So often, we think of vulvodynia as a condition of the skin. And it is….kind of. Vulvodynia is a long-term pain (or burning, discomfort, or itching) that is present in the outer genitals, also known as the vulva. This condition is defined as a discomfort that has lasted longer than 3 months. The symptoms of vulvodynia can vary. In some patients, it is provoked (brought on by touch or stimulation), and in some cases, it is unprovoked (present without stimulation). Some patients have pain just in the outer vulva, while others also present with pelvic floor muscle tension or urethra, bladder, or vaginal canal irritation.
The definition of vulvodynia itself states there is no known reason. This means it is not because of a skin disruption, hormonal disorder, herpes or other skin conditions, or active infection, such as yeast. This means we really don’t know just why a person has symptoms once they have been medically ruled out.
When we look at the symptoms of neuralgia (an irritated or overly talkative nerve), we find symptoms listed such as pain, hypersensitivity, burning, tingling, itching, or trigger points. Certainly, there is a lot of overlap between neuralgia symptoms and vulvodynia symptoms.
When there is compression of a nerve, it can create neuralgia of the affected dermatome. In fact, in studies, we find neural proliferation of the peripheral nerve with vulvodynia in cell biopsy in women or in animal models (1, 2). Often, neural compression is part of the problem, and this is why we see treatment models proving effective at times with nerve blocks or nerve decompression (3, 4).
Of course, when treating such patients, we can and should still employ proven topical agents to make the treatments comfortable and effective, such as lidocaine solutions (5). Vulvodynia is best treated and managed as a team, with manual therapy and patient education from pelvic health providers being a very important limb of treatment.
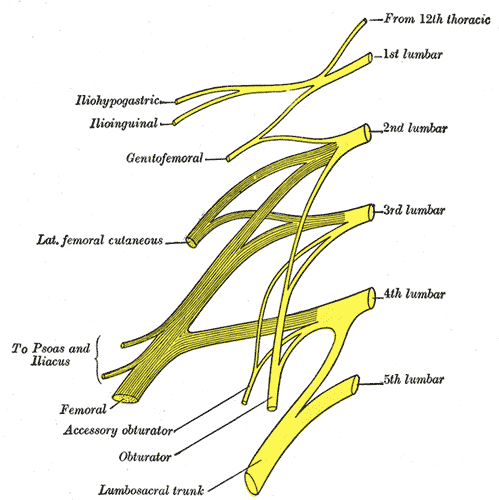
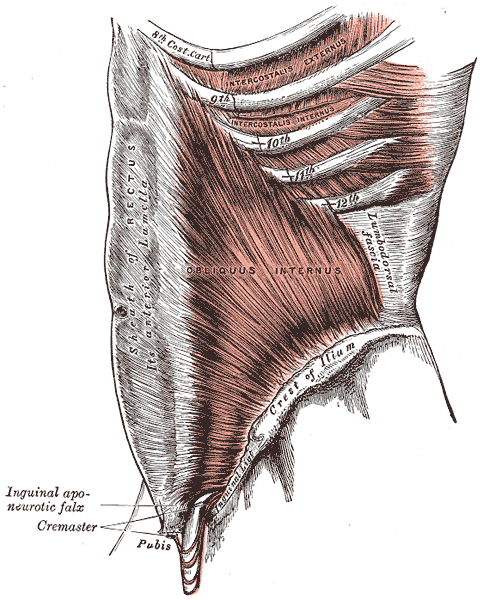
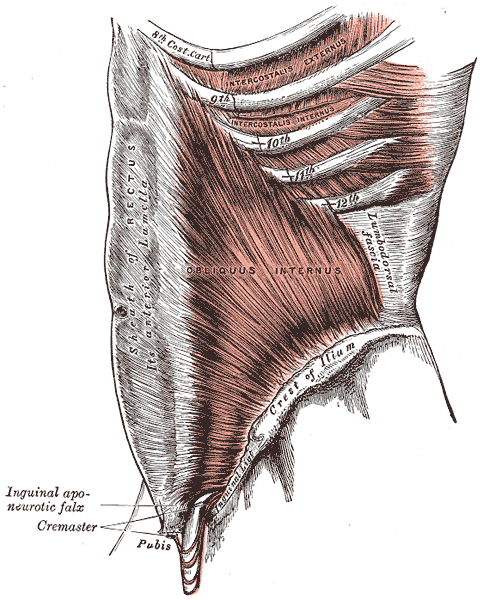
By treating fascial tunnels that nerves run through, treating the fascia around the clitoris, and treating the deep fascia and tissues of the labia majora and mons, we can have an effect on the pudendal nerve branches, as well as the genitofemoral and ilioinguinal nerves supplying this region. In Lumbar Nerve Manual Assessment and Treatment scheduled for May 17-18, and Sacral Nerve Manual Assessment and Treatment scheduled for May 31-June 1, both heavy manual therapy classes, we learn to decompress the neurovascular bundle from proximal to distal and to treat distal soft tissue structures that may be compressing nerves.
