Aparna Rajagopal, PT, MHS, WCS, PRPC, Capp-OB Certified is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interest in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction.
Leeann Taptich DPT, SCS, MTC, CSCS leads the Sports Physical Therapy team at Henry Ford Macomb Hospital where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
Aparna and Leeann co-authored the course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Abdominal bloating and distension are two very commonly reported GI symptoms in the pelvic practice setting. However, these symptoms are not commonly recognized in other physical therapy settings. While many people experience occasional bloating/discomfort it does not necessitate medical intervention, but repeated and long-standing bloating/distention can impact the quality of life.
One diagnosis which is associated with these symptoms is Abdomino-Phrenic dyssynergia where patients develop a paradoxical abdomino-phrenic response. Normally, as a response to an increase in intraluminal gas, the diaphragm relaxes, and the abdominal musculature contracts. When dyssynergia is present, the opposite happens and the diaphragm contracts, and the abdominals relax. Abnormal pelvic floor function is also associated with this diagnosis. Treatments typically used are biofeedback therapy and breathing techniques.
Where Leeann and I work, we are seeing patients increasingly referred with this diagnosis. Recently we treated a 72-year-old female patient with a long-standing history of troublesome bloating and distention, with the diagnosis of Abdomino phrenic dyssynergia.
- The patient had complaints of bloating and abdominal distension all day long, worsening toward evening
- She reported limiting her food intake in the evenings on account of the discomfort and "tightness" in the abdomen
- She rated the discomfort as 3-5/10 in the morning time with an increase to 8/10 by late evening
- She also reported poor sleep because of how "hard and tight" the abdomen felt by bedtime
Upon examination, amongst other findings, the patient demonstrated:
- Significant tightness in her posterior chain and her erector spinae in both thoracic and lumbar regions
- Decreased thoracic rotation/mobility
- Increased connective tissue restrictions in both upper abdominal quadrants, especially in the epigastric area and inferior to the rib cage
- Decreased lower rib cage mobility
- Poor ability to prolong exhale or to exhale strongly
- Decreased ability to relax the pelvic floor musculature after a contraction
In addition to biofeedback and visceral mobilizations, treatment techniques included joint mobility techniques inclusive of simple rib and thoracic spine mobilizations, soft tissue mobility techniques including gentle diaphragm releases, breath training, and breathing techniques to aid in pelvic floor relaxation.
The patient received 9 treatment sessions and a home maintenance program which she followed with good compliance. She reported a 70% overall improvement and was now able to sleep through the night and eat in the evenings without discomfort.
In our course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, you will learn:
- Explain normal diaphragmatic breathing and the role of the internal and external oblique musculature.
- Assess and treat dysfunctional breathing patterns including but not limited to chest, abdominal, and paradoxical breathing patterns.
- Understand the concept of Intra-Abdominal Pressure (IAP) and the control and use of IAP with the diaphragm in a lowered position as a stabilizing mechanism for the spine.
- Understand the concept of regional interdependence and its application in the treatment of back or pelvic pain patients.
- Recognize the effects of postural patterns and the linkage to the diaphragm and pelvic floor.
- Understand the muscles and myofascial components involved in dysfunctional breathing and techniques to effectively treat the same.
- Understand and demonstrate mobilizations of the rib and thoracic spine and develop a comprehensive treatment program.
- Develop an exercise progression for dysfunctional breathing for use in the clinic and in-home programs.
- Integrate diaphragmatic breathing and mobility in the athletic clientele

Course Dates: April 22-23
Price: $450
Experience Level: Beginner
Contact Hours: 14
Description: This remote course is an integrated approach where participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes while looking at structures from the glottis and the cervical region to the pelvic floor.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. Instructed techniques are applicable to patients who present with Diastasis Rectus Abdominis, pelvic pain, incontinence, and prolapse, as well as cervical, thoracic, scapular, and lumbar pain.
