For decades, the G-spot has captivated attention, sparking debates in science and popular culture. Is it a distinct anatomical structure, a myth, or simply the same region as the 'female prostate'? While opinions differ, the heart of the discussion may be less about anatomy and more about semantics. Let’s explore the evidence and why this debate persists.
The Anatomy of the G-Spot and Female Prostate
The term 'G-spot' was introduced by German gynecologist Ernst Gräfenberg in 1950, describing a sensitive area on the anterior vaginal wall linked to the urethra and its surrounding tissues (near the bladder neck). In 1981, sexologists Beverly Whipple and John D. Perry popularized the term in their book, emphasizing that this area could enhance pleasure for some women. Notably, the G-spot was never claimed to be a single 'magic button' but rather a zone of heightened sensitivity.
Modern research has shifted focus to the female prostate, also known as Skene’s glands, which are located near the urethra. These glands share histological and functional similarities with the male prostate, contributing to urinary health, sexual arousal, and orgasm.
Evolving Perspectives on the Debate
Early Skepticism: In 2001, Terrence Hines dismissed the G-spot as a 'modern gynecologic myth,' citing inconsistent evidence and suggesting its existence was more cultural than anatomical.
Reframing as the Female Prostate: A 2022 review proposed reclassifying Skene’s glands as the female prostate. It argued that sensations attributed to the G-spot may stem from the stimulation of these glands and surrounding tissues.
A Matter of Semantics?
Does the debate boil down to terminology? Gräfenberg’s description of the G-spot and modern studies on the female prostate appear to refer to the same periurethral region. Whether we call it the G-spot or the female prostate, the area has been scientifically linked to pleasure. The controversy seems less about function and more about naming conventions.
Orgasms are Diverse: The vaginal (G-spot) orgasm isn’t the only type of orgasm or pathway to pleasure. Research indicates that approximately 70–80% of women require direct clitoral stimulation to achieve orgasm, as the clitoris contains a high concentration of nerve endings, making it particularly sensitive
Statistics on Female Orgasm:
- 40.9% of women orgasm from both clitoral stimulation and vaginal penetration.
- 35.4% orgasm solely from clitoral stimulation.
- 20.1% orgasm solely from vaginal stimulation.
- 16% report pleasurable sensations from cervical stimulation.
- 3.6% are unable to achieve orgasm.
Final Thoughts
The evidence suggests that the G-spot, as a distinct entity, is less about anatomical uniqueness and more about the interplay of surrounding tissues, including the female prostate. What’s more important than terminology is recognizing and embracing the diversity of orgasmic experiences. Whether clitoral, vaginal, cervical, or a combination, all forms of pleasure are valid and backed by science. Moving forward, let’s focus less on labels and more on understanding and normalizing the spectrum of female sexual health and pleasure.
Join Tara Sullivan in her upcoming remote course, Sexual Medicine in Pelvic Rehab, on January 18-29, 2025 if you are interested in learning more about hymen myths, squirting, G-spot, prostate gland, sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post prostatectomy; as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus.
References:
The statistics provided on female orgasm are derived from various studies, primarily published in The Journal of Sexual Medicine. Below are the references for these statistics:
- "40.9% of women orgasm from both clitoral stimulation and vaginal penetration" and "35.4% orgasm solely from clitoral stimulation"
These figures are from a study published in The Journal of Sexual Medicine, which examined women's orgasmic experiences through self-reported surveys:- Herbenick, D., Reece, M., Sanders, S. A., Dodge, B., & Fortenberry, J. D. (2010). Women's Experiences with Vaginal Penetration and Its Association with Orgasm and Sexual Pleasure: Findings from a Nationally Representative Sample of Women in the United States. The Journal of Sexual Medicine, 7(Suppl 5), 324–333. DOI: 10.1111/j.1743-6109.2010.01814.x
- "20.1% orgasm solely from vaginal stimulation"
This statistic comes from the same study, which highlighted how a subset of women can achieve orgasm through vaginal stimulation alone but noted variability based on anatomy and personal preferences. - "16% report pleasurable sensations from cervical stimulation"
This finding comes from a 2023 study published in The Journal of Sexual Medicine, which focused on sensations related to cervical stimulation:- Schubach, L. A., et al. (2023). Cervical Sensitivity and Orgasm: Self-Reported Experiences from an Online Survey. The Journal of Sexual Medicine, 20(1), 49–59. DOI: 10.1093/jsm/jqac115
- "3.6% are unable to achieve orgasm"
This figure is derived from population-level studies on sexual dysfunction and orgasm prevalence:- Kingsberg, S. A., et al. (2019). Orgasmic Dysfunction in Women: Epidemiology and Treatment Outcomes.Obstetrics and Gynecology International Journal, 27(6), 10–17.
