Emily McElrath, PT, DPT, MTC, CIDN is instructing her upcoming course Pregnancy & Postpartum Considerations For High Intensity Athletics scheduled on May 21, 2023. This one-day remote continuing education course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high intensity interval training (HIIT).
Emily is a native of New Orleans and received her undergraduate degree in Athletic Training at the University of Southern Mississippi and went on to receive her Doctorate of Physical Therapy from the University of St. Augustine for Health Sciences. She is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance. Emily is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and Cross-fitter and has personal experience modifying these activities during pregnancy and postpartum.
Introduction: Although routine exercise has long been recommended throughout pregnancy by medical professionals, High Intensity Athletics like Crossfit, weightlifting, and HIIT have received mixed approval amongst healthcare providers. There seems to be limited knowledge on how this form of exercise affects the pelvic floor and abdominal wall throughout pregnancy and postpartum, thus creating a limited understanding of proper recommendations by healthcare providers in regard to how and when a patient can safely continue and/or return to high intensity athletics during pregnancy and postpartum. Unfortunately, some (likely well-intended) medical professionals have gone so far as to instruct their patients to completely avoid these types of exercise throughout pregnancy. But are these limitations really necessary? Does the research support these recommendations? Or is there a way we can help these women continue to safely participate in high intensity athletics throughout pregnancy, and return appropriately in the postpartum phase?
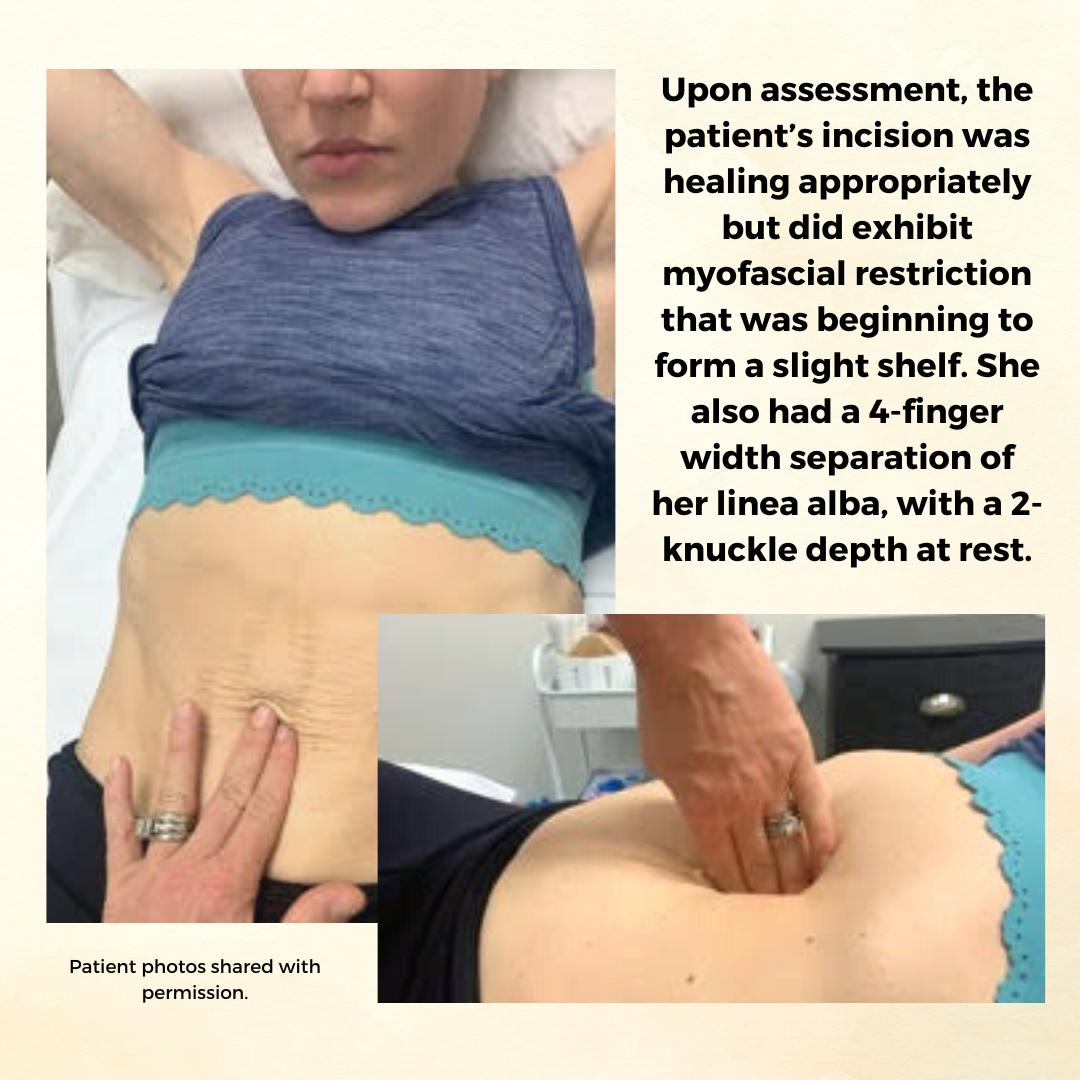