Resources:
1. Goetsch MF, Morgan TK, Korcheva VB, Li H, Peters D, Leclair CM. Histologic and receptor analysis of primary and secondary vestibulodynia and controls: a prospective study. Am J Obstet Gynecol. 2010;202:614.e1–614.e8. doi: 10.1016/j.ajog.2010.01.028.
2. Bornstein J. Vulvar disease. Cham: Springer International Publishing; 2019. Vulvar pain and vulvodynia; pp. 343–367.
3. Vulvodynia treatments, National Vulvodynia Association (nva.org)
4. Possover M, Forman A. Pelvic Neuralgias by Neuro-Vascular Entrapment: Anatomical Findings in a Series of 97 Consecutive Patients Treated by Laparoscopic Nerve Decompression. Pain Physician. 2015 Nov;18(6):E1139-43. PMID: 26606029.
5. Loflin BJ, Westmoreland K, Williams NT. Vulvodynia: A Review of the Literature. J Pharm Technol. 2019 Feb;35(1):11-24. doi: 10.1177/8755122518793256. Epub 2018 Aug 20. PMID: 34861006; PMCID: PMC6313270.
AUTHOR BIO:
Nari Clemons, PT, PRPC
 Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment and Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jenna Ross, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jenna Ross. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment and Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jenna Ross, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jenna Ross. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari’s passions include teaching students how to use their hands more receptively and precisely for advanced manual therapy skills while keeping it simple enough to feel successful. She also is an advocate for therapists learning how to feel well and thrive as they care for others, which is a skill that can be developed. “Basically, I love helping therapists learn to help themselves and others more while having a lot of fun doing it.” Nari lives in Portland Oregon, where she runs a local study/mentoring group and has a private practice, Portland Pelvic Therapy. Her interests include meditation, working out, nature, and being constantly humbled from raising her three amazing teenagers!

The pelvis contains several parallel nerve groups. One of which is the lumbar plexus and its sensitive branches. This nerve web arises from the anterior rami of lumbar spinal nerves L1 to L4 and T12 from the thoracic spinal nerve.
Nari Clemons instructs the remote course, Lumbar Nerve Manual Assessment and Treatment, which addresses assessments for the contributory nerves from the lumbar plexus, anatomy, differential diagnosis, and objective findings for specific nerves of the lumbar plexus. This advanced-level course also provides twelve lab techniques for manually treating the nerves of the lumbar plexus.
Peripheral lumbar plexus nerves included in this course are Iliohypogastric, Ilioinguinal, Genitofemoral, Lateral Femoral Cutaneous, Femoral, and Obturator Nerves. These nerves are vital for the functioning of the lower extremities, including maintaining the ability to extend the knee, flex the hip, and adduct the thigh.
When a nerve becomes restricted, it disrupts the nerve signal allowing for symptoms to present as possible pain, weakness, numbness, or tingling. The lumbar plexus is vulnerable to injury when its bony protection, the pelvis, is compromised. Based on research from Anthony Chiodo, retroperitoneal hemorrhage, superior ramus fractures, traction, and penetrating injuries all can cause injury to the lumbar plexus. There are also a variety of conditions such as herniated disc, spinal arthritis, repetitive activities, and even poor posture that can lead to lumbar nerve pain, or a pinched nerve.
