When we think of pelvic floor dysfunction, our minds often go straight to adults. We may even consider toddlers or children struggling with conditions like constipation or bedwetting. A population I frequently find missed is the infant! Many providers don’t realize that the pelvic floor issues that show up in infancy don’t have to be waited out.
As pediatric pelvic health providers, we have a unique and powerful role to play in helping babies who struggle with common challenges like reflux, colic, constipation, feeding difficulties, and even motor delays. At the root of many of these concerns lies the pelvic floor—an area often overlooked in traditional pediatric care. These parents will go to their providers, and they’ll be offered advice like “hold them upright for 20 minutes after feeding” or “try a lactation consultation,” but what happens if these interventions are not enough, OR what happens if a rehab provider wants to provide more support to a struggling family.
You may be thinking, “I don’t do pediatrics.” If that is your stance, I recommend you keep reading. You don’t have to be a dedicated pediatric therapist to provide families struggling with cranky or uncomfortable babies. Even if you don’t want to provide specific recommendations and treatment, you can still screen and offer referrals for support and even this step will create improvement in the quality of life of your families.
Understanding the Infant Pelvic Floor: More Than Just Diaper Changes
The abdominal canister in infants is still developing and is deeply interconnected with multiple systems in the body:
- The digestive system (contributing to reflux, gas, and constipation)
- The nervous system (especially for babies with difficulty calming or regulating)
- The musculoskeletal system (torticollis, body tension, abnormal movement patterns)
- The oral-motor system (especially in cases of tethered oral tissues or poor latch)
When these systems are under stress or not functioning in sync, the baby will likely be showing difficulty in performing regular functions, causing them to be uncomfortable. All babies express their discomfort differently, but this can lead to stressful symptoms such as crying, fussing, gassiness, constipation, reflux, and vomiting, leading to abnormal posturing and gross motor delays due to these adverse symptoms.
What Infant Pelvic Floor Dysfunction Looks Like
Pelvic floor issues in babies don’t always look like they do in adults. Instead, rehab providers may notice:
- Chronic straining to poop or lack of bowel movement coordination
- Irregular bowel habits, bloating, and gas
- Body tension that affects feeding or limits comfortable tummy time
- Shallow or inefficient breathing patterns
- Arching or clenching behaviors in response to gas or discomfort
- Difficulty tolerating changes in position or touch
These signs are often dismissed as “just colic” or “something they’ll grow out of,” but we know that targeted therapy can make a significant difference—not just in comfort, but in functional development.
 The Role of Rehab Providers: PTs and OTs Working Together
The Role of Rehab Providers: PTs and OTs Working Together
Both physical therapists and occupational therapists play essential roles in assessing and treating infant pelvic floor dysfunction.
Physical therapists focus on:
- Core and pelvic floor coordination
- Alignment and tension patterns affecting bowel/bladder mechanics
- Breathing mechanics and diaphragm coordination
- Tummy time, head shape, and early motor development
Occupational therapists bring expertise in:
- Feeding and oral-motor function
- Sensory integration, especially around elimination and body awareness
- Nervous system regulation and co-regulation strategies for parents
- Positioning to support optimal arousal and digestion
Together, this integrative approach addresses the whole baby, not just their symptoms.
Why This Matters: Long-Term Impacts Start Early
We’re not just aiming to reduce fussiness or help with pooping (although that’s often where we start!). We’re helping to lay the foundation for:
- Healthy bowel and bladder habits
- Confident motor skill development
- Positive body awareness and sensory processing
- Easier transitions to solids and potty training down the road
Early therapy can prevent compensatory patterns and teach families tools that make everyday care easier and more connected.
A Tool for Your Toolbox: Pediatric Pelvic Floor Play Skills
To help bridge the gap between pelvic health and pediatric development, we offer a class called Pediatric Pelvic Floor Play Skills. It’s designed for rehab professionals to learn specific play skills and actionable treatment techniques for each age group of the pediatric client, from the infant to the teen/tween.
For each age category we cover:
- Age-specific considerations, tips, and tricks
- Play-based strategies to support pelvic floor coordination for each age
- How to support pelvic health treatment
- Case studies and hands-on tools for both PTs and OTs
- Problem solving for more difficult cases and situations
If you're looking to expand your skill set, collaborate across disciplines, or just get more confident in treating your littlest patients - this class is for you. Join me next weekend on May 4th!
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating pelvises and ages with a variety of Pelvic Health dysfunctions. There is not much she has not treated since beginning this journey, and she is always happy to further her education to better help her patients meet their goals.
Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating pelvises and ages with a variety of Pelvic Health dysfunctions. There is not much she has not treated since beginning this journey, and she is always happy to further her education to better help her patients meet their goals.
Dr. Pluchino strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at present. In 2020, she opened her own practice called Practically Perfect Physical Therapy to help meet the needs of more clients. She has been a guest lecturer for Rutgers University's Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.
Sometimes as rehab providers, we find patients have deep posterior pain, or they have a “hitting something” sensation with intimacy. Maybe they have a deep pelvic ache or nerve sensation with sitting or passing bowels.
We know the deep structures all have the word “coccygeus” in them: iliococcygeus, pubococcygeus, and coccygeus. We also know there are ligaments that attach to this coccyx (sacrospinous ligament and sacrotuberous ligament), creating a web of support in the posterior pelvis, which has very little bony structure. When we are treating someone with deep vaginal or deep posterior pelvic pain, do we really have to “go there” and treat the coccyx internally?
Did you know that actual spinal cord fibers enter the top of the sacral foramen, travel through this tunnel in the sacrum, and come out the bottom, where they fuse with the posterior coccygeal ligament on the dorsal surface of the coccyx? They can be a tremendous source of neural and pain dysfunction in the pelvis.
In addition, the gluteus maximus attaches at the coccyx, as well as attachments from a deep bowl of fascia, called the endopelvic fascia, that lines the pelvis. The endopelvic fascia is a tremendous source of support in the pelvis but is also often a pain generator. On top of this, the massive sacrotuberous and sacrospinous ligaments also attach at the sacrococcygeal junction.
In Sacral Nerve Manual Assessment and Treatment, scheduled for May 31 through June 1, we spend time addressing how to externally treat the deep structures that attach at the posterior pelvic floor and coccyx. We address ways to treat the incredibly dense sacrotuberous and sacrospinous ligaments that attach to the coccyx from the outside. All of the nerves that supply the posterior hip, glutes, and pelvic floor squeeze between the piriformis and the sacrospinous ligament. This site where these nerves, including the pudendal, sciatic, inferior gluteal, nerve to obturator internus, and posterior femoral cutaneous, can also be a common site of dysfunction and compression. We will learn how to decompress all of this in class, as well as the surrounding soft tissues.
