HW is excited to announce the addition of a brand-new course to our Pelvic Function (PF) Series!
Pelvic Function Level 2C (PF2C): the Male Pelvic Floor and Men’s Pelvic Health
Formerly the stand-alone course, Male Pelvic Floor Function Dysfunction and Treatment, this course is now being adapted and reformatted to be a part of the PF Series, reflecting the inclusive stance of H&W core series instructing in the care of all patients. This course is intended for the pelvic health clinician who treats patients with conditions including post-prostatectomy urinary incontinence, erectile dysfunction, and chronic pelvic pain (CPP).
This course will be offered as satellite, self-hosted, and in-person options in order to provide the most flexible pathway for participants.
It is a reality of our field that pelvic rehab evolved from a tradition of “women’s health physical therapy”, and that is reflected in the prior vulvovaginal emphasis of the existing coursework. As the scope of pelvic rehab has expanded to encompass men’s health and care for all genders, it is important that all pelvises be incorporated at every level of our series, and that men’s health be a foundational part of our curricula, rather than being siloed as a specialty offering.
It is now our expectation that providers who want to care for patients around topics provided in the men’s health course will now take our introductory course, Pelvic Function 1. This is a necessary change reflecting growth and progression of our field of pelvic healthcare. Over the years, it was helpful to offer a course focusing on post-prostatectomy dysfunction, pelvic and genital pain and sexual health and function that was open to all levels. However, while participants who took the former Male Pelvic Floor course developed competence in the instructed skills, by missing the rest of the series, foundational conversations including physiology of urinary function, discussion of trauma-aware care, and bowel health basics that often affect other pelvic functions were abbreviated. Including men’s health within the rest of the foundational series resolves the missed content from our foundational course. Attendees to our PF1 course will find that it has been elevated to be a more inclusive course that covers information about pelvic health which will allow a beginning pelvic health practitioner to immediately apply introductory principles of care to all genders.
More questions about changes to the PF series? Please see this FAQ page: https://hermanwallace.com/frequently-asked-questions#2024-PF-Series-Update

Within the walls of the pelvic rehabilitation clinics, we often hear more intimate details than we ever imagined we would, could, or perhaps should. With increasing patient care experiences, most therapists demonstrate increased knowledge, awareness, and with some practice, increased skill at discussing sensitive issues such as sexuality. Every person and relationship is unique and we are sometimes asked questions by our patients such as "Should I be having more sex?" or "Am I normal?"
I have sometimes been surprised when a patient reports that he or she is "not having sex often enough" and for that patient it means that daily sexual activity is no longer happening. Other patients are quite satisfied with their sexual activity occurring 2-3x/month. We meet patients who have gone for years without engaging in sexual activity, perhaps because of pain, or lack of intimate partnership, or medical issues with a partner. It is very useful to avoid having expectations for what we as therapists think a patient should or should not be doing, whether that pertains to a particular sexual practice or to a level of involvement with a partner.
-Holly Tanner. Sexuality and the Older Patient. Tuesday, 13 September 2011.
Herman & Wallace offers several course options that deal with these sexual topics. Those courses that have upcoming course dates are:
Enjoy a 10% discount on these 3 courses if you register between now and midnight Wednesday, December 6th, 2023 with coupon code: SEXED10
Application Fee: $375.00 Experience Level: Beginner Contact Hours: 12
Course Date: December 9-10, 2023
It is vital that providers working with pelvic floor concerns have the necessary education and training to work with patients on issues of sexual dysfunction. It is also important that providers be aware of their own biases and be introduced to the various sexual health resources available to providers and patients.
Sexuality is core to most human beings’ identity and daily experiences. When there are concerns relating to our sexual identity, sexual health, and capacity to access our full potential, it affects our quality of life as well as our holistic well-being. Working with folks on issues of sexual health and decreasing sexual dysfunction encourages awareness and encourages healing. Imagining a world where human beings don’t walk around holding shame or traumatic pain is imaging a world of health and happiness.
Often unwanted sexual pain goes unaddressed. Why? Because we are not taught about the interactions between feelings, relationships, and our body. We are not taught that sex should not be painful; that pain is (likely) our body giving us information that something is going on (Hello crappy sex education and the stigma of sexual health and body awareness!). It’s not uncommon that most people who experience sexual pain often feel they are broken.
How to heal from unwanted sexual pain? There’s a trifecta! Effective healing comes from working with a sex-positive medical provider, sex therapist, and pelvic floor therapist. We will all collaborate!
Sex is not supposed to be painful. You are not broken.
Sexual Interviewing for Pelvic Health Therapists is two day course, written and instructed by a Licensed Marriage and Family Therapist and AASECT Certified Sex Therapist and is intended for pelvic rehab therapists who want to learn tools and strategies from a sex therapist’s toolkit. Lecture topics include bio-psycho-social-spiritual interviewing skills, maintaining a patient-centered approach to taking a sexual history, and awareness of potential provider biases that could compromise treatment. Labs take the form of experiential practice with Bio-Psycho-Social-Spiritual-Sexual Interviewing Skills, case studies and role playing.
Upon completion of this course, participants will be able to provide a Comprehensive Sexual Health Interview, recognize potential biases when working with patients, identify ethical considerations, and effectively collaborate with behavioral health providers upon referral. This course is intended for participants in the medical profession who work with patients experiencing pelvic pain, pelvic floor hypertonicity, and other pelvic floor concerns.
-Mia Fine. Pain during sex? It might be Dyspareunia. Tuesday, 18 May 2021.
Application Fee: $275.00 Experience Level: Beginner Contact Hours: 9.75
Course Date: January 7, 2024
CASE STUDY: Sarah is a 23-year-old woman who presents to your office for an evaluation. Upon scheduling, she did not wish to disclose to your office manager what kind of pelvic health issue she wants to be seen for.
Upon patient interview, Sarah reveals that she has been married for 8 months and all attempts at intercourse have been unbearably painful. She reports a 14/10 on a pain scale and that she has vocally cried out in pain with any attempts at penetration. She is feeling hopeless that this will ever get better, and is concerned that something is wrong with her and that her vagina is “too small” for intercourse. Sarah admits that she has never examined her own vaginal opening or seen it in a mirror because it “grosses her out”.
Sarah is otherwise in good health but has never had a gynecological exam. She and her husband are both from a conservative religious background and were educated in religious schools with limited sex education, and were provided with little information about sex prior to marriage. Neither of them had been sexually active prior to marriage. Sarah currently ascribes to her religious beliefs and practice which prohibits any conversations about sex with anyone other than her partner. She expresses an aversion to sexual activity and to her husband’s genitalia and semen. Sarah confides that she feels guilty that she is not able to have intercourse and “make her husband happy”.
Although she denies any discomfort with sitting or wearing tight-fitted garments and has no other pain in her body, recently she has started to have pain in her vulvar area that starts before attempting intercourse. After attempts at penetration, she has difficulty falling asleep due to her pain.
She has a self-diagnosed “tiny bladder” and frequently has to urinate every hour. Sarah reports a long history of constipation, with bowel movements about once a week with straining (type 1-2 on the Bristol stool scale)
She reports regular periods, but excruciating pain the first 2-3 days that can be debilitating at times. She has never successfully inserted a tampon.
