The Untold Story of Nerve Damage with C-section Affecting Diastasis and Persistent Pain
Birthing can be an unpredictable process for mothers and babies. With cases of fetal distress, the baby can require rapid delivery. Alternatively, in cases with cephalo-pelvic disproportion, the baby has a larger head, or the mother has a decreased capacity within the pelvis to allow the fetus to travel through the birthing canal. Additionally, the baby may have posterior presentation, colloquially known as “sunny side up” in which the baby’s occipital bone is toward the sacrum. With any of these situations, it is good to know c-sections are an option to safely deliver the child.
 Women may also be inclined to try to get a c-section to avoid pelvic complication or tears or because of a history of a severe prior tear. As pelvic therapists, we know that the number of vaginal births and history of vaginal tears increase the risk of urinary incontinence and prolapse. Yet, many therapists are unfamiliar with the effects of c-section and the impact of rehab for diastasis.
Women may also be inclined to try to get a c-section to avoid pelvic complication or tears or because of a history of a severe prior tear. As pelvic therapists, we know that the number of vaginal births and history of vaginal tears increase the risk of urinary incontinence and prolapse. Yet, many therapists are unfamiliar with the effects of c-section and the impact of rehab for diastasis.
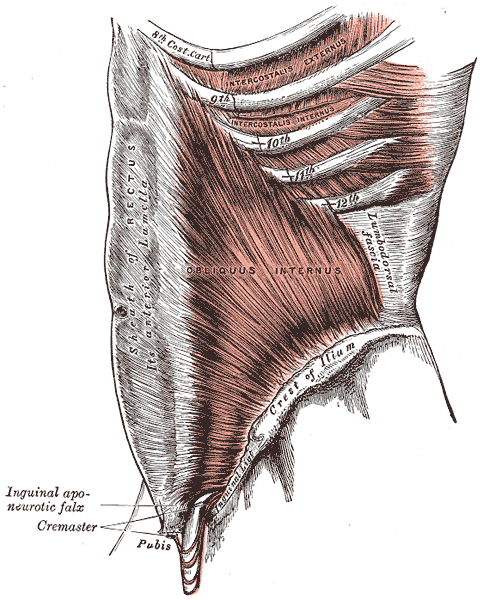
A 2008 dissection study of 37 cadavers studied the path of the ilioinguinal and Iliohypogastric nerves. The course of the nerves was compared with standard abdominal surgical incisions, including appendectomy, inguinal, pfannestiel incisions (the latter used in cesarean sections). The study concluded that surgical incisions performed below the level of the anterior superior iliac spines (ASIS) carry the risk of injury to the ilioinguinal and iloiohypogastric nerves 1. Another 2005 study reported low transverse fascial incision risk injury to the ilioinguinal and Iliohypogastric nerves, and the pain of entrapment of these nerves may benefit from neurectomy in recalcitrant cases.2
Why does injury to the nerves matter? After pregnancy, patients may need rehab and retraining of their abdominal recruitment patterns for diastasis and stability. The ilioinguinal and Iliohypogastric nerves are the innervation for both the transverse abdominus and the obliques below the umbilicus. When we are working to retrain the muscles, certainly neural entrapment or poor firing can greatly impact the success of our intervention as rehab professionals. Interestingly, a study from Turkey showed patients had a significant increase in diastasis recti abdominis (DRA) with a history of 2 cesarean sections and increased parity and recurrent abdominal surgery increase the risk of DRA.2
A fourth study looked at 23 patients with ilioinguinal and Iliohypogastric nerve entrapment syndrome following transverse lower abdominal incision (such as a c-section). In this study, the diagnostic triad of ilioinguinal and Iliohypogastric nerve entrapment after operation was defined as 1) typical burning or lancinating pain near the incision that radiates to the area supplied by the nerve, 2). Clear evidence of impaired sensory perception of that nerve, and 3) pain relieved by local anaesthetic.4
One of the other symptoms we may see in an area of nerve damage is a small outpouching in the area of decreased innervation on the front lower abdominal wall.
So, what can we do with this information? The good news is that as rehab professionals, we can treat along the fascial pathway of the nerve to release in key areas of entrapment. We can mobilize the nerve directly. Neural tension testing can help us differentiate the nerve in question and we can use neural glides and slides after having freed up the nerve from the area of compression. Then, we can increase the communication of the nerve with the muscles by using specific, localized strengthening and stretch in areas of prior compression. All of these techniques are taught in in our course, Lumbar Nerve Manual Treatment and Assessment. Come join us in San Diego May 3-5, 2019 to learn how to differentially diagnose and treat entrapment of all of the nerves of the lumbar plexus.
Okiemy, G., Ele, N., Odzebe, A. S., Chocolat, R., & Massengo, R. (2008). The ilioinguinal and iliohypogastric nerves. The anatomic bases in preventing postoperative neuropathies after appendectomy, inguinal herniorraphy, caesareans. Le Mali medical, 23(4), 1-4.
Whiteside, J. L., & Barber, M. D. (2005). Ilioinguinal/iliohypogastric neurectomy for management of intractable right lower quadrant pain after cesarean section: a case report. The Journal of reproductive medicine, 50(11), 857-859.
Turan, V., Colluoglu, C., Turkuilmaz, E., & Korucuoglu, U. (2011). Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekologia polska, 82(11).
Stulz, P., & Pfeiffer, K. M. (1982). Peripheral nerve injuries resulting from common surgical procedures in the lower portion of the abdomen. Archives of Surgery, 117(3), 324-327.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./








































