Discover Inclusive Care for Gender and Sexual Minorities in this interview with Brianna Durand, an expert in inclusive care for gender and sexual minorities. In this insightful video, Durand discusses the importance of tailored and compassionate healthcare for individuals who identify as LGBTQ+.
Gain valuable insights as Durand shares her extensive knowledge on the unique challenges faced by these communities and how to provide comprehensive and inclusive care. With a focus on creating safe and welcoming spaces for all individuals, this video provides valuable information for healthcare professionals and anyone looking to support the LGBTQ+ community.
Are you looking to improve your knowledge and understanding of inclusive care for the LGBTQ+ community? Look no further! Our remote course on Inclusive Care for Gender and Sexual Minorities is here to guide you through the most important principles and best practices in providing compassionate and equitable care for individuals of all gender identities and sexual orientations.
Led by industry expert, Brianna Durand, this comprehensive course will cover topics such as terminology, cultural competency, and the unique healthcare needs of gender and sexual minorities. By the end of the course, you will have the tools and resources to confidently offer inclusive and affirming care to all patients, regardless of their gender or sexual identity.
Don't miss this opportunity to learn from one of the top leaders in inclusive healthcare. Enroll now in the December 9th Inclusive Care for Gender and Sexual Minorities Course and take the first step towards becoming a more inclusive healthcare provider.

This article was originally posted on the Medbridge Blog site: https://www.medbridgeeducation.com/blog/2021/11/six-actionable-ways-to-be-a-better-lgbtq-ally/.
Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians. Brianna owns and operates Empower Physiotherapy, a private practice in Seattle. As a competitive powerlifter, Brianna enjoys working with strength athletes who experience pelvic floor dysfunction, especially stress incontinence. She is passionate about providing care to individuals in the LGBTQ+ community, including those undergoing hormonal/surgical transition. Brianna's additional clinical interests include prenatal/postpartum care for trans and gender-nonconforming folx and pelvic floor care for patients that are intersex. Brianna curated and teaches LGBTQ+ cultural competency for practitioners in her course - Inclusive Care for Gender and Sexual Minorities.
LGBTQIA2S+. Does it seem like that acronym is ever-growing? That’s because it is!
As our society evolves, more people are feeling safe and comfortable to live as their authentic selves, and every day there is more evidence to support that.
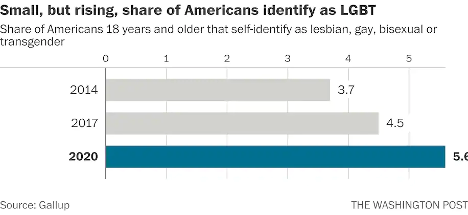
According to Gallup polls, the percentage of people in the U.S. that identify as lesbian, gay, bisexual, or transgender has increased to 5.6 percent.3 That is three times the entire population of Colorado! These numbers are even higher amongst younger generations—up to 20 percent in Gen Z and millennials by some estimates. In 2019, nearly 80 percent of surveyed Americans state that they personally know someone who identifies as LGBTQIA2S+ or queer.2 And while the word “queer” has a nasty history as a derogatory slur, it is increasingly used by folks in the LGBTQIA2S+ community to describe those who do not identify as cisgender or heterosexual.
What Is the Importance of Sexual Orientation or Gender Identity in Healthcare?
Recent years have provided a groundswell of awareness building around this community—from representation in entertainment, discussion about participation in athletics, and changes occurring at the legislative level. However, one area of society in which awareness is still lacking is in modern-day medicine, so let’s explore the significance of sexual orientation and gender identity (SOGI) as it pertains to healthcare.
As a medical professional, you may wonder “Can’t I simply treat all people the same?” While this idea may be filled with good intentions, the unfortunate reality is that we do not yet have access to this utopian future. There are real, measurable differences in the health of all marginalized communities, including gender and sexual minorities (GSM).
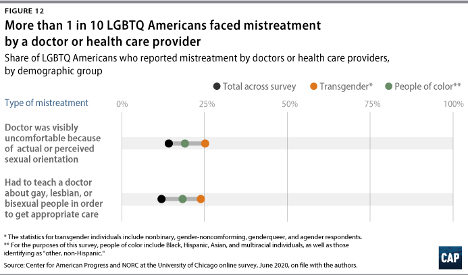
In 2020, 1 in 10 LGBTQIA2S+ Americans faced some form of mistreatment from a healthcare professional.1 These negative experiences strongly correlate with postponing or altogether avoiding medical care in the future, further contributing to the collective LGBTQIA2S+ fear of discrimination. The statistics are even worse when specifically looking at queer and trans people of color.
