Mora Pluchino is instructing her ethics course, Ethical Considerations from a Legal Lens, which is scheduled for June 3, 2023. This remote course covers ethical considerations from a legal lens for professionals working in the area of Pelvic Health. Health Care Professionals have many day-to-day ethical considerations to “do no harm” including basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges, and the legalities of pelvic health can add further complications for patient care, business, and clinical practice decisions.
The patient is a 70 cis-gender female:
- Primary complaints - Painful sitting, terrible tailbone pain x 2 years
- Secondary complaints - SUI, fecal urgency, mild POP
- Prior therapy - multiple, most recent Hospital Based OPPT 3 x per week x 8 weeks (24 visits)
- Progress - minimal to none, the patient actually thinks her symptoms are worsening, pain is unbearable
- Other diagnoses - Parkinson’s Disease, HTN, high cholesterol
- Primary Insurance - Medicare
SEPTEMBER
The patient presents to the provider for specialized pelvic floor therapy. The patient is seen 1 x per week for a total of 6 visits. The patient reports a 75% reduction in symptoms, adheres to her HEP, and attends all scheduled visits.
Treatment Included:
- Internal rectal musculature work (Instructed in Pelvic Floor Level 2A)
- Body mechanics and coccyx mobilization - internal and external (Instructed in Coccydynia & Painful Sitting)
- Sacral nerve release techniques (Instructed in Sacral Nerve Manual Assessment and Treatment)
NOVEMBER
The patient is now able to participate in her ADL, regular exercise routine, and her social life and she has noticed how her endurance and balance have declined as she tries to return to normal. She starts to come in 2 x per week, one day a week focusing on her pelvic floor complaints and one day a week focusing on her endurance, balance, and Parkinson’s symptoms. She completes an additional round of therapy 2x per week for 8 weeks. She progresses slowly but objectively measures small therapy gains.
Additional treatment:
- General strength and endurance training and conditioning
- Large amplitude movement program
- Education for a home walking program
- Connection to a Parkinson’s boxing program in the community
FEBRUARY
The patient gets sick, misses 2 weeks of therapy, and has a return in her coccyx pain and an exacerbation of her Parkinson’s symptoms. Her tremors became so bad that she has to cancel multiple sessions at the last minute. She is now also having swallowing and speech problems. She finally gets in with her neurologist who explains her Parkinson’s has progressed. They recommend changing her medications, assessment for a brain stimulator, and trying an intensive LSVT BIG Program 4x per week for 4 weeks.
Please pause and take a moment to think about a few things that may pop up for a provider from an ethical or legal lens!
SOME ETHICAL + LEGAL CONSIDERATIONS FOR THE CASE
- Prior to beginning the LSVT BIG program, the patient is already at 46 visits in total
- Your practice is a small, niche market practice that specializes in Pelvic Health - this patient only ended up with you due to her tailbone pain - your location is small and does not have “big gym” equipment or space
- You do have two providers that have prior LSVT BIG training
- This patient has worked with and reports feeling safe and comfortable with both providers
- Sitting in the car for more than 45 minutes is again a challenge for the patient and you are the closest qualified provider to her home
- You are the only Pelvic Floor clinic within the 15-mile radius
- To accommodate this patient’s scheduling needs will make your waitlist longer for others
- Medicare has an annual cap for services which changes based on practice setting. Physical therapy and Speech therapy share this cap.
- This patient has been plateauing/ possibly worsening as her Parkinson’s progresses and sessions are feeling like maintenance therapy.
- There are hospital-based LSVT BIG programs 55 minutes away from the patient's home.
The fun and challenging part about ethics is that the possibilities and scenarios are many and ever-changing. This is a real live case and an example of what therapists have to navigate on a day-to-day basis. Sadly, there is no right or wrong. Ethics and Law are areas of more gray than black and white.
Ethical Considerations from a Legal Lens has the following goals:
- Define basic Ethical Framework topics
- Perform Core Values Self Assessment
- Identify the components of the RIPS model and the Model Rules of Professional Conduct
- Explore Pelvic Health from a Legal Lens
- Apply the RIPS model to real-life legal scenarios
- Devise a plan of action or solution to legal and ethical scenarios
The hope is that with this understanding of things like beneficence (balance harms and benefits), non-malfeasance (do no harm), justice (fairness), and autonomy (respect for self-determination) as well as being well-versed in patient care topics like consent, abuse, misconduct, discrimination, and our individual practice acts, providers will feel more comfortable in their ethical decision making.
Ethical Considerations from a Legal Lens and Ethical Concerns for the Pelvic Health Professionals both offer the information needed to have these conversations and start problem-solving these decisions. It is encouraged as part of the precourse work to send in the ethical concerns that have you stuck in the clinic or keep you awake at night!
Ethical Considerations from a Legal Lens
Price: $175.00 Experience Level: Beginner Contact Hours: 6 hours
Course Dates: June 3 and November 12
Description: This one-day remote course covers ethical considerations from a legal lens for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day to day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges, and the legalities of pelvic health can add in further complications for patient care, business and clinical practice decisions.
Ethical Concerns for the Pelvic Health Professionals

Price: $175.00 Experience Level: Beginner Contact Hours: 6 hours
Course Dates: September 16
Description: This one day remote course covers ethical considerations for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day to day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges due to the anatomical areas being treated, topics being discussed, and intimacy of sessions.

Dawn Sandalcidi PT, RCMT, BCB-PMD is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO. Additionally, she runs an online teaching and mentoring platform for parents and professionals at www.kidsbowelbladder.com.
Dawn is a national and international speaker in the field, and she has gained so much from sharing experiences with her colleagues around the globe. In addition to lecturing internationally on pediatric bowel and bladder disorders, You can join Dawn Sandalcidi with H&W in her courses, Pediatrics Level 1 - Treatment of Bowel and Bladder Disorders and Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders. This year H&W is excited to announce that Dawn will be teaching live for the first time since 2020, join her at the Pediatrics Level 1 course in Syracuse NY on June 3-4, 2023.
Why you should have these tools in your toolbox today.
As a clinician, it can be challenging to take a step back and look at every single patient as a whole person. Time constraints, hectic schedules, and never-ending notes make it difficult for you to do everything you’d like. Have you ever fantasized about an all-inclusive, multi-disciplinary center where physical therapists, occupational therapists, speech therapists, and other professionals gather weekly to assess a caseload of patients and make recommendations personalized to those patients?
Although clinics like this are not very common, you can bring a sense of this comprehensive approach to your clinic by expanding what you offer. As you know, many pediatric clinics offer PT, OT, Speech, and maybe aquatic therapy or early intervention services. Clinics offering pediatric pelvic floor therapy are more limited but on the rise.
You can bring these much needed services to your own clinic, and gain this knowledge without even leaving your home! If you’ve never considered expanding your services to include pelvic floor therapy for your pediatric patients, it’s time to explore exactly how this skill set can impact your patients’ lives.
Who Needs Pediatric Pelvic Floor Therapy?
Pediatric pelvic floor therapy is for children with bowel and bladder issues. Many of them also have special needs and will frequent your pediatric therapy centers. Since these patients in need will already be in your clinic, why not address as many of their issues as possible, all in one place?
Neurotypical children, as well as those with special needs (like children with cerebral palsy, spina bifida, sensory processing disorders, and other developmental or behavioral issues) often struggle with bowel and bladder conditions in addition to their chief complaints. These families may struggle on a daily basis to manage exercises, feeding, play, and oftentimes, toileting troubles as well.
You may be thinking that bowel and bladder issues are reserved only for children with more severe conditions, however many children with bowel and bladder issues do not have any underlying neurological conditions. Oftentimes, these bowel and bladder issues in children are due to pelvic floor dysfunction (PFD).

It’s not as easy for children to communicate when something is wrong, PFD can go undetected for long periods of time in this population. A study from 2019 found that 46% of constipated children and 67% of children with fecal incontinence rated bowel habits as good or very good. The authors also noted 50% of constipated children did not mention their symptoms to anyone.
Parents don’t always know what’s normal and even when they do figure out there’s an issue, they often don’t have a clue about where to start, or what pediatric pelvic floor therapy even is.
What is Pediatric Pelvic Floor Therapy?
Pediatric pelvic floor therapy is a specialty area with a focus on pelvic conditions and symptoms for children up to 18 years old. Pelvic conditions and symptoms will frequently affect both bowel and bladder function in children.
