
By taking a step BACK we can take a step FORWARD to assist individuals with eating disorders. Use your toolbox to build theirs.
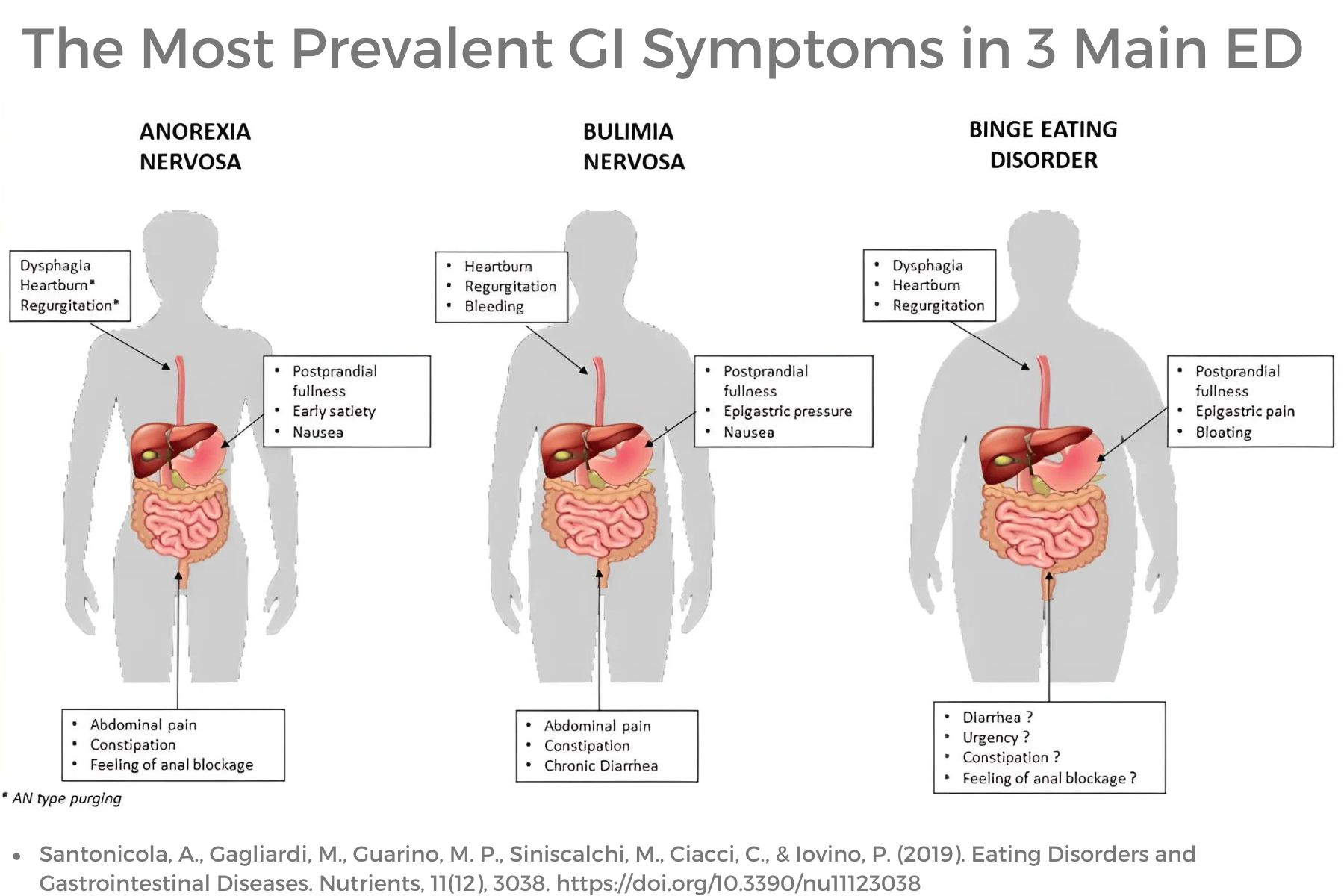
Eating disorders are mental health conditions characterized by severe and persistent disturbance in eating behaviors with associated distressing thoughts and emotions that affect an individual’s physical, psychological, and social function. Eating disorders are serious mental illnesses with physical manifestations and serious and sometimes life-threatening medical complications. Common eating disorders are Anorexia Nervosa (AN), Bulimia Nervosa (BN), Binge Eating Disorder (BED), Otherwise Specified Feeding and Eating Disorders (OSFED), and Avoidant Restrictive Food Intake Disorder (ARFID). Pica and Rumination Disorder are also included in the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM TR).
