So often as “pelvic floor therapists”, our name and scope of manual treatment can seem to center around stretching or strengthening pelvic floor muscles. But, if you have been practicing for a while, maybe you want to go deeper.
We talk in the Pelvic Function Series about “zooming out” (considering postural, musculoskeletal, breathing, autonomics, and pressure systems). We also have noticed in our field an increased emphasis on the nervous system for regulating the system.
We also talk about “zooming in”, bringing our focus inside the pelvis. That could be pelvic floor muscles, but if we want to zoom in even deeper, we may start to look at peripheral nerves, supportive ligaments, and the interplay between bones, ligaments, fascia, and muscles that could be keeping pain, dysfunction, over-activity, or tension syndromes alive.
The sacrospinous and sacrotuberous ligaments are incredible structures we often don’t give enough attention to. Both the SS and ST ligaments have coccyx attachments and can affect coccyx pain, position, and create tension in the coccygeal nerves.
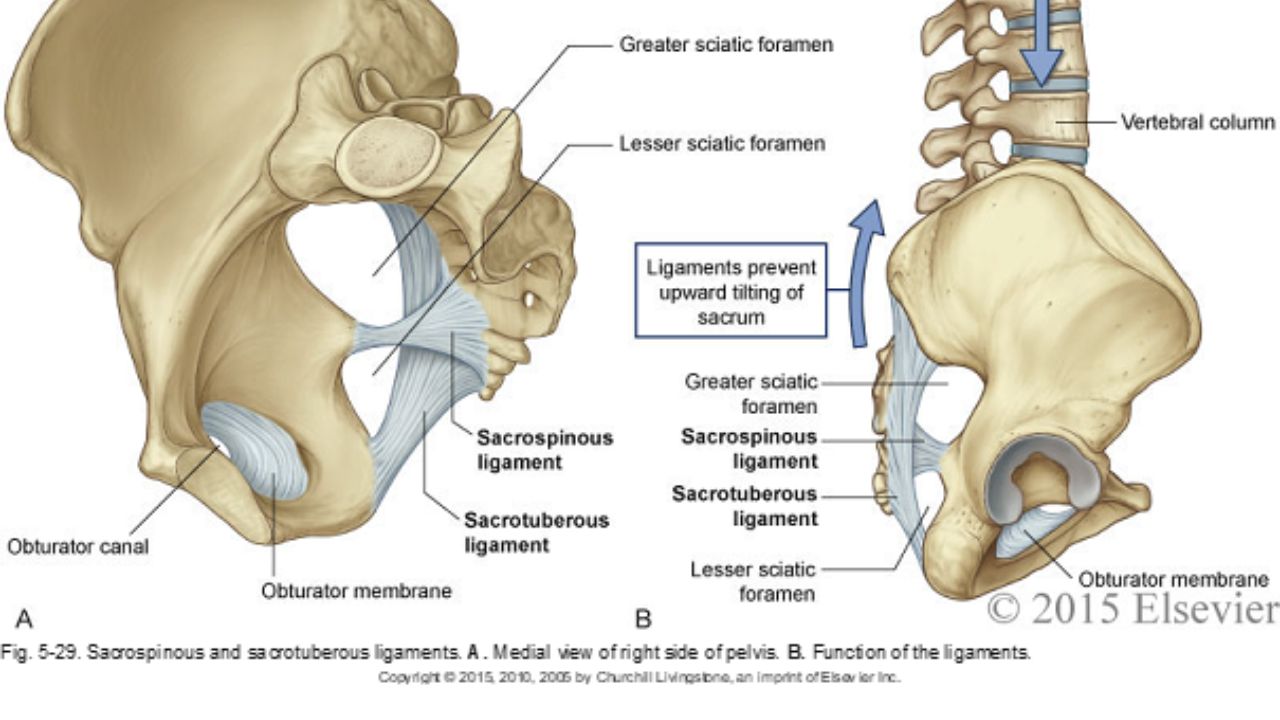
The entire support and structure of the posterior-lateral pelvic bowl is constructed from these two ligaments (with the posterior longitudinal SI ligament). They can become tight and rigid from bearing the burden of stabilizing. The SS ligament may even hold the support for the vaginal canal after hysterectomy. These two ligaments create the greater and lesser sciatic foramen and the nerves of the sacral plexus (pudendal, sciatic, gluteal nerves, and posterior femoral cutaneous nerves) all have intimate relationships and are affected by the tension in these ligaments.
In the Sacral Nerve Manual Assessment and Treatment Class, we learn techniques to deeply release these ligaments (without stressing our hands), external fascial techniques for the coccyx fascia and ligaments, releases for the deep hip muscles that these nerves run through, and how to individually do neuro-lymphatic work to decrease perineural thickening and swelling within the nerve that prevents pain-free gliding. We use differential diagnosis, manual technique, home program, and intricate anatomy study to learn how to get closer to the root of dysfunction in the pelvic floor and posterior gluteals, saddle region, and leg. Come join us on May 11&12 to add depth to your toolbox and understanding of the anatomy of the pelvic nerves.
*Images used with permission from Elsevier 2015.
AUTHOR BIO:
Nari Clemons, PT, PRPC

Nari Clemons was born and raised in the Midwest before moving to Portland, Oregon. At Herman & Wallace, Nari teaches the Pelvic Function Series (PF1, 2A, 2B, and PF Capstone). She was one of three co-authors. Her passion is taking difficult concepts and techniques and simplifying them so that participants can leave courses with confidence, enthusiasm, and feeling empowered in their clinical practice.
Nari graduated from the Medical College of Ohio in consortium with the University of Toledo, with a degree in physical therapy. She owns a private practice, Portland Pelvic Therapy, where she focuses on pelvic, abdominal, and neural issues. Nari has studied visceral and neural manipulation extensively, traveling as far as France to take courses from Jean Pierre Barral. She is also a registered yoga teacher, having trained at the Yoga Center of Seattle and It’s Yoga. Additionally, she has accumulated months of time at intensive meditation retreats. Nari’s approach to the body is holistic and eclectic while being well-rooted in research.