Nari Clemons - Actually, I used to have a meditation and neuroscience class for Herman Wallace. It was a shorter class. But, I felt it was lacking in tools for the provider. For example, as an empathic provider, I felt I was very aware, very mindful that I was losing energy, that I was "picking things up" from my patients, and that I was really not enjoying my job or life balance as much as I used to. I became ill and burnt out, working in this intensive field. It felt like the joy of my life was kind of being sucked up by my job. Jen and I launched our own journeys, together, trying to understand how this world of boundaries and balance could help us in our own lives. So much changed and grew from that. So, in time we decided to combine the two into one class, to help practitioners integrate meditation into their practice and life, but also how to come back to loving their jobs with balance, as we were able to.
What are the top 3 takeaways a practitioner could hope to gain from this class?
NC - 1. Better self-care in and out of the clinic. 2. A more effective and less taxing way to interact with clients, share responsibility, and communicate in more helpful ways for both practitioner and patient. 3. enjoying their life and having more energy for their life outside of work.
JVV - 1. You don’t have to do it all. 2. We want to support you with tools to help your patients take more responsibility for their care and their outcomes. 3. YOU ARE VALUABLE…and here are ways you can care for yourself, have healthy boundaries, and align your actions with your priorities so you can leave work at work and truly enjoy your life outside of work.
Who do you think needs to take this class?
NC - Any practitioner who is finding work more and more emotionally taxing or draining. Really, there are a few patterns that benefit from this class. People who over-give and over-function in relationships in their life, including patient relationships. Often there can be a bit of a people-pleasing tendency in these situations. Also and especially if a participant is one of those people who have always been a little sensitive to energy: feel things, pick up things, notice their energy changes when they interact with others. I feel like this is the only class I know of that specifically gives tools and strategies for this kind of provider.
JVV - EVERYONE! LOL. People who are wrestling with healthy work/life balance, who find themselves staying late after work or working through lunch, health care providers who tend to care more for their patients than they do for themselves, those of us who leave work drained and only have meager offerings of energy for our families.
What was your favorite feedback from participants in taking this class?
NC - We hear a lot from participants that other classes made them have better clinical skills, but this class has helped them to enjoy their own life and their job more and to feel more balanced and professional as they employ better boundaries and shared responsibility.
JVV - Ahhh, it is true joy when participants are empowered and equipped to set healthy boundaries, care for themselves, and feel more joy in their lives.
How is this class different from other classes through H&W?
NC - Kind of along the same lines, this class does give you skills for use with patients, but they are the skills that help your life feel better, and your job feels better. They give you permission to change your paradigm of treatment from "how much can I possibly give" to "how do I shift my job, self, and communication, to allow my job to be just one part of my life that is enjoyable and doesn't take so much energy away from the other parts of my life."
JVV - This is the only class that focuses both on skills to use for patients and skills to use FOR YOURSELF. To keep yourself healthy, balanced, and whole as a medical provider in a demanding, challenging role.
Why are there two parts to this class?
NC - Because it is a lot of information, a lot of life changes to integrate. It takes time. We like the idea of a month of growth and change. Participants do pre-work to prepare for the first weekend, which starts the process of change. Then, they do work in the following month and really work on the intensive integration, new habits, new patterns, and new neuronal networks. Then, we come back for another day for the second part of learning that participants will be ready for after integrating some of the basics of the first weekend.
JVV - We just had SO MUCH we wanted to share!! And we found having two classes spaced a month or so apart really lets participants ingest and apply one level of change before being ready and hungry for the next level. The first part focuses on establishing good boundaries with patients, self-care practices including meditation, and identifying areas of their lives that need support or intervention to be healthier. The second class dives deeper into thoughts, emotions, and actions. Practices like gratitude, visualization, and deeper mediation practices.
Boundaries, Self-Care, and Meditation - Part 1
Course Dates: March 18
Price: $400
Experience Level: Intermediate
Contact Hours: 12.5
Description: The instructors recommend completing this series in two parts to allow time to process and implement one leg of the journey before undertaking the next. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Please plan for up to 12 hours of pre-course work. This sets the stage for you to find your path to experiencing more joy, energy and balance.
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focus on the neuroscience of pain trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values, as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.
This week Jennafer Vande Vegte and Nari Clemons sat down to share their course Boundaries, Self-Care, and Meditation with us to give a peek into the why, what, and how of it all.