Pediatric pelvic floor therapy is one of several treatment methods under the umbrella of “Urotherapy”. Urotherapy is a non-standardized conservative based treatment option for children with voiding dysfunctions.2 Dysfunctional voiding (DV) refers to a group of abnormal lower urinary tract (LUT) symptoms such as straining, hesitancy, and dysuria. Other LUT symptoms involved are related to bladder storage, such as frequency, urgency, and incontinence.
Pediatric pelvic floor therapy is a great first-line treatment option for functional constipation. This refers to a vicious cycle of stool retention in the rectum which eventually leads to distention, loss of urge, and more constipation. Functional constipation is directly related to LUT symptoms and DV. It is estimated that up to 50% of children suffer from LUT symptoms with constipation at some point.
A majority of children with bowel and bladder dysfunction can be successfully treated with pediatric pelvic floor therapy. Your treatment plan may include education, lifestyle changes, bowel and bladder diaries, pelvic floor and trunk muscle retraining, sEMG, and more. In order to provide the best recommendations for families with children suffering from bowel and bladder dysfunction, it’s important to begin with a thorough initial evaluation.
What Does a Pediatric Pelvic Floor Therapy Evaluation Involve?
I would argue that almost every child could benefit from a pediatric pelvic floor therapy evaluation. Just like with pelvic floor therapy for adults, much of what you’ll do for pediatric pelvic floor patients is completely external. So many children will have significantly improved quality of life with basic behavioral changes.

Pediatric pelvic floor therapy evaluations involve first investigating the source of bowel and/or bladder dysfunction. Tools such as questionnaires and subjective assessments are integral to your assessment and provide measures for tracking success. Ultrasound is another tool commonly used to help gather information and make bowel and bladder dysfunction diagnoses in children.
This may seem obvious, but the orthopedic physical assessment you regularly perform as a pediatric therapist is another very useful tool used in determining sources of bowel and bladder dysfunction. You may be surprised to learn how frequently side-to-side discrepancies or overactive hip muscles play a role in bowel and bladder dysfunction. As with all diagnoses, determining the root of the problem will drive your treatment planning.
What Treatments Are Involved in Pediatric Pelvic Floor Therapy?
Pediatric pelvic floor therapy can be intimidating to therapists who have never treated PFD before. First, know that success can be achieved without any internal examination or treatment at all.
Pediatric pelvic floor therapy treatments may include bowel and bladder diaries, breath work, stretches, abdominal massage, behavioral modification, and exercises to achieve balance in trunk and lower extremity strength, length, and function. Parents are often encouraged to be involved in treatment techniques as they’re with their children a majority of the time.

Where Do Pediatric Patients with Pelvic Floor Dysfunction Currently Receive Care?
You may be wondering, “If pediatric bowel and bladder issues are so common, who is treating all these patients?” This is a great question, and the answer will likely disappoint you.
Since I started doing pediatric pelvic floor therapy over 30 years ago, I’ve met thousands of children from birth to 17 years old. I can’t count how many older children are referred to my clinic with issues they’ve had for as long as they can remember. PFD in children often goes untreated — this population is severely underserved.
Children suffer from embarrassment, isolation from peers, and decreased quality of life because of bowel and bladder dysfunction. Parents often don’t know where to go for help or what options exist, so the issues commonly persist into adulthood.
If a child is lucky enough to be referred to someone aware of pediatric pelvic floor therapy, this is the best first-line treatment. Oftentimes, however, parents and pediatricians alike are unaware of this option, and they never make it to our offices. Children may be treated by pediatricians with medication, or referred to specialists.
When is Medical Treatment Indicated over Pediatric Pelvic Floor Therapy?
It’s pretty mainstream to recommend physical or occupational therapy for children with fine or gross motor delays, but how often are pediatricians recommending therapy for bedwetting, incontinence, or constipation? Physicians are great gatekeepers and it’s your job as a therapist to partner with local pediatricians in your area so they know who you are and how you can help them, especially if you decide to add pediatric pelvic floor therapy as a service in your clinic.
Many children are unnecessarily referred to gastroenterology or urology for bowel and bladder issues that could be managed with pediatric pelvic floor therapy (and without the need for medication). I would argue that medications are often used more quickly than necessary, but that doesn’t mean they don’t have a place in the management of pediatric bowel and bladder dysfunction.

Laxatives are commonly recommended to treat constipation. There are also medications that can be prescribed for bedwetting and incontinence. Enemas are used for chronic constipation issues that either do not respond to initial treatment or are medically indicated for other reasons.
I almost always recommend trying dietary, behavioral, and physical interventions first. If a child is not responding well to these interventions after 30-60 days of treatment, medical intervention may be indicated. In my courses I go in depth about titrating medications and how you can assist families in finding the best overall treatment regimen for them in conjunction with their pediatrician.
How Can You Get Training for Pediatric Pelvic Floor Therapy?

You likely didn’t learn much of anything about pediatric pelvic floor therapy in school. Now that you know the basics about pediatric pelvic floor therapy and the dire need for more professionals trained in helping these patients, you’re likely wondering how you can dive in and help.
I offer live and online courses to train healthcare professionals interested in treating pediatric bowel and bladder disorders. Why not offer your patients more than the standard, “hopefully you’ll grow out of it”? Your patients and their families deserve the best care available, and if I were a betting person, I’d bet on you!
Click below to learn more about my online and live course offerings for pediatric pelvic floor therapy. Hope to see you there!
This blog originally was posted on August 9, 2022, by Dawn Sandalcidi at https://kidsbowelbladder.com/why-add-pediatric-pelvic-floor-therapy-to-your-treatment-arsenal/.
Pediatrics Level 1 - Bowel and Bladder Disorders - Syracuse, NY
Price: $625
Experience Level: Beginner
Contact Hours: 19.5
Description: This two day, in-person course includes pre-recorded learning followed by a live, in-person course taught by instructor Dawn Sandalicidi, PT. The pre-recorded learning must be viewed in Teachable before Day One of the course.
This course begins with instruction in anatomy, physiology, and in development of normal voiding reflexes and urinary control. The participant will learn terminology from the International Children's Continence Society, medical evaluation concepts for bowel and bladder dysfunction, and common dysfunctions in voiding and defecation. Common causes of incontinence in the pediatric patient will be covered, and a comprehensive approach to evaluation will be instructed including video examinations of the pelvic floor and surface electromyography (or sEMG, a form of biofeedback).
Pediatrics Level 1 - Bowel and Bladder Disorders
Price: $625
Experience Level: Beginner
Contact Hours: 19.5
Description: This two day, in-person course includes pre-recorded learning followed by a live, in-person course taught by instructor Dawn Sandalicidi, PT. The pre-recorded learning must be viewed in Teachable before Day One of the course.
This course begins with instruction in anatomy, physiology, and in development of normal voiding reflexes and urinary control. The participant will learn terminology from the International Children's Continence Society, medical evaluation concepts for bowel and bladder dysfunction, and common dysfunctions in voiding and defecation. Common causes of incontinence in the pediatric patient will be covered, and a comprehensive approach to evaluation will be instructed including video examinations of the pelvic floor and surface electromyography (or sEMG, a form of biofeedback).
Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders
Price: $600
Experience Level: Intermediate
Contact Hours: 15
Description: This course will give you the confidence to treat any pediatric patient with bowel or bladder issues. Forget the days of a referral coming across your desk and thinking, “what in the world?”, then frantically searching the web for more information. This course gives you a lifetime of access to all things advanced pediatric pelvic floor, such as:
- In-depth rib cage assessment
- Next-level core evaluation and treatment techniques
- Updated DRA/pressure system exercise guidance
- Full-body movement analysis as it relates to the pelvic floor
- A deep dive into how specific disorders change a patient's movement and what to do about it
Emily McElrath, PT, DPT, MTC, CIDN is instructing her upcoming course Pregnancy & Postpartum Considerations For High Intensity Athletics scheduled on May 21, 2023. This one-day remote continuing education course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high intensity interval training (HIIT).
Emily is a native of New Orleans and received her undergraduate degree in Athletic Training at the University of Southern Mississippi and went on to receive her Doctorate of Physical Therapy from the University of St. Augustine for Health Sciences. She is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance. Emily is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and Cross-fitter and has personal experience modifying these activities during pregnancy and postpartum.