The following is part three in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part One and Part Two of the patient case study on the Pelvic Rehab Report. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
 On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
“Well, there’s another important component to that- one that we call optimal alignment. When we sit or stand in a flexed posture, those two opposing forces do not line up well and can put undue stress and pressure on our body, particularly the vertebral bodies.” I showed her the spine again with an increased flexion (hyper-kyphosis) in the thoracic area. “It’s normal to have a kyphosis in the thoracic spine. What we don’t want is a hyper-kyphosis. We often see the apex of the increased curve around T-7, 8, 9 levels near the bra line. We also call it the “slouch line” because from the front, that’s where we slouch in sitting. A thoracic hyper-kyphosis can lead to hyper-lordosis in the lumbar spine as the body tries to counteract the flexion forces above with extension or arching in the low back. We know that Wolff’s Law states that bone in a healthy person will adapt to the loads under which it is placed.1 But we want those loads to be optimally transmitted; otherwise the adaptation can be problematic.”
With Maryanne sitting in a Perch Posture position on the side of the low mat table, I placed a 4 foot dowel rod alongside her back, touching her sacrum and apex of her thoracic curve. I instructed her to bring her occiput back toward the dowel without extending her neck. I wanted her to do more of a cervical retraction move. She was a good 3+ inches away. Previously I had measured her using the WOD (Wall to Occiput Distance).2 This helps patients understand when they are forward flexed in the upper thoracic and cervical area and becomes an exercise as well. Since Maryanne was not safe in a standing position, we used an armless chair against the wall. I turned it sideways so the side of the chair was snugged up to the wall and transferred her to the chair, sitting so that her sacrum was flush against the wall. “Bring your upper back against the wall without allowing your low back to arch forward”, I told her as I placed a folded towel behind her head. “Now you’re going to press the back of your head into the towel, just as you do when lying down in the Re-alignment routine. Before you perform the Head Press, inhale to prepare, start your exhale, then do the head press. Hold for 3 -5 seconds as you continue to exhale, then relax as you inhale. Do 3-5 reps.”
The Head Press in standing, (or in Maryanne’s case, sitting) is a convenient way to not only strengthen the back muscles isometrically, but also increase awareness of body in space and relationship of head to trunk positioning. For any individual who has developed a forward head position over a period of years, there is a loss of the proprioceptive feedback necessary to know when we’re not in alignment, even if we have the ROM to achieve it. And often a lack of strength and especially muscle endurance to maintain that optimally aligned position is problematic. Using the wall several times a day can assist in building strength and awareness. In Maryanne’s case we needed a folded towel behind her occiput to give her something to press into and prevented her from going into increased cervical extension.
“I still want you to do the Head Press in supine as part of the Re-alignment routine everyday”, I told her. “But also practice it in sitting against a wall, making sure your sacrum is right up against it. Do this several times a day for several minutes, holding 3-5 seconds each. And be sure to use your breath to maintain neutral alignment of your lumbar spine.”
And with that, our work for the day was done.
1. Wolff's Law and bone's structural adaptations to mechanical usage: an ... https://www.ncbi.nlm.nih.gov/pubmed/8060014
2. Concurrent Validity of Occiput-Wall Distance to Measure Kyphosis in Communities. Journal of Clinical Trials. May 18, 2012 Sawitree Wongsa1,4, Pipatana Amatachaya2,4, Jeamjit Saengsuwan3,4 and Sugalya Amatachaya1,4*