What are boundaries? Boundaries are when we need to set a limit. It’s that capacity to say here’s where I need to draw the line so that I stay grounded and centered and feel good about myself. Self-care is what we do to replenish those energy reserves every day. To replenish our joy. To replenish our sense of awe and gratitude. Then meditation is a beautiful way to rewire the brain. To get to the reasons and roots of why we are getting depleted, we need to have a high level of honesty and introspection.
This is a course that gives you that permission and a lot of tangible tools. Nari shares that students have told her that "all of the other courses give us manual skills, but this course changed my life." Jen adds to this, "BUT you got to put in the work. This course is science and research-based and used in a way to transform lives." Part one is a deep dive into the science of the brain. Pain, trauma, PTSD and how that changes the brain, and how that has changed the brains of patients and of us. Meditation practices are explained from a scientific perspective about how they can come in and rewire the nervous system and help your patterns.
Part two is about a month later and gets a little bit softer. In this portion, Nari and Jenn focus on relationships, not just with our patients but with ourselves and the people that we love in our lives. How to construct healthy relationships and build that patient shared responsibility model in our practices. They also dive into the visualization of what we want in our practices and lives, self-care, and meditation. The course comes to a close with case studies and an action plan to bring what you’ve learned into the clinic. They’ve also established an online network where you can sign up for continued community. We’re all going through this journey together.
Boundaries, Self-Care, and Meditation Part 1 is scheduled for April 24th.
Boundaries, Self-Care, and Meditation Part 2 is scheduled for June 12th.

Part 1: Burnout
Let’s get real for a minute.
You are a highly educated professional. If you are reading this blog, I can assume you are invested in your career and your continued education. You are probably pretty skillful, and you help a lot of people.
BUT
How are you doing once you leave work?
Does your life outside of work give you joy and fulfillment?
Or do you leave your work setting completely drained, snippy with your loved ones, and too tired to care for yourself?
You have at least one advanced degree, probably some certifications, but did anyone ever teach you how to get your paperwork done on time?
Or how to leave work at work and not have your patients popping into your head day and night?
What about energy conservation? In fact, we may have been taught to give our ALL to work, to our patients, to strive for productivity and accomplishment. But where does that leave us?
BURNED OUT.
Part 2: Mindset
Taking continuing education classes was my pathway to becoming a better physical therapist.
But I had to go to therapy to learn how to survive as a physical therapist.
There were struggles.
Paperwork. I could NEVER finish in a timely way.
Timeliness. I was OFTEN running behind for patients.
Discharge. I had some patients for YEARS because I did not know how to discharge them even though they weren’t getting better. They depended on me, and I also depended on them.
Boundaries. I had none.
And here’s something that surprised me.
I had to change the way I THOUGHT before I could change my BEHAVIOURS.
I had to change my mindset.
I used to show up at work with the idea of Helping People. I felt responsible for their outcomes. If they weren’t doing well, I assumed I was missing something.
The shift looked like this:
I can show up at work to coach people who are responsible for their own outcomes. If they aren’t doing well, we can have honest communication about next steps (medical or otherwise), discharge, or resistance.
My patients are not my family, they are not my friends. I show up as a coach who is very interested in understanding their story and helping them reach their goals through a shared responsibility model of care.
My free time is sacred. I need to protect it for my mental, physical, spiritual, and emotional health. Because I am a priority, I will use 5 minutes of each treatment session to complete the patient’s treatment by doing paperwork.
Now, therapy is INVALUABLE. Don’t get me wrong, but paperwork, timeliness, discharge, and healthy boundaries are things MANY of us struggle with. So Nari Clemons and I designed a Continuing Education COURSE. We believe that therapists deserve to learn skills to preserve our wellbeing and strengthen our resilience against burnout.
Especially since the pandemic, more and more health care workers are reporting very high levels of burnout. Nari Clemons and I went through a period of burnout earlier in our careers. The tools and techniques we learned to heal ourselves and develop new patterns of delivering care are powerful. We know you might also be struggling and we want to help. So we developed a course to equip you. We would love to learn with you at Boundaries, Self-Care, and Meditation. A two-part, online journey toward experiencing a practice you enjoy and a life you love.