Introduction: Although routine exercise has long been recommended throughout pregnancy by medical professionals, High Intensity Athletics like Crossfit, weightlifting, and HIIT have received mixed approval amongst healthcare providers. There seems to be limited knowledge on how this form of exercise affects the pelvic floor and abdominal wall throughout pregnancy and postpartum, thus creating a limited understanding of proper recommendations by healthcare providers in regard to how and when a patient can safely continue and/or return to high intensity athletics during pregnancy and postpartum. Unfortunately, some (likely well-intended) medical professionals have gone so far as to instruct their patients to completely avoid these types of exercise throughout pregnancy. But are these limitations really necessary? Does the research support these recommendations? Or is there a way we can help these women continue to safely participate in high intensity athletics throughout pregnancy, and return appropriately in the postpartum phase?
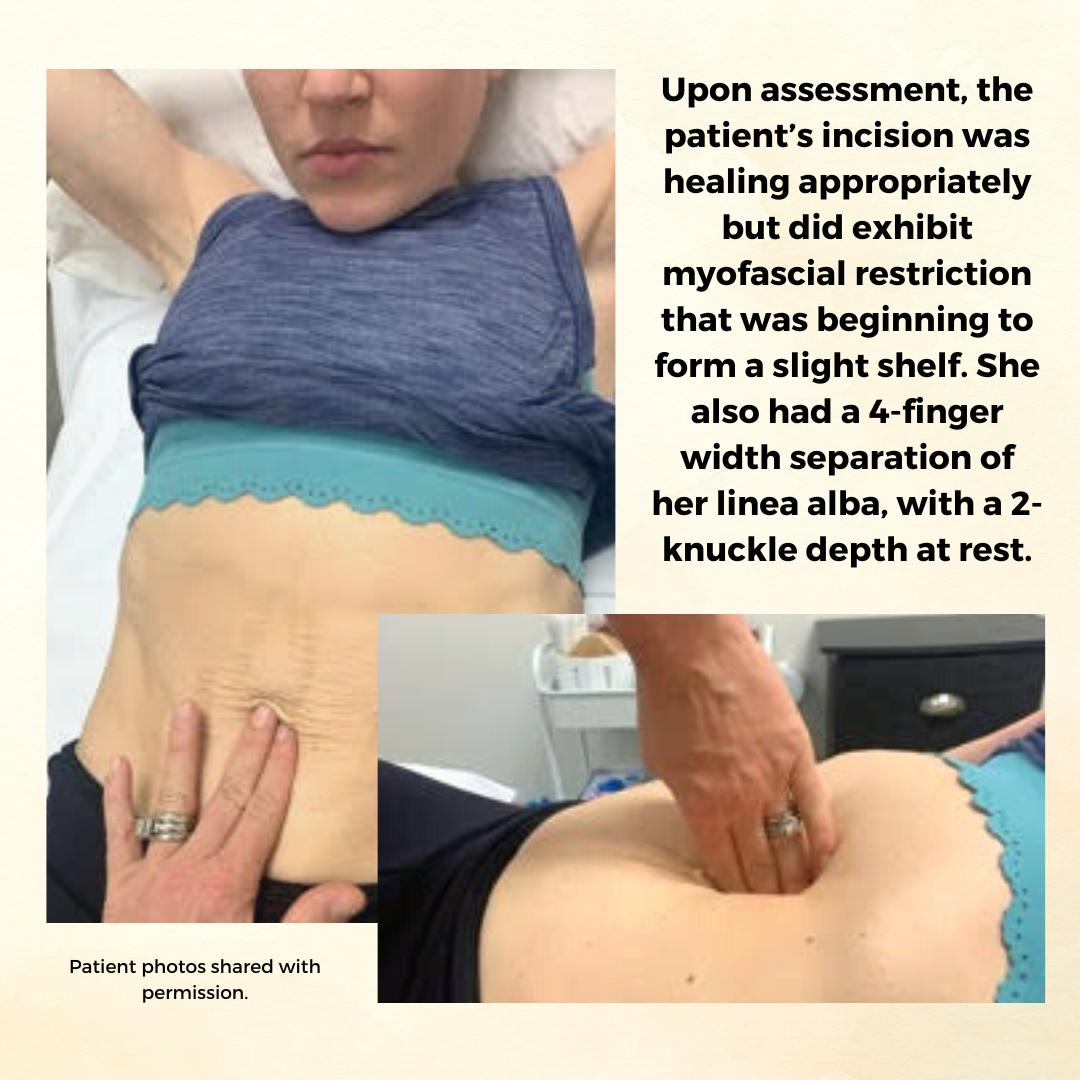
Background: The patient is a 34 y/o female who reported to the Physical Therapy clinic at 2 months postpartum from a cesarean delivery of twins. The patient was seen prior to her delivery (beginning at 24 weeks gestation) to prepare for a vaginal delivery, address chronic constipation, and to receive guidance on how to safely continue Crossfitting during pregnancy. She had been a Crossfitter (5-6 x weekly) for roughly 10 years at the time of her evaluation and was a track athlete and distance runner prior to that. Prior to pregnancy, the patient competed in local and regional Crossfit competitions in the RX division. The patient continued to Crossfit throughout her pregnancy and was able to avoid any pelvic floor dysfunction with proper modification and guidance. The patient returned for postpartum assessment at 8 weeks. At the time of the evaluation, she had begun taking short walks and performing body weight strengthening exercises. Her main concern at the time of the evaluation was a significant diastasis recti (DRA), and a self-reported decrease in core control and awareness. While the patient no longer desired to compete in local or regional competitions, she did want to continue Crossfit 5-6 x weekly and wanted to make sure she was able to safely do so with her DRA. Upon assessment, the patient’s incision was healing appropriately but did exhibit myofascial restriction that was beginning to form a slight shelf. She also had a 4-finger width separation of her linea alba, with a 2-knuckle depth at rest. Initially, the patient was unable to perform a proper transverse abdominus (TrA) contraction and was subsequently unable to create good tension across the gap. She also demonstrated compensatory recruitment of her obliques with attempts to perform a TrA contraction. The patient demonstrated mildly improved TrA recruitment in standing and following treatment, which consisted of myofascial release to her abdominal wall and incision, dry needling to her obliques, and internal trigger point release to her pfm. The pt exhibited limited pfm motor control at the time of her postpartum evaluation, and her PERF score was 2/6/5/2. The pt also exhibited myofascial restriction of her thoracolumbar fascia, proximal adductors, and B glutes. The pt continued to be seen for roughly 1 year following the delivery of her twins. In that time a variety of treatment strategies and techniques were used.
Methods: The methods used to treat this patient included education on proper pressure management strategies (including modification to breathing strategies during exercise), exercise scaling and modification, internal trigger point release to the pfm, followed by neuromuscular re-education once the normal resting tone of the pfm had returned, myofascial release to her abdominal wall and cesarean scar, dry needling, and education on a home exercise program (HEP). The pressure management strategies provided to the patient focused primarily on the various breathing patterns she could utilize to prevent breath holding, improve pelvic floor contraction, and reduce intra-abdominal pressure. The use of the Valsalva was not re-introduced until the patient had normal pfm motor control, exhibited proper tension across her DRA with no evidence of doming or conning, and only in limited circumstances (primarily when the weight was over 80% of her max for that movement). Pelvic floor motor control was assessed via internal palpation, in standing, and with a load (ie back squat and deadlift). Activity modification included modification of the speed of various movements, the load (weight) of various movements, the velocity of various movements (barbell cycling versus slow reps and strict gymnastics versus kipping), and the volume of various movements (number of repetitions or rounds/time of time of a metcon). If the patient’s tissues still could not handle the load with the above modifications, the movement was changed altogether (i.e. mountain climbers versus toe to bar). Measures used to indicate tissue tolerance to the load included: abdominal doming or coning, urinary incontinence, pelvic pain or heaviness, pulling or pain along her incision, and low back pain. If the patient experienced any of these symptoms, the movement was modified until she was able to complete the movement without symptoms. Additionally, the patient received internal trigger point release to the pfm, dry needling to the abdominal wall, glutes, proximal adductors, and lumbar paraspinals, myofascial release to the same muscle groups, neuromuscular re-education, and kinesiotaping to the abdominal wall.
Results: At the time of her discharge, the patient was able to fully return to all desired Crossfit activity. This process took roughly 1 year and required a gradual loading of her tissues through activity modification, to allow them to properly manage the load placed on them. For her, gymnastics movements on the rig took the longest to return to. She did not fully return to these movements (pull-ups, toes to bar, chest to bar pull-ups, and muscle-ups) until roughly 8-9 months postpartum. At the time of her discharge, she was able to create good tension across the gap and had improved her DRA to only less than 1 finger width separation and less than 1 knuckle of depth at rest. When performing a TrA contraction, there was no depth or width of separation. The pt also had an improved PERF score of 5/10+/10/8. The pt exhibited normal pfm motor control and excellent pressure management at the time of discharge.
