Simple Screening Questionnaire for Pelvic Floor Dysfunction
Earlier diagnosis is clearly a huge need for patients with pelvic floor dysfunction. Many patients suffer with their symptoms for years before even hearing the words “pelvic floor,” or realizing that a pelvic floor physical therapist may be able to help. For interstitial cystitis, one large survey article found fewer than 10% of patients with the condition had been correctly diagnosed with IC, even after years of symptoms and visits with multiple doctors.
Even after being diagnosed, patients still don’t learn about how the pelvic floor can be causing or exacerbating their symptoms. In one study of our interstitial cystitis patients, 46% learned about the importance of the pelvic floor on their own and sought out treatment independently, while nearly half felt they were referred by their physician to physical therapy far too late, as a ‘last resort.’ This is despite the fact that many of these patients had seen five or more physicians and physical therapy is considered the most proven treatment for IC by the American Urological Association.
Physicians, orthopedic physical therapists, other practitioners, and patients themselves need a simple, proven way to identify pelvic floor dysfunction to help patients find pelvic floor physical therapy earlier in their medical journey.
In a large survey of our patients with confirmed pelvic floor dysfunction, we examined what symptoms and medical history was most closely correlated with pelvic floor dysfunction. Any screening questionnaire would ideally be able to identify a wide variety of pelvic floor dysfunction, including patients with chronic pelvic pain, pelvic organ prolapse, orthopedic pain with a pelvic floor component (low back, hip, groin), urinary urgency/frequency, and/or bowel dysfunction.
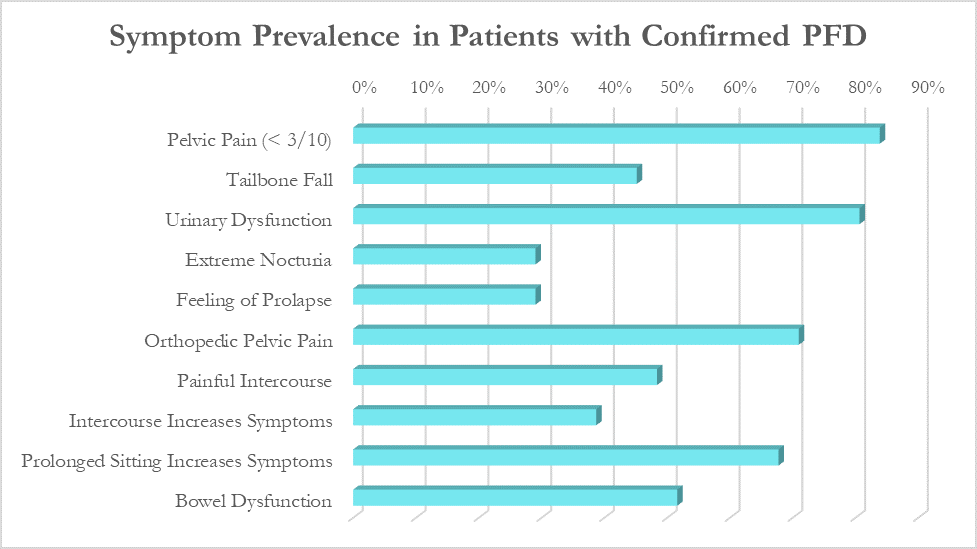
While these patients all had different medical diagnoses, many symptoms were common across the patient population. The most common were pelvic pain (84%), urinary urgency, frequency, or incontinence (81%), orthopedic pelvic pain (71%) and symptoms that worsen with prolonged sitting (68%).
Based on the survey results, we created the Cozean Pelvic Dysfunction Screening Protocol to screen for pelvic floor dysfunction and published the results in the International Pelvic Pain Society (2017). The goal was to correctly identify more than 80% of the patients with pelvic floor dysfunction (sensitivity). For ease of use by both practitioners and patients, the questions were phrased so they could be answered with a simple ‘yes/no’ (as a check box). If patients answers ‘yes’ to 3 or more of the questions, pelvic floor dysfunction is highly likely.