Boundaries, Self-Care, and Meditation is a two-part series intended to be completed in order. Participants should register for Part 1 and Part 2 at the same time, or complete Part 1 and wait to complete Part 2 at a later date. This course was developed by Nari Clemons, PT, PRPC, and Jennafer Vande Vegte, PT, PRPC and was "born out of our own personal and professional struggles and our journey to having a life and a practice that we love and can sustain." The intention of this class is deep, personal, and professional transformation through evidence-based information and practices. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Nari shares that "This sets the stage for you to find your path to experiencing more joy, energy, and balance."
Boundaries, Self-Care, and Meditation - Part 1 - Remote Course
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focusing on the neuroscience of pain, trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course
Part Two continues the focus on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". Course discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.
A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Tory Pines State Park provided much needed rejuvination. Ahh sea air.
2. Self-care is mandatory:
We spent Friday relaxing at a beautiful resort in Del Mar. We are learning we don’t need to justify or feel bad about caring for ourselves. It’s necessary and important. We are responsible for meeting our own needs and for refueling ourselves when we provide care for others.
3. Get out of your comfort zone:
The robes we got from the resort were super cozy and it was chilly on the beach, so why not walk the beach in a robe? We laughed at ourselves and others laughed at us and with us. But we were comfy and warm.
4. Do the work when it is time to do the work:
Instead of thinking and talking about the course all day we committed ourselves to being in the moment. When it came time to discuss the details of the next three days, a plan came together with relative ease. This is us working at the resort.
5. Challenges can change your perspective. And a change in perspective can help you with challenges:
This is a (terrible, sorry) picture of us interrupting our morning run to climb a tree. It was a fun challenge and gave us an interesting perspective on our day.
A little more about the course. Woah. The people who showed up came with open minds and hearts, ready and ripe for change. We had powerful times of sharing, listening, learning, and supporting. Meditation and yoga and a healing, honest and real atmosphere brought about transformation in the most beautiful awe-inspiring way. We were profoundly moved. The changes Nari suggested were PERFECT and I was grateful for her innovations. We were all pretty much out of our comfort zones, but that is where change happens.
In the words of one student, “This course couldn’t have come at a more appropriate time because I was in major burnout. I was becoming an unhappy person both professionally and personally. I needed to make a change. Now I am leaving this course empowered to care for myself so I can help patients in a healthy way and enjoy my job again. I am walking away from this course with so many valuable strategies and also feel so much more relaxed and hopeful”
6. Be silly sometimes:
Laugh a lot. Especially at work. Play jokes, have fun. You know what they say about all work and no play. Play.
7. At the end of the day Shake it off (and use pain science as needed):
Our last day we took a run to the beach. When crossing a rail line I tripped and bashed the HECK out of my lower leg. Since I could still run I repeated the mantra “Hurt not harm!!” (which we discuss in class) with great vigor until the throbbing subsided, and we enjoyed a beautiful sunset and the conclusion of our time in San Diego.
Last words of Wisdom:
Gratitude can change us in powerful ways.
A huge and heart felt thank you to Herman & Wallace, our host site, and for each and every participant. We couldn’t do what we do without you and for this we are eternally grateful.
Thank you. Thank you. Thank you.

Part 3: Carefully Choosing to Say Yes or No (or The Summer that Almost Wasn’t)
*Disclaimer: this essay is meant to be read in a voice of complete transparency and humility.
 Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Rewind a bit. Two years prior I also got a call. Would I be interested in writing a chapter in a Urology textbook on alternative care for pelvic pain conditions…edited by and partnering with a big name in pelvic floor rehab? Oh yes indeed I would! I have always dreamed of seeing my name in print. Was I scared out of my mind? Heck yes! I was working 20 hours a week, part time home schooling my girls and teaching for Herman & Wallace. I had one day a week to myself for cleaning, errands, the occasional book reading or interacting with friends. I decided I could spend my next year of Fridays researching, writing and editing said chapter. Oh, I also started therapy for the anxiety increase that came with the project. My therapist suggested I hire help with house cleaning, which I did. She also suggested meditation, mindfulness and using essential oils. I opted not to enact these suggestions. It was a crazy year, but I learned a ton and was proud of my contribution to the publication.
In the brief time that I caught my breath from the book chapter, I was invited to be part of the team writing the Pelvic Floor Capstone course. What an honor! I had always wanted to try writing a course and this would be a perfect opportunity to collaborate with others on such a big project. I committed, worsening my anxiety with heart palpitations which escalated to a level that required medication. My Fridays and evenings were again occupied for quite some time. Luckily, I still had the cleaning help and the therapist which were really just the skinniest strings that were maintaining my sanity.