AUTHOR BIO:
Tara Sullivan, PT, DPT, PRPC, WCS, IF
 Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage, anatomy, and physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage, anatomy, and physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara established the pelvic health program at HonorHealth in Scottsdale and expanded the practice to 12 locations across the valley. She continues treating patients with her hands-on individualized approach, taking the time to listen and educate them, empowering them to return to a healthy and improved quality of life. Dr. Tara has developed and taught several pelvic health courses and lectures at local universities in Arizona including Northern Arizona University, Franklin Pierce University, and Midwestern University. In 2019, she joined the faculty team at Herman and Wallace teaching continuing education courses for rehab therapists and other health care providers interested in the pelvic health specialty, including a course she authored-Sexual Medicine in Pelvic Rehab, and co-author of Pain Science for the Chronic Pelvic Pain Population. Dr. Tara is very passionate about creating awareness of Pelvic Floor Dysfunction and launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
In March 2024, Dr. Tara left HonorHealth and founded her company Mind to Body Healing (M2B) to continue spreading awareness on pelvic health, mentor other healthcare providers, and incorporate sexual counseling into her pelvic floor physical therapy practice. She has partnered with Co-Owner, Dr. Kylee Austin, PT.
Tara Sullivan instructs her course Sexual Medicine in Pelvic Rehab on October 19-20. Her course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Menopause is a natural phase in a woman's life, signaling the end of her reproductive years. While many are familiar with common symptoms such as hot flashes, night sweats, brain fog, and mood changes, there is another less-discussed condition that affects many women: Genitourinary Syndrome of Menopause (GSM). GSM encompasses a range of symptoms affecting the genital and urinary systems, profoundly impacting a woman’s quality of life. Understanding GSM is crucial for women entering menopause and healthcare providers, especially pelvic floor specialists.
What is Genitourinary Syndrome of Menopause (GSM)?
Genitourinary Syndrome of Menopause (GSM) refers to a collection of signs and symptoms associated with the changes in estrogen levels that occur during menopause. These hormonal changes affect the tissues of the vulva, vagina, urethra, and bladder, leading to a variety of symptoms that can be both uncomfortable and disruptive.
GSM was formerly referred to as vulvovaginal atrophy, but this term was considered limited because it didn’t encompass the full scope of symptoms women experience, particularly those related to the urinary system. The term "GSM" is now preferred as it better reflects the diverse nature of the condition.
Common Symptoms of GSM
- Vaginal Dryness and Irritation: One of the most frequently reported symptoms of GSM is vaginal dryness. This occurs because estrogen levels drop, causing the vaginal tissue to become thinner, less elastic, and less lubricated. This dryness can lead to itching, burning, and irritation.
- Painful Intercourse (Dyspareunia): Vaginal dryness can make sexual activity uncomfortable or even painful. Women may also experience tearing or bleeding during intercourse due to the thinning of the tissue specifically around the vaginal opening.
- Urinary Symptoms: GSM can cause a range of urinary issues, including increased frequency of urination, urgency, urinary tract infections (UTIs), and incontinence. Estrogen plays a role in maintaining the health of the urinary tract, so its decline can lead to irritation and increased susceptibility to infections.
- Pelvic Floor Dysfunction: abnormal tone or weakening of pelvic floor muscles exacerbates urinary symptoms and pain, and contributes to conditions like pelvic organ prolapse.
- Changes in Vaginal pH: Estrogen plays a critical role in maintaining a healthy vaginal environment. With lower estrogen levels, the vaginal pH becomes less acidic, making the area more susceptible to infections such as bacterial vaginosis and yeast infections.
Causes and Risk Factors
GSM is directly related to the reduction in estrogen production during menopause. Estrogen is responsible for maintaining the thickness, elasticity, and moisture of the vaginal and urinary tissues. As levels drop, these tissues undergo changes that lead to GSM.
While GSM is most commonly associated with natural menopause, it can also occur in women who experience early menopause due to surgery or cancer treatments like chemotherapy and radiation. Women who smoke or have never given birth vaginally are also at a higher risk for developing GSM.
Treatment Options:
The good news is that GSM is treatable. While you might think, systemic hormone replacement therapy (HRT) is enough to resolve GSM, that’s not typically the case. More often, even if one is on already on estrogen HRT, or for those who cannot or will not take systemic estrogen, they can still apply a low dose estradiol cream specifically to the vestibule, urethra, and vaginal opening to target the tissue most affected by GSM. Local topical estradiol cream is considered a safe option. In a recent article, “In a large, claims-based analysis, we did not find an increased risk of breast cancer recurrence within 5 years in women with a personal history of breast cancer who were using vaginal estrogen for genitourinary syndrome of menopause”
However, if one is still opposed to using estradiol, other non-hormonal options are available to treat GSM symptoms:
- Vaginal Moisturizers and Lubricants: For women experiencing mild symptoms, over-the-counter vaginal moisturizers and lubricants can provide relief from dryness and discomfort. These products can be used regularly to help maintain vaginal moisture and make intercourse more comfortable.