Conclusion: While there is not a large amount of research available on the effects of high intensity athletics on the function of the pelvic floor and abdominal wall, we are beginning to see an increase in research on new, and more functional approaches to evaluating and treating Diastasis recti (DRA). There has also been a recent increase in research looking at the effects of various breathing techniques during exercise (including the Valsalva) and how it affects both the mother and the baby. Consistent review of the most current research, a thorough understanding of the mother’s anatomy and how it changes during pregnancy and postpartum, as well as each patient’s unique history and goals is necessary for clinicians to provide the highest quality of care for each patient. This is how we can move away from blanketed natal and postnatal exercise recommendations, and develop patient centered, sport-specific treatment plans that will allow each patient safely and effectively participate in high intensity athletics.
Pregnancy & Postpartum Considerations For High Intensity Athletics

Price: $225.00 Experience Level: Beginner Contact Hours: 8.25 hours
Course Dates: May 21, September 10, and November 19
Description: This one-day remote course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high intensity interval training (HIIT). In this cours participants will review the current literature, discuss the unique needs of pregnant and postpartum high intensity athletes, and learn how to most effectively treat these patients as practitioners. The main focus of this course will be to learn how exercising throughout pregnancy, or returning to exercise postpartum may look different for a high intensity athlete versus a non HIIT athlete.
Participants will discuss how anatomical and hormonal changes will affect training for the pregnant and postpartum athlete, and review various modifications for this population. We will also discuss how various stresses placed on the body during these activities may affect pelvic floor muscle function, and review various pressure management strategies that can be utilized during high intensity interval training. The lab will be broken up into pregnancy considerations and postpartum considerations. During the pregnancy lab, we will review specific exercise modifications for pregnancy, utilization of breathwork to properly support the pelvic floor during pregnancy, and review how to assess for and tape for diastasis recti. In the postpartum lab we will review how to determine proper activity modification based on ability to manage pressure, review specific activity modifications and breathwork, review accessory work for return to activity, and discuss how to assess pelvic organ prolapse in standing.

Rivki Chudnoff, MSPT is instructing her new course, Cultural Sensitivity: Treating Conservative Religious Patients, which debuts on May 7, 2023. Save 10% off registration with discount code NEWCOURSE10. We look forward to seeing you in class! This course is designed to provide guidance and skills for engaging patients from religiously conservative backgrounds in a culturally sensitive manner and will gain a foundational understanding of the various traditions, customs, laws, and values associated with Muslim, Jewish, Hindu, and Christian faiths as they pertain to sexuality and pelvic health.
CASE STUDY: Sarah is a 23-year-old woman who presents to your office for an evaluation. Upon scheduling, she did not wish to disclose to your office manager what kind of pelvic health issue she wants to be seen for.
Upon patient interview, Sarah reveals that she has been married for 8 months and all attempts at intercourse have been unbearably painful. She reports a 14/10 on a pain scale and that she has vocally cried out in pain with any attempts at penetration. She is feeling hopeless that this will ever get better, and is concerned that something is wrong with her and that her vagina is “too small” for intercourse. Sarah admits that she has never examined her own vaginal opening or seen it in a mirror because it “grosses her out”.
Sarah is otherwise in good health but has never had a gynecological exam. She and her husband are both from a conservative religious background and were educated in religious schools with limited sex education, and were provided with little information about sex prior to marriage. Neither of them had been sexually active prior to marriage. Sarah currently ascribes to her religious beliefs and practice which prohibits any conversations about sex with anyone other than her partner. She expresses an aversion to sexual activity and to her husband’s genitalia and semen. Sarah confides that she feels guilty that she is not able to have intercourse and “make her husband happy”.
Although she denies any discomfort with sitting or wearing tight-fitted garments and has no other pain in her body, recently she has started to have pain in her vulvar area that starts before attempting intercourse. After attempts at penetration, she has difficulty falling asleep due to her pain.
She has a self-diagnosed “tiny bladder” and frequently has to urinate every hour. Sarah reports a long history of constipation, with bowel movements about once a week with straining (type 1-2 on the Bristol stool scale)
She reports regular periods, but excruciating pain the first 2-3 days that can be debilitating at times. She has never successfully inserted a tampon.
Sarah’s personal goals for treatment are:
- To have intercourse without pain
- To become pregnant as soon as possible, as is expected in her social circles and close-knit community
What other questions would you like to ask this patient?
What is your next move?
What would your treatment plan look like for this patient?
What other healthcare providers might you refer her to?
Cultural Sensitivity: Treating Conservative Religious Patients has the following goals:
- Demonstrate a foundational understanding of the various traditions, customs, laws, and values associated with Christian, Hindu, Jewish and Muslim faiths.
- Identify potential challenges and barriers to care unique to pelvic health patients from conservative religious backgrounds.
- Describe five strategies for increasing comfort and confidence in interfacing with patients from different religious backgrounds.
- Apply cultural sensitivity to patient interviewing and education techniques.
- Discuss collaborative approaches to evaluation and treatment that are compliant with the patient’s religious and cultural norms.
- Evaluate culturally sensitive intervention in a case study format with your peers.
As pelvic health providers, we go into this special field with the desire to provide the best care for our patients in the most sensitive way possible. It can be particularly daunting when we encounter patients from religious backgrounds and cultures that are unfamiliar to us. In our attempts to be sensitive, we may be tempted to shy away from asking patients the questions that really need to be asked. We may avoid providing patient education we may have otherwise provided because we don’t want to offend, or may tiptoe around a treatment session where we may have otherwise taken a more confident approach. My hope is that practitioners will leave my course, Cultural Sensitivity: Treating Conservative Religious Patients, confident in their abilities to provide the highest level of care with confidence, sensitivity, and compassion for all of their patients.
Who are you? Describe your clinical practice.
I’m a mom of a bunch of adolescent kids and a dog. I drive a minivan with the sunroof open blasting Bon Jovi, Janet Jackson, Madonna, and Lizzo down the New Jersey Turnpike with a trunk full of mall returns and reusable shopping bags like a wild woman. Fun fact - I’m married to a gynecologist (no it’s not weird, and no, he’s not my gynecologist, because that would actually be weird).
My secret identity is as a pelvic health physical therapist at my private practice in Bogota, NJ where I hide from said teenagers.
I have been privileged to be involved in the field of pelvic health for the last two decades, both treating patients with a wide variety of pelvic health issues as well as providing community outreach and developing educational initiatives.
I have been joyfully teaching the pelvic floor series at Herman & Wallace for the last several years both in person and in the remote format. This is my maiden voyage teaching my own course for the Institute. I’m working on the accompanying soundtrack for the course and am taking requests.
What made you want to create this course?
At one of the first H&W courses I attended as a participant, I noticed it was a combination of women of different faiths (myself, an Orthodox Jew included) that were all treating each other behind the modesty curtains during lab. I remember thinking, “Cool, it’s like a pelvic health United Nations going on back here”.
I realized I was not alone. Individuals from a myriad of different backgrounds have challenges navigating the intersection of their religious world, its culture of modesty and conservative religious values, and the world of pelvic and sexual health. The very rules, spoken and unspoken that govern religious cultures and are innate to its members, can be mysterious and even surprising to people from more secular backgrounds. My hope is for this course to be the bridge between the two worlds, to be traveled comfortably by all those who wish to partake in the journey.
What need does your course fill in the field of pelvic rehabilitation?
Having expert clinical, diagnostic, and treatment skills are essential components of providing effective treatment. However, seasoned clinicians know these skills will only get their patients halfway there. My course, Cultural Sensitivity: Treating Conservative Religious Patients, falls under the other half of care: bedside manner, and building a therapeutic alliance. The focus of this course is the way we frame the care we are providing, and the way we interact with the human element within ourselves and within our patients that is more than muscles, nerves, joints, ligaments, and fascia.
Who, what demographic, would benefit from your course?