While teaching our first Capstone class, although both of us were struggling with burnout, Nari Clemons and I had a moment of euphoria, seeing everything come together and watching students learn. We decided we would design and write another course and put together an outline and a plan for Boundaries, Self-Care and Meditation.
I think you might be getting a picture of my prior lifestyle. If there was time, I filled it. If there was an opportunity, I took it. If I did something once, I could do it again. But applying the concepts of our boundaries course to myself changed everything.
Nari and I knew we were burning out and needed change. I have always had anxiety, but it had escalated to the point of requiring both therapy and medication. I was giving my all, my best, to everyone else and my family got my scrappy leftovers, the worse of me. I had been functioning in these patterns my whole life and had no idea how to get off the hamster wheel.
As we developed Boundaries, Meditation and Self Care I became my own research study, incorporating the material we would be teaching into my own life. I finally started setting priorities and boundaries that helped put my family first and give them the best of me. I said no to a variety of opportunities that I then delegated to colleagues who were delighted to step up. I started meditating, practicing mindfulness and using essential oils as part of my self-care as my therapist suggested a year ago. I even enrolled my kids in full time school for the upcoming year. I was feeling so much better!
So when the next call came, I was prepared.
The editor and famous pelvic floor PT I had worked with on the book chapter was in need of an editor for an article that was going to be published in a medical journal. There was a lot of editing that needed to be done and time was of the essence. My contribution as editor would list me as a co-author. How many of you also dream of seeing your name attached to an article in a peer reviewed medical journal? Because of what I had learned through therapy and practiced with meditation I had the ability to pause, reflect, and make an informed choice that considered how this opportunity lined up with my priorities. I replied with much gratitude for the offer, but this time I said no. It was difficult to say no, and I had to work through some regret, but in the end I made the right choice and we had a great summer.
Life is funny sometimes and lessons in humility are plentiful. Back track again to when the urology text came out a few years ago. I excitedly ordered a print copy. When I opened to the chapter which I contributed, I discovered another person’s name had accidently been printed where mine should have been. The mistake was corrected for the ebooks but more paper copies were not printed. I may never see my name in print, but the Summer That Almost Wasn’t taught me that there are more important things in life.
If you find yourself struggling with boundaries, saying no, and prioritizing the things that are important to you personally and as a therapist, know that you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject or taking Boundaries, Meditation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Meditation and Self Care this November 9-11, 2019 in San Diego, CA.
Most clinicians will agree that stress can amplify a patient’s pain and slow recovery. Mindfulness training provides patients with the ability to self-regulate their stress reaction and has been shown to reduce pain and depression and improve quality of life in patients with chronic pain conditions.1 The growing popularity of meditation training to manage stress has led to an increased interest in the physiological mechanisms by which meditation influences the body’s stress reaction. A systematic review and meta-analysis examined the results of randomized controlled trials that compared the impact meditation interventions to active control groups on stress measures. 2 Forty-five studies were included. Meditation practices examined were focused attention, open monitoring and mantra repetition. Outcome measures studied were cortisol, blood pressure, heart rate, lipid and peripheral cytokine expression. Studies had diverse participants including healthy adults, undergraduate students, army soldiers, veterans, cancer survivors, and individuals with chronic pain conditions, cardiovascular disease, depression and hypertension.
 When all meditation forms were analyzed together, meditation reduced blood cortisol, C-reactive protein, resting and ambulatory blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha. The effect of meditation on:
When all meditation forms were analyzed together, meditation reduced blood cortisol, C-reactive protein, resting and ambulatory blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha. The effect of meditation on:
- Cortisol and resting heart rate was considered to be high level of evidence.
- C-reactive protein, blood pressure, triglycerides and tumor necrosis factor-alpha was considered to be moderate level of evidence.
Analyzed individually:
- Open monitoring meditation reduced ambulatory systolic blood pressure, systolic blood pressure following a stress test and resting heart rate. Effects assessed as providing moderate level of evidence.
- Focused awareness reduced blood cortisol and resting systolic blood pressure. Effects assessed as providing low level of evidence.
- Mantra repetition reduced systolic blood pressure. Effects assessed as providing low level of evidence.
Authors report the primary reason for downgrading the grade of evidence when analyzing meditation practices individually was the limited number of studies available and small sample sizes. They conclude overall, when compared to an active control (relaxation, exercise or education) meditation practice leads to decreased physiological markers of stress in a range of populations.