So, coming back to our question. With all this soft tissue and ligament work that can be external, can we forego internal rectal work? Actually….no. Both are important. The best way to treat a side-bent coccyx or an excessively flexed coccyx is internally. However, the real magic is addressing the alignment interiorly and then addressing all the softer tissues (ligaments, fascia, skin, muscle) that keep pulling the bone back into its old bad habits and misalignment.
AUTHOR BIO:
Nari Clemons, PT, PRPC
 Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment and Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jenna Ross, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jenna Ross. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment and Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jenna Ross, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jenna Ross. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari’s passions include teaching students how to use their hands more receptively and precisely for advanced manual therapy skills while keeping it simple enough to feel
A few years ago, I was convinced my left hip pain was due to osteoarthritis. When my hip locked up after a 14 mile run, my manual therapist husband differentially diagnosed the pain as discogenic. Partly in denial and partly wanting to know the extent of the “damage,” I got an x-ray of my left hip, which was completely normal, and a lumbar MRI, which wasn't pretty. The source of my hip pain was a disc bulge at L3-4 and L4-5 with a Schmorl's node at L5-S1 to boot. Instead of riding the train of thought that we treat what hurts, therapists need to disembark and look further for the source, as suggested in the course, “Finding the Driver in Pelvic Pain.”
A case report published in the International Journal of Sports Physical Therapy by Livingston, Deprey, and Hensley (2015) documents the discovery of a deeper problem than the referring diagnosis of greater trochanteric pain syndrome. A 29 year old female had to stop running because of lateral hip pain that began 3 months after increasing the intensity and frequency of her running and low impact plyometrics. She had pain in sitting and while running. During the evaluation, she demonstrated a positive Trendelenburg, weak and painless hip abductors, and a positive single leg hop test on concrete. When the pain was not elicited with single leg hop on a foam surface, the patient was referred back to the physician for magnetic resonance imaging. The patient was later diagnosed with an acetabular stress fracture. The therapist’s thorough examination helped prevent possible avascular necrosis or a more traumatic fracture of the pelvis.
In a 2013 issue of the same journal, Podschum et al. presents a case report on deciphering the diagnosis in a female runner with deep gluteal pain with pelvic involvement. A 45 year old female marathon runner reported pulling her hamstring and complained of left ischial tuberosity pain with aching into the gluteal and pubic ramus regions that eventually forced her to stop running. She had pain in sitting and could not tolerate speed work. She had a history of low back and pelvic floor pain, with an MRI showing osteitis pubis, a lateral L3-4 bulge, and facet hypertrophy at L4-5. The physical therapist ruled out lumbar disc lesion, radiculopathy, sacroiliac joint dysfunction, and hip labral tear with special tests. Initial treatment focused on the differential diagnoses of hamstring syndrome and ischiogluteal bursitis based on subjective complaints and objective findings. After 4 visits, her deep ache shifted to the inferior pubic ramus in sitting as the ischial tuberosity pain diminished. A trained therapist then conducted a thorough pelvic floor exam. Pelvic floor hypertonic dysfunction was diagnosed and took over the “driver’s seat” as the focus for the rest of the treatment of this patient. Symptoms resolved and the patient returned to running marathons without any of her initial presenting symptoms.
If we let specific pain complaints guide our treatment, we will run out of steam with the lack of progress. Finding the true source of symptoms is critical in physical therapy. Sometimes so much is going on with our patients we have to sort through the weeds before we can access the actual road to recovery. The lumbar spine, hips, and pelvic floor create an intricate map of U-turns and two-way streets, so we need to deepen our understanding of how to navigate the regions. Only then will be able to confidently diagnose the “driver” and let the other areas call “shotgun.”
References:
Livingston, J. I., Deprey, S. M., & Hensley, C. P. (2015). DIFFERENTIAL DIAGNOSTIC PROCESS AND CLINICAL DECISION MAKING IN A YOUNG ADULT FEMALE WITH LATERAL HIP PAIN: A CASE REPORT. International Journal of Sports Physical Therapy, 10(5), 712–722.
Podschun, L., Hanney, W. J., Kolber, M. J., Garcia, A., & Rothschild, C. E. (2013). DIFFERENTIAL DIAGNOSIS OF DEEP GLUTEAL PAIN IN A FEMALE RUNNER WITH PELVIC INVOLVEMENT: A CASE REPORT. International Journal of Sports Physical Therapy, 8(4), 462–471.
Have you ever gambled with what you thought was gas, only to find out that it was not? When my son was little, he asked me one day, “Mom did you ever try to fart, but it wasn’t really a fart?” At the time, I told him it was called a “shart.” Of course, being a little boy, he thought that was funny. However, being an adult and thinking you are passing gas, and it not be only gas can be mortifying. Think about how that could affect your quality of life and ability to go out in public. If you can’t trust your anal sphincters and anal canal to not know what you are letting go, it can be stressful!
What can lead to confusion and issues with sensation in this area? There are many different reasons that this area may not function ideally and be able to identify what is within the anal canal. These reasons can range from surgery in the area, radiation therapy, more minor procedures such as hemorrhoid treatment, and even chronically ignoring the urge to defecate. When sensation changes, the function of the sampling response and rectoanal inhibitory reflex (RAIR) or sampling response is changed.
The sampling response is when a small amount of fecal matter accumulates in the rectum, and a stretch occurs in the area. This then triggers a relaxation of the internal anal sphincter, and a contraction of the external anal sphincter that allows a small amount of the fecal matter to drop down into the anal canal. The contents of fecal matter are sampled, and it is determined if it is solid, liquid, or gas. If it is gas, then we can select to expel it; if it is liquid we usually respond with a stronger contraction of the external anal sphincter to hold it in. If it is solid, we can determine whether or not it is a good time to go. If it is, then we head to the restroom; if it is not, we engage the rectoanal inhibitory reflex and hold the stool until we decide there is a better time. You can see, if this sampling and identifying of the contents is off and not functioning properly, then we can have some issues arise and situations with “sharts” that would not be ideal!
We as pelvic rehab clinicians are the perfect people to help people when their sensation is not optimal, and they may have some issues with fecal and flatulence incontinence. Using rectal balloon catheters has been a game changer in my practice when working with these patients that have issues with sensation in their anal canal. The balloon retraining helps with retraining sensation in this area. I use it along with strengthening the pelvic floor and external anal sphincter; along with any manual therapy that may be needed, and defecation training. The addition of the balloons allows me to address sensation. The use of adding or removing small amounts of air in an inflated balloon allows the patient to learn what changes in sensation in the area feel like, which improves sensation and awareness of the contents within the anal canal. If you think about it, there isn’t another way to treat sensation inside of the anal canal. If we can retrain sensation, then we can make it less likely for a patient to think they are safe with expelling gas but be surprised when more comes out!
Join me for the May 17th course offering of Anorectal Balloon Catheters- Intro and Practical Applications. In this short course, you will learn how to use balloon catheters and even practice a lab using balloons. The purchase of a balloon is needed before the course so that you can participate in the labs. This course can change how you treat your patients who may suffer from fecal incontinence and constipation.