Anyone who treats patients with pelvic health concerns will leave this course with something they can incorporate into their practice. As pelvic health providers, we go into this special field with the desire to provide the best care for our patients in the most sensitive way possible. The problem is, we don’t always know what that is supposed to look like. It can be particularly daunting when we encounter patients from religious backgrounds and cultures that are unfamiliar to us. Most of us did not learn this in school. In our attempts to be sensitive, we may be tempted to shy away from asking patients the questions that really need to be asked. We may avoid providing patient education we may have otherwise provided because we don’t want to offend, or may tiptoe around a treatment session where we may have otherwise taken a more confident approach. My hope is that practitioners will leave this course confident in their abilities to provide the highest level of care with confidence, sensitivity, and compassion for all of their patients.
Cultural Sensitivity: Treating Conservative Religious Patients

Course Date: May 7th - Save 10% off registration with discount code NEWCOURSE10
Experience Level: Beginner
Contact Hours: 9.75 hours
Description: This course is designed to provide guidance and skills for engaging patients from religiously conservative backgrounds in a culturally sensitive manner. Participants will gain a foundational understanding of the various traditions, customs, laws, and values associated with Muslim, Jewish, Hindu, and Christian faiths as they pertain to sexuality and pelvic health.
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
When diagnosed early, testicular cancer can be very curable and have more favorable outcomes. However, the US Preventative Services Task Force recommends against regular screening for testicular cancer. It is classified as a Grade D recommendation. This means they do not recommend clinical screening in asymptomatic individuals, or teaching patients to perform self-exams because they do not have certainty that screening has a benefit. However, recently several authors are asking for reconsideration to change the rating to a Grade B. A grade B classification is recommended when there is a benefit from doing the screening. These researchers are arguing that new studies support the benefits of regular screening by patients and their physicians. They further argue that not only will earlier diagnosis help with more favorable outcomes but that the current grade confuses individuals about the importance of self-care and wellness and reinforces negative cultural attitudes about wellness and screening.
We have several self-screens that we should be doing regularly; dermatological skin checks, vulvar skin checks, and self-breast exams. It makes sense to me to include a quick check of the testicles as well.
This made me wonder, how often individuals were being educated in how to perform self-testicular exams? I surveyed 10 individuals with testicles from different regions across the country on whether or not they had been educated on how to perform a self-testicular exam or had a testicular exam performed during their annual physical. Of the 10 people I interviewed, only 1 was educated by their physician on how to perform a self-testicular exam, and he was a little “hazy” about the instructions of what to do. Another two had been proactive and looked up instructions of how to do this on the internet, both of them initiated the search after a friend was diagnosed with testicular cancer. Another 3 more mentioned that their physician had performed a testicular exam during their physical. The other 4 individuals only mentioned that a prostate exam was performed.
A testicular exam does not take long to perform. Knowing how our bodies feel in health will allow us to know if there are changes over time. Feeling what the testicles feel like at baseline will allow individuals to know if there is atrophy, swelling, lumps, or shape changes occurring. As pelvic rehab professionals, we can teach our patients how to perform self-testicular exams, and to teach patients to advocate for themselves to be sure their physicians are performing testicular exams during their annual exam. Testicular cancer is most common between the ages of 15 and 35. It is important for teens to learn to do this exam as well! Here are some simple directions you can provide your patients:
- It is best to perform this test monthly.
- It is easiest to perform this test in the shower. The warm shower will relax the muscles holding the testicles, making it easier to perform.
- Gently grip the top of the scrotum with the thumb on top and fingers underneath. Slightly pinch this area so that the testicle stays put and won’t move while you do the exam. You will feel the spermatic cord between your fingers and thumb. The spermatic cord connects the testicle to the rest of your body.
- With your other hand, gently roll the scrotum between your fingers and thumb to feel the surface of the testicle. Glide your thumb and fingers from top to bottom, do this on front to back and on the sides.
- Check for any lumps, or bumps, and report to a physician if you find something unusual. Lumps could be as small as a piece of rice or a pea.
- Make note of size changes over time. Swelling of the testicle or scrotum should be reported to a physician.
- If you feel any dull soreness or heaviness in the testicle, report this as well.
- Check both sides.
- It is easy to mistake the epididymis for something unusual. The epididymis is a set of tubes that are coiled and line the back and top of each testicle. You will feel this as a normal lump on the top back portion of the testes. It may feel tender to the touch, but this is normal.
- You can learn more specifics on testicular cancer in Oncology of the Pelvic Floor Level 2A (OPF2A). We not only discuss testicular cancer, but also go in-depth learning about penile cancer, prostate cancer, anal, and colorectal cancers. The next offering of OPF2A is May 20-21.
References:
- Fadich A, Giorgianni SJ, Rovito MJ, et al. USPSTF testicular examination nomination-self-examinations and examinations in a clinical setting. Am J Mens Health. 2018; 12(5): 1519-1516. Doi: 10.1177/1557988318768597
*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2A - partner needed for registration
Price: $495.00 Experience Level: Intermediate Contact Hours: 17.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on male pelvic cancers, colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient's body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: May 20--21
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Sandra Gallagher has served on varied committees and boards at the state and national level, most recently as the chair of the CAPP-OBC committee for the Academy of Pelvic Health of the APTA. She has presented on the role of PT in gender-affirming vaginoplasty at UCSF Transgender Health Summit, APTA Combined Sections Meeting, and at the 2018 international meeting of the World Professional Association for Transgender Health (WPATH). Join Transgender Patients: Pelvic Health and Orthopedic Considerations with instructors Sandra Gallagher, PT, DPT, WCS & Caitlin Smigelski, PT, DPT on April 29th.
In working with surgeons that perform and patients undergoing gender-affirming genital surgery I’ve had the chance to recognize that some of our most basic skills of assessing tissue and tissue healing play a huge role and optimizing healing. I personally have loved taking another look at some of the wound healing principles that I used early in my career in the 90s, to assist in developing timelines for post-surgical recoveries of gender surgeries.
In addition to the basic science of tissue healing, we’ve integrated current and novel neuroscience to develop Graded Motor Imagery guidelines to improve the sensory outcomes of vaginoplasty and phalloplasty surgeries. Graded Motor Imagery (GMI) is a treatment approach commonly associated with treating pain. It is generated from understanding the underlying neuroplasticity of complex pain conditions such as phantom limb pain. (1) Graded Motor Imagery in rehabilitation means that the focus is placed on synaptic exercise and health. The use of neuroplasticity to change sensory experiences occurs in other parts of rehab and goes under different names. Sensory integration, cortical integration, or mapping, are some other terms used. In addition to being used for reducing pain in complex regional pain syndrome, the techniques are used for reducing limb neglect in stroke rehab, and restoring limb function in complex hand surgeries (2,3,4,5). In pelvic rehab, we are using these concepts with urinary urgency suppression and in cis females with vaginal pain. There are handfuls of article exploring the presence and phenomena of phantom penis in trans men (6,7,8)
Using GMI for Phalloplasty
When using GMI for phalloplasty, the primary goal is to improve erogenous sensation in the penis. This is done with three main techniques: visualization of static and dynamic functions of the penis, tactile stimulation starting with a simple touch and progressing toward sensory stimulation, and sexual/erogenous stimulation (9). As people move through the process they use stimulation of the buried erectile tissue and other erogenous parts of their body while touching the penis. This can be a partnered or independent activity. This can be adapted regardless of the number of stages involved in the surgery.
Using GMI for Vaginoplasty
With vaginoplasty, the attaining pain-free and erogenous sensation typically progresses more directly than in phalloplasty, as there are fewer complications with vascular and nerve recovery. The clitoris and its neurovascular bundle are intact and continue to be perineal tissue. We use traditional pelvic rehab interventions of clinical EMG, and a robust home program of dilation, exercise, TENS, and self-care including patient-directed manual interventions. The addition of GMI guidelines for vaginoplasty more commonly is directed toward reducing vulvovaginal pain. Whereas the phalloplasty sensory protocol is initiated early in the surgical process, the vaginoplasty guidelines are more commonly applied when post-surgical pain limits someone's function. The GMI process here uses visualization and activities of seeing vulvas in one's surrounding environment, such as flowers, folded fabrics, and Georgia O'Keefe artworks. This is intended to be a neutral practice. Similar to the desensitization process in limb rehab, using various textures and depth of touch, combined with watching the light touch can help with pain reduction. As pain abates using stimulation of other erogenous tissue while touching the vulva or dilating can be added.