The following is part two in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part one of the patient case study on the Pelvic Rehab Report here. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
On Maryanne’s second visit, she reported she had been doing her “homework” and didn’t have any questions. Just to be sure, we reviewed them and I had her demonstrate. In Decompression position, she was lying supine with her hands on her abdomen, a common mistake I see. Usually this is due to tightness in pec minor with protracted scapulae. Patients unknowingly resort to the path of least resistance to take the strain off of the muscles. I explained to her that we want to use gravity to gently lengthen those muscles and “widen” the collarbones to allow for improved alignment. With her shoulders abducted to approximately 30 degrees and palms up, I propped a couple of small towels under her forearms which allowed her shoulders to relax into a more posterior and correct position.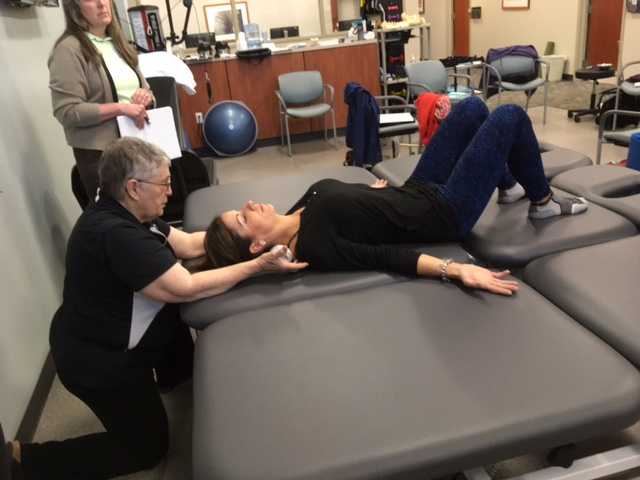
“Today we begin the Re-alignment routine,” I said, “starting with the Shoulder Press.” I showed her how to gently press the back of her shoulders down into the mat without arching her lumbar spine. “As you press your shoulders down, exhale through your mouth as if you’re fogging a mirror. This will help activate your core muscles to keep your back in good alignment. Hold for 2-3 seconds, and then relax. Repeat 3 times.” Maryanne looked at me as if I’d lost my mind. “Did you say do 3 reps?” she asked. “I do 2 sets of 20 reps at the gym,” she said with obvious pride in her voice. “Yes, that’s where we start, and there are a couple of reasons. First, these are very site specific exercises which focus on the exact areas that need strengthening. Exercises done in a gym setting are often more general and usually involve compensation. We are minimizing any compensation such as allowing your low back to arch. There is probably weakness in those upper back muscles as well as the tightness seen in your anterior chest muscles and we need to go slowly. Also, we are simultaneously stretching while we strengthen. Our society is so forward biased (we work on computers, drive cars, make beds, eat- it’s all forward, forward, forward), that the anterior muscles get tight and the upper back muscles get overstretched and weak. We need to reverse that pattern. Take a look at our younger population and their texting postures. Yikes! We will be layering on more exercises as your technique improves so you’ll be doing more than just 3 reps, I promise.”
After the Shoulder Press we proceeded with the Head Press, Leg Lengthener and Arm Lengthener, spending time to make sure her cervical spine stayed in neutral as she pressed her head down into the mat. Head Press (cervical retraction) performed in supine allow patients to have something to press against and helps inhibit the tendency to move into cervical extension. It can also be done standing against the wall with a small pillow or folded towels between the occiput and the wall.
We ended with Maryanne in standing at the kitchen sink to promote functional activities and weight bearing positions. I reminded her to do the Foot Press through the floor using the Triangle of Foot Support visual. This helped to elongate her spine. “Imagine a bungie cord running from the top back of your head to the ceiling” I said which further increased her standing height. “Now I want you to imagine a shelf running straight out from your breastbone with a glass of some very expensive fine drink sitting on it. Do not spill your libation! Oh, and one last thing Maryanne. Breathe!!!” At which point she collapsed into laughter and our session was over. “Busted”, she said.
The following case study comes from faculty member Deb Gulbrandson, PT, DPT, a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method. Join Dr. Gulbrandson in The Meeks Method for Osteoporosis on September 22-23, 2018 in Detroit, MI!