AUTHOR BIO
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC (she/her) has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health, including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC (she/her) has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health, including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies and physicians.
Outside of work, Allison enjoys spending time with her family, caring for her animals, reading, traveling, and most importantly of all, being a mom! She lives in the Denver metro area with her family.

So often, we think of vulvodynia as a condition of the skin. And it is….kind of. Vulvodynia is a long-term pain (or burning, discomfort, or itching) that is present in the outer genitals, also known as the vulva. This condition is defined as a discomfort that has lasted longer than 3 months. The symptoms of vulvodynia can vary. In some patients, it is provoked (brought on by touch or stimulation), and in some cases, it is unprovoked (present without stimulation). Some patients have pain just in the outer vulva, while others also present with pelvic floor muscle tension or urethra, bladder, or vaginal canal irritation.
The definition of vulvodynia itself states there is no known reason. This means it is not because of a skin disruption, hormonal disorder, herpes or other skin conditions, or active infection, such as yeast. This means we really don’t know just why a person has symptoms once they have been medically ruled out.
When we look at the symptoms of neuralgia (an irritated or overly talkative nerve), we find symptoms listed such as pain, hypersensitivity, burning, tingling, itching, or trigger points. Certainly, there is a lot of overlap between neuralgia symptoms and vulvodynia symptoms.
When there is compression of a nerve, it can create neuralgia of the affected dermatome. In fact, in studies, we find neural proliferation of the peripheral nerve with vulvodynia in cell biopsy in women or in animal models (1, 2). Often, neural compression is part of the problem, and this is why we see treatment models proving effective at times with nerve blocks or nerve decompression (3, 4).
Of course, when treating such patients, we can and should still employ proven topical agents to make the treatments comfortable and effective, such as lidocaine solutions (5). Vulvodynia is best treated and managed as a team, with manual therapy and patient education from pelvic health providers being a very important limb of treatment.
By treating fascial tunnels that nerves run through, treating the fascia around the clitoris, and treating the deep fascia and tissues of the labia majora and mons, we can have an effect on the pudendal nerve branches, as well as the genitofemoral and ilioinguinal nerves supplying this region. In Lumbar Nerve Manual Assessment and Treatment scheduled for May 17-18, and Sacral Nerve Manual Assessment and Treatment scheduled for May 31-June 1, both heavy manual therapy classes, we learn to decompress the neurovascular bundle from proximal to distal and to treat distal soft tissue structures that may be compressing nerves.
Resources:
1. Goetsch MF, Morgan TK, Korcheva VB, Li H, Peters D, Leclair CM. Histologic and receptor analysis of primary and secondary vestibulodynia and controls: a prospective study. Am J Obstet Gynecol. 2010;202:614.e1–614.e8. doi: 10.1016/j.ajog.2010.01.028.
2. Bornstein J. Vulvar disease. Cham: Springer International Publishing; 2019. Vulvar pain and vulvodynia; pp. 343–367.
3. Vulvodynia treatments, National Vulvodynia Association (nva.org)
4. Possover M, Forman A. Pelvic Neuralgias by Neuro-Vascular Entrapment: Anatomical Findings in a Series of 97 Consecutive Patients Treated by Laparoscopic Nerve Decompression. Pain Physician. 2015 Nov;18(6):E1139-43. PMID: 26606029.
5. Loflin BJ, Westmoreland K, Williams NT. Vulvodynia: A Review of the Literature. J Pharm Technol. 2019 Feb;35(1):11-24. doi: 10.1177/8755122518793256. Epub 2018 Aug 20. PMID: 34861006; PMCID: PMC6313270.
AUTHOR BIO:
Nari Clemons, PT, PRPC
 Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment and Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jenna Ross, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jenna Ross. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment and Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jenna Ross, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jenna Ross. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari’s passions include teaching students how to use their hands more receptively and precisely for advanced manual therapy skills while keeping it simple enough to feel successful. She also is an advocate for therapists learning how to feel well and thrive as they care for others, which is a skill that can be developed. “Basically, I love helping therapists learn to help themselves and others more while having a lot of fun doing it.” Nari lives in Portland Oregon, where she runs a local study/mentoring group and has a private practice, Portland Pelvic Therapy. Her interests include meditation, working out, nature, and being constantly humbled from raising her three amazing teenagers!
Let me share one of my past patients with you.
Joe came in every day for treatment with a bandana that matched the color of his shirt, carefully wrapped around the four residuums that ended at his first metacarpals. My clinical instructor Nicki, a hand specialist, introduced me to the set of dowels that we used to help desensitize Joe’s residuums to prepare him for fitting with a prosthetic hand. Together, we slowly worked through the dowels, gently massaging his scars to help Joe tolerate pressure and touch on his sensitive severed finger stumps.
Watching his progress that summer from his first day of treatment, when he could barely tolerate unwrapping his hand from the bandana that protected his raw injury from all contact with the outside world, to his tolerating increased pressure and challenging textures with the dowels, I was as inspired by his courage as I was by his progress. I marveled at the body’s ability to respond to treatment. The same stimuli that was once so painful could become tolerable and even painless with time and treatment.
Several years and many Herman & Wallace courses later, I started treating patients with dyspareunia and pelvic pain in my private practice. My patients’ expressions of anxiety with the unwrapping, of fear of pain with anticipation of touch seemed familiar, I remembered Joe. The body parts may be different, but the nervous system is one and the same.
While Joe’s injury and source of pain and sensitivity was obvious even to the layperson, our patients with dyspareunia and pelvic pain are suffering with pain whose source is often invisible even to the most trained clinical eye.
Yet, the treatment principles are similar. Every day, we help patients feel safe in their own bodies by providing both gentle treatment and teaching self-treatment techniques that empower patients to help heal themselves. Dilator training can be viewed in this lens as a master class in desensitization and sensory integration of the vagina. We are teaching the pelvic floor muscles and surrounding tissue to gradually accommodate to the increased size of the dilator being inserted without setting off a five-alarm fire and cascade of painful responses in the nervous system.
We load our treatment toolboxes with deep breathing, relaxation techniques, and biofeedback to help rewire and re-educate the body's responses to stimuli.
This treatment is often compounded when patients come from religiously conservative backgrounds and are raised with restrictive sexual values. This places them at a higher risk of experiencing dyspareunia and painful intercourse. In addition to their pain, they may also be struggling with sexual shame and lack of sexual education, creating a greater barrier to treatment and care. Gaining patients' trust and “buy in” may require a higher level of cultural competence and religious sensitivity than other less emotionally charged specialties.
So, let’s talk about it in my upcoming course, Sex and Religion: Treating Conservative Religious Patients with Cultural Sensitivity, on May 18th. I created this course to help both seasoned and newer therapists open their skill sets to reach more diverse patient populations. In this course, I delve into these topics and explore challenges that face patients who come from conservative religious communities as they interface with the wild world of pelvic health. You leave my course with practical skills for patient interviewing, treatment strategies, and creating a safe and comfortable space for both patients and providers.