Carolyn will offer her popular course, Mindfulness-Based Pain Treatment, in Portland OR, July 27 and 28 and again in Houston TX, October 26 and 27. We recommend these unique opportunities to train with Carolyn, a nationally recognized leader trailblazing the successful applications of mindfulness into pain treatment and the field of physical therapy. Hope to see you there!
1. Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199-213.
2. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J Psychiatr Res. 2017;95:156-78.
The following is the first in a series on self-care and preventing practitioner burnout from faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC. Jennafer is the co-author and co-instructor of the Boundaries, Self-Care, and Meditation course along with Nari Clemons, PT, PRPC.
Part 1: Boundaries
“I just want you to fix me.” How many times have we heard this statement from our patients? And how do we respond? In my former life as a “rescuer” this statement would be a personal challenge. I wanted to be the fixer, find the solution and identify the thing that no one else had seen yet. Then, if I am being completely honest, bask in the glory of being the “miracle worker” and “never giving up” on my patient.
 If you recognize that this attitude was going to run me into some problems, kudos to you. If you are thinking, “well of course, isn’t that your job as a pelvic floor physical therapist?” Please read on.
If you recognize that this attitude was going to run me into some problems, kudos to you. If you are thinking, “well of course, isn’t that your job as a pelvic floor physical therapist?” Please read on.
On my very first job performance review, when it came time to discuss my problem areas my supervisor relayed I was “too nice” and cited some examples: giving a patient a ride home after therapy (it was raining and she would have had to wait for the bus), coming in on Saturdays to care for patients (he was sick and couldn’t make it in during the week but was making really good progress). You get the picture. At the time, I didn’t understand how this could be something I needed to work on. I was going above and beyond and I got so much satisfaction from taking care of others!
Fast forward 10 years and add to my life a husband, two daughters, a teaching job, part time homeschooling, and writing course material. I was an emotional mess. Anxiety was my permanent state of mind. I gave my best to my patients while my family got my meager emotional leftovers. Something had to change and luckily it did. I got help and learned exactly what boundaries are and how to develop as well as enforce them.
There are several resources that discuss professional boundaries in health care, like this from Nursing Made Incredibly Easy. In this particular article, health care professionals are exhorted to stay in the “zone of helpfulness” and avoid becoming under involved or over involved with patients. Health care professionals are also urged to examine their own motivation. Am I using my relationship with my patient to fulfill my own needs? Am I over involved so that I can justify my own worth?
Here are some warning signs that you are straying away from healthy boundaries with patients and becoming over involved:
- Discussing your intimate or personal issues with a patient
- Spending more time with a patient than scheduled or seeing a patient outside of work
- Taking a patient's side when there's a disagreement between the patient and his or her close relations
- Believing that you are the only health care member that can help or understand a patient
For some people, certain patients who push professional boundaries will cause the therapist to feel threatened and under activity is the result. This might result in talking badly about the patient to other staff, distancing ourselves, showing disinterest in their case, or failing to utilize best care practices for the patient.
Per Remshard 2012, “When you begin to feel a bit detached, stand back and evaluate your interactions. If you sense that boundaries are becoming blurred in any patient care situation, seek guidance from your supervisor. A sentinel question to ask is: ‘Will this intervention benefit the patient or does it satisfy some need in me?’”
Healthy professional boundaries are imperative for us and for our patients. Boundaries also help prevent burnout. Remshard delineates what healthy boundaries look like:
- Treat all patients, at all times, with dignity and respect.
- Inspire confidence in all patients by speaking, acting, and dressing professionally.
- Through your example, motivate those you work with to talk about and treat patients and their families respectfully.
- Be fair and consistent with each patient to inspire trust, amplify your professionalism, and enhance your credibility.
If you struggle with professional and personal boundaries, you are not alone and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject or taking Boundaries, Self-Care, and Meditation, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Self-Care, and Meditation this November 9-11, 2019 in San Diego, CA.
Look forward to my next blog where The Rescuer (me) needs Rescuing and learn about the Drama Triangle.