Background: The patient is a 34 y/o female who reported to the Physical Therapy clinic at 2 months postpartum from a cesarean delivery of twins. The patient was seen prior to her delivery (beginning at 24 weeks gestation) to prepare for a vaginal delivery, address chronic constipation, and to receive guidance on how to safely continue Crossfitting during pregnancy. She had been a Crossfitter (5-6 x weekly) for roughly 10 years at the time of her evaluation and was a track athlete and distance runner prior to that. Prior to pregnancy, the patient competed in local and regional Crossfit competitions in the RX division. The patient continued to Crossfit throughout her pregnancy and was able to avoid any pelvic floor dysfunction with proper modification and guidance. The patient returned for postpartum assessment at 8 weeks. At the time of the evaluation, she had begun taking short walks and performing body weight strengthening exercises. Her main concern at the time of the evaluation was a significant diastasis recti (DRA), and a self-reported decrease in core control and awareness. While the patient no longer desired to compete in local or regional competitions, she did want to continue Crossfit 5-6 x weekly and wanted to make sure she was able to safely do so with her DRA. Upon assessment, the patient’s incision was healing appropriately but did exhibit myofascial restriction that was beginning to form a slight shelf. She also had a 4-finger width separation of her linea alba, with a 2-knuckle depth at rest. Initially, the patient was unable to perform a proper transverse abdominus (TrA) contraction and was subsequently unable to create good tension across the gap. She also demonstrated compensatory recruitment of her obliques with attempts to perform a TrA contraction. The patient demonstrated mildly improved TrA recruitment in standing and following treatment, which consisted of myofascial release to her abdominal wall and incision, dry needling to her obliques, and internal trigger point release to her pfm. The pt exhibited limited pfm motor control at the time of her postpartum evaluation, and her PERF score was 2/6/5/2. The pt also exhibited myofascial restriction of her thoracolumbar fascia, proximal adductors, and B glutes. The pt continued to be seen for roughly 1 year following the delivery of her twins. In that time a variety of treatment strategies and techniques were used.