For providing optimal care, knowledge of the intricacies of gender transition is essential. Join me in Transgender Patients: Pelvic Health and ORTHO Considerations on April 29th to learn more regarding gender-affirming genital surgeries, discussion of other gender-affirming surgeries, and medical interventions that people transitioning might choose. We provide that overview in this course. Topics covered include:
- Societal influence on gender transition including interactions with healthcare providers
- Recognizing the difference between sex, sexuality, and gender
- Understanding the complexities of the legal system for the person transitioning genders
- Tips and tools for a trauma-informed intake and examination
- Health effects of hormones for gender transition as related to differential diagnosis in rehabilitation
- Supporting healing after gender-affirming surgery
- Operative procedures for face and chest
- Operative procedures for masculinizing and feminizing genital surgery
- Preoperative evaluation, treatment, and education issues
- Post-operative evaluation, treatment, education and follow-up for genital surgeries
- Outcome measures with rehab focus for people undergoing gender-affirming surgeries
- Fertility and pregnancy in gender-diverse people
References:
- Moseley GL. Graded motor imagery for pathologic pain: a randomized controlled trial. Neurology. 2006 Dec 26;67(12):2129-34. doi: 10.1212/01.wnl.0000249112.56935.32. Epub 2006 Nov 2. PMID: 17082465.
- Smart KM, Wand BM, O'Connell NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. Cochrane Database Syst Rev. 2016 Feb 24;2(2): CD010853. doi: 10.1002/14651858.CD010853. Pub2. Update in: Cochrane Database Syst Rev. 2022 May 17;5:CD010853. PMID: 26905470; PMCID: PMC8646955.
- Leifert-Fiebach G, Welfringer A, Babinsky R, Brandt T. Motor imagery training in patients with chronic neglect: a pilot study. NeuroRehabilitation. 2013;32(1):43-58. doi: 10.3233/NRE-130822. PMID: 23422458.
- Simon JJ, Welfringer A, Leifert-Fiebach G, Brandt T. Motor imagery in chronic neglect: An fMRI pilot study. J Clin Exp Neuropsychol. 2019 Feb;41(1):58-68. doi: 10.1080/13803395.2018.1500527. Epub 2018 Aug 6. PMID: 30080434.
- Kahn LC, Moore AM. Donor Activation Focused Rehabilitation Approach: Maximizing Outcomes After Nerve Transfers. Hand Clin. 2016 May;32(2):263-77. doi: 10.1016/j.hcl.2015.12.014. PMID: 27094897.
- Chris Straayer (2020) Phantom Penis: Extrapolating Neuroscience and Employing Imagination for Trans Male Sexual Embodiment, Studies in Gender and Sexuality, 21:4, 251-279, doi: 10.1080/15240657.2020.1842075.
- Ramachandran VS, McGeoch PD. Occurrence of phantom genitalia after gender reassignment surgery. Med Hypotheses. 2007;69(5):1001-3. doi: 10.1016/j.mehy.2007.02.024. Epub 2007 Apr 8. PMID: 17420102.
- Gherovici, Patricia. (2020). A Phantom Phallus? Studies in Gender and Sexuality. 21. 296-301, doi: 10.1080/15240657.2020.1842070.
- Peters BR, Annen AA, Berli JU, Gallagher S, Smigelski C, Kahn LH, Skelton HE. Neurosensory Re-education following Gender-affirming Phalloplasty: A Novel Treatment Protocol. Plast Reconstr Surg Glob Open. 2022 Oct 24;10(10):e4616. DOI: 10.1097/GOX.0000000000004616. PMID: 36299822; PMCID: PMC9592297.
Transgender Patients: Pelvic Health and ORTHO Considerations
Price: $500 .00 Experience Level: Beginner Contact Hours: 17 hours
This course is appropriate for any physical rehabilitation professional, regardless of their specialty area, who has an interest in better serving the people who are gender diverse. There is specific content aimed at teaching pelvic health therapists how to expand their skills for working with people of all gender identities. There will be particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
Course Dates: April 29 and August 19
Aparna Rajagopal, PT, MHS, WCS, PRPC, Capp-OB Certified is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interest in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction.
Leeann Taptich DPT, SCS, MTC, CSCS leads the Sports Physical Therapy team at Henry Ford Macomb Hospital where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
Aparna and Leeann co-authored the course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Abdominal bloating and distension are two very commonly reported GI symptoms in the pelvic practice setting. However, these symptoms are not commonly recognized in other physical therapy settings. While many people experience occasional bloating/discomfort it does not necessitate medical intervention, but repeated and long-standing bloating/distention can impact the quality of life.
One diagnosis which is associated with these symptoms is Abdomino-Phrenic dyssynergia where patients develop a paradoxical abdomino-phrenic response. Normally, as a response to an increase in intraluminal gas, the diaphragm relaxes, and the abdominal musculature contracts. When dyssynergia is present, the opposite happens and the diaphragm contracts, and the abdominals relax. Abnormal pelvic floor function is also associated with this diagnosis. Treatments typically used are biofeedback therapy and breathing techniques.
Where Leeann and I work, we are seeing patients increasingly referred with this diagnosis. Recently we treated a 72-year-old female patient with a long-standing history of troublesome bloating and distention, with the diagnosis of Abdomino phrenic dyssynergia.
- The patient had complaints of bloating and abdominal distension all day long, worsening toward evening
- She reported limiting her food intake in the evenings on account of the discomfort and "tightness" in the abdomen
- She rated the discomfort as 3-5/10 in the morning time with an increase to 8/10 by late evening
- She also reported poor sleep because of how "hard and tight" the abdomen felt by bedtime
Upon examination, amongst other findings, the patient demonstrated:
- Significant tightness in her posterior chain and her erector spinae in both thoracic and lumbar regions
- Decreased thoracic rotation/mobility
- Increased connective tissue restrictions in both upper abdominal quadrants, especially in the epigastric area and inferior to the rib cage
- Decreased lower rib cage mobility
- Poor ability to prolong exhale or to exhale strongly
- Decreased ability to relax the pelvic floor musculature after a contraction
In addition to biofeedback and visceral mobilizations, treatment techniques included joint mobility techniques inclusive of simple rib and thoracic spine mobilizations, soft tissue mobility techniques including gentle diaphragm releases, breath training, and breathing techniques to aid in pelvic floor relaxation.
The patient received 9 treatment sessions and a home maintenance program which she followed with good compliance. She reported a 70% overall improvement and was now able to sleep through the night and eat in the evenings without discomfort.
In our course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, you will learn:
- Explain normal diaphragmatic breathing and the role of the internal and external oblique musculature.
- Assess and treat dysfunctional breathing patterns including but not limited to chest, abdominal, and paradoxical breathing patterns.
- Understand the concept of Intra-Abdominal Pressure (IAP) and the control and use of IAP with the diaphragm in a lowered position as a stabilizing mechanism for the spine.
- Understand the concept of regional interdependence and its application in the treatment of back or pelvic pain patients.
- Recognize the effects of postural patterns and the linkage to the diaphragm and pelvic floor.
- Understand the muscles and myofascial components involved in dysfunctional breathing and techniques to effectively treat the same.
- Understand and demonstrate mobilizations of the rib and thoracic spine and develop a comprehensive treatment program.
- Develop an exercise progression for dysfunctional breathing for use in the clinic and in-home programs.
- Integrate diaphragmatic breathing and mobility in the athletic clientele
Course Dates: April 22-23
Price: $450
Experience Level: Beginner
Contact Hours: 14
Description: This remote course is an integrated approach where participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes while looking at structures from the glottis and the cervical region to the pelvic floor.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. Instructed techniques are applicable to patients who present with Diastasis Rectus Abdominis, pelvic pain, incontinence, and prolapse, as well as cervical, thoracic, scapular, and lumbar pain.
Join me on April 22 to begin this quest to learn more about signs, symptoms, and the journey that individuals with eating disorders endure. We will also explore ways that we as Pelvic Health Professionals can assist them on this journey in Eating Disorders and Pelvic Health Rehabilitation. This course will not have all the answers; rather will be a step forward for clinicians to expand their understanding and to seek out additional resources to learn more and provide evidence-based treatment for these individuals.
We, as pelvic health practitioners are NOT going to treat eating disorders… we are NOT going to diagnose eating disorders… but we CAN and SHOULD be asking questions… encouraging patients to seek additional support… and helping them find appropriately trained providers. We can ALSO provide support and speak with words that promote validation, wellness, and healing rather than words that are unintentionally triggering, harmful or nonvalidating. IN ADDITION, we can provide these individuals with manual skills, activities, and educational “tools'' to assist in GI distress, constipation, abdominal bloating, urinary dysfunction, pelvic pain, sexual dysfunction, POP issues, postural / body mechanics, abdominal canister coordination/function, tightness in trunk, hips, shoulders, rib cage, etc. These individuals would benefit from pelvic health professionals being an additional part (not the lead) of their treatment team.