- Pelvic Floor Physical Therapy: Many women with GSM benefit from pelvic floor physical therapy, which can strengthen the muscles of the pelvic floor, improve bladder control, and enhance sexual function. Physical therapists specialized in pelvic health can provide individualized treatments to address specific concerns.
- Laser Therapy: A newer, non-invasive option for GSM is laser therapy, such as fractional CO2 lasers. This therapy stimulates collagen production in the vaginal tissues, promoting healing and improving symptoms of dryness, pain, and laxity.
- Lifestyle Modifications: Quitting smoking, maintaining a healthy weight, and staying sexually active can also help reduce symptoms of GSM. Regular sexual activity increases blood flow to the vaginal area, helping to maintain tissue health.
Our Role as Pelvic Floor Therapist:
Despite affecting up to half of postmenopausal women, GSM remains underdiagnosed and undertreated. Many women may feel uncomfortable discussing these symptoms with their healthcare providers, or they may assume that these changes are a natural part of aging that must be endured. That is where pelvic floor specialists have a unique opportunity to educate these women. We have the luxury of one-on-one time and we are one of the only specialists that fully assess the vulvar tissue, specifically the vestibule and urethral opening where GSM is most identifiable. Understanding the research on estradiol treatment as well as other non-hormonal options can greatly improve our patients' quality of life.
Join Tara Sullivan in her upcoming course to learn more about Sexual Medicine in Pelvic Rehab on October 19-20. Lecture topics include hymen myths, squirting, G-spot, prostate gland, sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post-prostatectomy; as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus.
Resource:
- Agrawal P, Singh SM, Able C, Dumas K, Kohn J, Kohn TP, Clifton M. Safety of Vaginal Estrogen Therapy for Genitourinary Syndrome of Menopause in Women With a History of Breast Cancer. Obstet Gynecol. 2023 Sep 1;142(3):660-668. doi: 10.1097/AOG.0000000000005294. Epub 2023 Aug 3. PMID: 37535961. https://pubmed.ncbi.nlm.nih.gov/37535961/
AUTHOR BIO:
Tara Sullivan, PT, DPT, PRPC, WCS, IF
 Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage, anatomy, and physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage, anatomy, and physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara established the pelvic health program at HonorHealth in Scottsdale and expanded the practice to 12 locations across the valley. She continues treating patients with her hands-on individualized approach, taking the time to listen and educate them, empowering them to return to a healthy and improved quality of life. Dr. Tara has developed and taught several pelvic health courses and lectures at local universities in Arizona including Northern Arizona University, Franklin Pierce University, and Midwestern University. In 2019, she joined the faculty team at Herman and Wallace teaching continuing education courses for rehab therapists and other health care providers interested in the pelvic health specialty, including a course she authored-Sexual Medicine in Pelvic Rehab, and co-author of Pain Science for the Chronic Pelvic Pain Population. Dr. Tara is very passionate about creating awareness of Pelvic Floor Dysfunction and launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
In March 2024, Dr. Tara left HonorHealth and founded her company Mind to Body Healing (M2B) to continue spreading awareness on pelvic health, mentor other healthcare providers, and incorporate sexual counseling into her pelvic floor physical therapy practice. She has partnered with Co-Owner, Dr. Kylee Austin, PT.
Tara Sullivan, PT, DPT, PRPC, WCS, IF sat down with Holly Tanner and The Pelvic Rehab Report to discuss her course, Sexual Medicine in Pelvic Rehab. Tara started in the healthcare field as a massage therapist, practicing for over ten years including three years of teaching massage and anatomy, and physiology. Tara has specialized exclusively in Pelvic Floor Dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012.
Hi Tara, can you introduce yourself and tell us a little bit about your background?
Sure! So I’m Tara. I’ve been a pelvic health rehab therapist for about 10 years now. I started right out of PT school and I got a job at a local hospital where they were looking to grow and build the pelvic rehab program. So of course, I found Herman & Wallace and started taking all of the classes there that I could and just kept learning over the years. Now the program is expanded across the valley, we have nine different locations, and it’s been very successful and fulfilling. It’s my passion.
Recently, I would say the past four to five years of my career, I’ve started getting more into sexual dysfunctions. I was always into pelvic floor dysfunction in general - bowel, bladder, sexual dysfunction, and chronic pelvic pain, but I didn’t get specifically into the sexual medicine side of it until recently. I did the fellowship with ISSWSH that really pulled all of that information together with what I’ve learned through the years.
Can you explain what ISSWSH is and how that combined with the knowledge base that you already had?
