-pelvic dysesthesia: first description and a systematic review of the literature. J Eat Disord. 2022;10(1):159. Published 2022 Nov 10. doi:10.1186/s40337-022-00687-7
- Juszczak, K., & Thor, P. J. (2012). The integrative function of vagal nerves in urinary bladder activity in rats with and without intravesical noxious stimulation. Folia medica Cracoviensia, 52(1-2), 5–16.
- Karwautz, A. F., Wagner, G., Waldherr, K., Nader, I. W., Fernandez-Aranda, F., Estivill, X., Holliday, J., Collier, D. A., & Treasure, J. L. (2011). Gene-environment interaction in anorexia nervosa: relevance of non-shared environment and the serotonin transporter gene. Molecular psychiatry, 16(6), 590–592. https://doi.org/10.1038/mp.2010.125
- Keel, P. K., Eckel, L. A., Hildebrandt, B. A., Haedt-Matt, A. A., Murry, D. J., Appelbaum, J., & Jimerson, D. C. (2023). Disentangling the links between gastric emptying and binge eating v. purging in eating disorders using a case-control design. Psychological medicine, 53(5), 1947–1954. https://doi.org/10.1017/S0033291721003640
- Kim H, Jung HR, Kim JB, Kim DJ. Autonomic Dysfunction in Sleep Disorders: From Neurobiological Basis to Potential Therapeutic Approaches. J Clin Neurol. 2022;18(2):140-151. doi:10.3988/jcn.2022.18.2.140
- Laino, F. M., de Araújo, M. P., Sartori, M. G. F., de Aquino Castro, R., Santos, J. L. F., & Tamanini, J. T. N. (2023). Urinary incontinence in female athletes with inadequate eating behavior: a case-control study. International urogynecology journal, 34(2), 431–438. https://doi.org/10.1007/s00192-022-05349-5
- Leonardo, K., Seno, D. H., Mirza, H., & Afriansyah, A. (2022). Biofeedback-assisted pelvic floor muscle training and pelvic electrical stimulation in women with overactive bladder: A systematic review and meta-analysis of randomized controlled trials. Neurourology and urodynamics, 41(6), 1258–1269. https://doi.org/10.1002/nau.24984
- Marjoux, Sophie & Bennadji, Boubekeur & de Parades, Vincent & Mosnier, Henri & Atienza, Patrick & Barth, Xavier & François, Yves & Faucheron, Jean & Roman, Sabine & Mion, Francois & Damon, Henri. (2012). Mo1059 Rectal Prolapse and Anorexia Nervosa: About 24 Cases. Gastroenterology. 142. S-584. 10.1016/S0016-5085(12)62240-9.
- Mazi, B., Kaddour, O., & Al-Badr, A. (2019). Depression symptoms in women with pelvic floor dysfunction: a case-control study. International journal of women's health, 11, 143–148. https://doi.org/10.2147/IJWH.S187417
- Micali N, Martini MG, Thomas JJ, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med. 2017;15(1):12. Published 2017 Jan 17. doi:10.1186/s12916-016-0766-4
- Micali N, Treasure J, Simonoff E. Eating disorders symptoms in pregnancy: a longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res. 2007;63(3):297-303. doi:10.1016/j.jpsychores.2007.05.003
- Mitchell, N., & Norris, M. L. (2013). Rectal prolapse associated with anorexia nervosa: a case report and review of the literature. Journal of eating disorders, 1, 39. https://doi.org/10.1186/2050-2974-1-39
- Ng QX, Lim YL, Loke W, Chee KT, Lim DY. Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective. Int J Environ Res Public Health. 2022;19(8):4874. Published 2022 Apr 17. doi:10.3390/ijerph19084874
- Nitsch, A., Watters, A., Manwaring, J., Bauschka, M., Hebert, M., & Mehler, P. S. (2023). Clinical features of adult patients with avoidant/restrictive food intake disorder presenting for medical stabilization: A descriptive study. The International journal of eating disorders, 56(5), 978–990. https://doi.org/10.1002/eat.23897
- Onur, Ö. Ş., & Teksin, G. (2023). Clinical Features of Women with Genito-Pelvic Pain, Penetration Disorder and Disordered Eating Attitudes: A Cross Sectional Study. Noro psikiyatri arsivi, 60(4), 327–334. https://doi.org/10.29399/npa.28313
- Panariello F, Borgiani G, Bronte C, et al. Eating Disorders and Disturbed Eating Behaviors Underlying Body Weight Differences in Patients Affected by Endometriosis: Preliminary Results from an Italian Cross-Sectional Study. Int J Environ Res Public Health. 2023;20(3):1727. Published 2023 Jan 18. doi:10.3390/ijerph20031727
- Paslakis G, de Zwaan M. Clinical management of females seeking fertility treatment and of pregnant females with eating disorders. Eur Eat Disord Rev. 2019;27(3):215-223. doi:10.1002/erv.2667
- Peinado-Molina, R. A., Hernández-Martínez, A., Martínez-Vázquez, S., Rodríguez-Almagro, J., & Martínez-Galiano, J. M. (2023). Pelvic floor dysfunction: prevalence and associated factors. BMC public health, 23(1), 2005. https://doi.org/10.1186/s12889-023-16901-3
- Prescott SL, Liberles SD. Internal senses of the vagus nerve. Neuron. 2022;110(4):579-599. doi:10.1016/j.neuron.2021.12.020
- Porges SW. The polyvagal theory: new insights into adaptive reactions of the autonomic nervous system. Cleve Clin J Med. 2009;76 Suppl 2(Suppl 2):S86-S90. doi:10.3949/ccjm.76.s2.17
- Schmidt U, Sharpe H, Bartholdy S, et al. Treatment of anorexia nervosa: a multimethod investigation translating experimental neuroscience into clinical practice. Southampton (UK): NIHR Journals Library; August 2017.