What Can You Do as a Healthcare Provider?
While the system and the education that trains our clinicians could benefit from a renovation, here are six actionable steps you can take now to facilitate a safer space for your LGBTQIA2S+ patients:
1. Recognize your own potential to cause harm.
As healthcare professionals, we have some degree of inherent privilege. With this privilege comes the capacity to inflict harm, intentional or not. While intentions matter, they do not supersede the impact your words or actions have on another. Assumptions matter, too. While assumption making is common and normal—an evolutionarily advantageous adaptation of the brain—they are not facts, and they are not harmless. Erroneous assumptions about a person’s gender or sexual identity by a medical professional can lead to behaviors that cause discomfort in and discrimination towards LGBTQIA2S+ patients and clients, even if inadvertently.
By recognizing the power differential that exists in the patient/provider relationship and the implications that come with it, we are likely to be more aware of our words and actions when they come up, and more willing to address them when they do. And by taking a position of genuine care and curiosity rather than assumption, we can affirm the relationship between the person whom we are helping and their body.
2. Update your language.
Always use the correct pronouns and name of the person with whom you are working. One easy way to do this is simply by mirroring the language they use when describing themself. However, if you are meeting someone for the first time, you may unintentionally use language that is not in line with your patient or client’s identity. For example, you may use someone’s dead name (the name assigned to them at birth) which may still be listed on their legal and medical documentation.
You can preempt this kind of unintentional harm by including areas for clarification on intake paperwork. This will allow you the opportunity to affirm the pronouns of the person in your care upon your first interaction. While pronoun affirmation may seem like a small action, it has shown to be effective in reducing suicidal ideation and depression.4 Another way to update your language for greater inclusivity is by using the term “spouse” or “partner” when inquiring if a patient has someone at home that can help with their activities of daily living or rehabilitation. Additionally, when referring to pregnancy, birthing, and postpartum care, practice saying “pregnant person” or “birthing parent” rather than “pregnant woman” or “mother.”
3. Speak up….even if the LGBTQIA2S+ person or target of the harm isn’t present.
Shaming someone’s behavior is unlikely to result in positive change or self-reflection. Instead, we can follow the steps of stopping, educating, and being proactive to foster learning in our colleagues. This kind of dialogue offers the opportunity for the individual to participate in the discussion by learning about their behavior, rather than feeling pushed out of the conversation which could limit their chance to grow.
- First, STOP the discussion or action taking place by intervening with “Those words can be hurtful.”
- Next, EDUCATE in lieu of asserting judgment. Proceed from a lens of curiosity. Asking the person “Do you know what those words mean?” or genuinely inquiring about their intention and understanding. Doing this will facilitate conversation and enhance one’s knowledge of their damaging actions, reducing the chance that they will repeat the harmful behavior.
- Finally, BE PROACTIVE by following up with resources for further learning such as GLMA, WPATH, or The Fenway Institute.
It is important to note the significance of taking this action even if the LGBTQIA2S+ person was not present for the encounter. This breaks the notion that harmful language is acceptable so long as the subject of the harm is not privy to it. If the LGBTQIA2S+ person is present for the encounter, it is best to first pull them aside to check in with them, make sure they are alright, and ask if they want your help. Some folks prefer to avoid drawing attention to themselves. It is also a skill of allyship to know when not to talk.
4. Be receptive to feedback.
When an LGBTQIA2S+ person, or a person from any marginalized group for that matter, corrects your language or behavior, practice saying “thank you” rather than “sorry” and avoid explaining yourself. It is a privilege to learn about oppression rather than to experience it for yourself. When someone corrects you, not only are they bravely honoring their authentic identities, but they are doing emotional labor on your behalf, and in the age of freely available information, it is never the responsibility of marginalized folks to educate others for free. These interactions are opportunities for personal growth—don’t let them pass you by!
5. Suggest practical changes to make the workplace more inclusive.
Does your workplace have gender-neutral bathrooms? Many LGBTQIA2S+, queer, and trans people avoid using public restrooms to avoid harassment and violence. Such aggressions can have very tangible consequences to their physical health, such as pelvic floor dysfunction. If there aren’t any inclusive restrooms in your workplace, make a suggestion to change that.
How inclusive are the brochures in your waiting room? Do the patient education materials that you provide to a patient after evaluation use language and imagery that include the LGBTQIA2S+ community? These are areas that can be improved upon with the suggested language updates we discussed above in action step two.