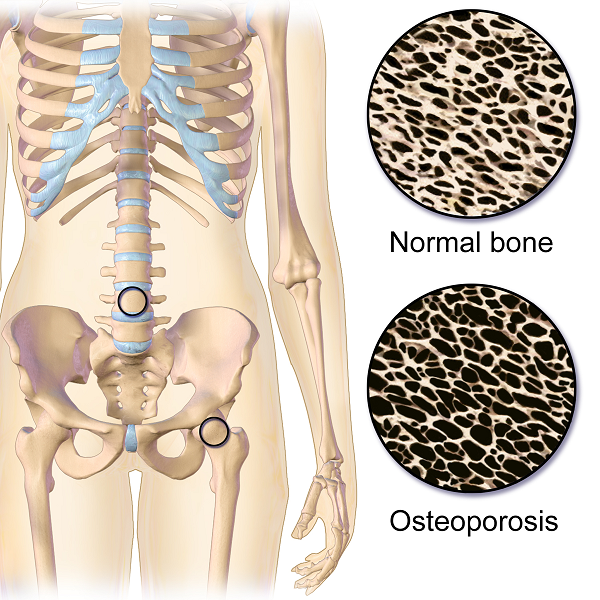
The first sight I had of my new patient was watching her being wheeled across the parking lot by her husband. A petite 72-year-old, I could see her slouched posture in the wheelchair. With the double diagnosis of osteoporosis and Multiple Sclerosis (MS) it didn’t look good. However, “Maryanne“ greeted me with a wide grin and a friendly, “I’m so excited to be here. I’ve heard good things about this program and can’t wait to get started.“
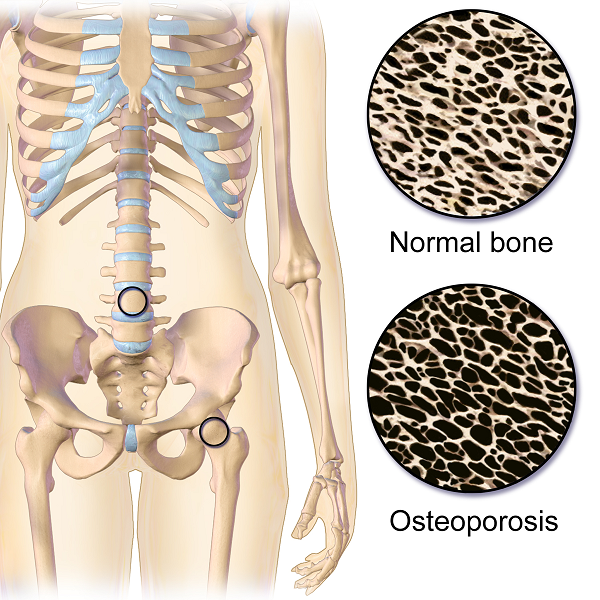 That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
Even though she had been exercising on a regular basis, she was unfortunately doing many of the wrong exercises. Her workout consisted of sit-ups and crunches. She used the Pec Deck bringing her into scapular protraction and facilitating forward flexion. She was also stretching her hamstrings by long sitting reaching to touch her toes.
Spinal flexion is contraindicated in patients with osteoporosis. A landmark study done in 19841 divided a group of women with osteoporosis into 4 groups. One group performed extension based exercises, a second group did flexion. A third group used a combination of flexion and extension and the fourth was the control and did no exercises. Below are the results 1-6 years later.
- Extension Group: 16% incidence of fracture or wedging of vertebral bodies
- Flexion Group: 89% rate.
- Combination Extension/Flexion: 53% rate
- No Exercise Group: 67%
The results were astounding. Granted, it was a small study- 59 participants and it was done a long time ago. But this is a one study that no one wants to repeat, or volunteer for!
Several take home messages followed this study.
- Flexion is contra-indicated for individuals with osteoporosis.
- It’s better to do no exercise than the wrong exercise. The No Exercise group faired better than the Flexion group although at 67% it’s clear that many of our everyday activities- making beds, placing items on low shelves, and now computing and texting put us at risk.
Sadly, many individuals with osteoporosis are told by their physicians to start exercising.......but without any guidance they do what Maryanne did. Just start exercising. And putting themselves at greater risk.
Maryanne was also doing nothing to strengthen her back extensors and scapular area. After giving an overview of the vertebral bodies, pelvis, and hip joint with my trusty spine, I showed both my patient and her husband how forward flexion puts increased compression on the anterior aspect of the spine, particularly in the thoracic curve at T 7, 8, 9, the most common site of compression fractures. We started with Decompression, which is the beginning position for the Meeks method. Many therapists know this as hooklying. This position allows the spinous processes to press against the hard surface of the floor, opening up the anterior portion of the spine and providing tensile forces throughout the length of the spine. With the help of her husband, Maryanne could get down on the floor but I often advise patients who are unable to safely transfer to the floor to lay across the end of their bed. This is less cushy than lying longways where they sleep. Adding a yoga mat or a quilt on top to give more firmness improves the effect.