Resources:
- Patanwala I, Lamvu G, Mizera M, Fisk M, Blanton E. Learning restrictive sexual values may be associated with dyspareunia. Journal of Endometriosis and Pelvic Pain Disorders. 2020;12(2):61-68. doi:1177/2284026519900108.
- Schermer Sellers, T. (2017). Sex, God, and the Conservative Church: Erasing Shame from Sexual Intimacy (1st ed.). Routledge. https://doi.org/10.4324/9781315560946.
AUTHOR BIO
Rivki Chudnoff, MSPT
 Rivki Chudnoff, MSPT (she/her) is a Midwesterner at heart, born and raised in Chicago. At her private practice, Hamakom Physical Therapy, in Bogota, NJ, she focuses on women’s health and pelvic health rehabilitation for women and children. Rivki graduated from Stern College with a BA in Biology and from the University of Medicine and Dentistry of New Jersey (Rutgers) in 1999 with a Masters of Science in Physical Therapy. Rivki started her physical therapy career in pediatrics, working with children with severe disabilities.
Rivki Chudnoff, MSPT (she/her) is a Midwesterner at heart, born and raised in Chicago. At her private practice, Hamakom Physical Therapy, in Bogota, NJ, she focuses on women’s health and pelvic health rehabilitation for women and children. Rivki graduated from Stern College with a BA in Biology and from the University of Medicine and Dentistry of New Jersey (Rutgers) in 1999 with a Masters of Science in Physical Therapy. Rivki started her physical therapy career in pediatrics, working with children with severe disabilities.
In her practice, Rivki is privileged to work with women at different stages of life. Rivki uses a biopsychosocial approach to guide her patients through the many challenges that they encounter along their journey to healing. Rivki has written extensively on women’s health issues and has presented on pelvic health internationally to sex educators, at community events, and at marriage retreats. In her free time, she enjoys vacationing at Trader Joe’s, burning dinner, and trying to figure out new ways to embarrass her children with her professional life.
As a small business owner, I’m grateful to have weathered the COVID-19 storm. When reflecting on the 5 year anniversary of the shutdown, I remember how we adapted day after day — masking up, running air filtration systems, and feeling grateful that we could continue to do our work safely. Yet, despite prioritizing sleep, nourishing my body with fresh food, staying active, and hydrating well, I sometimes still feel myself carrying a lingering undercurrent of stress and tension in my physical body.
We have spent years holding our breath—both literally and figuratively. The weight of collective uncertainty, change, and grief may have left some imprints on our bodies. I was reminded of this when a sudden flare of lumbopelvic pain forced me to pay closer attention to my own breath patterns. It became clear that I needed to soften, to release layer by layer of held tension, and to deepen my own breathwork and meditation practice.
As healthcare providers, our work extends beyond addressing physical concerns. We are honored to hold space for our patients' grief—whether it stems from physical trauma, medical challenges, gaslighting, or life's hardships.
They trust us, not just for guidance on optimizing their pelvic health, but as guides on their healing journeys. And yet, we too are human. We experience burnout, fatigue, and emotional strain.
We often teach our patients that breath is a bridge—connecting the nervous system, digestion, spine, pelvic floor, and our emotional state. It is one of the most powerful tools we have to remind the body that it is safe. And yet, even with this knowledge, we may find ourselves unconsciously holding our breath because we are humans living in this unpredictable and sometimes challenging world. When we resist feeling something, we don’t breathe. When we are afraid, we hold tension in our ribs. Even in moments when we think we are relaxed, we can sometimes still be bracing our jaw, back, or pelvic floor.
Let’s take a moment to pause.
Notice your body. Try not to make any adjustments to “fix” your posture.
- Where is your ribcage in relation to your pelvic floor?
- Does the breath feel deep or shallow, smooth, or restricted?
- Where do you sense movement—your chest, ribs, belly?
- What temperature is the air as it enters your nose?
What does it feel like to exhale?
- Does your breath release with ease or feel held back?
- Can you soften just a little more with each out-breath?
- Notice if there is a natural pause before your next inhale—what does that moment of stillness feel like?
If you're sitting, allow yourself to slouch for a moment.
- How does your breath feel in this position?
- Is it shallow or restricted?
- Now, gently imagine your head and spine being drawn upward, as if a magnet is lifting you toward the ceiling. Take another breath. Does it feel different? Notice any shifts in ease of expansion or softening more fully after the exhale.
Now, let’s zoom into the intercostal spaces.
- Imagine this space expanding with each inhale and softening with each exhale.
- Can you soften any more in your ribcage?
- Picture your shoulders softening, warm water is dripping down the upper trap and down the arms.
- Let your jaw unclench, your tongue relax, the space between your eyebrows melt.
Take another long, conscious breath.
- What do you notice?
- Does your body feel a little softer, a little more open, or is there still a place holding tension, waiting for a little more attention?
As practitioners, we give so much to others all day long and sometimes forget to remember to check in with ourselves. Staying connected to our own breath and body serves us just as much as it serves our patients. When we remain grounded and at ease, we can reduce fatigue, physical discomfort, and emotional exhaustion.
So, let’s remind ourselves—throughout the day—to take long easy breaths, soften our jaws, and allow our bodies to move with greater ease. It is not only a gift to ourselves to prevent burn out, but also helps us facilitate co-regulation with our patients’ nervous systems.
If you enjoyed this article, then join Dustienne in her upcoming remote course Yoga for Pelvic Health, on May 3-4, 2025. This two-day remote course offers participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain and focuses on two of the eight limbs of Patanjali’s eight-fold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back and pelvic pain. The course will describe the role of yoga within the medical model, discuss contraindicated postures, and explain how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
AUTHOR BIO
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller PT, MS, WCS, CYT (she/her) is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for the Radio City Christmas Spectacular. She is currently an assistant professor of jazz dance at Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
In a recent article entitled “The Effectiveness of Pelvic Floor Muscle Training in Men After Radical Prostatectomy Measured with the Insert Test,” published in the International Journal of Environmental Research and Public Health in March of 2022, the use of surface EMG biofeedback (sEMG) was one of three cohorts for men with post-operative incontinence. While all participants improved in control over micturition, the cohort of men in the group using sEMG biofeedback had the best results post-treatment./p>
So, what is it about biofeedback that improves control in patients with pelvic floor muscle dysfunction?
Biofeedback provides visual and auditory feedback of muscle activity. It is a non-invasive technique that teaches patients how to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process. It is presented visually on a computer screen, giving the patient immediate knowledge of muscle function and enabling the patient to learn how to alter the physiological process through verbal and visual cues.