Nari explains in the Lumbar Course anatomy lecture that, "Dura matter covers the brain, spinal cord, and peripheral nerve. If you have tension in the peripheral nerves it can cause tension in the central nervous system and vice versa. When working with the nerves it is important to down-train the nervous system. Because the nerves run continuously it is always important to down-train and practice pain theory." She continues to explain that "The osteopathic approach to the fascial system of the peripheral nerve does not have a grounding in scientific research and is based on clinical experience from individuals using peripheral nerve palpation as a method for the evaluation of the nerve's function."
This means that there is not a singular proven technique that is more helpful than another when addressing nerves. The Lumbar Nerve Manual Assessment and Treatment course is essentially a melting pot that pulls from multiple studies and research. The evidence-based, step-by-step approach to treating the lumbar nerve includes
- Decompression to clear the path of the nerve and potential sites of restriction.
- Fascial techniques, just like those that we use with the other fascia of the body.
- Slacking the nerve towards its origin to create ease.
- Gliding the nerve in a pain-free manner.
- Strengthening the weakened muscles.
Differential diagnosis and treatment of these lumbar plexus nerves can allow patients to return to full daily function. Learn manual assessment and treatment techniques from Nari Clemons in the next Lumbar Nerve Manual Assessment and Treatment remote course, scheduled for September 11-12, 2021.
The lumbar sacral nerve plexus can be divided into the direction the nerves travel, either anterior or posterior. This post will focus on anterior hip nerves. I remember writing about the brachial plexus over and over in physical therapy school, but only a few times for the lumbosacral plexus. Patients frequently report anterior hip and pubic pain and can often have signs and symptoms of nerve entrapment. This article orients the reader to links between signs and symptoms and examination to help appropriately diagnosis specific nerves in the athletic population.
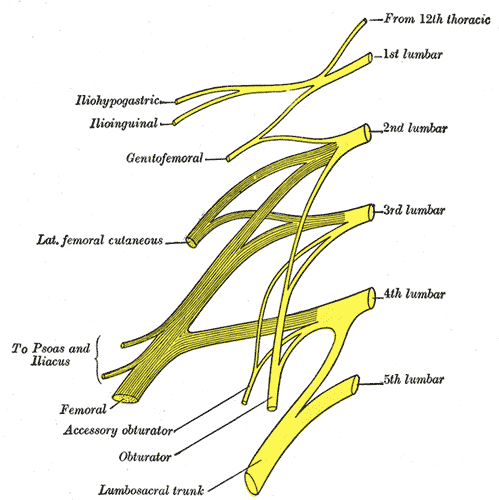 The obturator, femoral and lateral femoral cutaneous are more commonly entrapped in sports injuries. Although the three nerves that travel together through the inguinal canal (ilioinguinal, iliohypogastric, and genitofemoral) are less common, however surgery can create nerve entrapment sequelae.
The obturator, femoral and lateral femoral cutaneous are more commonly entrapped in sports injuries. Although the three nerves that travel together through the inguinal canal (ilioinguinal, iliohypogastric, and genitofemoral) are less common, however surgery can create nerve entrapment sequelae.
There are a few places where the obturator nerve can become squished. Typically, as it leaves the obturator canal which presents at medial thigh pain, and then again in the fascia of the adductors which presents as pain with abduction. The challenge is to differentiate between the nerve and adductor strain. Obturator nerve entrapment will test positive with passive hip abduction and extension, but negative resisted hip adduction.
The femoral nerve can become entrapped in a kind of compartment syndrome as it goes between the psoas and iliacus. This can lead to compression to the neurovascular bundle with resultant swelling, edema, and ischemia. Signs of femoral nerve compression include anterior thigh numbness and paresthesias. Occasionally, this can also include the saphenous nerve with symptoms continuing along medial knee to foot. Femoral nerve entrapment can create quadricep muscle weakness and atrophy, with diminished or absent patella tendon reflexes. Symptoms are reproduced with hip extension and knee flexion thereby elongating the femoral nerve.
The lateral femoral cutaneous (LFC) nerve is sensory. Diagnosed as meralgia paresthetica, the LFC nerve is typically entrapped where it penetrates under the inguinal ligament just medial to the anterior superior iliac spine (ASIS). Symptoms include numbness, tingling, hypersensitivity to touch, burning along outer thigh along the iliotibial band. The LFC nerve can often be compressed by wearing heavy belts (scuba divers, construction belts, etc). Special tests that indicate LFC are pelvic compression in side lying with involved side up to slack the inguinal ligament and Tinels sign.