Sarah’s personal goals for treatment are:
- To have intercourse without pain
- To become pregnant as soon as possible, as is expected in her social circles and close-knit community
- What is your next move?
- What other questions would you like to ask this patient?
- What would your treatment plan look like for this patient?
- What other healthcare providers might you refer her to?
Sex and Religion has the following goals:
- Demonstrate a foundational understanding of the traditions, customs, laws, and values associated with different faiths.
- Identify potential challenges and barriers to care unique to pelvic health patients from conservative religious backgrounds.
- Describe five strategies for increasing comfort and confidence in interfacing with patients from different religious backgrounds.
- Patient interview and education techniques.
- Discuss collaborative approaches to evaluation and treatment that are compliant with the patient’s religious and cultural norms.
- Evaluate culturally sensitive intervention in a case study format with your peers.
As pelvic health providers, we go into this special field with the desire to provide the best care for our patients in the most sensitive way possible. It can be particularly daunting when we encounter patients from religious backgrounds and cultures that are unfamiliar to us. In our attempts to be sensitive, we may be tempted to shy away from asking patients the questions that really need to be asked. We may avoid providing patient education we may have otherwise provided because we don’t want to offend, or may tiptoe around a treatment session where we may have otherwise taken a more confident approach. My hope is that practitioners will leave my course Sex and Religion confident in their abilities to provide the highest level of care with confidence, sensitivity, and compassion for all of their patients.
-Rivki Chudnoff. A Case Study in Cultural Sensitivity. Friday, 14 April 2023
Application Fee: $450.00 Experience Level: Beginner Contact Hours: 15
Course Date: January 20-21, 2024, June 15-16, 2024, and October 19-20, 2024
Anatomical information centralized around the medical field has been historically male-dominated, affecting how the world discusses and understands anatomy and their bodies even in the current day. In 2005 Wade, Kremer and Brown ran a study on college students and found that 29% of women and 25% of men could not identify the clitoris on a diagram of the vulva. We need to revolutionize female sexuality in general, change the focus from the linear model where penetrative sex and orgasm are the focus as it’s been traditionally taught.
The full clitoris goes far beyond the crown which is the external tip. The clitoris actually extends several inches into the body where it branches into a shape similar to a wishbone. I want to share a description that I love from Latham Thomas, “It’s all this amazing erectile tissue that wraps around, and it all engorges when it’s stimulated. Pound for pound, if you have a vulva, you actually have the same amount of erectile tissue that people with penises have, but it’s just internal.” These clitoral legs are responsible for the sensations where the front wall of the vagina connects to the paraurethral glands (the G-spot) and for female ejaculation.
I authored the Herman & Wallace Sexual Medicine in Pelvic Rehab course for practitioners to have a platform to learn proper anatomy, identify misconceptions, and understand that sexuality is circular with satisfaction as the focus. With the understanding of ‘normal’ anatomy and function, we can help our patients with sexual dysfunctions return to a healthy sexual lifestyle.
Sexual Medicine in Pelvic Rehab is a two-day, remote continuing education course designed for pelvic rehab specialists who want to expand their knowledge, experience and treatment in sexual health and dysfunction. This course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions for the gender and sexual spectrum, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, female squirting, G-spot, prostate gland, female and male sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm. Other topics include the function (and specific dysfunction) treated by physical therapy in detail including: vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post-prostatectomy; as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.

Aparna Rajagopal, PT, MHS, WCS, PRPC, Capp-OB Certified, and Leeann Taptich DPT, SCS, MTC, CSCS co-authored the course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Assessment of both static and dynamic posture is something we are taught very early on in physical therapy school. Posture and postural deviations have been shown in the literature to have a direct correlation to pelvic floor function and dysfunction. Multiple EMG studies have demonstrated that foot/ankle position can influence pelvic floor activity and that there is increased pelvic floor activity with the ankle positioned in dorsiflexion.(1)
Similarly, increased thoracic kyphosis and decreased lumbar lordosis can increase the likelihood of developing pelvic organ prolapse by influencing intra-abdominal pressure and causing extra pressure on the pelvic floor. Postural deviations far away from the pelvic floor can also affect the pelvic floor. Rounded shoulders and forward head posture are common findings during our assessments. Shoulder protrusion is a common finding in chronic pelvic pain patients.(1)
Education about posture during Activities of Daily Living by itself can lead to significant improvement in Pelvic floor muscle power, and endurance.(3) Understanding myofascial connections, is a small start in understanding how/why some of these things occur. The myofascial connections from the Thoracolumbar fascia connect the pelvic floor muscle to the sacrum and the neck.(2) It also connects the Gluteals, the Latissimus dorsi, and the External Obliques to the pelvic floor.(2) Optimal functioning of the pelvic floor depends on the entire chain of the musculoskeletal system. 2 Incorporating a full body assessment including the myofascial system is important in treating patients with pelvic dysfunction.
In the Breathing and the Diaphragm course taught by Aparna Rajagopal and Leeann Taptich, various commonly seen postures, thoracic mobility and how it relates to these postures, as well as all the myofascial connections to these postures will be discussed. The implementation of a regional interdependence model is discussed to ensure a holistic assessment and treatment plan. Join them on December 9 and 10, 2023 to learn more about posture, breathing, and the pelvic floor.
References:
- Zhoolideh P, Ghaderi F, Salahzadeh Z. Are There Relations Between Posture and Pelvic Floor Disorders? A Literature Review. Crescent Journal of Medical and Biological Sciences. 2017; 4(4): 153-159.
- Tim S, Mazur-Bialy AI. The Most Common Functional Disorders and Factors Affecting Female Pelvic Floor. Life. 2021; 11: 1397. https://doi.org/10.3390/life11121397.
- Jorasz K, Truszczynska-Baszak A, Dabek A. Posture correction therapy and pelvic floor muscle function assessed by sEMG with intravaginal electrode and manometry in female with urinary incontinence. Int J of Environ Res and Public Health 2023;20:369. Doi:10.3390/ijerph20010369.
Breathing and the Diaphragm
Price: $450.00 Experience Level: Beginner Contact Hours: 14 hours
Course Date: December 9-10
Description: This remote continuing education course is presented live on Zoom and is designed to expand the participant's knowledge of the diaphragm and breathing mechanics. Through multiple lectures and detailed labs, participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes.
As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi-component system that works together. Optimal function of the diaphragm and breathing patterns are key to a healthy pelvic floor, a normal functioning core, and postural stability. Evidence-based methods to assess the diaphragm and breathing mechanics are presented along with easy-to-apply practical intervention strategies.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. The assessment concepts and treatment techniques can easily be integrated into a therapist's current evaluation and intervention strategies.
The course information is applicable to patients who present with Diastasis Rectus Abdominis, pelvic pain, incontinence, prolapse, cervical/thoracic/scapular/ and lumbar pain. In addition, current literature has shown that these breath and diaphragm training techniques can effectively improve athletic performance in Labs will be demonstrated and will be participatory where possible.
Participants may practice labs on a family member or friend or team with a fellow participant where possible.

The upcoming Modalities and Pelvic Function course is a collaboration of different faculty members working to bring participants the information they have been asking for about modalities, ever since COVID forced a shift in Herman & Wallace's course format. This is a two day, in-person, hands-on course, created to be a very research based and intervention heavy learning experience for participants.