Kaufman states, “Without full knowledge of the use of the sEMG biofeedback equipment, many providers may miss important components to treatment.” For example, patients may inadvertently hold pelvic muscles in a chronic state of tension in an effort to avoid leakage, reducing the range of muscle excursion available for proper muscle contraction and control. Additionally, poor pelvic floor isolation can compound symptoms of incontinence when larger muscle groups such as the abdominals are co-contracting, reducing the effectiveness of the pelvic floor effort.
Importantly, biofeedback gives the skilled clinician the opportunity to evaluate proper muscle function in all three positions: supine, sitting and standing. According to Lee, “You will typically see the muscle dysfunction in the standing posture, which is not typically assessed in manual treatment.” Furthermore, in supine the muscle may not have dysfunctions and the provider will miss what happens when position is altered, and gravity negatively influences the muscle contraction.
Kaufman adds, “The only true way to determine muscle tone is through the use of sEMG biofeedback.” Manual skills alone may falsely indicate there is no muscle excursion with palpation when, in fact, the use of sEMG biofeedback reveals the presence of high tone in the pelvic muscles at rest. By restoring normal muscle resting tone the patient gains more muscle excursion and is better able to utilize and feel the muscle contract.
Case Study Example
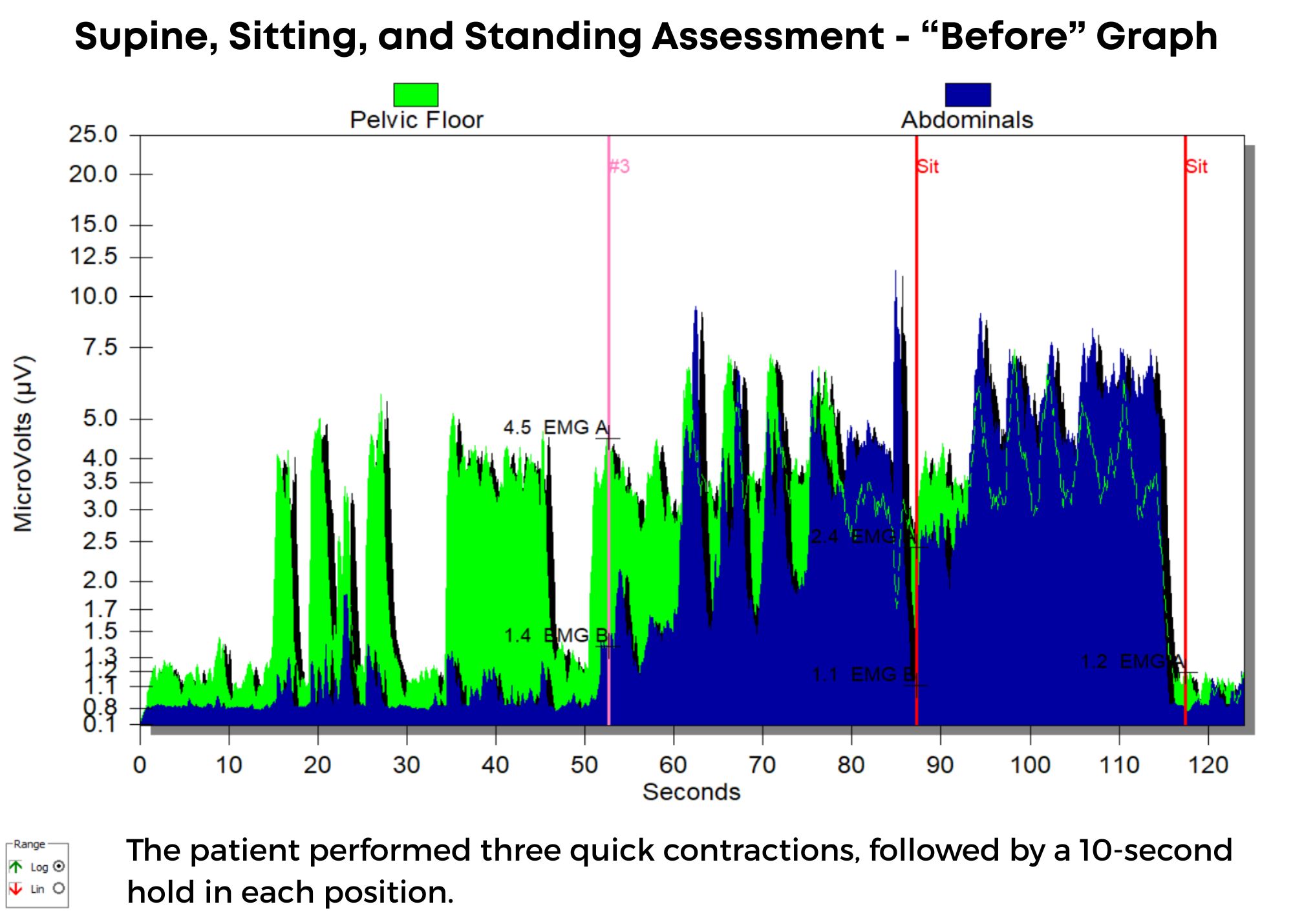
The patient is a 63-year-old computer specialist who underwent radical prostatectomy three years ago due to prostate cancer. He has been relocated for work twice in that time and has seen two pelvic floor therapists during that period who worked exclusively with manual internal and external muscle techniques. Finally, he was referred to a biofeedback board-certified therapist who did a supine, sitting, and standing muscle assessment using two-channel sEMG biofeedback: one channel was for a rectal sensor, and the other monitored the obliques.
The "before" graph is a supine, sitting, and standing assessment. The patient is asked to perform three quick contractions, followed by a 10-second hold in each position. In the supine position, the patient demonstrated good muscle resting tone, endurance, and isolation, but once in sitting, he began to demonstrate poor pelvic floor muscle endurance, poor isolation, and higher resting tone. In standing, his pelvic floor muscle was completely overpowered by his obliques and rectus abdominis, and he had very limited pelvic muscle endurance and poor resting tone. His frustration with lack of bladder control led to withholding fluids (making symptoms worse).