Anterior hip pain is fairly common in pelvic floor patients. Differential diagnosis and treatment of these anterior nerves can allow patients to return to full daily function. To learn manual assessment and treatment techhniques for the lumbar nerves, consider attending Lumbar Nerve Manual Assessment and Treatment.
Martin R, Martin HD, Kivlan BR. Nerve Entrapment In The Hip Region: Current Concepts Review. Int J Sports Phys Ther. 2017 Dec;12(7):1163-1173.
Birthing can be an unpredictable process for mothers and babies. With cases of fetal distress, the baby can require rapid delivery. Alternatively, in cases with cephalo-pelvic disproportion, the baby has a larger head, or the mother has a decreased capacity within the pelvis to allow the fetus to travel through the birthing canal. Additionally, the baby may have posterior presentation, colloquially known as “sunny side up” in which the baby’s occipital bone is toward the sacrum. With any of these situations, it is good to know c-sections are an option to safely deliver the child.
 Women may also be inclined to try to get a c-section to avoid pelvic complication or tears or because of a history of a severe prior tear. As pelvic therapists, we know that the number of vaginal births and history of vaginal tears increase the risk of urinary incontinence and prolapse. Yet, many therapists are unfamiliar with the effects of c-section and the impact of rehab for diastasis.
Women may also be inclined to try to get a c-section to avoid pelvic complication or tears or because of a history of a severe prior tear. As pelvic therapists, we know that the number of vaginal births and history of vaginal tears increase the risk of urinary incontinence and prolapse. Yet, many therapists are unfamiliar with the effects of c-section and the impact of rehab for diastasis.
A 2008 dissection study of 37 cadavers studied the path of the ilioinguinal and Iliohypogastric nerves. The course of the nerves was compared with standard abdominal surgical incisions, including appendectomy, inguinal, pfannestiel incisions (the latter used in cesarean sections). The study concluded that surgical incisions performed below the level of the anterior superior iliac spines (ASIS) carry the risk of injury to the ilioinguinal and iloiohypogastric nerves 1. Another 2005 study reported low transverse fascial incision risk injury to the ilioinguinal and Iliohypogastric nerves, and the pain of entrapment of these nerves may benefit from neurectomy in recalcitrant cases.2
Why does injury to the nerves matter? After pregnancy, patients may need rehab and retraining of their abdominal recruitment patterns for diastasis and stability. The ilioinguinal and Iliohypogastric nerves are the innervation for both the transverse abdominus and the obliques below the umbilicus. When we are working to retrain the muscles, certainly neural entrapment or poor firing can greatly impact the success of our intervention as rehab professionals. Interestingly, a study from Turkey showed patients had a significant increase in diastasis recti abdominis (DRA) with a history of 2 cesarean sections and increased parity and recurrent abdominal surgery increase the risk of DRA.2
A fourth study looked at 23 patients with ilioinguinal and Iliohypogastric nerve entrapment syndrome following transverse lower abdominal incision (such as a c-section). In this study, the diagnostic triad of ilioinguinal and Iliohypogastric nerve entrapment after operation was defined as 1) typical burning or lancinating pain near the incision that radiates to the area supplied by the nerve, 2). Clear evidence of impaired sensory perception of that nerve, and 3) pain relieved by local anaesthetic.4
One of the other symptoms we may see in an area of nerve damage is a small outpouching in the area of decreased innervation on the front lower abdominal wall.
So, what can we do with this information? The good news is that as rehab professionals, we can treat along the fascial pathway of the nerve to release in key areas of entrapment. We can mobilize the nerve directly. Neural tension testing can help us differentiate the nerve in question and we can use neural glides and slides after having freed up the nerve from the area of compression. Then, we can increase the communication of the nerve with the muscles by using specific, localized strengthening and stretch in areas of prior compression. All of these techniques are taught in in our course, Lumbar Nerve Manual Treatment and Assessment. Come join us in San Diego May 3-5, 2019 to learn how to differentially diagnose and treat entrapment of all of the nerves of the lumbar plexus.
