Milk Duct Blockage
Milk duct blockage is a common condition in breast feeding mother’s that can cause a multitude of problems including painful breasts, mastitis, breast abscess, decreased milk supply, breast feeding cessation, and poor confidence with decreased quality of life. A recent study in 2015 in The Journal of Women’s Health Physical Therapy1, showed that physical therapy (PT) maybe a helpful treatment for the lactating mother experiencing milk duct blockage when conservative measures have failed. Common conservative measures typically recommended are self-massage, heat, and regular feedings. The World Health Association, the American Academy of Pediatrics, and Academy of Breast Feeding Medicine, all recommend breast feeding as the primary source for nutrition for infants. There are many benefits to both the mother, and the infant, when breast feeding is used as the primary source for nutrition in infants. Having blocked milk ducts make it difficult and painful to breast feed and can lead to poor confidence for the mother and a frustrated baby as the milk supply could be reduced or inadequate. The primary health concern for blocked milk ducts is mastitis. Mastitis is defined as an infection of breast tissue leading to pain, redness, swelling, and warmth, possibly fever and chills and can lead to early cessation of breast feeding.
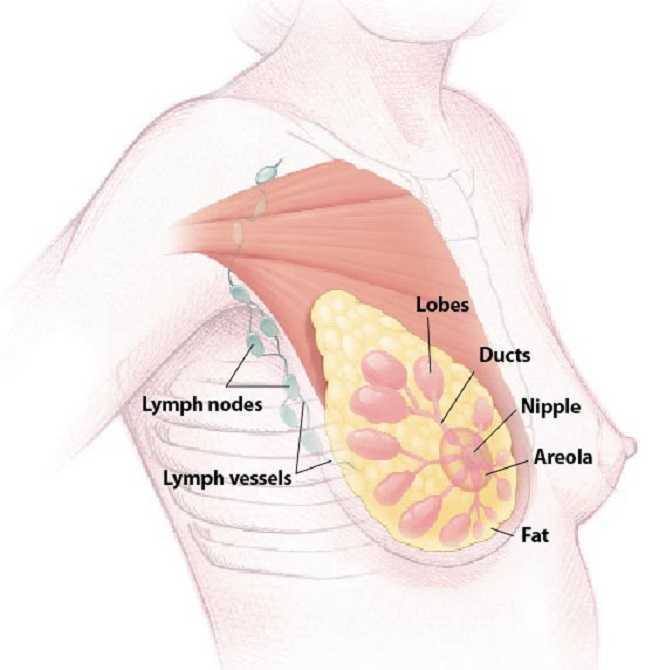 A blocked milk duct is not a typical referral to PT, however, this study outlined a protocol used for 30 patients with one or more blocked milk ducts that were referred to PT by a qualified lactation consultant. This study was a prospective pre/posttest cohort study. As an outcome measure, this study utilized a Visual Analog Scale (VAS) for 3 descriptive areas: pain, difficulty breast feeding, and confidence in independently nursing before and after treatment. The treatment protocol included moist heat, thermal ultrasound, specific manual therapy techniques, and patient education for treatment and prevention of the blockage(s). The thermal ultrasound and moist heating provided the recommend amount of heat to relax tissue around the blockage. Ultrasound also provided a mechanical effect that assists in the breaking up of the clog and increased pain threshold for the patient to improve tolerance to the manual clearing techniques. Next, the specific manual therapy was provided to directly unclog the blockage(s), and lastly the education provided was to help the patient identify and clear future blockages to prevent recurrence. 22 of the 30 patients were seen for 1-2 visits, 6 were seen for 3-4 visits, and none of the mother’s condition progressed to infective mastitis or developed breast abscess’s.
A blocked milk duct is not a typical referral to PT, however, this study outlined a protocol used for 30 patients with one or more blocked milk ducts that were referred to PT by a qualified lactation consultant. This study was a prospective pre/posttest cohort study. As an outcome measure, this study utilized a Visual Analog Scale (VAS) for 3 descriptive areas: pain, difficulty breast feeding, and confidence in independently nursing before and after treatment. The treatment protocol included moist heat, thermal ultrasound, specific manual therapy techniques, and patient education for treatment and prevention of the blockage(s). The thermal ultrasound and moist heating provided the recommend amount of heat to relax tissue around the blockage. Ultrasound also provided a mechanical effect that assists in the breaking up of the clog and increased pain threshold for the patient to improve tolerance to the manual clearing techniques. Next, the specific manual therapy was provided to directly unclog the blockage(s), and lastly the education provided was to help the patient identify and clear future blockages to prevent recurrence. 22 of the 30 patients were seen for 1-2 visits, 6 were seen for 3-4 visits, and none of the mother’s condition progressed to infective mastitis or developed breast abscess’s.
The results of the study showed the protocol used was helpful to ease pain, reduce difficulty with breast feeding, and improve confidence with independent breast feeding for lactating women that participated in the study. Although treatment of blocked milk ducts in lactating mothers is not a common PT referral, this study shows that PT may be one more helpful treatment for a patient experiencing this problem that is not responding to traditional conservative treatment. Since breast feeding is important to both mother and infant and is the primary recommended source for infant nutrition, it is important that a lactating mother receives quick, effective treatment for blocked milk ducts to prevent onset of mastitis and breast abscess that lead to early cessation of breast feeding. The cited study recommends that women who suspect a blocked milk duct or are having problems with breast feeding always seek care from a certified lactation consultant first, and that PT may be a referral that is made.
Cooper, B. B., & Kowalsky, D. S. (2015). Physical Therapy Intervention for Treatment of Blocked Milk Ducts in Lactating Women. Journal of Women’s Health Physical Therapy, 39(3), 115-126.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./



