I feel like ISSWSH for me, where I came full circle. I finally was like “I get it.” ISSWSH is the International Society for the Study of Women’s Sexual Health and it’s all the gurus like Dr. Goldstein, Rachel Rubin, and Susan Kellogg that have been around forever doing the research on sexual medicine. I started attending their conferences, became a faculty member, and presented at their annual fall meeting here in Scottsdale. Then I ended up doing their fellowship. Every year I would attend the conference, but it took a couple of years for all of that knowledge to soak in and for me to be able to really apply it. For example, that patient with that sticky discharge, maybe that is lichen planus – that’s the kind of medical side that you don’t necessarily learn in physical therapy school.
That for me just really helped my differential diagnosis which means that you can get the patient’s care faster. Get them to that resolution faster because you are working with a team of people and we all have our roles. As PTs and rehab practitioners, we have the time to sit with our patients. We are so blessed to have an hour, and the medical doctors don’t, for us to really take that time to figure out the patient’s history and what they’ve been through, and what could be the cause of it. We have the time to be the detective and help them get the care they need. Whether it’s with us, or in conjunction with something else. My goal is to never tell someone that I can’t help them because it’s not muscular.
How has this knowledge helped you in your collaboration with other practitioners in your practice?
I feel like this knowledge was the missing link for me. It brings it all together for the patient. So the patients come here and the urologist says “that’s not my area,” and then the gynecologist says “that’s not my area.” Then they come to you and you’re like “it’s kind of my area, but I can’t prescribe the medication that you need.”
My practice got so much better, just in the sense of the overall quality of care, when I was able to develop those relationships with the doctors. I could pick up the phone and say “Hey, that patient that you sent me – I think they have vestibulodynia, and I think it’s from their long-term use of oral contraceptive pills. I think that they might benefit from some local estrogen testosterone cream.” They would say, I don’t know about that, and I’d respond “let me send you some articles. Let me tell you what I’ve learned.”
Now I can just pick up the phone or send them a text asking them to prescribe so and so. It really helped bridge that gap. The doctors now will say “Ok. I know something’s going on, but I don’t know if it’s muscular or tissue. I don’t have that training, what do you think?” So it’s just been such a collaboration, it’s been so great. Then I’ll go the reverse of that and watch them do a surgery, watch them do a procedure.
For our patients, we need to take that time and work with the physicians and develop that relationship with them, because it’s easy to pass it off as “that’s not my job.” Especially the vestibule! The gynecologist goes right through it and looks into the vaginal canal and then the urologist is like I’m going to look at the urethra but I’m not looking around it, let me just stick that scope in. This knowledge and ability to use differential diagnosis, for me just brings it all together.
Does your course have an online, pre-recorded portion as well as a live component?
Yes. There are about nine lab videos on manual techniques because everyone wants to know what to do. For me, it’s more about what you know. What can you identify and differentiate with the differential diagnosis. Then we have about two hours of just the basic lectures on general pain and overactivity of the pelvic floor so that we can spend our time in the live lecture getting into the very specific conditions that we as PTs are, not necessarily diagnosing, but recognizing and sending for further care. That’s really where I wanted this class to fill the gap between the urologist, the gynecologist, and the PT.
Is your course primarily vulvo-vaginal conditions or are there some penile, scrotal, or other conditions?
It is both male and female dysfunctions, and I have a few transgender cases. I don’t personally treat the transgender population very often so I only have a couple of examples of that. I have a lot of examples where I’m trying to get practitioners to recognize the problem by what the patient is saying and their history, and how to funnel this into their differential diagnosis. Case studies include different types of vestibulodynia and causes, all the different skin conditions…and it’s not necessarily something that they didn’t learn in one of the Pelvic Floor Series courses, but I wanted one class where they could just talk about all the sexual dysfunctions and get into some of the ones that we don’t see as often but are present.
We also talk about PGAD (persistent genital arousal disorder), and with male dysfunctions, we talk about spontaneous ejaculation and urethral discharge, post finasteride syndrome. All of these things that you might not see every day, but when you see them you’ll recognize them so that you can help patients talk to the doctor and get the proper care. There are a lot of random, not as obvious, conditions that are not as prevalent. Then there are the common conditions that we see every single day like lichens.
What is the biggest takeaway that practitioners have who come into your class?
It is really being able to access and effectively use differential diagnosis. A lot of practitioners in the course are like “I always wondered what that was.” I have a ton of pictures that I share, and I’m like, I know have seen this before. I think a lot of it is the differential diagnosis. The feedback that I get from every class is “I feel like I can go to the clinic on Monday and apply what I learned.” “I’m going to go buy a q-tip and start doing a q-tip test because now I know what to do with that information.” They feel that confidence of really being able to apply it, talk to the patient, talk to the doctors, and figure out that meaningfulness.