The majority of the in-person learning is interactive or lab based with the lectures being primarily focused on how to apply these modalities to clinical experiences and practice. If you can think of a modality, it is probably mentioned, if not practiced or sampled during this class. You can check out the schedule for an extensive list of all of the modalities included in this class. If there was a modality that could not be experienced as a group, there are interspersed expert interviews reviewing those concepts.
This class is for all types of learners and will definitely meet the needs of people missing in person learning opportunities. Because this class is so lab focused, hands-on and has so much equipment involved, there will only be a few offerings with small in person class sizes.
From the Desk of Holly Tanner (Director of Education)
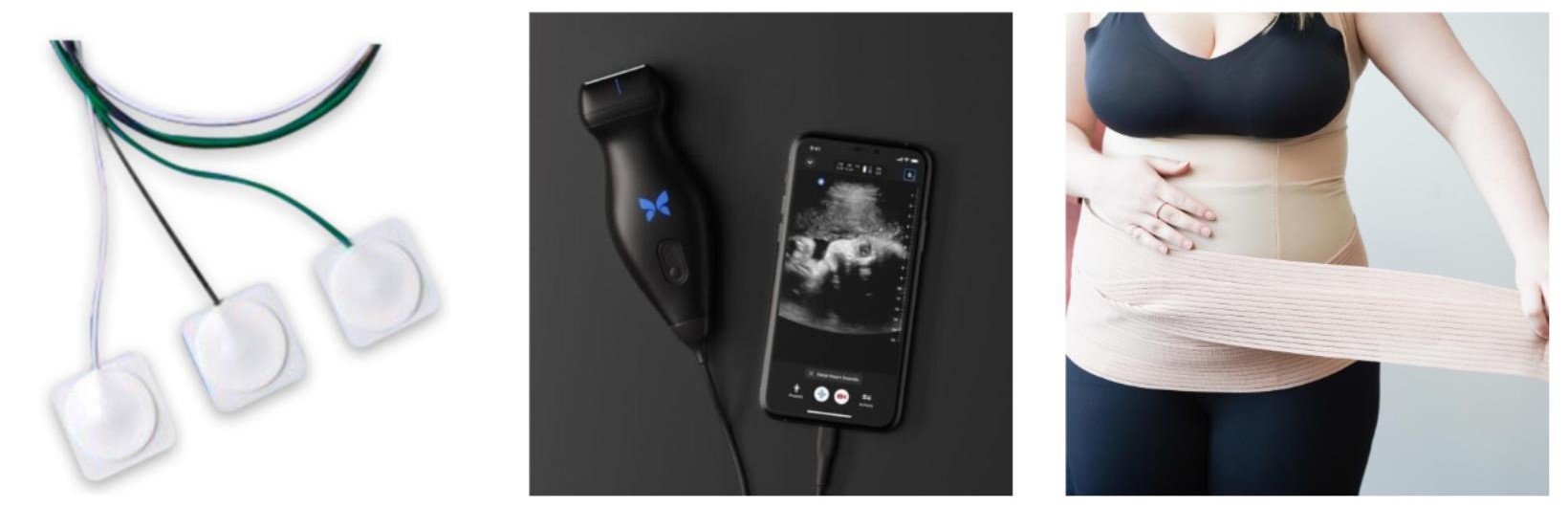
One of the course content pieces that was left out of the Zoom world transition in our popular Pelvic Floor Level 1 course that introduces participants to the world of pelvic health has been our usual modalities focus, namely that of surface electromyography (sEMG) training and electrical stimulation. For the right patient, these tools are efficient and effective; the equipment is also difficult to ship to multiple Satellite locations around the country. Herman & Wallace is thrilled to announce that not only have we solved this issue, but designed a way for clinicians to learn about dozens of modalities in an environment that allows the clinician to move beyond theoretical and soundly into the practical delivery of a variety of technologies and tools.
The new Modalities and Pelvic Function course answers the clinician’s need to understand how to choose and access the right tools both for in-clinic care and for patient self-care application. While biofeedback and electrical stimulation are covered in this course, so are introductions to understanding tools such as shockwave, dry needling, real time ultrasound, laser, and electrotherapies. With hands-on lab time, and learning modules grouped into tools specific to pelvic health conditions such as bowel dysfunction, sexual health challenges, practitioners will have the opportunity to trial a variety of tools and applications that previously may have only been available as an image in a presentation.
Current Medical Technologies will be in-person with us as we design this learning experience and will be available to answer your questions about products and clinical set-up. The interactive environment has been designed to be stimulating and allow the clinician to apply a variety of learning strategies including tactile opportunities to try things on themselves or a lab partner. This is a unique course that provides foundational understanding of technology and tools, clinical practice research and recommendations in an in-person environment. Many equipment providers have been generous in providing sample products for trial and even some giveaways to take home! We believe this modalities course is so foundational to our skillset in pelvic health that we almost put into our core pelvic function series lineup. If you’re wondering “when should I take this course?” the answer is “as soon as you can!” The only pre-requisite for this course is having taken one entry-level pelvic health course that instructs internal pelvic health examination.
Price: $645.00 Experience Level: Intermediate Contact Hours: 18.5 hours
Course Dates & Locations Coming Soon!
Now Seeking New Hosts!
Herman & Wallace is excited to announce that beginning in 2024, we will be offering our Pelvic Floor Series courses with in-person instruction.
This means that we are seeking hosts who are interested in having a faculty member come to their location to teach one of the following courses:
- Pelvic Function Level 1
- Modalities and Pelvic Function
- Pelvic Function Level 2A/2B/2C
- Dry Needling and Pelvic Health
If you are in a densely-populated area and have a space that can accommodate 36+ course participants and are interested in hosting an in-person event, please review the information at https://www.hermanwallace.com/host-a-course and let us know!
For those with slightly less space, we are actively seeking hosts for courses offered in the Satellite Lab format. Satellite lab courses use video conferencing to allow smaller groups around the country to learn under the direction of local lab assistants. If you would like to host a satellite, and have space for 16+ course participants, visit https://www.hermanwallace.com/host-a-course to get in touch.
Thank you to author Serra Shelton, SPT for sharing her article with the Pelvic Rehab Report. You can find Serra's original article published on the Empower Physiotherapy website: https://www.empower.physio/blog-all/aghx7wyg00seoe5ylk5mh3gadvr1a7. You can learn about making your practice more inclusive and comprehensive in Brianna Durand's upcoming course, Inclusive Care for Gender and Sexual Minorities, scheduled for December 2-3, 2023.
I am a 2nd year physical therapy student about to start my clinical rotations, and I have been interested in pelvic floor PT since the beginning of my academic journey. However, since it is a somewhat niche specialty, my general coursework provided only 2 lectures on pelvic floor therapy in the entire program. Despite seeking out exposure to pelvic floor education in other ways, such as taking a courses with the Herman & Wallace Institute and a pelvic health elective at the University of Washington, I wanted to learn more than the brief glimpse I had seen so far—and that is how I found myself creating an independent study course with Dr. Brianna Durand, an LGBTQIA+ pelvic floor/outpatient orthopedic physical therapist. Let me give you a sense of what this experience was like.