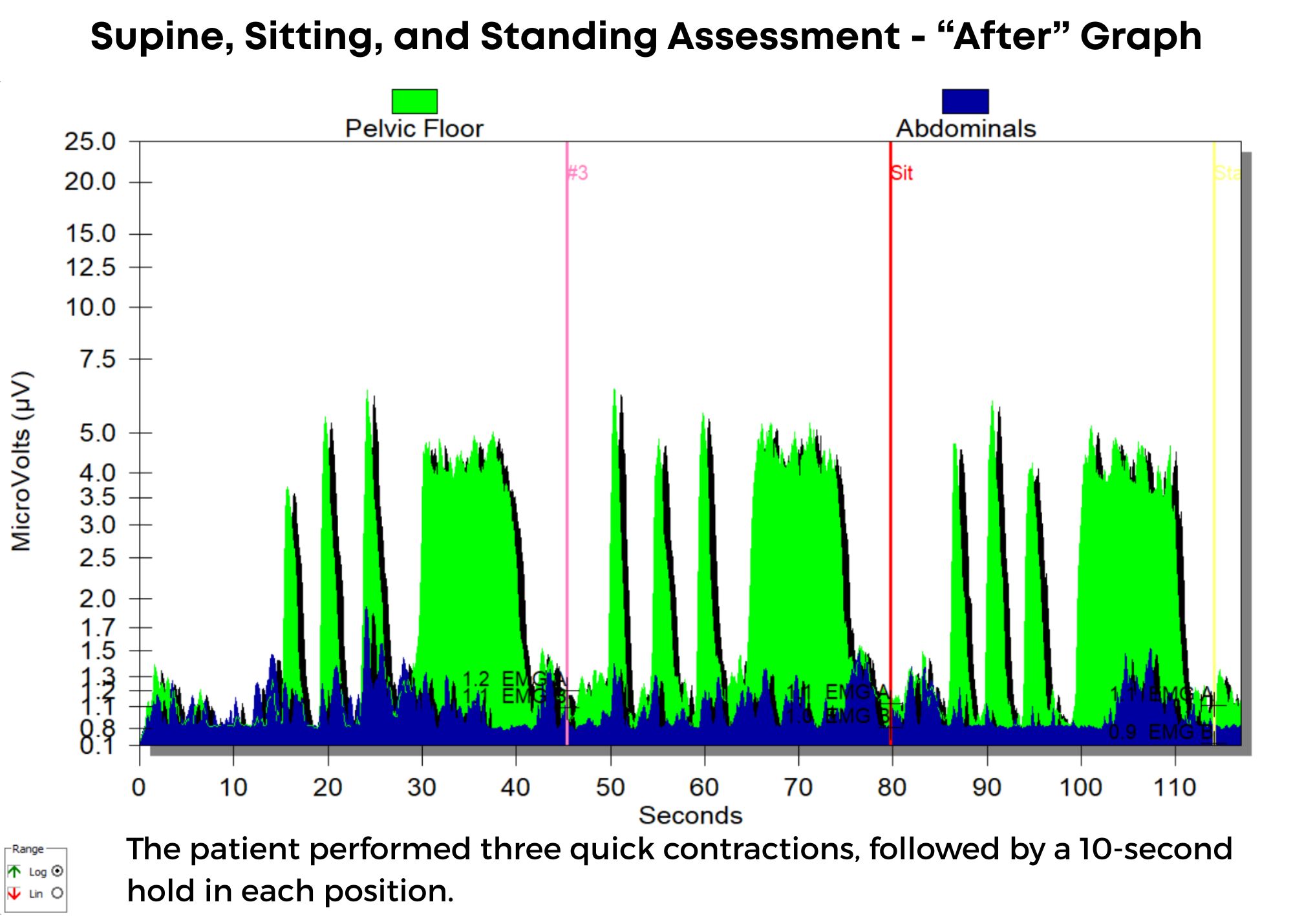
Once the patient was instructed in techniques to restore normal pelvic floor muscle tone and isolated contractions using sEMG biofeedback, he began to note improved control over bladder function, and after eight visits, he was discharged from care, having achieved all treatment goals. In his "after" graph, he exhibited good muscle tone, endurance, and isolation, and did not have his abdominals overpowering his pelvic floor. He also consumed adequate water intake again but without negative effects on bladder control. He no longer needed protective undergarments.
Conclusion
A long history of scientific evidence supports using sEMG biofeedback in managing incontinence or pain symptoms. As a noninvasive, cost-effective, and powerful treatment modality, healthcare providers should consider this tool when managing pelvic floor dysfunction. Providers should be educated in adequately using this valuable modality to gain the most out of the skills and knowledge achieved through this intervention. For more information regarding courses and certification, please visit www.pelvicfloorbiofeedback.com.
Biofeedback for Pelvic Muscle Dysfunction, a self-hosted lab course scheduled for May 4, 2025, is led by Instructors Kaufman and Lee who introduce participants to the use of biofeedback when treating bladder, bowel, and pelvic floor disorders. In this course, participants learn about surface EMG biofeedback by using the equipment on themselves to experience dynamic muscle assessment in supine, sitting, and standing positions. This dynamic course also includes behavioral strategies for relearning proper muscle control for improved pelvic floor function.
Instructors Kaufman and Lee have over fifty years of combined experience using this amazing clinical tool. This treatment approach uses sEMG biofeedback to visualize muscle dysfunction, then allows for proper training and education to re-establish proper muscle movement patterns, enabling patients to gain control over function and realize they can succeed in improving symptoms. Lee adds, “Patients are constantly validating the usefulness of this modality by reaping the benefits of skilled training and behavior modification strategies.”
References:
- Cram, J. R., & Kasman, G. S. (2011). The basics of surface electromyography. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7). Jones and Bartlett
- Kaufman, J., Stanton, K., & Lee, T. E. (2021). Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Biofeedback, 49(3), 71-76.
- Shelly, Beth & Kaufman, Jane (2023). Foundations of Pelvic Floor Muscle Assessment Using Surface Electromyography. APTA Academy of Pelvic Health Physical Therapy.
- Szczygielska D, Knapik A, Pop T, Rottermund J, Saulicz E. (2022). The Effectiveness of Pelvic Floor Muscle Training in Men after Radical Prostatectomy Measured with the Insert Test. Int J Environ Res Public Health. 2022 Mar 2;19(5):2890. doi: 10.3390/ijerph19052890. PMID: 35270582; PMCID: PMC8910379.
AUTHOR BIO
Tiffany Lee, OTR, OTD, MA, BCB-PMD, PRPC
 Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman and Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.
Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman and Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.

As rehabilitation professionals, we must ask ourselves: Are we fully educating our patients on all available rehab techniques beyond just Kegels? Here’s an evidence-based overview of penile rehabilitation following radical prostatectomy, emphasizing the importance of a comprehensive approach to restore erectile function and maintain overall penile health.
Understanding Penile Rehabilitation
Penile rehabilitation focuses on enhancing blood flow to the penis after radical prostatectomy (removal of the prostate). Even with nerve-sparing techniques, the cavernous nerves—essential for erections—can sustain trauma. This injury, known as neuropraxia, may require up to two years to recover from, potentially leading to temporary or prolonged changes in erectile function.
Why Rehabilitation Is Critical
- Preservation of Function: Rehabilitation helps sustain blood flow and minimizes the risk of venous leakage, where the veins fail to maintain blood within the penis.
- Preventing penile atrophy: The "use it or lose it" principle is fundamental in penile rehabilitation.
- Prevention of Fibrosis: Consistent treatment can reduce the formation of scar tissue (fibrosis), which may otherwise contribute to conditions such as Peyronie’s disease.
- Maintenance of Penile Length: Emerging evidence suggests that a well-structured rehabilitation program may help restore or maintain penile length, which is compromised after surgery.