Sexual Medicine in Pelvic Rehab
Course Dates:
January 14-15, 2023
May 13-14, 2023
September 23-24, 2023
Price: $450
Experience Level: Beginner
Contact Hours: 15
Description: This two-day course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, squirting, G-spot, prostate gland, sexual response cycles, hormone influence on sexual function; the anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function, and specific dysfunction treated by physical therapy in detail. Including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, and post-prostatectomy, as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD), and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Course Reviews:
- The instructor offered excellent examples of what can be seen in the patient population and advised good treatment plans to help. She was very thorough in answering questions and very well-informed on all topics presented in this class. I was so thankful to learn more about the hormone component of pelvic floor rehab, as I feel that this is greatly lacking in the Midwest -- we still live on the idea that hormones and HRT are BAD! Looks like I will be doing some heavy marketing soon with research articles! Thank you so much for all of this information!
- Various topics only glossed over in other courses were covered in detail to meet the various levels of knowledge of all students in the class. On top of this, new and useful material was also introduced and explained very well.
- Tara gave practical tips for us to start using in clinical practice and her notes to her lecture were KEY!

The following is an excerpt from the short interview between Holly Tanner and Tara Sullivan discussing her course Sexual Medicine in Pelvic Rehab. Watch the full video on the Herman & Wallace YouTube Channel.
Hi Tara, can you introduce yourself and tell us a little bit about your background?
Sure! So I’m Tara. I’ve been a pelvic health rehab therapist for about 10 years now. I started right out of PT school and I got a job at a local hospital where they were looking to grow and build the pelvic rehab program. So of course, I found Herman & Wallace and started taking all of the classes there that I could and just kept learning over the years. Now the program is expanded across the valley, we have nine different locations, and it’s been very successful and fulfilling. It’s my passion.
Recently, I would say the past four to five years of my career, I’ve started getting more into sexual dysfunctions. I was always into pelvic floor dysfunction in general - bowel, bladder, sexual dysfunction, and chronic pelvic pain, but I didn’t get specifically into the sexual medicine side of it until recently. I did the fellowship with ISSWSH that really pulled all of that information together with what I’ve learned through the years.
Can you explain what ISSWSH is and how that combined with the knowledge base that you already had?
I feel like ISSWSH for me, where I came full circle. I finally was like “I get it.” ISSWSH is the International Society for the Study of Women’s Sexual Health and it’s all the gurus like Dr. Goldstein, Rachel Rubin, and Susan Kellogg that have been around forever doing the research on sexual medicine. I started attending their conferences, became a faculty member, and presented at their annual fall meeting here in Scottsdale. Then I ended up doing their fellowship. Every year I would attend the conference, but it took a couple of years for all of that knowledge to soak in and for me to be able to really apply it. For example, that patient with that sticky discharge, maybe that is lichen planus – that’s the kind of medical side that you don’t necessarily learn in physical therapy school.
That for me just really helped my differential diagnosis which means that you can get the patient’s care faster. Get them to that resolution faster because you are working with a team of people and we all have our roles. As PTs and rehab practitioners, we have the time to sit with our patients. We are so blessed to have an hour, and the medical doctors don’t, for us to really take that time to figure out the patient’s history and what they’ve been through, and what could be the cause of it. We have the time to be the detective and help them get the care they need. Whether it’s with us, or in conjunction with something else. My goal is to never tell someone that I can’t help them because it’s not muscular.
How has this knowledge helped you in your collaboration with other practitioners in your practice?
I feel like this knowledge was the missing link for me. It brings it all together for the patient. So the patients come here and the urologist says “that’s not my area,” and then the gynecologist says “that’s not my area.” Then they come to you and you’re like “it’s kind of my area, but I can’t prescribe the medication that you need.”
My practice got so much better, just in the sense of the overall quality of care, when I was able to develop those relationships with the doctors. I could pick up the phone and say “Hey, that patient that you sent me – I think they have vestibulodynia, and I think it’s from their long-term use of oral contraceptive pills. I think that they might benefit from some local estrogen testosterone cream.” They would say, I don’t know about that, and I’d respond “let me send you some articles. Let me tell you what I’ve learned.”
Now I can just pick up the phone or send them a text asking them to prescribe so and so. It really helped bridge that gap. The doctors now will say “Ok. I know something’s going on, but I don’t know if it’s muscular or tissue. I don’t have that training, what do you think?” So it’s just been such a collaboration, it’s been so great. Then I’ll go the reverse of that and watch them do a surgery, watch them do a procedure.
For our patients, we need to take that time and work with the physicians and develop that relationship with them, because it’s easy to pass it off as “that’s not my job.” Especially the vestibule! The gynecologist goes right through it and looks into the vaginal canal and then the urologist is like I’m going to look at the urethra but I’m not looking around it, let me just stick that scope in. This knowledge and ability to use differential diagnosis, for me just brings it all together.
Does your course have an online, pre-recorded portion as well as a live component?
Yes. There are about nine lab videos on manual techniques because everyone wants to know what to do. For me, it’s more about what you know. What can you identify and differentiate with the differential diagnosis. Then we have about two hours of just the basic lectures on general pain and overactivity of the pelvic floor so that we can spend our time in the live lecture getting into the very specific conditions that we as PTs are, not necessarily diagnosing, but recognizing and sending for further care. That’s really where I wanted this class to fill the gap between the urologist, the gynecologist, and the PT.