Supine is the least compressive of all positions; sitting is the most compressive. While Decompression may not seem like much of an exercise it is vital to reduce the effects of gravity and compression on the spine.
We addressed sitting posture by firming up the base of her wheelchair as well as recommending transferring into other chairs and positions frequently throughout the day. Spending time sitting towards the edge of a firm chair in what we call Perch Posture and practicing Foot Presses into the floor created improved alignment in her spine as well as isometrically activating glutes, abs, quads. Using the Foot Press is an example of Newtons 3rd Law, “For every action there’s an equal and opposite reaction” so by pressing her feet down she actually lengthened her torso and head. We also discussed discontinuing the contraindicated exercises in her workout routine and I assured her that the Meeks method would progressively challenge her core (the reason everyone thinks they should do sit-ups) and target the right muscles to help strengthen her bones. We use site specific exercises to target certain muscles that pull on the bone and increase bone strength.2
With instructions to Decompress several times daily to reduce compression on the spine along with the other adjustments made, I felt Maryanne was on her way to reducing her risk of fracture and increasing the quality of her life. She thanked me profusely for the education and the exercise of that session. We both look forward to the next one.
1. Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984 Oct;65(10):593-6.
2. Frost HM1. Wolff's Law and bone's structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64(3):175-88.
 Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Do you ever have patients where you feel stuck, who are not progressing as you would like them to in treatment? We all do! It is frustrating, isn’t it? The physical therapist called me and asked me to evaluate the patient using real-time ultrasound imaging. The therapist said “If the patient can just see what she is doing, she will then be able to learn how to work the muscles correctly.” She referred the patient to me so I could use ultrasound imaging within the treatment to better assess her activation strategies and use the imaging for biofeedback for with the patient. The patient was amazed with the ability to see what the different layers of muscles were doing. We found she was contracting her TA but only on her left side, and her deep multifidus was not firing at all. Using the ultrasound images, the patient was able to learn the proper way to activate her muscles. She is now working on a strengthening program for her local core muscles including her TA, pelvic floor, and multifidus. Within two treatments, the patient was able to fire her muscles in a different way and reports her back has felt better than it has in years!
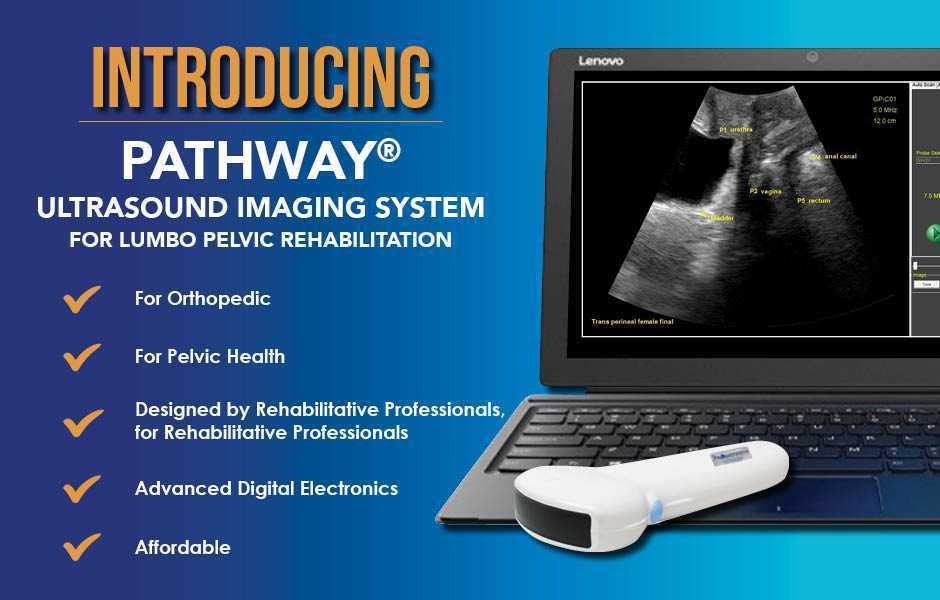
The Pathway Ultrasound Imaging System, available from The Prometheus Group, is a portable ultrasound solution for pelvic rehab
I cannot emphasize enough how using ultrasound might change your practice! It not only can help you when you are stuck with a patient’s progress, but it can attract more patients to your practice. There are a lot of visual learners out there and access to visual images in therapy can influence progress and the results that are achieved. You not only can use the ultrasound to retrain the local core muscles for back and pelvic instability patients, but you can use it for incontinence patients, prolapse patients, and post prostatectomy patients as well. You can strengthen the pelvic floor without having to disrobe the patient each visit. How many men and women would appreciate that?