Key Rehabilitation Techniques
- Mechanical Devices:
- Penile Pump/Vacuum Device: Utilizes negative pressure to draw blood into the penis, assisting in achieving an erection.
- Medications:
- Intracavernosal Injections: Direct injection of medications like Trimix or Caverject into the penis to induce an erection.
- Low-Dose PDE5 Inhibitors: Daily administration of drugs such as Viagra or Cialis is used to enhance blood flow and protect the endothelial cells lining blood vessels. It’s important to note that these drugs depend on functional erectile nerves to produce an erection, so their role is primarily to provide vascular support.
- Sexual Activity:
- Regular Arousal and Orgasm: Encouraging regular sexual activity, whether through masturbation or with a partner, is beneficial. Even without an erection, achieving orgasm (which will be dry post-surgery due to the removal of the prostate and seminal vesicles) can significantly improve blood flow.
- Pelvic Floor Exercises:
- Strengthening Muscles: Targeting the pelvic floor muscles can enhance blood flow and support neural arousal signals, contributing to improved erectile function.
- Cardiovascular Exercise:
- Overall Circulation: Regular cardiovascular workouts are crucial for heart health and circulation, which in turn supports erectile health.
Remember, as rehab professionals, education is our most important treatment. Educate patients on all the available options they can be utilizing.
Final Considerations for Providers
While these strategies show considerable promise, recovery is a gradual process, and patient outcomes may vary. It is essential to have open, detailed discussions with patients about these options. Tailoring a rehabilitation program that addresses each individual’s needs and recovery trajectory can significantly impact both their sexual function and overall vascular health after prostate surgery.
By expanding our education and ensuring our patients are well-informed about all available rehabilitation options, we can optimize recovery and improve long-term outcomes.
If you would like to learn more about this topic and other topics in sexual medicine, then join Tara Sullivan in Sexual Medicine in Pelvic Rehab on May 3-4, 2025. This course provides thorough introduction to pelvic floor sexual function, dysfunction and treatment interventions for males and females of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Mechanical Devices (Penile Pump/Vacuum Devices)
Mulhall, J. P. (2020). Penile rehabilitation: Preserving erectile function after radical prostatectomy. Current Urology Reports, 21(3), 14. https://doi.org/10.1007/s11934-020-00961-3
Medications: Intracavernosal Injections and PDE5 Inhibitors (also relevant to sexual activity)
Burnett, A. L., Nehra, A., Breau, R. H., Culkin, D. J., Faraday, M. M., Hakim, L. S., Heidelbaugh, J., Khera, M., McVary, K. T., Miner, M. M., … & Shindel, A. W. (2018). Erectile dysfunction: AUA guideline. The Journal of Urology, 200(6), 633–641. https://doi.org/10.1097/JU.0000000000000626
Sexual Activity (Regular Arousal and Orgasm): This concept is also emphasized in the AUA guideline above, which supports the role of ongoing sexual activity in penile rehabilitation.
Burnett, A. L., Nehra, A., Breau, R. H., Culkin, D. J., Faraday, M. M., Hakim, L. S., Heidelbaugh, J., Khera, M., McVary, K. T., Miner, M. M., … & Shindel, A. W. (2018). Erectile dysfunction: AUA guideline. The Journal of Urology, 200(6), 633–641. https://doi.org/10.1097/JU.0000000000000626
Pelvic Floor Exercises
Wong, C., Louie, D. R., & Beach, C. (2020). A systematic review of pelvic floor muscle training for erectile dysfunction after prostatectomy and recommendations to guide further research. The Journal of Sexual Medicine, 17(4), 737–748. https://doi.org/10.1016/j.jsxm.2020.01.008
Sivaratnam, L., Selimin, D. S., Abd Ghani, S. R., et al. (2021). Behavior-related erectile dysfunction: A systematic review and meta-analysis. The Journal of Sexual Medicine, 18(1), 121–143. https://doi.org/10.1016/j.jsxm.2020.09.009
Mulhall, J. P. (2020). Penile rehabilitation: Preserving erectile function after radical prostatectomy. Current Urology Reports, 21(3), 14. https://doi.org/10.1007/s11934-020-00961-3. This review provides updated insights into penile rehabilitation strategies after radical prostatectomy, highlighting the early use of VEDs as a means to “exercise” the penile tissues, sustain blood flow, and prevent atrophy.
Hatzimouratidis, K., Giuliano, F., Moncada, I., et al. (2018). EAU guidelines on erectile dysfunction. European Urology, 76(1), 72–79. https://doi.org/10.1016/j.eururo.2018.01.024\
Cardiovascular Exercise (Physical Activity)
Silva, A. B., Sousa, N., Azevedo, L. F., & Martins, C. (2017). Physical activity and exercise for erectile dysfunction: Systematic review and meta-analysis. British Journal of Sports Medicine, 51(20), 1419–1424. https://doi.org/10.1136/bjsports-2016-096418
AUTHOR BIO
Tara Sullivan, PT, DPT, PRPC, WCS, IF
 Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage and anatomy & physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in the field of pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage and anatomy & physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in the field of pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara established the pelvic health program at HonorHealth in Scottsdale and expanded the practice to 12 locations across the valley. She continues treating patients with her hands-on, individualized approach, taking the time to listen and educate them, empowering them to return to a healthy and improved quality of life. Dr. Tara has developed and taught several pelvic health courses and lectures at local universities in Arizona, including Northern Arizona University, Franklin Pierce University, and Midwestern University. In 2019, she joined the faculty team at Herman & Wallace, teaching continuing education courses for rehab therapists and other healthcare providers interested in the pelvic health specialty, including a course she authored - Sexual Medicine in Pelvic Rehab, and co-authored Pain Science for the Chronic Pelvic Pain Population. Dr. Tara is very passionate about creating awareness of Pelvic Floor Dysfunction and launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
In March 2024, Dr. Tara left HonorHealth and founded her company Mind to Body Healing (M2B) to continue spreading awareness on pelvic health, mentor other healthcare providers, and incorporate sexual counseling into her pelvic floor physical therapy practice. She has partnered with Co-Owner Dr. Kylee Austin, PT.

“The times they are a-changin,” Bob Dylan once sang.(1) Dylan’s song may have been from 1964, but the lyrics can be applied to the present day. Very recently, the world, and the United States in particular, has seen rapid changes in political landscapes.