We, as pelvic health professionals, need to: know what eating disorders are and are not, understand how this mental illness creates issues in all body functions, and what we can do to provide relief or reduction in some of their symptoms.
These case scenarios may be familiar or may have occurred without our awareness. These scenarios are based on real lives…and we likely see similar situations like this almost every day…
_____________________________________________________________________
Hope
Hope is a 31-year-old woman with an eight-year-old daughter with special needs. She is in your office for the second episode of care as she had COVID and her grandmother became terminally ill. Hope had come to PT before for severe abdominal pain and bowel dysfunction after a perforated colon during an ovarian cyst removal which resulted in a perforation in her colon, hemicolectomy, sepsis, and traumatic ICU hospitalization.
She had offered to you during her first episode of care that she had a history of anorexia. She was walking 7-9 miles a day, doing yoga 5 days a week, and seeing chiropractic care for fibromyalgia and chronic pain in the back/neck. She had been seeing an eating disorder mental wellness therapist and an eating disorder dietician for a while but had not seen them for some time. At the time of her first couple of visits, she was encouraged to make an appointment with both a mental wellness therapist and a dietician who both focused on eating disorders with who she was comfortable in the past. She agreed to do this but then stopped coming to therapy as mentioned above due to COVID and family emergencies.
When she came back to therapy, she looked much different. Her eyes were sunken, she had a thin layer of hair (lanugo) over her cheeks (what could be seen with the mask) and over her abdomen. Her fingernails were brittle and split.
She reported today that she has lost 25 more pounds because she thought that would help with the abdominal pain. Her new dietician (NOT an ED dietician) had her keeping a log of her food and has told her, according to Hope, that her body does not need more than 1500 calories a day and that she was eating “way too much”. She now logs everything she eats and counts calories.
Hope describes how she is now staying with her grandmother during the day in a skilled nursing facility and is supporting her grandfather. She is also caring for her 8-year-old daughter with special needs who is now in school during the day. She continues to exercise every day no matter what and is now not only walking the 7-9 miles but she is now doing strength training 4 days a week and yoga about 3-5 days a week. She seems to be almost superhuman as she juggles and manages all of these difficult situations.
After assessment of orthostatics, and standing blood pressure - her systolic BP dropped 25 mmHG and diastolic BP dropped 10 mmHg and her heart rate increased by 25 bpm after 5 minutes standing.
What might be some red flags here? What might your recommendations be? Who would you contact?
_____________________________________________________________________
Faith
Faith is a 24-year-old woman who came to pelvic floor physical therapy for urinary incontinence and dyspareunia which began after the cesarean section birth of her first child six months ago. She does not understand why she has all of the extensive "stretch marks" on her abdomen and why her cesarean section scar looks so large. She is very unhappy about how her body looks after giving birth.
Upon further conversation, she shares that she only eats a “super clean diet” and has cut out major food groups such as dairy, sugar, and meat because those foods are "high in calories" and "not healthy". She sparingly consumes any carbs and mainly eats vegetables and some fish sometimes.
She has experienced episodes of lightheadedness and near syncope for years. She reports that has been very “bendy” and was a cheerleader in high school. Faith has had painful joints and subluxations in her hips and knees for as long as she can remember.
Faith also shares that it is always so tiring. She also reports that she worries a lot about her newborn and is having a hard time juggling all of the demands of work, home, and caring for her baby. Her husband is helpful though has to work a lot.
After the assessment of orthostatics, Faith becomes lightheaded when standing. She was orthostatic for heart rate (>20 bpm) after 1, 3, and 5 minutes in standing. Her blood pressure also drops a bit in standing (<10 mmHg systolic) though was not considered orthostatic. She also has a Beighton score of 7 out of 9, has piezogenic papules on both of her heels, and soft velvety skin which is easily stretched.
Faith is asked if she would consider trying some salty snacks and some Gatorade to see if this helps with her lightheadedness. She responds that she will not eat pretzels or salty snacks because they are too high in carbs and she will not consider Gatorade because she doesn't drink beverages that are high in calories.
She keeps touching her abdomen and is uncomfortable about the “stretch marks'' that she has. She also keeps looking at herself in the mirror that is in the treatment room pulling her baggy sweater over her body.
She shares that she has always had constipation and abdominal pain - however this has really worsened lately. Faith also reports pelvic pressure at times and hopes that she does not have to deal with a pelvic organ prolapse like her mother had a few years ago.
During her first visit, she speaks very quickly and appears quite anxious.
This is only part of the history…but what might be helpful to say, do, explore, and assess?
_____________________________________________________________________
Brian
Brian is a 17-year-old wrestler who is coming to pelvic floor physical therapy for abdominal and pelvic pain. He shares that when he has to make "weight" before each meeting he will restrict water, and food and will exercise with layers of clothing on. He will drink about a cup of water during the day on those days and sometimes will just eat some chocolate, such as a peppermint patty, for dinner. After the meeting, he will sometimes eat a lot. He will often have significant abdominal pain and it will make him double over sometimes. He went to the GI doctor and was told that he has gastroparesis. He does not not know what he is supposed to do. If he doesn't eat, his abdomen hurts, and if he does eat it hurts too.
He also shares that he doesn't like school so much anymore. There is a lot of pressure to get a college scholarship and he is waiting to hear from a couple of his top choices. He doesn't feel like hanging out with some of his friends so much anymore. They always want to go out to eat and he can't do that. He typically will spend time with other wrestlers or will just stay at home. He reports being exhausted and having a hard time concentrating on his schoolwork.
Brian shares with you that he has to strain so much to have a bowel movement that he sometimes feels a bulging from his anus. He has a bowel movement about once a week and it is painful.
He does have urinary urgency and reports urinating "a little bit" many times during the day. His urine is tan in color.
When further questioned about Brian's response on the male genitourinary pain index (GUPI), he reports that he does not have pain with sexual climax because he does not have any desire to be sexually active anymore.
This is just a glimpse of Brian's journey... What other questions might you have? What can we do to help? What else would you be assessing?
_____________________________________________________________________
Joy
Joy is a 34-year-old musician with a history of binge eating disorder, which has been well-controlled for over five years. She comes to you with pelvic pain, dyspareunia, abdominal pain, and a history of constipation and urinary incontinence.
Joy saw a pelvic pain specialist who recommended a tricyclic antidepressant for pelvic pain. Joy also has bipolar disorder. She is in DBT treatment weekly (group and individual) and is well supported by her psychiatrist.
She is reporting new binge-related urges that are becoming hard to control since beginning the new medication. She is concerned about these new urges and this is causing additional anxiety. Her pelvic pain is actually worsening now with the additional anxiety and she is beginning to leak urine more frequently. Bowels are becoming firmer and harder to pass.
What are some next steps with Joy? What can we do to assist with her situation?
_____________________________________________________________________
Eating Disorders and Pelvic Health Rehabilitation: The Role of a Rehab Professional is a live remote course (including lab and lecture) with required seven-hour pre-course content accessible on Teachable. During the live course, there will be lectures, interactive discussions, and lab activities. We recommend, if possible, having another human available during the lab activities to practice the techniques discussed.
I look forward to seeing you on April 22!
Eating Disorders and Pelvic Health Rehabilitation
Course Dates: April 22
Price: $395
Experience Level: Beginner
Contact Hours: 13.25
Description: This course explores types of eating disorders including anorexia nervosa, bulimia nervosa, binge eating disorder, ARFID (Avoidant Restrictive Feeding Intake Disorder), and OSFED (Otherwise Specified Feeding and Eating Disorder). We will also discuss conditions that do not yet have formal diagnostic criteria such as orthorexia and diabulimia and we will touch on Pica and Rumination Disorders. Most healthcare professionals understand very little about eating disorders and disordered eating. There is a weight stigma with health care identifying “health” in terms of weight, BMI, body appearance, exercise, and activity. As rehabilitation professionals, it is our responsibility to understand that health looks and feels different for everyone. In addition, we may be able to identify signs and symptoms of eating disorders and be able to provide support for these individuals through proper referral and modification of our rehabilitation plan of care.