Okiemy, G., Ele, N., Odzebe, A. S., Chocolat, R., & Massengo, R. (2008). The ilioinguinal and iliohypogastric nerves. The anatomic bases in preventing postoperative neuropathies after appendectomy, inguinal herniorraphy, caesareans. Le Mali medical, 23(4), 1-4.
Whiteside, J. L., & Barber, M. D. (2005). Ilioinguinal/iliohypogastric neurectomy for management of intractable right lower quadrant pain after cesarean section: a case report. The Journal of reproductive medicine, 50(11), 857-859.
Turan, V., Colluoglu, C., Turkuilmaz, E., & Korucuoglu, U. (2011). Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekologia polska, 82(11).
Stulz, P., & Pfeiffer, K. M. (1982). Peripheral nerve injuries resulting from common surgical procedures in the lower portion of the abdomen. Archives of Surgery, 117(3), 324-327.
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.

What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
New pain theory also supports that much of pain perception is the body perceiving danger or injury to a nerve. By clearing up the path of the nerve and mobilizing it, we can decrease the body's perception of nerve entrapment and thus create change in pain levels.
What do you hope practitioners will get out of this series that they can't find anywhere else?
I hope they will leave the course able to treat the nerves of the region, which is essentially the transmission pathway for most pelvic pain. I don't know of other courses that have this emphasis.
You've recently split your nerve course in two. Why the split?
I didn't want this class to be a bunch of nerve theory without the manual intervention to make change. After running the labs in local study groups, we found it took more time for people's hands to learn the language, art, and techniques of nerve work. To truly do the work justice and for participants to have a firm grasp of the manual techniques without being rushed, we found it takes time, and I wanted to honor that, as well as treating enough of the related factors and anatomy to make real and lasting change for patients.
How did you decide to divide up content?
Basically, we divided them up by anatomical origin:
The lumbar course covers the nerves of the lumbar plexus, the abdominal wall when treating diastasis, and treatment of the inguinal canal (obturator nerve, femoral nerve, iliohypogastric, ilioinguinal, genitofemoral nerves). Also, the lumbar nerves have more effect in the anterior hip, anterior pelvis, and abdominal wall.
The sacral nerve course covers all the nerves of the sacral plexus (pudendal, sciatic, gluteal/cluneal, posterior femoral cutaneous, sciatic, and coccygeal nerves), as well as subtle issues in the sacral base and subtle coccyx derangement work as well as the relationship with the uterus and sacrum, to take pressure off the sacral plexus. The sacral nerves have more effect in the posterior and inferior pelvis and into the posterior leg and gluteals.
What are the main stories that either course tells?
Both courses tell the story of getting closer to the root of the pain to make more change in less time. Muscles generally just respond to the message the nerve is sending. Yet, by treating the nerve compression directly, we are getting much closer to the root of the issue and have more lasting results by changing the source of abnormal muscle tone. Rather than an intellectual exercise of discourse on nerves, we devote ourselves to the art of manual therapy to change the restrictions on the pathway of the nerve and in the nerve itself.
If someone went to the old nerve course, what's the next best step for them?
The first course was initially all the lumbar nerves with a dip into the pudendal nerve. They would want to take the sacral nerve course, as those nerves were not covered in the first round.
Anything else you would like to share about these courses?
Sure. Essentially, we will take each nerve and do the following:
- Thoroughly learn the path of the nerve
- Fascially clear the path of the nerve
- Manually lengthen supportive structures and tunnels that surround the nerve.
- Directly mobilize the nerve
- Glide the nerve
- Learn manual local regional integration techniques for the nerve after treatment
- Receive handouts for and practice home program for strengthening and increasing mobility in the path of the nerve
Join Nari at one of the following events to learn valuable evaluation and treatment techniques for sacral and lumbar nerves
Upcoming sacral nerve courses:
Sacral Nerve Manual Assessment and Treatment - Winfield, IL
Oct 11, 2019 - Oct 13, 2019
Sacral Nerve Manual Assessment and Treatment - Tampa, FL
Dec 6, 2019 - Dec 8, 2019
Upcoming lumbar nerve courses:
Lumbar Nerve Manual Assessment and Treatment - Phoenix, AZ
Jan 11, 2019 - Jan 13, 2019
Lumbar Nerve Manual Assessment and Treatment - San Diego, CA
May 3, 2019 - May 5, 2019