For instance, America has seen an increase in anti-transgender legislation over the last several years, but also in the past few weeks and months. Many of these laws seek to ban gender-affirming care for transgender, gender non-conforming, and non-binary people, youth in particular., Another bill was introduced just 1 week prior to this post that would make it illegal to identify as transgender on legal documents in Texas, calling it “gender identity fraud,” and carrying with it potential felony charges and jail-time.(2)
What many don’t know is that in addition to charges like the one above, many of these bills also contain exceptions that allow for non-consensual surgeries to be performed on intersex infants and children. The Human Rights Watch states that these procedures on intersex children “are justified by decision-makers on the grounds that they will reduce stigma and prevent gender dysphoria, but they often have the opposite effect and also carry risks of scarring, loss of sensation, lifelong sexual dysfunction, urinary incontinence, psychological trauma, and permanent sterilization.”(3)
For example, in January 2025, an Executive Order from the United States government stated that it would “not fund, sponsor, promote, assist, or support” gender-affirming care for children under the age of 19 “and it will rigorously enforce all laws that prohibit or limit” gender-affirming procedures and treatments.(4) Many American hospitals immediately paused surgical and hormonal gender-affirming treatments for patients under the age of 19 following the order.(5) However, it was found by March 2025 that despite gender-affirming surgeries being paused, non-consensual surgeries were allowed to continue and were still being performed on Intersex infants and children during that time. These non-consensual Intersex procedures were performed by many of the same providers at hospitals who had stopped performing the gender-affirming procedures.(6)
On January 16, 2025, the United States Department of Health & Human Services released the Advancing Health Equity for Intersex Individuals report. This report affirmed the rights of Intersex people to bodily autonomy and informed consent, mentioned health equity barriers for Intersex people, and said that “health care providers and parents can work together to decide that it is in the best interest of the child to delay any non-emergent medical interventions until an intersex child is old enough to be involved in the decision-making about their sexual and reproductive health.”(7) InterACT Advocates for Intersex Youth, called the HHS report, “a victory for the right of intersex children to make their own choices about their own bodies.”(8)
Just days after the release of the HHS report, new government Executive Orders were issued that redefined words like “male,” “female,” “woman,” “man,” and “sex.”(9) This order was intended to impact the transgender and gender diverse communities. However, these Executive Orders impact the Intersex community, as well, as Intersex people can have any gender identity. InterACT says that “many grow up with a gender identity that does not align with their assigned sex at birth – meaning that there is overlap among transgender and intersex communities.”(10) These orders impact cisgender Intersex people, as well. According to InterACT, as “a woman with Complete Androgen Insensitivity (CAIS) may be assigned female at birth, and identify as a woman all her life, while having internal testes – yet the Order would define her sex by her gonads and the reproductive cells they produce.”(10)
***It’s important to note that with the introduction of the new Executive Order, the HHS report has been removed from the HHS and other government websites. InterACT saved the HHS report, and it is accessible on InterACT’s website at this time.***
As laws, reports, and orders are quickly shifting, the healthcare world is rapidly transforming with it. We may not know what local, national, or global changes are on the horizon for the world of politics, the world of healthcare, or the world in general. But one thing that we do know is that healthcare providers need to continue to be advocates for and continue to provide the best evidence-based healthcare to all of our patients, including those who are intersex or transgender.
To learn more about how to be an ally in healthcare and provide better evidence-based care to intersex folx, come take Intersex Patients: Rehab & Inclusive Care with me on May 3, 2025!
Resources
- Dylan, B. (1964). The Times They Are A-Changin [Album]. Columbia Records.
- Yurcaba, J. (2025, March 10). Texas Bill Would Make Identifying as Transgender a Felony Punishable By Jail. NBC News. https://www.nbcnews.com/nbc-out/out-politics-and-policy/texas-bill-identify-transgender-state-felony-rcna195642.
- Human Rights Watch. (2022, October 26). S. Anti-Trans Bills Also Harm Intersex Children. https://www.hrw.org/news/2022/10/26/us-anti-trans-bills-also-harm-intersex-children.
- The White House. (2025, January 28). Protecting Children from Chemical and Surgical Mutilation. https://www.whitehouse.gov/presidential-actions/2025/01/protecting-children-from-chemical-and-surgical-mutilation/.
- Betts, A. (2025, February 3). U.S. Hospitals Suspend Healthcare for Transgender Youth After Trump Order. The Guardian. https://www.theguardian.com/us-news/2025/feb/03/trans-youth-healthcare-hospitals-trump.
- Rodriguez, B., & Sosin, K. (2025, March 10). Hospitals that Paused Youth Gender-Affirming Care Continued Controversial Intersex Surgeries, Group Says. The 19th*. https://19thnews.org/2025/03/hospitals-intersex-surgery-gender-affirming-care-youth/.
- S. Department of Health & Human Services Office of the Assistant Secretary for Health. (2025, January 16). Advancing Health Equity for Intersex Individuals. InterACT Advocates for Intersex Youth. https://interactadvocates.org/wp-content/uploads/2025/01/intersex-health-equity-report.pdf.
- (2025, January 16). Intersex Health Equity Report. https://interactadvocates.org/hhs-supports-bodily-autonomy/.
- United States Presidential Actions. (2025, January 20). Defending Women from Gender Ideology Extremism and Restoring Biological Truth to the Federal Government Executive Order. https://www.whitehouse.gov/presidential-actions/2025/01/defending-women-from-gender-ideology-extremism-and-restoring-biological-truth-to-the-federal-government/.
- InterACT Advocates for Intersex Youth. (2025, January 21). Trump’s Executive Order Ignores Science to Push Discriminatory Agenda. https://interactadvocates.org/trumps-executive-order-ignores-science-to-push-discriminatory-agenda/.
AUTHOR BIO
Molly O’Brien-Horn, PT, DPT, CLT, PCES
 Molly O’Brien-Horn, PT DPT, CLT, PCES graduated from Rutgers School of Biomedical & Health Sciences (formerly the University of Medicine & Dentistry of New Jersey) with her Doctor of Physical Therapy degree. She is a Pelvic Health Physical Therapist, a Certified Lymphedema Therapist and an LSVT BIG Parkinson’s Disease Certified Therapist. Molly is also a sex counselor, a trained childbirth doula, and a trained postpartum doula. Molly is a member of the American Physical Therapy Association Academy of Pelvic Health Physical Therapy and is also a Teaching Assistant with the Herman & Wallace Pelvic Rehabilitation Institute.
Molly O’Brien-Horn, PT DPT, CLT, PCES graduated from Rutgers School of Biomedical & Health Sciences (formerly the University of Medicine & Dentistry of New Jersey) with her Doctor of Physical Therapy degree. She is a Pelvic Health Physical Therapist, a Certified Lymphedema Therapist and an LSVT BIG Parkinson’s Disease Certified Therapist. Molly is also a sex counselor, a trained childbirth doula, and a trained postpartum doula. Molly is a member of the American Physical Therapy Association Academy of Pelvic Health Physical Therapy and is also a Teaching Assistant with the Herman & Wallace Pelvic Rehabilitation Institute.
Molly is passionate about providing accessible healthcare to pelvic health patients of all age ranges, all gender identities, all sexualities, all body variations, and all ability levels.
She also has experience in a variety of physical therapy settings over the years, including pediatric and adult oncology, school-based pediatrics, inpatient and intensive care unit hospital-based settings, skilled nursing facilities, outpatient and sports-based orthopedics, and wound care.