It was the first day of my independent study in which I would shadow Brianna as she practiced.
We started off the day with a returning patient, and Brianna began by asking for updates on her symptoms. As the patient recounted her status since her last session, Brianna typed away at her computer, asking for more details here and there.
When the patient had finished, Brianna turned away from her computer, made eye contact, and said “So to recap, since our last session you had a nasal endoscopy with negative findings, you saw an endocrinologist for the first time who ordered new tests, you had another biopsy, and you had a particularly stressful week at work.” The patient nodded emphatically. I was impressed—
I had never observed a physical therapist summarizing the patient’s words back to them. It seemed like a simple yet highly effective technique for the patient to feel fully seen and heard, and to make sure no important information had been missed.
Brianna sat back in her chair, her expression concerned, and said, “It sounds like you’ve been through an incredible amount of medical stress since our last session. No wonder you weren’t able to stick with your home dilator schedule.” The patient nodded even more, and I raised my eyebrows in surprise— we had talked about the importance of empathizing with the patient’s emotions in classes, but this was the first I had seen it in action.
“Here’s my plan for the session,” Brianna continued as she listed off the types of interventions she wanted to do that day, and why. Finally, as the icing on the cake, she added “are there any things you would like to address with today’s session?”
I was awestruck.
It was new for me to watch a physical therapist outline the exercises they planned to do with the patient prior to the session, explain the clinical reasoning behind them, and encourage the patient to contribute.
It was a beautiful way to give the patient agency over their treatment and allow them to give true consent to the session, rather than being herded from one exercise to another with little explanation, as I had been trained to do so far.
As I watched Brianna treat several more patients that day, I realized that this type of care was not isolated to the first patient, and was applied to pelvic floor and orthopedic patients alike. Every session I noticed her repeating back the patient’s subjective, validating any strong emotions the patient might be feeling, outlining the planned treatment session, and asking for input. This was simply her standard of care for everyone who walked through her door, and I was impressed by the skill and care with which she executed it.
I think Brianna delivers such consistently exceptional patient care in part because of her training in pelvic floor physical therapy.
Due to the sensitive nature of that body region, pelvic floor physical therapy faces the practitioner with some of the most vulnerable, traumatized, ashamed, and fearful aspects of the patient’s life.
From what I have seen so far, the specialty has evolved to meet the needs of its patient population by leaning into gentleness, empathy, deliberateness, and a return of agency to the patient in a way that the wider world of physical therapy could benefit from. For example, one lecture from a pelvic floor elective class I took discussed consent and trauma-informed care more thoroughly than all the rest of the two years of my program combined.
Additionally, a Herman & Wallace Pelvic Floor class I attended last spring went in-depth into exam strategies to give the patient more agency and how to build comfort for saying “no.” The instructors counseled us to use these strategies with all of our patients, whether we are aware of a trauma history or not, because every pelvic floor patient benefits from this level of thoughtful care. I would take it one step further, and argue that every physical therapy patient in any setting or specialty benefits from this type of communication and care.
I think pelvic floor physical therapy should be included more in the core curriculum of physical therapy doctorate programs.
The philosophy behind pelvic floor care would improve student’s abilities to engage with difficult patient experiences, whether they practice pelvic floor therapy after graduation or not. Experience of trauma is not limited to the pelvic region, and any instance where someone’s body is touched against their will can create a traumatic experience.
We do not know if something seemingly harmless, such as a tactile cue to the low back, could cause a patient to feel out of control of the situation or bring back traumatic memories. I have often wondered this as I watch the way our profession tosses exercises at patients, thrusting weights and straps into their hands, bundling them onto a machine before explaining what the machine does, correcting and poking and instructing with little respect for the incredible trust it takes to allow yourself to be touched by a stranger. Could we take the time to be more thoughtful about the dynamic we create with patients? Would we see better health outcomes if we did?
I first became interested in pelvic floor physical therapy before applying to graduate school, when trying to connect myself with the community of queer physical therapists in my area. Not surprisingly, many of the LGBTQIA+ therapists I networked with were also pelvic floor specialists.
Because the genital region is the site of so much social, medical, and political trauma for those of us who are sexual and/or gender minorities, I think there is a desire to provide the type of safe, sensitive medical care to our community that we have struggled to find ourselves, to be one provider not adding to the horror stories our queer friends come home with every time they visit the doctor.
I believe that because of our insertion of ourselves into this specialty, the pelvic floor world has adapted to inclusivity in ways the rest of the physical therapy field is still struggling to catch up to. If you are treating a shoulder, you can culpably ignore the lived gender experience of your patient; however, if you are examining their pelvis, you cannot so easily bury your head in the sand. The difference has been stark in my experience as a student—within the general anatomy courses of my program, professors struggled and resisted using gender-neutral anatomical terms and persisted with language such as “male anatomy” and “biologically female,” despite widespread student protest.
From the first moment of my Herman & Wallace Pelvic Floor Level 1 course I took last spring, however, the instructors all consistently used gender neutral language such as “pregnant people” and “pelvis containing a penis” without fuss or fanfare. It was enough to make me want to weep with joy, to see how possible it was to have an inclusive and non-gendered medical education. The same experience was repeated later that year, when I took a pelvic floor elective as part of my second year coursework—even though my other coursework at that institution had no policy on inclusive language, the professors of this one elective course made a point of using gender neutral anatomical language throughout.
This is another huge gift that the pelvic floor community has to offer the wider field of physical therapy—an honest look at the impact our current medical language has on LGBTQIA+ patients, and how we can shift our teaching styles to do less harm. I think if pelvic floor physical therapy were more integrated into physical therapy core curriculum, we as a profession would become better healthcare providers to LGBTQIA+ patients across every physical therapy setting.
The nine weeks I worked with Brianna was an eye-opening experience.
She demonstrated a type of patient-centered care that I hope to emulate in my own career. I was reaffirmed in my reasons for being drawn to pelvic floor physical therapy, and gained a new appreciation for what pelvic floor physical therapy skills will add to my quality of care, across all settings and all patients I treat.
I was able to have vulnerable conversations about providing the best possible healthcare to members of my LGBTQIA+ community, and discuss queer-related patient care questions with her that professors at my program do not know how to address. I appreciate that doctorate programs are already intense educational experiences with little room to add to the curriculum, but in this case I think it is crucial for pelvic floor physical therapy to become a larger part of the core curriculum. It’s not just a matter of exposing students to a potential niche specialty, it’s about integrating a style of practice that will change the culture of our field of physical therapy to one that is more patient-centered, inclusive, empathetic, and intentional.
Inclusive Care for Gender and Sexual Minorities
Price: $495.00 Experience Level: Beginner Contact Hours: 15.5 hours
Course Date: December 2-3, 2023
Description: As healthcare providers, we often want to provide compassionate, well-informed, healing care that addresses the patient in their entirety. While many have taken active steps to be more inclusive and comprehensive in their treatment, it can remain a daunting task where one is uncertain where to begin. This 2-day online course is packed full of clinically relevant and applicable information designed to help those who are striving to reframe their understanding of sex and gender.