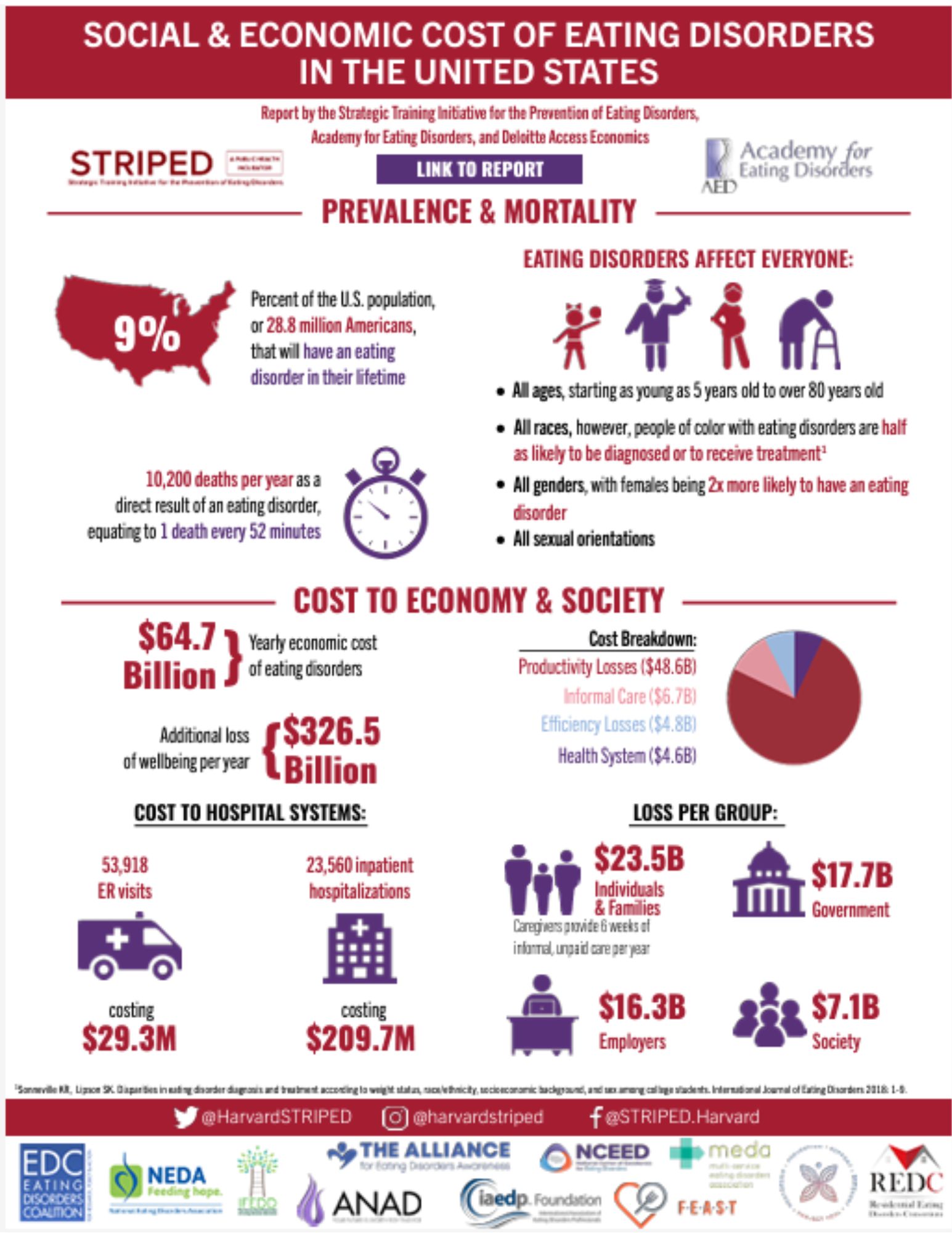
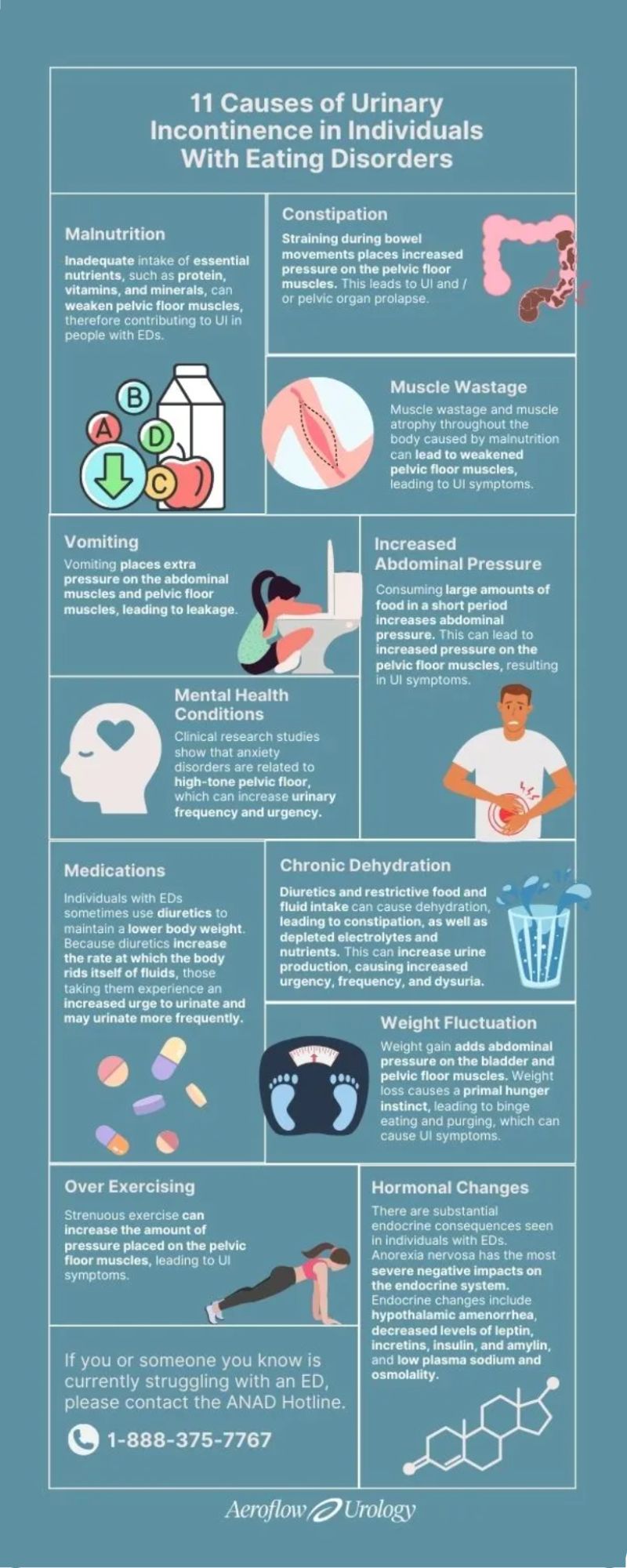
Bowel, bladder, and pelvic dysfunction are common with individuals with eating disorders. Fertility and negative effects on both baby and birthing parent are also common. Research is scant regarding pelvic rehabilitation interventions for this important group of individuals. More research is emerging, showing pelvic and gastrointestinal dysfunction with this population; however, pelvic-based rehabilitation has not been readily explored as an option for these individuals until last year.

HW faculty member Carole High Gross, PT, MS, DPT, PRPC instructs her remote course, Eating Disorders and Pelvic Health Rehabilitation, on October 19-20, 2024 that takes a deep dive into the role of pelvic health rehabilitation with individuals with eating disorders.
The role of a pelvic health rehabilitation professional includes caring for individuals with dysfunction within the pelvis and abdominal canister. We treat individuals with constipation, fecal incontinence, pelvic organ prolapse, urinary dysfunction, pelvic pain, abdominal pain, and bloating (to name a few). Individuals with eating disorders often experience ALL of these symptoms. Numerous studies demonstrate bowel, bladder, and pelvic dysfunction in those with eating disorders (see reference list for some of these studies). We CAN help!
Eating disorders are mental health conditions with serious biopsychosocial implications that negatively impact the function of the body, social interactions, and psychological well-being. The American Psychiatric Association characterizes Eating Disorders (ED) as “behavioral conditions characterized by severe and persistent disturbance in eating behaviors and associated distressing thoughts and emotions.” Types of eating disorders include:
Eating Disorders Awareness Week (EDAW), is February 26-March 3, 2024! It is an annual campaign to promote education about eating disorders. This week is also intended to provide hope and support for individuals and families affected by eating disorders. Awareness is key for both the public and the healthcare community.