If you are interested in learning more about how you can use ultrasound in your practice, join me in August in New Jersey, or in November in California for Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics! See you there!
Recently, I had a patient present to my practice with unretractable vaginal pain that was causing her quite a bit of suffering. Peyton (name changed) had been referred by a local osteopathic physician. For around a year, she had increasing severe vaginal pain. There was no history of assault, trauma, fall, or injury around the time of onset of symptoms. However, she had a kidney infection that caused back pain in the month prior to her pain onset.
 Peyton is home schooled, but she was unable to attend outings that required longer sitting, such as field trips or church. She also was having some urinary retention with start and stop stream and resultant urinary frequency. Peyton’s mother said the pain was distressing to Peyton and would cause her to cry. She had an unremarkable medical history. However, under further questioning, we discovered she did have a history of bed wetting later than usual (until age 7) and she had persistent leg pain. With standing longer than 15 minutes, her legs would hurt and feel weak, which prevented her from performing sports or being physically active. She also had experienced some achy low back sensations since the kidney infection. Peyton had been screened by urology, her primary care, an osteopath, as well as a vulvar pains specialist who diagnosed her with nerve pain, but said there is no good viable treatment.
Peyton is home schooled, but she was unable to attend outings that required longer sitting, such as field trips or church. She also was having some urinary retention with start and stop stream and resultant urinary frequency. Peyton’s mother said the pain was distressing to Peyton and would cause her to cry. She had an unremarkable medical history. However, under further questioning, we discovered she did have a history of bed wetting later than usual (until