Remshardt, Mary Ann EdD, MSN, RN "Do you know your professional boundaries?" Nursing Made Incredibly Easy!: January/February 2012 - Volume 10 - Issue 1 - p 5–6 doi: 10.1097/01.NME.0000406039.61410.a5
While my dad was visiting Michigan, we had the day to ourselves as my kids were in school. I was so excited to have quality time with my dad. Unfortunately it was pouring down rain. We decided on a leisurely brunch and then a movie. Dad chose the movie, “Wind River.” While not a movie I would normally pick, I was happy to go along. A little more than half way through…there was a horribly violent scene against a young women. I panicked, plugged my ears and closed my eyes. Unfortunately some images were burned into the back of my mind. When the movie was over, I remained seated and tears just came. My dad held me while I cried. I was able to calm down and leave the theater, but the images continued to bother me. During the next few days, I made it a priority to care for myself and allow my nervous system to process and heal.
 What happened to me? I have never had any traumatic personal experience. Why did I react so strongly? I talked with my therapist about it and she suggested I might have experienced secondary traumatic stress. We know, as pelvic health therapists, we need extra time to hear the “stories” of new patients. We do our best to create a safe space for them so they can trust us and we can help them discover pathways to healing. Yet no one has taught us what we are supposed to do with the traumatic stories our patients share. How are we to cope with holding space for their pain? How do we put on a happy face as we exit the room to get the next patient?
What happened to me? I have never had any traumatic personal experience. Why did I react so strongly? I talked with my therapist about it and she suggested I might have experienced secondary traumatic stress. We know, as pelvic health therapists, we need extra time to hear the “stories” of new patients. We do our best to create a safe space for them so they can trust us and we can help them discover pathways to healing. Yet no one has taught us what we are supposed to do with the traumatic stories our patients share. How are we to cope with holding space for their pain? How do we put on a happy face as we exit the room to get the next patient?
Teaching Capstone over the last few years, Nari Clemons and I have talked with many of you who were feeling emotionally overloaded especially when treating chronic pelvic pain and trauma survivors. Some of you were experiencing job burnout, others were deciding maybe it was time for a career shift, away from the pelvis. We realized something needed to be done as our field was losing talented pelvic health therapists. We have also struggled ourselves with various aspects of our profession.
There are no studies that directly look at job burn out, secondary traumatic stress, and compassion fatigue among pelvic health physical therapists. Yet these problems are common among social workers, physicians and other people groups in health care. There are individual as well as institutional risk factors that lead to the development of each. The solution, as one self-help module puts it, is developing resilience. A large part of this skill is making self-care a priority. The basics such as adequate sleep, nutrition, and exercise are foundational. Meditation, mindfulness, therapy, and spiritual practices, as well as supportive friends/groups are also imperative.
Nari and I realized that training to develop resilience in therapists was missing. Initially we equipped ourselves to have better boundaries, ground ourselves with meditation, mindfulness and exercise, which enhanced our skills in dealing with complex, chronic patients. We compiled what we have learned and want to share it with you. We would like to invite you to attend Holistic Interventions and Meditation: Boundaries, Self-Care, and Dialogue. We have designed this 3 day course to be partially educational and absolutely experiential. We are going to dig deeper into ways to calm our patient’s and our own nervous systems, explore and practice the latest recommendations on treatment of persistent pain, we will mediate and learn about mediation, play with essential oils, learn some new hands on techniques, and support and encourage one another as we build communication skills. We want you to leave feeling refreshed and equipped to continue to treat patients without losing yourself in the process. We want to invest in you so you can continue the investment you have made in your career and avoid job burnout, compassion fatigue and secondary trauma. We invite you to develop the resilience you need for a rewarding career in pelvic health physical therapy by joining us in Tampa this January.
Cieslak, R., Shoji, K., Douglas, A., Melville, E., Luszczynska, A., & Benight, C. C. (2014). A meta-analysis of the relationship between job burnout and secondary traumatic stress among workers with indirect exposure to trauma. Psychological services, 11(1), 75.
Meadors, P., Lamson, A., Swanson, M., White, M., & Sira, N. (2010). Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress. OMEGA-Journal of Death and Dying, 60(2), 103-128.
Sodeke-Gregson, E. A., Holttum, S., & Billings, J. (2013). Compassion satisfaction, burnout, and secondary traumatic stress in UK therapists who work with adult trauma clients. European journal of psychotraumatology, 4(1), 21869.
Stearns, S., & Benight, C. C. (2016). Organizational Factors in Burnout and Secondary Traumatic Stress. In Secondary Trauma and Burnout in Military Behavioral Health Providers (pp. 85-113). Palgrave Macmillan US.