Are there symbols or graphics that will welcome GSM, such as safe space signs, flags depicting an upside-down rainbow triangle, or “all-gender” verbiage in lieu of gender-specific? Both would make easy additions that signal to patients they are in an inclusive space. However, it is important to distinguish the difference between saying a space is safe, and actually making a space safe. A space can only be safe if the entire team of providers and office staff are on board. Labeling a space as safe when it is not has the propensity to cause further harm. Be sure before these indicators are put up in your practice, everyone is ready to support such efforts.
6. Be prepared to mess up—but don’t let that deter you from trying.
Any etymologist will tell you that languages are living things that are constantly evolving. Developments such as these can make it challenging to stay current on which terminology is most beneficial to our growing society. Sometimes just the fear of making a mistake can be intimidating enough to discourage people from trying. What is most important is not how well you use updated language but that you are trying. Your effort matters, and it is what will move the needle in the right direction. Cultural responsiveness is not knowing every nuanced detail of every demographic group. Cultural responsiveness is being willing to reflect and modify your viewpoints when presented with information that differs from what you previously held to be true. Try to accept that just with learning any new skill, mistakes are bound to happen. When they do be prepared to learn, and then move forward with that new knowledge in mind.
References:
- Cusick Director, J., Seeberger Director, C., Woodcome, T., Oduyeru Manager, L., Gordon Director, P., Shepherd, M., Parshall, J., Santos, T., Medina, C., Gruberg, S., Mahowald, L., Bleiweis, R., Graves-Fitzsimmons, G., & Zhavoronkova, M. (2021, November 7). The State of the LGBTQ Community in 2020. Center for American Progress. Retrieved November 23, 2021, from https://www.americanprogress.org/article/state-lgbtq-community-2020/.
- Ellis, S. K. (2019). GLAAD Accelerating Acceptance 2019 Executive Summary. GLAAD.
- Jones, J. M. (2021, November 20). LGBT identification rises to 5.6% in latest U.S. estimate. Gallup.com. Retrieved November 23, 2021, from https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx.
- Russell, S. T., Pollitt, A. M., Li, G., & Grossman, A. H. (2018). Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. Journal of Adolescent Health, 63(4), 503–505. https://doi.org/10.1016/j.jadohealth.2018.02.003
Additional resources:
- Schmidt, S. (2021, February 26). 1 in 6 Gen Z adults are LGBT. and this number could continue to grow. The Washington Post. Retrieved November 23, 2021, from https://www.washingtonpost.com/dc-md-va/2021/02/24/gen-z-lgbt/.
- Who Are We? Consortium. (n.d.). Retrieved November 23, 2021, from https://www.consortium.lgbt/intersex-inclusive-flag/.
Inclusive Care for Gender and Sexual Minorities
with instructor Brianna Durand, PT, DPT
When it feels overwhelming and nuanced, it can be tempting to avoid uncomfortable topics altogether. However, attendees for this course can expect to be gently guided into the sometimes confusing realm of gender and sexual orientation, and identity. This course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice. Although this course will cover pelvic floor physical therapy specifically, it is appropriate and useful for any medical professional as we all have patients in the LGBTQ+ community.
Molly O'Brien-Horn, PT, DPT, CLT is a pelvic health physical therapist in California. She is a teaching assistant with Herman & Wallace and will be acting as a TA in the upcoming remote course, Inclusive Care for Gender and Sexual Minorities. Molly is a Certified Lymphedema Therapist (CLT), an LSVT BIG Parkinson’s Disease certified therapist, a trained childbirth doula, and a trained postpartum doula. She is a member of the American Physical Therapy Association Section of Pelvic Health. She has experience in a variety of physical therapy settings, including pediatric oncology, school-based pediatrics, outpatient orthopedics, and wound care. Her passion, however, is working in the field of pelvic floor physical therapy with children, teens, and adults of all gender identities, all sexualities, and all ability levels. In her spare time, Molly enjoys doing yoga, hiking, and relaxing at the beach.
October is LGBT History Month. This annual occurrence is a month-long observance of lesbian, gay, bisexual, and transgender history, and the history of the gay rights and related civil rights movements. H&W is proud to offer courses for treating the whole patient across the gender and age spectrum. The remote courses featured in this blog are Inclusive Care for Gender and Sexual Minorities with instructor Brianna Durand, and Transgender Patients: Pelvic Health and Orthopedic Considerations with co-instructors Sandra Gallagher and Caitlin Smigelski.