Is your course primarily vulvo-vaginal conditions or are there some penile, scrotal, or other conditions?
It is both male and female dysfunctions, and I have a few transgender cases. I don’t personally treat the transgender population very often so I only have a couple of examples of that. I have a lot of examples where I’m trying to get practitioners to recognize the problem by what the patient is saying and their history, and how to funnel this into their differential diagnosis. Case studies include different types of vestibulodynia and causes, all the different skin conditions…and it’s not necessarily something that they didn’t learn in one of the Pelvic Floor Series courses, but I wanted one class where they could just talk about all the sexual dysfunctions and get into some of the ones that we don’t see as often but are present.
We also talk about PGAD (persistent genital arousal disorder), and with male dysfunctions, we talk about spontaneous ejaculation and urethral discharge, post vasectomy syndrome. All of these things that you might not see every day, but when you see them you’ll recognize them so that you can help patients talk to the doctor and get the proper care. There are a lot of random, not as obvious, conditions that are not as prevalent. Then there are the common conditions that we see every single day like lichens.
What is the biggest takeaway that practitioners have who come into your class?
It is really being able to access and effectively use differential diagnosis. A lot of practitioners in the course are like “I always wondered what that was.” I have a ton of pictures that I share, and I’m like, I know you guys have seen this before. I think a lot of it is the differential diagnosis. The feedback that I get from every class is “I feel like I can go to the clinic on Monday and apply what I learned.” “I’m going to go buy a q-tip and start doing a q-tip test because now I know what to do with that information.” They feel that confidence of really being able to apply it, talk to the patient, talk to the doctors, and figure out that meaningfulness.

2022 Course Dates:
July 16-17 2022 and October 15-16 2022
Sexual Medicine in Pelvic Rehab is designed for pelvic rehab specialists who want to expand their knowledge, experience, and treatment in sexual health and dysfunction. This course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions for all people and sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, as well as multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, female squirting, G-spot, prostate gland, female and male sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post-prostatectomy, as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Audience:
This continuing education course is appropriate for physical therapists, occupational therapists, physical therapist assistants, occupational therapist assistants, registered nurses, nurse midwives, and other rehabilitation professionals of all levels and experience. Content is not intended for use outside the scope of the learner's license or regulation. Physical therapy continuing education courses should not be taken by individuals who are not licensed or otherwise regulated, except, as they are involved in a specific plan of care.
Tara Sullivan, PT, DPT, PRPC, WCS, IF is on faculty with Herman & Wallace. She created Sexual Medicine in Pelvic Rehab and co-created Pain Science for the Chronic Pelvic Pain Population which she instructs alongside co-creator Alyson N Lowrey, PT, DPT, OCS. Tara started in the healthcare field as a massage therapist, practicing over ten years including three years of teaching massage and anatomy and physiology. Tara has specialized exclusively in Pelvic Floor Dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012. She is adjunct faculty speaking at the annual conference for the International Society for the Study of Women’s Sexual Health (ISSWSH) and teaches an elective course at Northern Arizona University (NAU) and Franklin Pierce University on Pelvic Health. Tara is very passionate about creating awareness on Pelvic Floor Dysfunction and recently launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
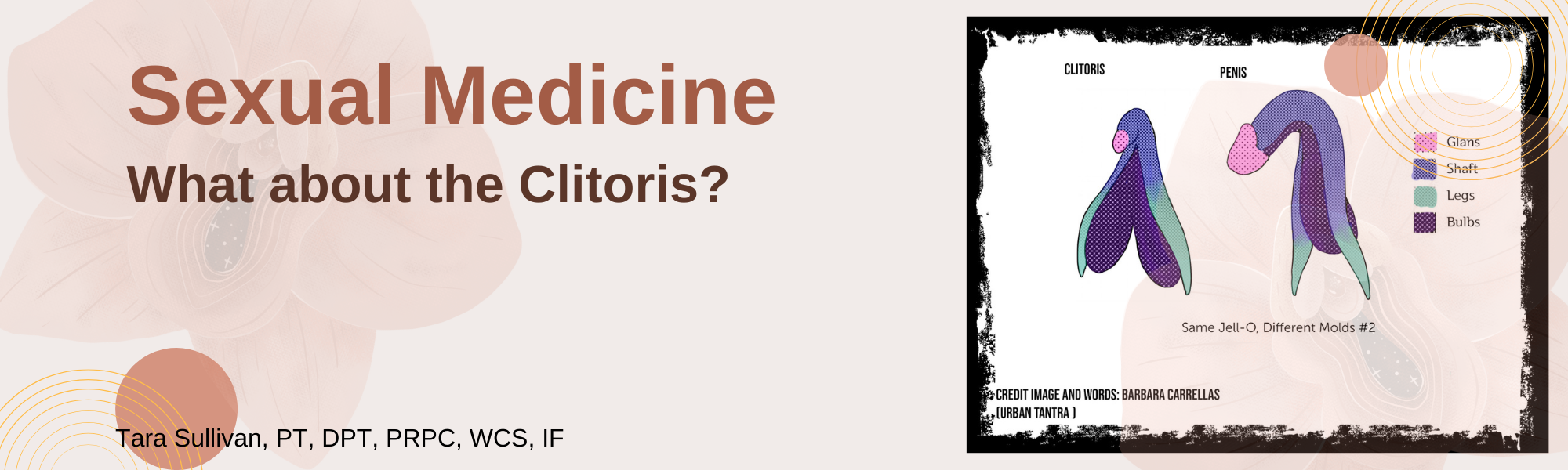
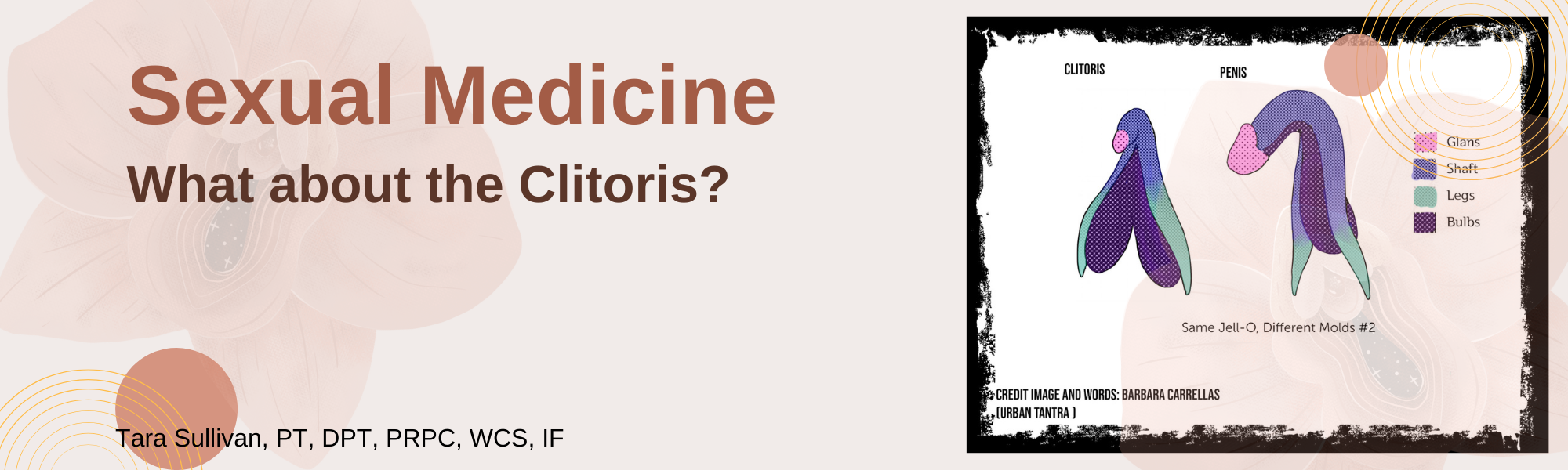
You may have heard of Jessica Pin. She’s been making headlines lately with the unconventional ways she is going about changing what medical texts and schools teach about the clitoris…..which is currently very little. According to Pin, who has a bachelor’s degree in biomedical engineering, the average textbook has over 50 pages more dedicated to the penis than compared to the clitoris. Jessica Pin started her journey to create awareness of clitoral anatomy because at 17 years old she had a labiaplasty leaving her with sensory loss. Jessica’s activism has so far changed 8 medical texts to include detailed anatomy of the clitoris in hopes knowledge of this anatomy is understood well, as it is critical prior to performing surgery near the clitoris.
Loss of clitoral function can also occur after labiaplasty, biopsies, cosmetic surgeries, and repair. As pelvic rehab providers, there is a level of responsibility we have to help shift the narrative. How often have we seen or heard similar stories of young patients undergoing cosmetic surgeries to try to ‘look normal’ or apologize for the way they look? We have such a unique position to spend time educating our patients and treating sexual dysfunctions across the spectrum.
The clitoris is analogous to the penis so what is the cause of this disparity? It could be that, traditionally, the focus has been on penetrative intercourse which largely overlooks that the clitoris is the primary sexual organ of the female sexual response and that 81.6% of women don’t orgasm from intercourse alone (without additional clitoral stimulation). Only 18.4% of women report that intercourse alone is sufficient to orgasm (Herbenick, et al. 2018).