Methods: The methods used to treat this patient included education on proper pressure management strategies (including modification to breathing strategies during exercise), exercise scaling and modification, internal trigger point release to the pfm, followed by neuromuscular re-education once the normal resting tone of the pfm had returned, myofascial release to her abdominal wall and cesarean scar, dry needling, and education on a home exercise program (HEP). The pressure management strategies provided to the patient focused primarily on the various breathing patterns she could utilize to prevent breath holding, improve pelvic floor contraction, and reduce intra-abdominal pressure. The use of the Valsalva was not re-introduced until the patient had normal pfm motor control, exhibited proper tension across her DRA with no evidence of doming or conning, and only in limited circumstances (primarily when the weight was over 80% of her max for that movement). Pelvic floor motor control was assessed via internal palpation, in standing, and with a load (ie back squat and deadlift). Activity modification included modification of the speed of various movements, the load (weight) of various movements, the velocity of various movements (barbell cycling versus slow reps and strict gymnastics versus kipping), and the volume of various movements (number of repetitions or rounds/time of time of a metcon). If the patient’s tissues still could not handle the load with the above modifications, the movement was changed altogether (i.e. mountain climbers versus toe to bar). Measures used to indicate tissue tolerance to the load included: abdominal doming or coning, urinary incontinence, pelvic pain or heaviness, pulling or pain along her incision, and low back pain. If the patient experienced any of these symptoms, the movement was modified until she was able to complete the movement without symptoms. Additionally, the patient received internal trigger point release to the pfm, dry needling to the abdominal wall, glutes, proximal adductors, and lumbar paraspinals, myofascial release to the same muscle groups, neuromuscular re-education, and kinesiotaping to the abdominal wall.
Results: At the time of her discharge, the patient was able to fully return to all desired Crossfit activity. This process took roughly 1 year and required a gradual loading of her tissues through activity modification, to allow them to properly manage the load placed on them. For her, gymnastics movements on the rig took the longest to return to. She did not fully return to these movements (pull-ups, toes to bar, chest to bar pull-ups, and muscle-ups) until roughly 8-9 months postpartum. At the time of her discharge, she was able to create good tension across the gap and had improved her DRA to only less than 1 finger width separation and less than 1 knuckle of depth at rest. When performing a TrA contraction, there was no depth or width of separation. The pt also had an improved PERF score of 5/10+/10/8. The pt exhibited normal pfm motor control and excellent pressure management at the time of discharge.
Conclusion: While there is not a large amount of research available on the effects of high intensity athletics on the function of the pelvic floor and abdominal wall, we are beginning to see an increase in research on new, and more functional approaches to evaluating and treating Diastasis recti (DRA). There has also been a recent increase in research looking at the effects of various breathing techniques during exercise (including the Valsalva) and how it affects both the mother and the baby. Consistent review of the most current research, a thorough understanding of the mother’s anatomy and how it changes during pregnancy and postpartum, as well as each patient’s unique history and goals is necessary for clinicians to provide the highest quality of care for each patient. This is how we can move away from blanketed natal and postnatal exercise recommendations, and develop patient centered, sport-specific treatment plans that will allow each patient safely and effectively participate in high intensity athletics.
Pregnancy & Postpartum Considerations For High Intensity Athletics

Price: $225.00 Experience Level: Beginner Contact Hours: 8.25 hours
Course Dates: May 21, September 10, and November 19
Description: This one-day remote course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high intensity interval training (HIIT). In this cours participants will review the current literature, discuss the unique needs of pregnant and postpartum high intensity athletes, and learn how to most effectively treat these patients as practitioners. The main focus of this course will be to learn how exercising throughout pregnancy, or returning to exercise postpartum may look different for a high intensity athlete versus a non HIIT athlete.
Participants will discuss how anatomical and hormonal changes will affect training for the pregnant and postpartum athlete, and review various modifications for this population. We will also discuss how various stresses placed on the body during these activities may affect pelvic floor muscle function, and review various pressure management strategies that can be utilized during high intensity interval training. The lab will be broken up into pregnancy considerations and postpartum considerations. During the pregnancy lab, we will review specific exercise modifications for pregnancy, utilization of breathwork to properly support the pelvic floor during pregnancy, and review how to assess for and tape for diastasis recti. In the postpartum lab we will review how to determine proper activity modification based on ability to manage pressure, review specific activity modifications and breathwork, review accessory work for return to activity, and discuss how to assess pelvic organ prolapse in standing.