age 7) and she had persistent leg pain. With standing longer than 15 minutes, her legs would hurt and feel weak, which prevented her from performing sports or being physically active. She also had experienced some achy low back sensations since the kidney infection. Peyton had been screened by urology, her primary care, an osteopath, as well as a vulvar pains specialist who diagnosed her with nerve pain, but said there is no good viable treatment.
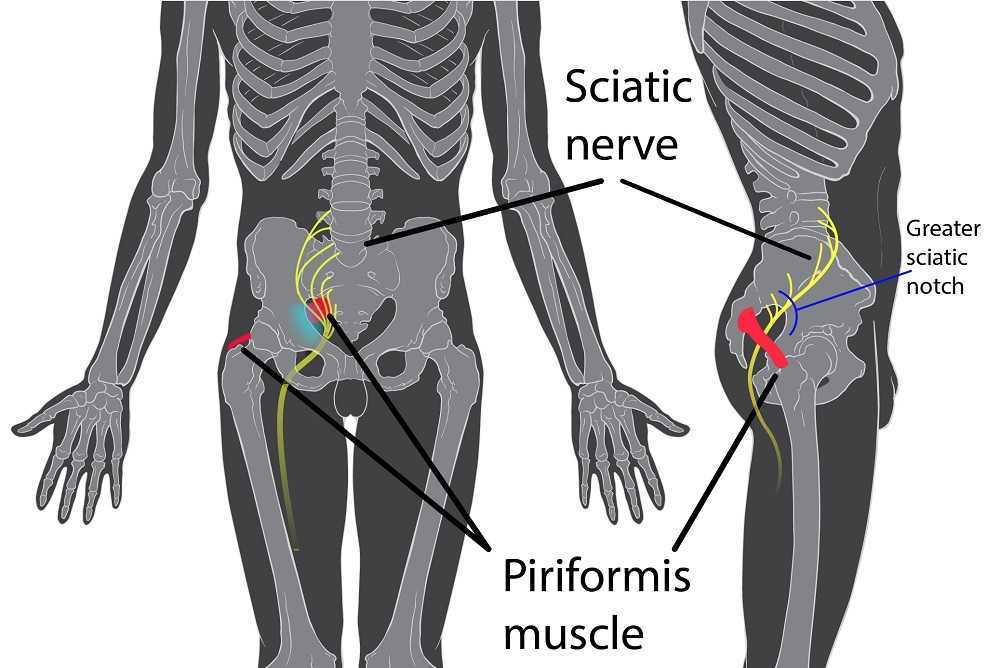
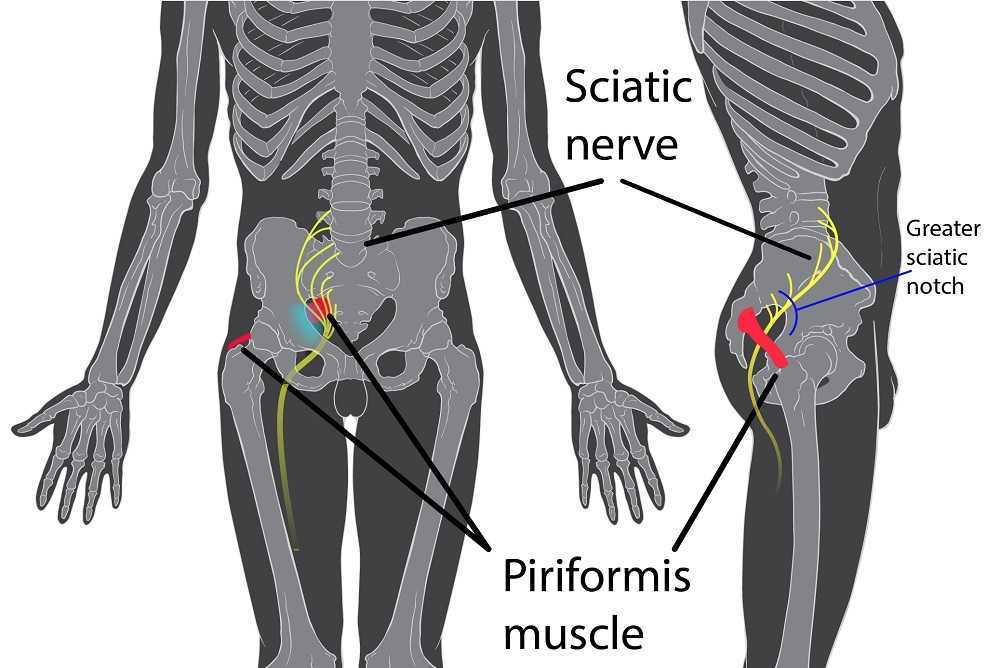
Objective findings revealed normal range of motion in her spine with the exception of limited forward flexion (feeling of back tightness at end range). Hip screening was negative for FABERS, labral screening or capsular pain patterns. General dural tension screening was positive for increased lower extremity and sensation of back tightness with slump c sit. Neural tension test was positive bilaterally for sciatic, R genitofemoral, L Iliohypogastric and Ilioinguinal nerves, and bilateral femoral nerves. Patient had a mild, barely perceptible lumbar scoliosis, and development of bilateral lower extremities and feet was symmetric and normal.
Because of the child’s age, we did not perform internal vaginal exam or treatment. This required treating the nerves that supply the vaginal area. All treatments were done with the patient’s mother present with both consent of the child and the mother.
For treatment, we started with the three inguinal nerves (Ilioinguinal, Iliohypogastric and genitofemoral) because of their relationship with the kidney (symptoms came on after kidney infection) as well as the correlation with the patient’s most limiting symptoms (genital pain). We cleared the fascia along the lumbar nerve roots, the lateral trunk fascia, the psoas, the inguinal region, the entrapments along the kidney and psoas, the inguinal rings and canal, and worked on neural rhythm (these techniques can be learned at the Pelvic Nerve Manual Assessment and Treatment class that I will be teaching later this month).