Participants will gain up-to-date, in-depth knowledge of the various terminology used by and relating to LGBTQ+ individuals. They will also acquire an understanding of the social, economic, psychological implications on the health of this community. This course will emphasize clinical interactions, currently available research, and professional accountability.
When it feels overwhelming and nuanced, it can be tempting to avoid uncomfortable topics altogether. However, attendees for this course can expect to be gently guided into the sometimes confusing realm of gender and sexual orientation and identity. This course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice. Although this course will cover pelvic floor physical therapy specifically, it is appropriate and useful for any medical professional as we all have patients in the LGBTQ+ community
Tina Allen, PT, PRPC has been a physical therapist since 1993 and has specialized exclusively in pelvic health in all genders and throughout the patient's life span for the past 28 years. She works at the University of Washington Medical Center in a multidisciplinary Pelvic Health Clinic where she collaborates with physicians to optimize patient recovery. Join Tina in her upcoming course Manual Therapy of the Abdominal Wall scheduled for November 18, 2023.
One option in our written documentation is to include information on pain, pigmentation, pliability, surface area, height, and patient-reported functional limits due to the scar. This can be time consuming and is difficult to replicate between sessions. As practitioners, we need to be able to show specific gains for insurance and to assist patients (and ourselves) in recognizing gains.
Did you know you can also utilize grading scales that originally were developed for usage with Burn survivors?
We could simply utilize a visual analog scale, but by using a scar assessment tool we can use one simple scale to quantify multiple factors affecting function for the patient. One such scar assessment tool is the Patient and Observer Scar Assessment Scale (POSAS version 2.0). The POSAS is free to access for clinical use and includes both a patient reporting form and a clinician reporting form.
Your patient can utilize the POSAS to report on their current experience of scar symptoms including location, pain presence, scar sensation and restrictions in movement/activity. While as the Clinician questionnaire includes rating from 1-10 regarding vascularity, pigmentation, thickness, relief, pliability, and surface area.
In the clinical environment, we often must justify our interventions with outcome measures, and to be able to add to the research supporting our interventions. In the case of scar management utilizing tools such as the POSAS goes a long way for us as rehab professionals.
Other scales include Manchester Scar Scale, The Stony Brook Scar Evaluation Scale and the Vancouver Scale.
Data from 2015 shows that 28% of pregnancies in developed countries end in C-section, and in April 2022 the American College of Surgeons reported that four-million abdominal surgeries are performed per year in the US. It is unclear why some patients develop painful scars or functional limitations from their scars, but those that do can benefit from Rehab Therapy interventions. Our rehabilitation skills in evaluation, movement education, and manual therapy can facilitate patients in their return to function.
By utilizing the above scales practitioners can assist with quantification of limitations while showing gains achieved from interventions.
Manual Therapy is a way for the clinician to manage tissue tension, holding patterns, and movement restrictions that have developed. Techniques learned in the foundational course, Manual Therapy for the Abdominal Wall, can be applied to the rest of the body and used as a building block for more specialized manual interventions. In the course we address observation and evaluation skills of the myofascial system including scar that assist the clinician in rating forms such as the POSOS scale. Participants in this course will learn to utilize the abdominal wall as a way to build and refine foundational skills of touch, loading, unloading and to address myofascial and functional restrictions.
References:
- https://www.posas.nl/.
- Deflorin, C., Hohenauer, E., Stoop, R., Van Daele, U., Clijsen, R., & Taeymans, J. (2020). Physical management of scar tissue: a systematic review and meta-analysis. The Journal of Alternative and Complementary Medicine, 26(10), 854-865.
- Olszewska, K., Ptak, A., Rusak, A., Dębiec-Bąk, A., & Stefańska, M. Changes in the scar tissue structure after cesarean section as a result of manual therapy. Advances in clinical and experimental medicine: official organ Wroclaw Medical University.
- https://www.facs.org/for-medical-professionals/news-publications/news-and-articles/press-releases/2022/machine-learning-and-patient-outcomes/.
Manual Therapy Allows a Patient to Move Better - An Interview with Tina Allen
Manual Therapy for the Abdominal WallManual Therapy for the Abdominal Wall
Price: $225.00 Experience Level: Beginner Contact Hours: 7 hours
Course Date: November 18, 2023
Description: This remote course is designed to provide an introduction to the basics of myofascial techniques and applying them to the abdominal wall. This course is intended for the pelvic rehab therapist who may be new to palpation and manual therapy techniques, or who wants to refine their skills of discriminate touch. These myofascial techniques can be utilized to assist with treatment of abdominal scars, endometriosis, IC/PBS and abdominal wall restrictions that impact pelvic girdle dysfunction.
Breast Cancer Awareness Month
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
October is breast cancer awareness month.
This is a great time to acknowledge all of the many individuals who have fought against this disease with such bravery and determination! If you have the opportunity to work with these patients, you know what an inspiration they are.
There are many factors that influence the development of breast cancer. From genetics, to environmental exposures, to hormonal influences, there is an abundance of information available to us. So much so that it can be overwhelming to sift through all of it, but it is not only the development of breast cancer that we have information on it is also how breast cancer influences the development of other cancers.
According to Cancer Research UK, having breast cancer in the past increases the risk for the development of gynecological cancers. The risk is higher in those individuals who were diagnosed at a younger age, and with estrogen negative breast cancer.1 In an article in Oncology NEWS International, some statistics were shared. The overall risk for development of ovarian cancer in breast cancer survivors is 1.30. This risk is higher if a patient was diagnosed prior to age 50, with the highest risk in patients that were diagnosed with breast cancer between the ages of 15 and 39.2 Not only is there an increased risk for ovarian cancer, but also for uterine and endometrial cancers.3,4 Especially if a patient was prescribed Tamoxifen in order to block estrogen in the body. The use of Tamoxifen may be used for up to 10 years after a breast cancer diagnosis to prevent recurrence. However, there is a risk of endometrial proliferation, endometrial hyperplasia, endometrial carcinomas, and uterine sarcomas with the use of Tamoxifen. 4
Many patients are bombarded with so many appointments concerning their diagnosis of breast cancer that their pelvic examinations are neglected. Since these patients do have an increased risk for the development of a second cancer and the development of a gynecologic cancer, we should educate our patients to continue to receive their annual pelvic exams. When you work with these patients, support them through their current recovery from a battle with breast cancer, but also encourage them to follow up with their wellness exams as well!
Herman & Wallace offers a series that can help prepare you for working with gynecological cancer patients. In Oncology and the Pelvic Floor Level 1 (OPF1) we cover general oncology. The course addresses cancer treatment, short-term side effects, long-term side effects, and learn rehab techniques to help these patients. Then in Oncology and the Pelvic Floor Level 2A (OPF2A) and Oncology and the Pelvic Floor Level 2B (OPF2B) we go more in depth with pelvic related cancers and in OPF2A we cover topics related to testicular cancer, prostate cancer, penile cancer, and colorectal cancers. In OPF2B we cover topics related to gynecological cancers and bladder cancer.
All three courses instruct hands-on treatment techniques to help patients recover function and feel better. Please join us by taking this series to be able to help these patients!