We, as pelvic health providers, have the privilege to work with people of all genders with complex and often complicated medical histories. What are we really missing? What do we read (or not read) between the lines? What are cries for help that we are not hearing or noticing? As pelvic providers, we just need to keep our eyes, ears, and hearts open to our patients. The art of listening, observing and respectfully inquiring may be our greatest superpower. Imagine we are doing a puzzle without the puzzle box. Often it will take us time to gather the pieces and start to see the fuller picture. As health care providers, we carefully look at the whole puzzle - not just one piece… and sometimes this does take time.
Let’s take a look at a typical day in our busy clinical lives. Maybe you can relate. On our first visit with our patient, we are working hard (and sometimes fast) to try to get a thorough history, have appropriate functional outcome measures completed, ensure that all of the necessary “paperwork” is completed for our office or health care system, do our objective examination, pelvic muscle assessment, establish a prognosis, goals, a plan of care, etc. Does this sound familiar? How much can we fit into the time we are allotted at our workplace to get a picture of our patient? During this first visit do we get all of our answers? Or do we instead have a lot more questions?

Carole High Gross, PT, MS, DPT, PRPC earned her Doctorate of Physical Therapy from Arcadia University in 2015, her Master of Science in Physical Therapy in 1992 from Thomas Jefferson University, and her Pelvic Rehabilitation Practitioner Certification in 2021. Carole works with Herman & Wallace as a Lead Teaching Assistant as well as an instructor for her own course Eating Disorders and Pelvic Health Rehabilitation. Carole serves on the Pelvic Workgroup of the Ehlers-Danlos International Consortium and has a special interest in working with individuals living with eating disorders, and hypermobility throughout the pregnancy and postpartum journey. In addition, Carole enjoys working with all genders with pelvic, bowel, bladder, and abdominal issues. You can join Carole in her next scheduled Eating Disorders and Pelvic Rehabilitation on October 28-29 2023.
The effects of weight stigma on individuals with and without clinical eating disorders are profound and detrimental. Weight stigma refers to the negative assumptions, attitudes, and beliefs that are directed towards a person based on their body weight, shape, or size. People with higher weight often experience stigma from health professionals, educators, peers, employers, the media, family, and friends.
Weight stigmatization may unintentionally occur with people who are seeking rehabilitation or medical services due to health professionals' implicit and explicit bias towards people with higher body weights. This negatively impacts the quality of healthcare and exacerbates the challenges of recovery for those struggling with eating disorders. In addition, the result of weight bias from health care providers impacts and reinforces increased internalization, negative body image, poor self-esteem, self-criticism, increased unhealthy eating behaviors, poorer health outcomes, and disruption of mental wellness. Fear of judgment or discrimination from a health care provider based on weight biases can lead to delayed or avoidance of health care, increased behaviors or symptoms, and increased risks of medical complications from eating disorders.

Join me on April 22 to begin this quest to learn more about signs, symptoms, and the journey that individuals with eating disorders endure. We will also explore ways that we as Pelvic Health Professionals can assist them on this journey in Eating Disorders and Pelvic Health Rehabilitation. This course will not have all the answers; rather will be a step forward for clinicians to expand their understanding and to seek out additional resources to learn more and provide evidence-based treatment for these individuals.
We, as pelvic health practitioners are NOT going to treat eating disorders… we are NOT going to diagnose eating disorders… but we CAN and SHOULD be asking questions… encouraging patients to seek additional support… and helping them find appropriately trained providers. We can ALSO provide support and speak with words that promote validation, wellness, and healing rather than words that are unintentionally triggering, harmful or nonvalidating. IN ADDITION, we can provide these individuals with manual skills, activities, and educational “tools'' to assist in GI distress, constipation, abdominal bloating, urinary dysfunction, pelvic pain, sexual dysfunction, POP issues, postural / body mechanics, abdominal canister coordination/function, tightness in trunk, hips, shoulders, rib cage, etc. These individuals would benefit from pelvic health professionals being an additional part (not the lead) of their treatment team.





