Recently I had a patient referred to me for fecal incontinence. She looked so familiar to me and we realized she had seen me before, years ago, for bladder issues. She was a sweet 60 something single woman who had raised 6 kids on her own after her husband left her. We laughed as she remembered something funny I had said back then. Then we got down to business. In recent years my patient “Inez” had been diagnosed with both diabetes and Crohn’s disease. She was managing the Crohn’s very well but her sugars were much harder for her to get under control. When I asked her about her current complaints and symptoms she reported that most days her bowels were perfect. She reported one or two soft easy to pass stools per day. But when she had to leave the house for a doctor appointment, she would have explosive diarrhea. This didn’t happen if she went to the grocery store or to visit a friend. Upon further questioning she realized she was really anxious about her diabetes and her interactions with her medical provider regarding her diabetes had not been positive. She felt frustrated, scared, and powerless. 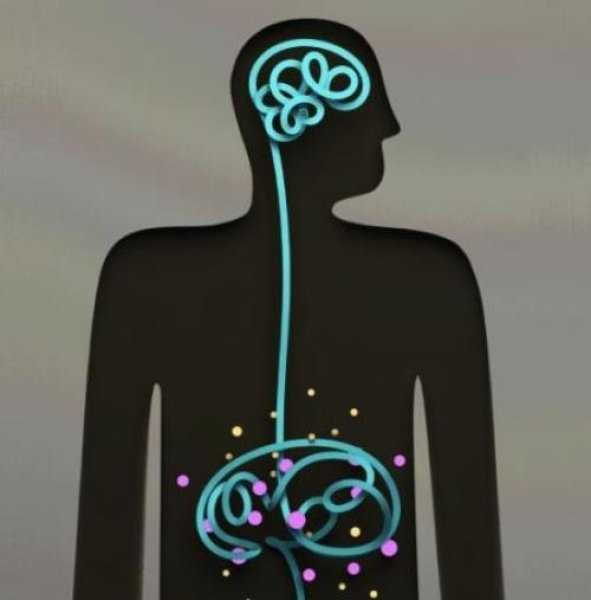
As a pelvic health PT I could have treated Inez in a variety of ways. With my initial exam I did not see any glaring musculoskeletal issues. I suggested to Inez the possibility that her nervous system was sending the wrong kind of signals to her bowels when she got anxious and that we could address this in PT. Inez agreed that she would like to try this approach. We decided that we would reevaluate after four visits to see if we needed to change the plan. Over four visits I used craniosacral therapy protocols to address nervous system upregulation and tension. I taught Inez relaxation techniques and encouraged 10 or 15 minutes of daily relaxation practice. Inez opened up about her relationship with her kids and how they tended to be takers but not givers. She would get frustrated and feel a bit used at times. We had conversations about boundaries and saying “no” and I shared some of my own experiences and struggles as well. Lastly we talked about how what we think can affect how we feel and what we do. Inez’s faith was important to her. She found a few bible verses that were meaningful to her about fear and anxiety and would repeat those during her daily relaxation time. On her fourth visit, Inez was all smiles. She brought me a jar of her homemade salsa as a graduation present. As we sat down to talk she reported to me that she saw her doctor yesterday. She had no bowel issues. And more than that, as her doctor began to talk over her she said to him, “No. Stop. You are always talking and never listening. I need you to listen to me today.” She went on to explain to him how it worried her that she was not able to control her diabetes well and she didn’t think he was doing enough to help her. Her physician did stop and listen and asked Inez, “what would you like me to do for you?” She asked for a referral to a specialist and he obliged. Inez was thrilled that she was able to manage her anxiety in a way that helped her bowels and to find the courage to confront her doctor to get the care she felt she needed.
As we grow in the knowledge of how the human body works it seems like all roads lead back to the nervous system. All of our treatments and interactions with patients affect the nervous system in one way or another. In our fast paced, stressed out world, finding ways to be intentional in addressing the nervous system can be a game changer for patients (as well as for ourselves). If this is an area you would like to grow in, please consider a new course being offered this January in Tampa, Florida. Participants taking Holistic Interventions and Meditation will experience and explore evidence-based information on strategies to address the nervous system. Topics covered include practical meditation, use of essential oils, supplements, yoga, calming and centering manual techniques and instruction in how to best dialogue with patients struggling with pain, anxiety and the effects of trauma. Nari Clemons and I hope to see you there.