References:
- Cancer Research UK. (2022, Feb 28). Risks and causes of ovarian cancer. https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/risks-causes
- Breast cancer survivors at increased risk for ovarian cancer. (1999). Oncology NEWS International. 8(7). https://www.cancernetwork.com/view/breast-cancer-survivors-increased-risk-ovarian-cancer
- Li Z, Wu Q, Song J, et al. (2018). Risk of second primary female genital malignancies in women with breast cancer: a SEER analysis. Horm Cancer. 9(3): 197-204. doi: 1007/s12672-018-0330-0
- (2022). Tamoxifen and uterine cancer. ACOG Clinical, Committee Opinion. 601. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2014/06/tamoxifen-and-uterine-cancer
Menstruation and Pelvic Health
Have you ever wondered if there is something more you could do to help your patients understand and improve their Menstrual Experience? The Menstrual Cycle has an impact on the health and wellbeing of many of the patients we see as health care providers, and understanding this impact allows us to provide more effective care to our patients. Dr. Amy Meehan and I are excited to offer this informational, interactive, and engaging course designed to provide you with tools and experience to invite your patient to engage in a Menstrual Dialogue to discuss topics that can be challenging and sensitive with the goal of making real changes in their Menstrual Experience. We identify Menstrual Stressors and create an Individual Combination Menstrual Action Plan designed to improve the overall Menstrual Experience. We focus on non-hormonal, non-surgical, and non-prescription interventions to be carried out in holistic collaboration with a physician and other health care providers. Although there is much overlap among the topics of fertility, contraception, and menopause, we don’t focus on these because each is a course unto itself.
In pre-recorded video sessions, we review of anatomic, physiologic, and cultural aspects of the Menstrual Experience and provide clarity to complex biological processes. We discuss what is a ‘normal’ parameter for a Menstrual Cycle and what symptoms should prompt a visit to a physician. We explore interesting topics such as cultural Menstrual Milestones, Menstrual Concealment, post-Traumatic Cycling, envisioning an ‘Ideal Menstrual Experience’, and even identifying and celebrating positive aspects of the Menstrual Experience. We use provocative thought experiments to re-envision the Menstrual Experience in a more positive light. Some of these are It Takes a Village, If Men Could Menstruate, The Unapologetically Cycle-Friendly Wardrobe, and The Kindest Gift: A Better Menarche.
In the live virtual sessions, we demonstrate what to expect in terms of Menstrual Volumes on different days of a typical cycle. We demonstrate and discuss pros and cons, care and use, and absorptive and collective properties of multiple Menstrual Products: 1) liners, pads, interlabial pads (disposable and re-usable), 2) tampons (different absorbencies, shape when expanded, applicator vs no applicator), 3) cups and discs (insertion and removal techniques and maintenance), 4) period underwear (effective, comfortable, stylish, and fun options), 5) period overnightwear (to decrease anxiety about overnight flooding), 6) period activewear (effective, comfortable, stylish, sporty, and fun options for gym, yoga, and around town), and 7) period swimwear (one piece and bikini, for competition, or just chillin’ in the sun). We learn how to create a Flow Management Plan that combines multiple Menstrual Products in the most effective way for each day of flow. We use common kitchen items to simulate different kinds of vaginal discharge your patients may experience and know when to seek help from a physician. We explore Menstrual Tracking and Menstrual Diaries to increase Menstrual Mindfulness of internal cues to adjust nutrition, fitness, and lifestyle. Dr. Meehan shares her expertise in applying yoga and exercise techniques to alleviate Menstrual Symptoms and carry out high-performance cycling.
We hope the time we spend together in this course will give you tools to help your patients create 1) Menstrual Optimism: living in the belief that the present is full of possibility for a better Menstrual Experience, 2) Menstrual Confidence: the belief that you can participate in things that are important to you…on ANY day of the month and that your voice is important…on EVERY day of the month, and 3) Menstrual Pride: living with a deep feeling of satisfaction, happiness, and contentedness that your body is the way it is and that it works the way it does…despite the challenging aspects of the Menstrual Experience and because of the rewarding aspects of the Menstrual Experience.
We look forward to taking steps with you on this exciting Menstrual Journey.
Dr. Niko and Dr. Amy
Course Testimonial
The Menstruation and Pelvic Health course was very helpful in deepening my understanding on how to enhance pelvic health treatment during the different stages of a woman’s cycle.
The video lectures and the material provided were clear and easy to digest and the live zoom class provided additional important information.
I can definitely say that my daily practice has improved since taking this class.
-Martina
Application Fee: $575.00 Experience Level: Beginner Contact Hours: 19 hours
Course Dates: October 28-29, 2023
Description: This course is designed for clinicians who want to obtain an advanced knowledge and skills to educate patients on non-hormonal, non-surgical, and non-prescription interventions for improving the Menstrual Experience. Developed by Nicholas Gaffga, MD, MPH, FAAFP and presented together with Amy Meehan, PT, DPT, MTC, this course is geared towards the pelvic rehab provider looking to impart Menstrual Interventions that:
- Put control in the hands of people who menstruate to identify and carry out the interventions that are appropriate to them
- Use a holistic approach and advanced knowledge and familiarity with body and mind
- Emphasize healthy practices that can positively impact the Menstrual Experience and beyond, in areas such as mental health and chronic diseases
- Discover root causes of issues, rather than quick fixes, to have benefits that are sustainable across the lifespan.
Special thanks to faculty member Mora Pluchino, PT, DPT, PRPC, and Carole High Gross, PT, DPT, PRPC taking time during HWConnect 2023 to sit down and do this interview. Carole earned her Doctorate of Physical Therapy from Arcadia University in 2015, and her Master of Science in Physical Therapy in 1992 from Thomas Jefferson University, and earned her Pelvic Rehabilitation Practitioner Certification and enjoys working as a Pelvic Clinical Rehabilitation Specialist for Lehigh Valley Health Network. She is a Lead Teaching Assistant and instructor with Herman & Wallace. You can meet Carole in her upcoming course Eating Disorders and Pelvic Health Rehabilitation: The Role of a Rehab Professional scheduled for October 28-29, 2023.
Join Carole High Gross on October 28th to begin the journey to learn more about signs, symptoms, and the journey that individuals with eating disorders endure. Explore the ways pelvic health professionals can assist them on this journey in Eating Disorders and Pelvic Health Rehabilitation.
As pelvic health practitioners:
- We are NOT going to treat eating disorders.
- We are NOT going to diagnose eating disorders.
- We CAN and SHOULD be asking questions!
- Encourage patients to seek additional support, help them find appropriately trained providers.
- We CAN provide support and speak with words that promote validation, wellness, and healing rather than words that are unintentionally triggering, harmful or nonvalidating.
- We CAN provide these individuals with manual skills, activities, and educational “tools'' to assist in GI distress, constipation, abdominal bloating, urinary dysfunction, pelvic pain, sexual dysfunction, POP issues, postural / body mechanics, abdominal canister coordination/function, tightness in trunk, hips, shoulders, rib cage, etc.
These individuals would benefit from pelvic health professionals being an additional part (not the lead) of their treatment team. This course will provide an opportunity for Pelvic health professionals to:
- Appreciate and begin to understand the biopsychosocial complexity of eating disorders
- Understand how this mental illness creates serious and life threatening issues in body functions
- Understand our role as pelvic practitioners and what we can offer to provide relief or reduction in symptoms
Eating Disorders and Pelvic Health Rehabilitation will not have all the answers but rather will be a step forward for clinicians to expand their understanding and to seek out additional resources to learn more and provide evidence-based treatment for these individuals.