- Silvernale, Casey & Kuo, Braden & Staller, Kyle. (2020). Sa1678 PELVIC FLOOR PROLAPSE ASSOCIATED WITH GI-SPECIFIC HEALTHCARE UTILIZATION AND ANOREXIA NERVOSA IN AN EATING DISORDER PATIENT COHORT. Gastroenterology. 158. S-379. 10.1016/S0016-5085(20)31642-5.
- Tobias A, Sadiq NM. Physiology, Gastrointestinal Nervous Control. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 26, 2022.
- Vrijens, D., Berghmans, B., Nieman, F., van Os, J., van Koeveringe, G., & Leue, C. (2017). Prevalence of anxiety and depressive symptoms and their association with pelvic floor dysfunctions-A cross sectional cohort study at a Pelvic Care Centre. Neurourology and urodynamics, 36(7), 1816–1823. https://doi.org/10.1002/nau.23186
- Weigel, A., Löwe, B., & Kohlmann, S. (2019). Severity of somatic symptoms in outpatients with anorexia and bulimia nervosa. European eating disorders review : the journal of the Eating Disorders Association, 27(2), 195–204. https://doi.org/10.1002/erv.2643
- Williams, M., Blalock, D., Foster, M., Mehler, P. S., & Gibson, D. (2024). Pelvic Floor Dysfunction in People with Eating Disorders and the Acute Effect of Different Interventions – A Retrospective Cohort Study. Clinical and Experimental Obstetrics & Gynecology, 51(5), 116. https://doi.org/10.31083/j.ceog5105116
- Worman, R. S., Stafford, R. E., Cowley, D., Prudencio, C. B., & Hodges, P. W. (2023). Evidence for increased tone or overactivity of pelvic floor muscles in pelvic health conditions: a systematic review. American journal of obstetrics and gynecology, 228(6), 657–674.e91. https://doi.org/10.1016/j.ajog.2022.10.027.
- Wojcik, M. H., Meenaghan, E., Lawson, E. A., Misra, M., Klibanski, A., & Miller, K. K. (2010). Reduced amylin levels are associated with low bone mineral density in women with anorexia nervosa. Bone, 46(3), 796–800. https://doi.org/10.1016/j.bone.2009.11.014
- Zachovajeviene, B., Siupsinskas, L., Zachovajevas, P., Venclovas, Z., & Milonas, D. (2019). Effect of diaphragm and abdominal muscle training on pelvic floor strength and endurance: results of a prospective randomized trial. Scientific reports, 9(1), 19192. https://doi.org/10.1038/s41598-019-55724-4
AUTHOR BIO:
Carole High Gross, PT, MS, DPT, PRPC

Carole High Gross, PT, MS, DPT, PRPC (she/her) earned her Doctorate of Physical Therapy from Arcadia University in 2015, and her Masters of Science in Physical Therapy in 1992 from Thomas Jefferson University. Carole earned her Pelvic Rehabilitation Practitioner Certification and enjoys working as a Pelvic Clinical Rehabilitation Specialist for Lehigh Valley Health Network. Carole serves as a Lead Teaching Assistant for the Herman and Wallace Pelvic Rehabilitation Institute for pelvic floor education courses. She is also an instructor with the Herman and Wallace Institute for Eating Disorders and Pelvic Health Rehabilitation: The Role of a Rehab Professional. Carole serves on the Pelvic Workgroup of the Ehlers-Danlos International Consortium. Carole has a special interest in working with individuals living with eating disorders, and hypermobility throughout the pregnancy and postpartum journey. In addition, Carole enjoys working with all genders with pelvic, bowel, bladder, and abdominal issues. Carole is passionate about lifelong learning. She resides in Bucks County, Pennsylvania, and enjoys spending time with her family and pups.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./





