Faurot, K. K. R., Gaylord, S., Palsson, O. S., Garland, E. L., Mann, J. D., & Whitehead, W. E. (2014). 715 Mindfulness Meditation Has Long-Term Therapeutic Benefits in Women With Irritable Bowel Syndrome (IBS): Follow-Up Results From a Randomized Controlled Trial. Gastroenterology, 146(5), S-124.
Kearney, D. J. (2012). Mindfulness meditation for women with irritable bowel syndrome–evidence of benefit from a randomised controlled trial. Evidence-based nursing, 15(3), 80-81.
Keefer, L., & Blanchard, E. B. (2001). The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behaviour research and therapy, 39(7), 801-811.
Help others by helping ourselves
As pelvic rehabilitation practitioners, we have all been there, looking ahead to see what patients are on our schedules and recognizing that several will require immense energy from us… all afternoon! Then we prepare ourselves, hoping we have enough stamina to get through, and do a good job to help meet the needs of these patients. Then we still have to go home, spend time with our families, do chores, run errands, and have endless endurance. This can happen day after day. Naturally, as rehabilitation practitioners, we are helpers and problems solvers. However, this requires that we work in emotionally demanding situations. Often in healthcare, we experience burnout. We endure prolonged stress and/or frustration resulting in exhaustion of physical and/or emotional strength and lack of motivation. Do we have any vitality left for ourselves and our loved ones? How can we help ourselves do a good job with our patients, but to also honor our own needs for our energy?
 How do we as health care practitioners’ prevent burnout?
How do we as health care practitioners’ prevent burnout?
Ever hear of “mindfulness” ... I am being facetious. The last several years we have been hearing a lot about “mindfulness” (behavioral therapy or mindfulness-based stress reduction) and its positive effects in helping patients cope with chronic pain conditions. Mindfulness is defined as “the practice of maintaining a nonjudgmental state of heightened or complete awareness of one's thoughts, emotions, or experiences on a moment-to-moment basis,” according to Merriam-Webster’s Dictionary. One can practice mindfulness in many forms. Examples of mindfulness-based practice include, body scans, progressive relaxation, meditation, or mindful movement. Many of us pelvic rehabilitation providers teach our patients with pelvic pain some form of mindfulness in clinic, at home, or both, to help them holistically manage their pain. Whether it is as simple as diaphragmatic breathing, awareness of toileting schedules/behavior, or actual guided practices for their home exercise program, we are teaching mindfulness behavioral therapy daily.
Why don’t we practice what we preach?
As working professionals, we are stressed, tired, our schedules too full, and we feel pain too, right? Mindfulness behavioral therapy interventions are often used in health care to manage pain, reduce stress, and control anxiety. Isn’t the goal of using such interventions to improve health, wellness, and quality of life? Mindfulness training for healthcare providers can reduce burnout by decreasing emotional exhaustion, depersonalization, and increasing sense of personal accomplishment. Additionally, it can improve mood, empathy for patients, and communication.1 All of these improvements, leads to improved patient satisfaction.
Let’s take what we teach our patients every day and start applying it to ourselves. An informal way to integrate mindfulness is by building it into your day. Such as when washing hands in between patients, or before you walk into the room to greet the patient. However, sometimes we have a need for a tangible strategy to combat stress and the desire to be guided by an expert with this strategy.2 I think one of the easiest ways to begin practicing mindfulness is to try a meditation application (app) on a smart phone or home computer. Meditation is one of the most common or popular ways to practice mindfulness and is often a nice starting point to try meditation for yourself or to suggest to a motivated patient. Many popular guided meditation apps include Headspace, Insight Timer, and Calm, just to name a few. Generally, these guided meditation apps have free versions and paid upgrades. Challenge yourself to complete a 10-minute guided meditation app, daily, for three weeks, and see how you feel. It takes three weeks to make a new habit. Hopefully, guided meditation will be a new habit to help you be present with your patients and improve your awareness and energy. After all, how can we help others heal, if we can’t help ourselves?
To learn more about ways, you as a professional can help yourself or your patients with meditation, consider attending Meditation for Patients and Providers.
1)Krasner, M.S., Epstein, R.M., Beckman, H., Suchman, A.L., Chapman, B., Mooney C.J., et al. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 302(12):1284–93.
2)Willgens, A. M., Craig, S., DeLuca, M., DeSanto, C., Forenza, A., Kenton, T., ... & Yakimec, G. (2016). Physical Therapists' Perceptions of Mindfulness for Stress Reduction: An Exploratory Study. Journal of Physical Therapy Education, 30(2).