Treating the nervous system
Recently I had a patient referred to me for fecal incontinence. She looked so familiar to me and we realized she had seen me before, years ago, for bladder issues. She was a sweet 60 something single woman who had raised 6 kids on her own after her husband left her. We laughed as she remembered something funny I had said back then. Then we got down to business. In recent years my patient “Inez” had been diagnosed with both diabetes and Crohn’s disease. She was managing the Crohn’s very well but her sugars were much harder for her to get under control. When I asked her about her current complaints and symptoms she reported that most days her bowels were perfect. She reported one or two soft easy to pass stools per day. But when she had to leave the house for a doctor appointment, she would have explosive diarrhea. This didn’t happen if she went to the grocery store or to visit a friend. Upon further questioning she realized she was really anxious about her diabetes and her interactions with her medical provider regarding her diabetes had not been positive. She felt frustrated, scared, and powerless. 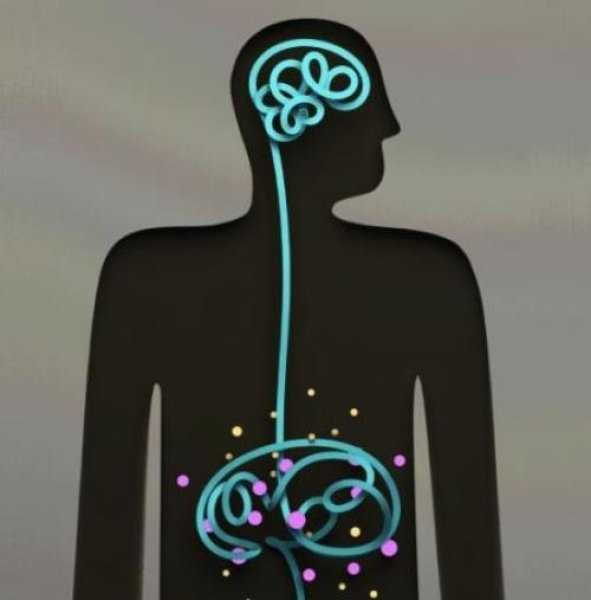
As a pelvic health PT I could have treated Inez in a variety of ways. With my initial exam I did not see any glaring musculoskeletal issues. I suggested to Inez the possibility that her nervous system was sending the wrong kind of signals to her bowels when she got anxious and that we could address this in PT. Inez agreed that she would like to try this approach. We decided that we would reevaluate after four visits to see if we needed to change the plan. Over four visits I used craniosacral therapy protocols to address nervous system upregulation and tension. I taught Inez relaxation techniques and encouraged 10 or 15 minutes of daily relaxation practice. Inez opened up about her relationship with her kids and how they tended to be takers but not givers. She would get frustrated and feel a bit used at times. We had conversations about boundaries and saying “no” and I shared some of my own experiences and struggles as well. Lastly we talked about how what we think can affect how we feel and what we do. Inez’s faith was important to her. She found a few bible verses that were meaningful to her about fear and anxiety and would repeat those during her daily relaxation time. On her fourth visit, Inez was all smiles. She brought me a jar of her homemade salsa as a graduation present. As we sat down to talk she reported to me that she saw her doctor yesterday. She had no bowel issues. And more than that, as her doctor began to talk over her she said to him, “No. Stop. You are always talking and never listening. I need you to listen to me today.” She went on to explain to him how it worried her that she was not able to control her diabetes well and she didn’t think he was doing enough to help her. Her physician did stop and listen and asked Inez, “what would you like me to do for you?” She asked for a referral to a specialist and he obliged. Inez was thrilled that she was able to manage her anxiety in a way that helped her bowels and to find the courage to confront her doctor to get the care she felt she needed.
As we grow in the knowledge of how the human body works it seems like all roads lead back to the nervous system. All of our treatments and interactions with patients affect the nervous system in one way or another. In our fast paced, stressed out world, finding ways to be intentional in addressing the nervous system can be a game changer for patients (as well as for ourselves). If this is an area you would like to grow in, please consider a new course being offered this January in Tampa, Florida. Participants taking Holistic Interventions and Meditation will experience and explore evidence-based information on strategies to address the nervous system. Topics covered include practical meditation, use of essential oils, supplements, yoga, calming and centering manual techniques and instruction in how to best dialogue with patients struggling with pain, anxiety and the effects of trauma. Nari Clemons and I hope to see you there.
Faurot, K. K. R., Gaylord, S., Palsson, O. S., Garland, E. L., Mann, J. D., & Whitehead, W. E. (2014). 715 Mindfulness Meditation Has Long-Term Therapeutic Benefits in Women With Irritable Bowel Syndrome (IBS): Follow-Up Results From a Randomized Controlled Trial. Gastroenterology, 146(5), S-124.
Kearney, D. J. (2012). Mindfulness meditation for women with irritable bowel syndrome–evidence of benefit from a randomised controlled trial. Evidence-based nursing, 15(3), 80-81.
Keefer, L., & Blanchard, E. B. (2001). The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behaviour research and therapy, 39(7), 801-811.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./



