The clitoris has historically been omitted from anatomical textbooks and then ‘rediscovered’ throughout medical history (O’connell, 1998). If you look at the 1948 Grey’s Anatomy textbook you will see that the clitoris was left out. Anatomical information centralized around the medical field has been historically male-dominated, affecting how the world discusses and understands anatomy and their bodies even in the current day. In 2005 Wade, Kremer and Brown ran a study on college students and found that 29% of women and 25% of men could not identify the clitoris on a diagram of the vulva. We need to revolutionize female sexuality in general, change the focus from the linear model where penetrative sex and orgasm are the focus as it’s been traditionally taught.
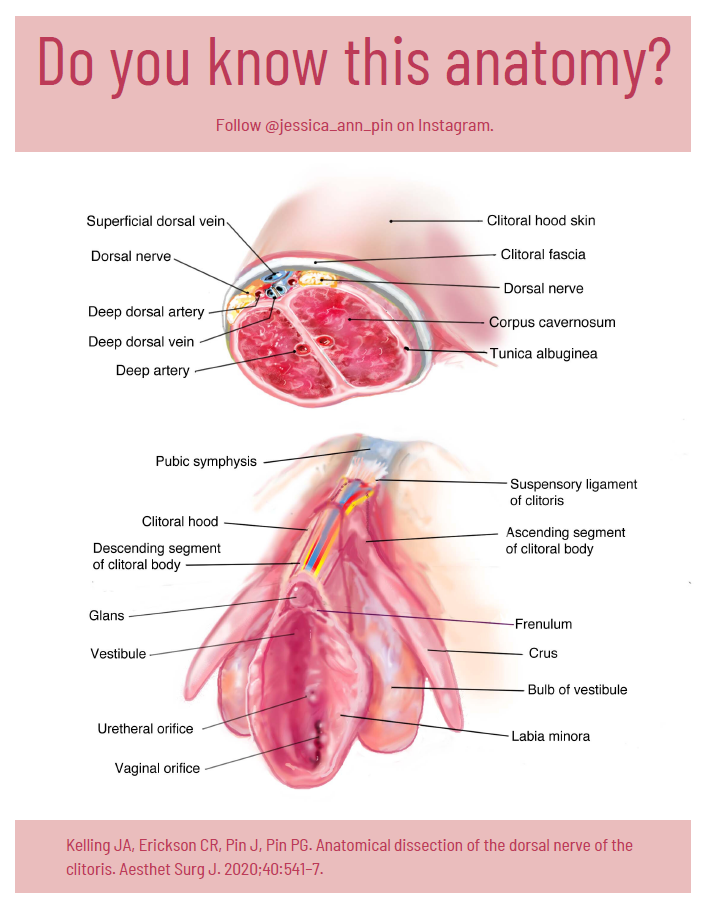
The full clitoris goes far beyond the crown which is the external tip. The clitoris actually extends several inches into the body where it branches into a shape similar to a wishbone. A description that I love is from Latham Thomas, “It’s all this amazing erectile tissue that wraps around, and it all engorges when it’s stimulated. Pound for pound, if you have a vulva, you actually have the same amount of erectile tissue that people with penises have, but it’s just internal.” These clitoral legs are responsible for the sensations where the front wall of the vagina connects to the paraurethral glands (the G-spot) and for female ejaculation.
I authored the Herman & Wallace Sexual Medicine in Pelvic Rehab course for practitioners to have a platform to learn proper anatomy, identify misconceptions, and understand that sexuality is circular with satisfaction as the focus. With the understanding of ‘normal’ anatomy and function, we can help our patients with sexual dysfunctions return to a healthy sexual lifestyle.
To sign the petition to get the nerves of the clitoris into the American College of OB/GYN curriculum go to:
Sexual Medicine in Pelvic Rehab is a two-day, remote continuing education course designed for pelvic rehab specialists who want to expand their knowledge, experience and treatment in sexual health and dysfunction. This course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions for the gender and sexual spectrum, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, female squirting, G-spot, prostate gland, female and male sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm. As well as the function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post-prostatectomy; as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Course dates in 2022 include:
Top Homogenous Image: Internal genitalia depicting homology (Carrellas, B. and Sprinkle, A., 2017).
Bottom Clitoral Anatomy Image: Jessica Pin, https://drive.google.com/file/d/1fS1HfBWYqXAEBu_jnAPuiulTE3nqIYYQ/view
O'Connell, H.E., Hutson, J.M., Anderson, C.R. and Plenter, R.J., 1998. Anatomical relationship between urethra and clitoris. The Journal of Urology, 159(6), pp.1892–1897.
Herbenick, D., Tsung, Chieh F., Arter, J. Women's Experiences With Genital Touching, Sexual Pleasure, and Orgasm: Results From a U.S. Probability Sample of Women Ages 18 to 94. https://www.tandfonline.com/doi/abs/10.1080/0092623X.2017.1346530
Wade, L.D., Kremer, E.C. and Brown, J., 2005. The incidental orgasm: The presence of clitoral knowledge and the absence of orgasm for women. Women & Health, 42(1), pp.117–138.