Course Testimonials

"This course was an eye-opener for me, and made me think back to patients who may have had eating disorders that I wasn’t aware of at the time. When healthcare providers think about eating disorders, we might think of a stereotype perpetuated by the media, and not realize that the patient in front of us, who doesn’t look like that stereotype, is in the throes of an eating disorder.
Worse, we may not realize that the words we use (even words and phrases that we were taught to use) can unintentionally cause harm to patients who are struggling with an eating disorder. Even if our patient discloses to us that they have an eating disorder, or we suspect that they do, what do we do with that important, sensitive information? How do we talk to them about it? How do we modify our treatment plan with them? How do we refer patients to the appropriate doctors, therapists, and dietitians?
This course has changed the way I think about and discuss fluid and fiber intake, abdominal bloating and cramping, constipation, and GI disorders with my patients, and has changed the way I educate patients on exercise, bowel and bladder habits. It has given me more confidence in having open, compassionate and vulnerable conversations with patients.
Not all eating disorders are alike. I work with many patients who have chronic illnesses, and after taking this class, I realized that Avoidant Restrictive Food Intake Disorder is prevalent in some of these populations.
This course gave me the opportunity to hear first-hand accounts from patients with eating disorders, how the medical system either harmed or supported them, and how skilled and understanding pelvic health providers, who were able to work with them non-judgmentally, changed their life for the better. Dr. Carole High Gross created this course not only to give pelvic health therapists an awareness of eating disorders, but to give us tangible treatment techniques including mindfulness techniques, breathing techniques, manual therapy techniques, and exercise interventions that we can use with this patient population."
~ Julia Kajen, PT, DPT, OCS
I attended the Herman and Wallace Eating Disorders and Pelvic Health Rehabilitation Course last year as I wanted to further grow my Pelvic Health expertise in working with teens and children. I am a certified Pelvic Health PT and have been treating Adults and children with pelvic health dysfunction for several years.
However, I was referred my first patient with an Eating Disorder so when I heard about this course I signed up right away.
Hands down, this has been the best course I have ever taken from Herman and Wallace.
Let me tell you why. This world of ED involves so much more than Physical Therapists and Physicians and Carole took the time to interview many other experts in the field and that was the mandatory pre course listening. It was a day full of exciting new learning, engaging me with a much bigger picture.
Because there are many more providers besides MDs involved with the care of these patients both before they come to us and while they are seeing us during aftercare, it is very important that we educate them about what a Pelvic Health Rehabilitation Therapist can do for their clients.
This has opened many new doors for me. These patients and their families need our expertise and I am very passionate about this new niche thanks to Carole’s education and her passion!
~ Carol Stillman, PT, DPT, PHC
CEO Sutton Place Physical and Aquatic Therapy
Certified Pelvic Health Therapist
Eating Disorders and Pelvic Health Rehabilitation

Price: $495.00 Experience Level: Beginner Contact Hours: 17 hours
Course Dates: October 28-29, 2023; April 6-7, 2024; October 19-20, 2024
Description: This course explores types of eating disorders including: anorexia nervosa, bulimia nervosa, binge eating disorder, ARFID (Avoidant Restrictive Feeding Intake Disorder) and OSFED (Otherwise Specified Feeding and Eating Disorder). We will also discuss conditions which do not yet have formal diagnostic criteria such as orthorexia and diabulimia and we will touch on Pica and Rumination Disorders.
Eating disorders are mental illnesses which manifest with physical complications which can be both dangerous and life-threatening. Eating disorders affect people of all ages, races, ethnicities, genders, shapes and sizes and do not discriminate. Individuals with eating disorders may or may not appear underweight and are often in larger bodies. Body size nor laboratory testing determine or confirm the severity of the dangerous consequences of the eating disorder. Specific causes of eating disorders are not clearly known, however, biological, psychological, and sociocultural factors contribute to the initiation and continuation of an eating disorder.
Many people have disordered eating patterns, however, nearly 1 in 10 will develop an eating disorder during their lifetime. Eating disorders are serious mental health AND physical illnesses characterized by highly distressing attitudes, beliefs and behaviors related to one’s food intake and in many cases body shape and weight. This results in associated distressing thoughts and emotions affecting physical, psychological and social function. Eating disorders included in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders: 5th Edition) are: Anorexia Nervosa (AN), Bulimia Nervosa (BN), Binge Eating Disorder (BED), Avoidant/Restrictive Food Intake Disorder (ARFID), Other Specified Feeding and Eating Disorder (OSFED), Unspecified Feeding or Eating Disorder (UFED), Pica and Rumination disorder. (psychiatry.org) .
Most health care professionals understand very little about eating disorders and disordered eating. There is a weight stigma with health care identifying “health” in terms of weight, BMI, body appearance, exercise and activity. As rehabilitation professionals, it is our responsibility to understand that health looks and feels different for everyone. In addition, we may be able to identify signs and symptoms of eating disorders and be able to provide support for these individuals through proper referral and modification of our rehabilitation plan of care.
Going one step further, pelvic / abdominal wall practitioners have a unique opportunity to work with individuals as they are experiencing GI distress, abdominal pain, abdominal bloating, bowel dysfunction (constipation or fecal incontinence), urinary issues, prolapse symptoms and pelvic pain. We also need to understand the impact of eating disorders has with pregnancy and during the postpartum time.
If we, as pelvic health providers, take the opportunity to listen and observe, we may be able to identify individuals of all genders who are struggling with disordered eating or an eating disorder which may or may not have been formally diagnosed. We have a specific skill set which has the potential to positively affect the abdominal, bowel, bladder and pelvic related symptoms - however, we may not be looking close enough into the causative reason for the dysfunctions.
Special thanks to faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC for writing this article. Jen began her career as a physical therapist at Spectrum Health in Grand Rapids, MI she has focused her professional attention on treating women, men, and children with pelvic health disorders since 2002. She has been faculty for Herman & Wallace since 2009 and loves to inspire other rehab professionals treating pelvic floor dysfunction. She is an author of the chapter, “Manual Therapy for the Pelvic Floor” which was published in the book, “Healing in Urology.”
To the physical therapists,
Do you remember what drew you to be a physical therapist?
Maybe it was a personal experience you had as a patient needing rehab after an injury?
Maybe, like me, you knew you wanted to go into medicine but the idea of being a doctor or a nurse didn’t quite fit?
Maybe you saw the power of physical medicine through a family member?
We all took different paths but ended up in the same place…a grueling college or university program where we challenged and pushed ourselves through semesters of anatomy, physiology, biology, chemistry and physics before we even got to curriculum that focused on all we would need to be excellent rehabilitation medicine providers. Then, said educational institutions deemed us WORTHY to go to hospitals and clinics to practice our new found skills, not just on each other, but on real people! How much did we get paid to perform these services? OHH nooo we didn’t get paid, in fact we had to PAY the university for this work expertise. We had clinical instructors who took the baton from our professors and refined our skills while helping us put our knowledge into practice.