Many LGBTQ+ individuals, drag artists, and cisgender and heterosexual persons engage in binding, tucking, packing, and padding for several reasons. These techniques can be life-changing. Many people use these techniques for gender expression, but they can also be used for gender affirmation.
Gender dysphoria occurs when an individual feels distress due to a mismatch between their assigned gender at birth and their own gender identity. For many folx who are transgender, non-binary, queer, or intersex, these practices help reduce gender dysphoria. Instead, they provide feelings of gender euphoria by creating joy, enhancing mental well-being, and improving quality of life through affirming gender identity. Additionally, these methods can provide safety by helping to protect folx in unsafe and unfamiliar environments. Some of these devices, such as packers, can even be used for sexual function and urination
So how does it all work? Binding is when a person wears a device, called a binder, to flatten or minimize the appearance of their chest. Many folx who identify as transmasculine and non-binary engage in binding. However, not all people who bind identify as transmasculine or non-binary. For example, cis and queer women, and cisgender men with gynecomastia may use binders. Also of note, not all people who bind use the same binding methods. Compression shirts and tops, sports bras, and tape are a few examples of the many different binding methods available.
Conversely, padding can be used to enhance the shape and appearance of one’s body, often at the hips and gluteal regions. Padded bras can also be used to enhance breast size and shape. Many transfeminine, queer, intersex, non-binary, and cisgender women often use some form of padding or shapewear devices to help create a more effeminate silhouette. Drag artists often use some form of padding to modify their appearance for their performances to achieve the optimal look for their drag persona. Transmen and cismen can also use padding. Furthermore, wigs and prosthetics (e.g. silicone breast forms, breastplates, and prosthetic vaginas) can be used by these populations to achieve a desired appearance.
Regarding prosthetics, many transmasculine folx, cisgender men, intersex folx, and queer individuals use prosthetics for packing. When someone packs, they use a phallic-shaped device to enhance the prominence of their genitals, often to create the appearance of a bulge in their pants. Some packers can extend the length of a phallus for sexual play, as well. This can be helpful for transmasculine folx post metoidioplasty, intersex folx who may have anatomical differences in sexual or reproductive anatomy, as well as cisgender men who suffer from erectile dysfunction. Packers are often made of silicone and can also include or not include certain features like pubic hair, moveable foreskin, and testes. However, packers don’t have to be made of silicone and can instead be made from other items, such as a pair of socks. They can have multiple functions and be used for things other than packing, such as standing for urination, sexual pleasure for oneself, and sexual pleasure for partners.
While packing increases the prominence of one’s genitals, tucking, conversely, is used to minimize the prominence of external genitalia by creating a flatter appearance between the legs. This act gets its name from the tucking of one's testicles into the inguinal canals, after which the penis and scrotum are then tucked between the legs back towards the anus. Frequently gaffs, tape, or tucking underwear are used to maintain the genitalia in these positions. Tucking is commonly used by transfeminine, non-binary, and intersex persons. However, tucking is not just limited to these groups, as cismen, drag artists, and other populations can tuck also.
While binding, packing, tucking, and padding have many positives, there can be some inherent drawbacks. For example, tucking can increase the risk of Urinary Tract Infections due to the position of the urethra close to the anus. Binding can alter posture and impact breathing by reducing diaphragmatic and rib mobility. Pads can be uncomfortable and hot, while packing devices, Stand-to-Pee devices, in particular, require regular cleaning to prevent unwanted smells and/or infections. All of these practices carry the risk of skin breakdown or irritation if performed too frequently or with improper technique. However, it is important to remember that even with these and other various drawbacks, these acts can be so lifesaving, gender-affirming, and life-protecting for many folx, that at times, the benefits of performing these practices greatly outweigh the risks.
The ins and outs of binding, packing, tucking, and padding can be quite complex, and there is so much to learn about proper usage and technique.
Want to learn more about these and other things related to LGBTQ+ health? Check out these remote course options:
- Inclusive Care for Gender and Sexual Minorities, Brianna Durand and her TA Molly O'Brien-Horn will dive deeper into these and other topics surrounding LGBTQ+ healthcare to educate pelvic health practitioners on how to provide better, safer, and more skilled care for the LGBTQ+ populations.
- Transgender Patients: Pelvic Health and Orthopedic Considerations, co-instructors Sandra Gallagher and Caitlin Smigelski will expand your skills for working with people of all gender identities. This course includes particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
What are you waiting for? Sign up and join us today!