What is a TA? In the world of the Herman & Wallace Pelvic Rehabilitation Institute, a TA is an abbreviation for teaching assistant. Herman & Wallace has always had teaching assistants (TAs) at lab courses to guide hands-on lab time to be extra hands and helpers for the instructors. Having exemplary instructors and the addition of more people on the teaching team in the room to answer questions, guide, and give clinical pearls is what creates the optimal learning experience through Herman & Wallace.
During COVID, the demand for quality pelvic health education was still high, but COVID limited travel and group gatherings. The Institute was able to pivot and reformat some courses into fully remote offerings. This allowed continuing education to continue but did not answer the question of the core series of pelvic floor courses and all of the other course offerings. This required some creativity. Some labs could be taught virtually, but some educational topics and skills could not be covered without in-person, hands-on learning in which participants got to practice on real bodies..The next pivot was to create a hybrid model of learning, in which some didactic skills were reformatted into pre-recorded content, and the labs were offered in smaller satellites around the country. Herman & Wallace had always been a leader in education because of the hands-on skills provided and learned during in-person labs. The question arose, who would help guide them and be the “boots on the ground” for lab skills?
Enter the teaching assistant team! Each satellite class for the Satellite Lab Courses comes with an experienced TA. These are practitioners who apply for the position or are invited by the Herman & Wallace staff because of their exemplary performance during other courses or their CV full of continuing education in the pelvic floor field. A teaching assistant must have taken the core classes including Pelvic Floor Levels 1, 2A, and 2B through Herman & Wallace Pelvic Rehabilitation Institute. They must feel comfortable learning along with the participants, guiding participants through labs, and sharing the clinical pearls they have as they relate to the content being taught.
TAs had always had an important role in courses, but as the primary educators during lab time, they were now a vital part of the learning experience for participants. In keeping with this bigger role, Herman & Wallace, created an elevated role called a Lead Teaching Assistant (Lead TAs). In addition to completing the education required of a teaching assistant, Lead Teaching Assistants have assisted at 5 or more classes with Herman & Wallace within a 2 year period, with a stellar record of not canceling on short notice after committing (TA cancellation is a big scheduling nightmare for the Institute). They have earned consistently positive feedback on surveys from their participants.
Lead TAs commit to TAing a minimum of 4 events per year and even will travel to do so if needed by HW. Lead TAs also have access to many of the bonus learning experiences and presentations that the Herman & Wallace Faculty have access to. Lead TAs are like super, fancy, ultra teaching assistants because it is literally their job to provide the best lab experiences for participants.
What are the benefits of being a TA? You get access to all of the updated course content. When you TA, you get Teachable access to the most up-to-date version of that class. Herman & Wallace is always updating, revising, and adding, so you get to learn all those new gems for FREE! If you’re like most participants, looking to take 20 other courses but trying to figure out how to afford it (without selling your firstborn), being a TA is the solution. You get paid in Herman & Wallace course credit, which means that if you TA a class you are pretty close to taking another class on the house! The chance to network with other therapists is another perk TAs often list. You also earn CEUs for the classes you assist, as long as you complete the course through Teachable. The last benefit comes if you are studying for a certification like your PRPC because it is a great way to “retake” and review the content. Did I mention the credit you receive from TAing can also be used to pay for your PRPC certification?
 What are the benefits of being a Lead TA? Really all of the above but it comes with more opportunities. Lead TAs become employees of Herman & Wallace which means that you can choose to be paid in course credit or money. You also get to attend monthly skill-building educational bonus opportunities created just for TAs. Lead TAs also get invitations to certain “Faculty Only” exclusive Herman & Wallace presentations. If you want to be able to write your own class or teach for the series, this is a great way to build your career towards this goal.
What are the benefits of being a Lead TA? Really all of the above but it comes with more opportunities. Lead TAs become employees of Herman & Wallace which means that you can choose to be paid in course credit or money. You also get to attend monthly skill-building educational bonus opportunities created just for TAs. Lead TAs also get invitations to certain “Faculty Only” exclusive Herman & Wallace presentations. If you want to be able to write your own class or teach for the series, this is a great way to build your career towards this goal.
Can I be a TA if I have not taken my education through H&W? Sadly, the answer is no. The Herman & Wallace Pelvic Rehabilitation Institute acknowledges that other education can have the ability to provide the same level of education and pelvic health knowledge. However, it is the Institute’s stance that teaching assistants for Herman & Wallace should be intimately familiar with the manner in which lectures and labs have been taught to participants through the Institute. Education through other avenues, while informative and valuable, does not provide these opportunities.
How do I know I am ready to be a Teaching Assistant? Are we ever really ready? As a therapist, I feel the more I learn, the more I learn what I don’t learn. But when you are working with participants, they want your reassurance and guidance during learning, not for you to know every single thing. I like to say “do your best until you know the rest” to participants (and myself) as we are all ALWAYS learning. You are ready when you feel you can come into the experience with a growth mindset of being as prepared as you can be and also have a plan for if you need help in teaching/supporting participants.
What if I don’t know the answer to a question? As someone who has been a TA to over twenty classes, I can say, you will not always have the answers. What you learned in college or when you took a class a few years ago may have changed or been updated. BUT you can be a resource and a guide to help work with participants in their learning to find those answers with the course instructor, research, and other pelvic health resources. Herman & Wallace offers a teaching team and you are one member of that team!
How can I be compensated? If you are a teaching assistant you will be compensated at a specific rate of Herman & Wallace course credits per day of service. If you are a Lead TA, you will also have the option to be paid in course credit or a cash rate. These rates will be discussed with the teaching assistant coordinator during the application process.
How do I pick what class to TA? Start with something you are comfortable with. This may be your favorite Herman & Wallace class, a clinic you are familiar with, or a topic you are really passionate about. It has to be a class you have taken through Herman & Wallace, but otherwise, you have quite a few choices! Please remember that you have to have completed all three of the H&W core pelvic floor courses to TA any of them. Other classes also have requirements to TA them. The best way to find out if you are qualified and what you are qualified to TA is to fill out the application.
Are you convinced to join the team as a Teaching Assistant? Click here to apply to be a Teaching Assistant.
Are you already a Teaching Assistant and ready for a promotion to Lead Teaching Assistant? Please email Megan Farr at This email address is being protected from spambots. You need JavaScript enabled to view it. and let her know you would like to be considered for a Lead TA role.
Would you like to chat with a Lead Teaching Assistant to find out if one of these tracks is right for you or to have some mentorship in your lab skills journey - please feel free to contact Megan Farr and she’ll help you get that conversation started too!
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
March is Colorectal Cancer Awareness Month. Did you know that the incidence rate of colorectal cancers is increasing? According to the International Agency for Research on Cancer, 1.9 million new cases of colorectal cancer were identified worldwide in 2020. This number is expected to grow even more. It is predicted that by 2040 the number of new cases of colorectal cancer will rise to 3.2 million new cases a year, and 1.6 million annual deaths worldwide. Additionally, did you know due to the fact that the incidence rate is increasing and it is being diagnosed in younger individuals, the age for screening for colorectal cancer has lowered to 45? At age 45 individuals should begin regular screening for colorectal cancer either via stool-based testing or visual-based screening via a colonoscopy. If someone has risk factors they may need to begin screening at a younger age.
Colorectal cancer can often be preventable through modifiable risk factors. Changing some of these risk factors, alongside the detection and removal of precancerous lesions can lower someone's risks. However, if a diagnosis is made, treatment can help to prolong the life of the patient. The treatment can include various surgeries, chemotherapy, and radiation. All of these treatments can cause changes to a patient's body. A rehab professional that has knowledge about both the body and how the medical treatment of cancer causes changes, can make all the difference in the world for that patient returning to activities that they enjoy and love after treatment.
There are not many opportunities for rehab professionals to learn about these changes and how we can help these patients. However, Herman & Wallace has a series focused on helping oncology patients. In this series, techniques are learned that can help colorectal cancer patients recover from their diagnosis and the medical treatment they go through. The oncology series is online and offered several times a year. You can attend the upcoming oncology courses on: Oncology of the Pelvic Floor Level 1 scheduled for July 8-9 and December 2-3, Level 2A scheduled for May 20--21, and Level 2B scheduled for December 9-10.
Reference:
Morgan E, Arnold M, Gini A, et al. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Colon. 2023; 72(2).
*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2A - partner needed for registration
Price: $495.00 Experience Level: Intermediate Contact Hours: 17.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on male pelvic cancers, colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient's body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: May 20--21
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./