But it all was worth it as we went out into the world and began our careers.
Some of us landed in our specialty of pelvic health right away. Some of us bounced around a bit before finding our pelvic passion! Some of us (me!) went kicking and screaming into our first pelvic rehab class, never expecting to fall in love. Regardless of our path, we all ended up here, in this diverse, unique, passionate and somewhat quirky family of pelvic health specialists!
Do you remember the first time you really made a difference for someone? The look in their eyes when they told you with complete and utter sincerity how much your care impacted their life? The words in the card and the feeling you had reading them? The flowers that were delivered? The taste of the homemade cookies someone made, just for you, just to say, Thank You?! Close your eyes right now, just for a bit, and reflect on the gratitude YOU have that the work you do has value and meaning. I think any and all rehab specialists have a treasured collection of these moments…but for us, the ability to hold space for healing in such a private, personal and sacred part of the body is incredibly powerful and unique.
Ahh, but there is also a flip side of this coin. The times when we are up at night thinking about that one person that presents a challenge to our skill set, clinical or interpersonal. The patients, families or situations that make us cry. The stories we wish we didn’t hear. The secondary trauma we face, that we didn’t realize we were signing up for and maybe weren’t equipped to handle.
As pelvic health physical therapists, we experience both sides of our profession. The joy and the pain, at times, in equal measure.
We put in long hours, work overtime, manage mounds of paperwork and emails. We are clinical staff, senior therapists, managers and supervisors. We are clinical instructors, college and university professors, researchers and political advocates. We work in hospitals, clinics, private practices, homes, rehabilitation centers, nursing homes, schools, for sports teams, for dance troupes, for circus performers and more. We specialize in pelvic health, but maybe we also have backgrounds or specialties in orthopedics, geriatrics, pediatrics, neurology, cardiopulmonary, pelvic health, inpatient care, sports rehab, cancer care, vestibular, aquatics, lymphedema, manual therapy, work hardening/conditioning and even more!
We interview, evaluate, assess, plan, execute, refine, redirect, prescribe, coach, motivate, understand, listen, cry and laugh. We use our brains, our hands, our bodies and especially… our hearts.
We are pelvic health physical therapists.
And this month we celebrate not just what we DO, but who we ARE.
Happy PT month!

Some benefits of gardening include:
- Fresh air
- Natural outdoor light
- Natural aromatherapy from plants
- Sensible sunshine exposure for vitamn D
- Relaxation and stress reduction
- Physical activity (squatting, bending, pulling, pushing, carrying)
- Improved hand dexterity and strength
- Develop friendships if performed in a group or community setting
- Growing your own natural fruits and vegetables for good health and sustainability
- Increasing fruit and vegetable intake
- Sense of purpose

Gardening helps you use your senses to hea your mind and body through:
- Touch – feeling the various textures of the plants and putting your hands in the soil
- Sight – seeing an array of colors
- Hearing – listening to the birds, rustling of the leaves or a backyard waterfall
- Smell – detecting the aroma from a variety of plants such as mint, rosemary, and basil
- Taste – enjoying the assortment of herbs in a salad or meal

Try growing the following in your backyard or greenhouse or in pots on your porch, balcony, patio, or windowsill:
- Fruits – apples, berries, grapes, plums
- Healing plants – aloe vera, lavender
- Herbs – basil, mint, parsley, rosemary
- Vegetables – cucumbers, tomatoes

Some precautions with gardening:
- Be aware of excess sun exposure
- Be aware that some individual who take certain medications may be photosensitive
- Be aware that some individuals may have seasonal allergies to pollens
- Be aware of insecticides and pesticides. Ideally, find natural alternatives
- Be aware of dehydration if outdoors for prolonged periods
- Be aware of heavy lifting and bending (especially for osteoporosis)

The following are selected studies relatiing to gardening:
- Improve health and well-being.
- A review by Howardth et al. (2020) found that “Gardens and gardening can improve the health and well-being for people with a range of health and social needs.”
- Reducing obesity and metabolic risk
- A study by Gatto et al. (2017) found that “LA Sprouts [a gardening, nutrition and cooking intervention] was effective in reducing obesity and metabolic risk…”
- Improved children’s fruit and vegetable intake.
- A systematic review by Savoie-Roskos et al. (2017) found that “…most studies suggest a small but positive influence of gardening interventions on children's fruit and vegetable (F/V) intake.”

Additional Resources:
- American Horticultural Therapy Association, http://ahta.org
- Bonsai Empire, www.bonsaiempire.com
- Bonsai Outlet, www.bonsaioutlet.com
- Green Exercise, www.greenexercise.org
- Japanese Gardening, www.japanesegardening.org
- National Gardening Association, www.garden.org
- North American Japanese Garden, www.najga.org
- Phipps Conservatory and Botanical Gardens, http://phipps.conservatory.org
- Therapeutic Landscapes Network, www.healinglandscapes.org
- Refer to the book Healing Gardens(Rawlings 1998).
- Refer to the book Healing Gardens: Therapeutic Benefits and Design Recommendations (Cooper-Marcus et al. 1999).
- Refer to the book Therapeutic Landscapes: An Evidence-Based Approach to Designing Healing Gardens and Restorative Outdoor Spaces(Cooper-Marcus et al.2014).

References:
- Rawlings R. Healing Gardens. Minocqua, WI: Willow Creek Press; 1998.
- Cooper-Marcus C, and Barnes M. (Eds.). Healing Gardens: Therapeutic.
- Benefits and Design Recommendations. New York, NY: John Wiley & Sons; 1999.
- Cooper-Marcus C, and Sachs NA. Therapeutic Landscapes: An Evidence.
- Based Approach to Designing Healing Gardens and Restorative Outdoor Spaces.
- Hoboken, NJ: John Wiley & Sons; 2014.
- Gatto NM, Martinez LC, Spruijt-Metz D, Davis JN. LA Sprouts randomized controlled nutrition, cooking, and gardening program reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatr Obes. 2017;12(1):28-37.
- Howarth M, Brettle A, Hardman M, Maden M. What is the evidence for the impact of gardens and gardening on health and well-being: a scoping review and evidence-based logic model to guide healthcare strategy decision making on the use of gardening approaches as a social prescription. BMJ Open. 2020;10(7):e036923.
Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management
.Price: $125.00 Experience Level: Beginner Contact Hours: 45 hours
Course Dates: November 18
Description: This continuing education course is targeted to physical therapists, physical therapist assistants and other rehabilitation professionals. Brief lectures will focus on the research and resources and labs will cover a toolbox approach for creating clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, expressive and art-based therapies, and the impact of nature on health. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis and self-massage.
This course was written and developed by Ziya “Z” Altug, PT, DPT, MS, OCS, a board-certified doctor of physical therapy with 32 years of experience in treating musculoskeletal conditions. He utilizes lifestyle and integrative medicine strategies in his clinical practice and is the author of Integrative Healing: Developing Wellness in the Mind and Body (Cedar Fort, Inc, 2018). Z Altug is member of the American Physical Therapy Association and American College of Lifestyle Medicine. He has taken workshops in yoga, Pilates, tai chi, qigong, meditation, Feldenkrais Method and the Alexander Technique. types of shockwave devices, and what
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./