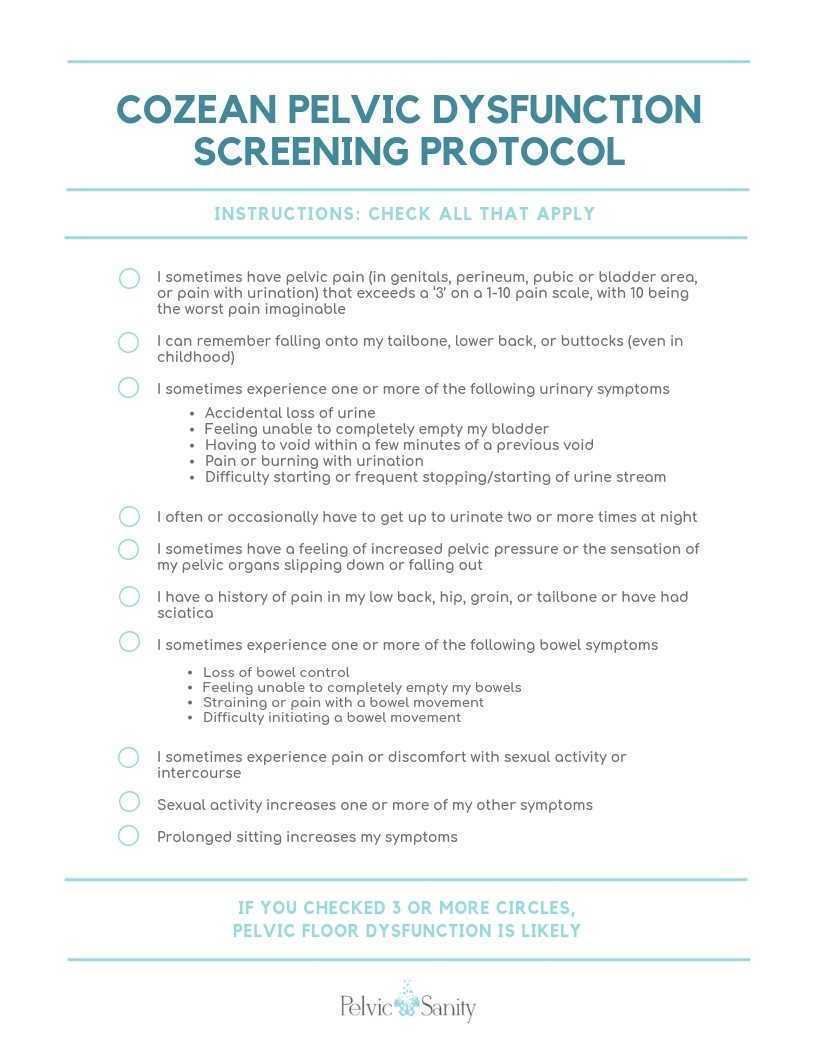 Document available for download at https://docs.wixstatic.com/ugd/d1026c_42a0fda8e5644930950d754619586614.pdf
Document available for download at https://docs.wixstatic.com/ugd/d1026c_42a0fda8e5644930950d754619586614.pdf
Testing the Model
In a model like this, we would expect a normal (bell-shaped) distribution curve of answers from patients with pelvic floor dysfunction. Some patients will score on the high end, others on the low, and the majority would be clustered in the middle. This is what we observe with use of the questionnaire, as seen by the trendline in the blow graph. Most patients with confirmed pelvic floor dysfunction cluster in scores between 3 and 7, with a few scoring at 8 or higher. Less than one out of ten patients with pelvic floor dysfunction score below a 2 on the questionnaire and would not be captured by this measure.
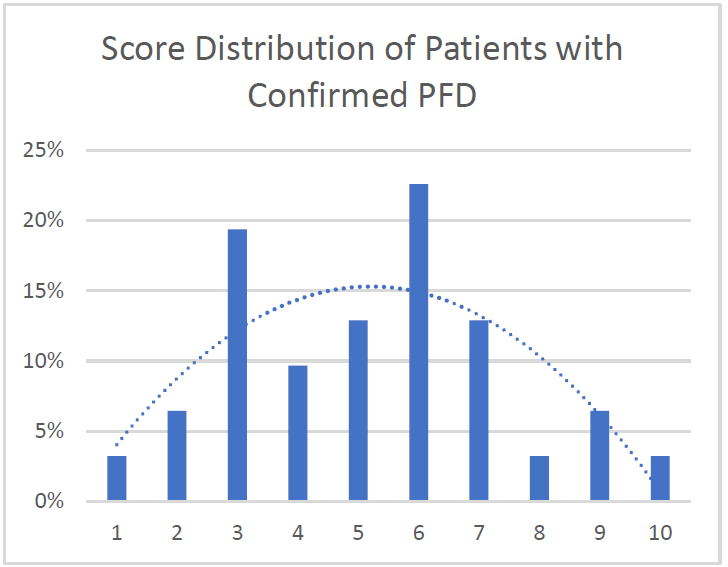
Specificity: 91%. More than 90% of patients with confirmed pelvic floor dysfunction were correctly identified by this screening protocol. Additional testing is required on a general population without PFD to determine the specificity of the questionnaire.
Average: 5.2. Of patients with confirmed PFD, the average score according to this screening protocol was 5.2 with a median score of 5 and a mode of 6. This is in line with what would be expected with a normal distribution curve.
We hope this 10-question survey is able to help patients with pelvic floor dysfunction be diagnosed earlier - whether by their physician, other physical therapists, or themselves – and seek pelvic floor physical therapy earlier in their medical journey. Please feel free to use the printable version of this protocol with your patients or in working with local practitioners.
Nicole Cozean will be teaching the course Interstitial Cystitis: Holistic Evaluation and Treatment in Princeton, NJ from April 6-7, 2019.
 Nicole Cozean is the founder of PelvicSanity physical therapy, in Orange County, California. Nicole was named the 2017 PT of the Year, is the first physical therapist to serve on the ICA Board of Directors, and is the award-winning and best-selling book The Interstitial Cystitis Solution (2016). She is an adjunct professor at her alma mater, Chapman University and teaches continuing education courses through the prestigious Herman & Wallace Institute.
Nicole Cozean is the founder of PelvicSanity physical therapy, in Orange County, California. Nicole was named the 2017 PT of the Year, is the first physical therapist to serve on the ICA Board of Directors, and is the award-winning and best-selling book The Interstitial Cystitis Solution (2016). She is an adjunct professor at her alma mater, Chapman University and teaches continuing education courses through the prestigious Herman & Wallace Institute.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./








