Over the next weeks, we used similar treatments for the sciatic nerve, femoral nerve, pudendal, and coccygeal nerves. We noted that the patient had an area of restricted tissue along her coccyx that was adhered, and her symptoms had some correlation with tethered cord. We did lots of soft tissue work along the coccyx and working along the coccyx roots, including some internal rectal work. We also did fascial and visceral work in the bladder region, as well as in the lumbar and sacro-coccygeal region.
Peyton’s referring physician and mother were notified of findings and possible tethered cord symptoms (leg weakness and pain, bladder symptoms, delayed nocturnal continence). The patient’s family felt she was getting better and was not interested in any kind of surgical intervention, and her physician also felt that with our progress, he was not interested in exploring that referral, unless the family was interested.
After just 4 treatments Peyton was no longer having any vaginal symptoms and was emptying the bladder normally. After 8 treatments Peyton was reporting no more lumbar pain or lower extremity symptoms, and follow up treatments were reduced to once a month. The patient was given a home program of neural flossing in a small yoga program we recorded on her mother’s phone. We had her mother work on the small area that remained adhered along patient’s tailbone. The area is much smaller, but it reproduces some pelvic pain for the patient, so we are carefully and slowly working along this area because of some of the global neural sx it produces.
The patient’s mother reports she is more active, no longer complaining of leg or vaginal pain. The patient has less generalized anxiety and she is able to void fully. When the pt grows in height, there is a return in some symptoms, likely due to increased neural tension. So, we have the family on standby and when the patient grows, they come back in for 2 visits, which is usually enough to get the patient back to her new baseline.
Today we pick up on Jennafer Vande Vegte's interview with her patient, "Ben", about his experience overcoming chronic pelvic pain syndrome. Ben's quality of life improved so much that he has returned to school in order to become a PTA, with a focus on pelvic rehabilitation!
Describe your physical therapy experience. Talk about your recovery process. Include the physical, mental and emotional components.
 For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
Over the course of many months of PT though we couldn’t pinpoint what started the pain, we knew my nervous system was keeping it going. Sensory signals had somehow been rerouted through pain centers in the delicate and complicated highway interstate of the nervous system. It was as if the Fed Ex truck that was supposed to carry a package from Miami to Denver got rerouted to New York, stuck in traffic in Manhattan, flipped off by cab drivers, beaten up by gang members, contents of the truck shaken up by the driver trying to flee the city, and then finally finding the way out of New York to the true destination of Denver – with damaged goods, and shaking with anxiety. As to who the idiot dispatcher was who re-routed the truck to New York, well, he’s really good at keeping himself secret and innocent-looking. Jerk!
Physical therapy, over time, began to work for me. It released trigger points which are the first step in the long process of recovery. As we know, chronic tension must be addressed in tissues and nerves, and the mind must relearn how to remain in neutral. I found that as I gained periods of relief I could see that there truly was a mind-body connection beyond what I could imagine. My physical therapist and I both knew that nerves are the slowest recovering tissue in the body, and when you combine that with an anxious mind, you have a complicated puzzle to solve. There is definitely a closed circuit that develops with chronic pelvic pain. Pain causes anxiety, anxiety causes pain and circularly they feed one another.
During my physical therapy I joined a male pelvic pain message board online. I began understanding that most men who develop pelvic pain also have experienced traumatic emotional stress. And a large part of chronic pelvic pain is rooted in a mind-body dysfunction. I had to learn how to stop thinking catastrophically, especially during flare ups. I had to trust that my body would heal and think positively. I had to learn how to relax, take care of myself, eat well, stretch and exercise daily.
When I started physical therapy, I hoped to escape the pain. My first 5 month phase of physical therapy helped to loosen the chronically tightened pelvic sphincter muscles. However, I still had allodynia. In my second phase of physical therapy I began experiencing reduction of pain for a longer duration of time. After about a year of therapy, I finally got to a point where I could see there was significant improvement, even though some intermittent pain and anxious symptoms stubbornly persisted. In late spring of 2017, I finally felt like I had conquered the pain by 98%. Occasionally flares would still come, but they were brief and nothing like before physical therapy.
How has your experience with chronic pelvic pain changed you?
CPPS has profoundly changed me. I don’t take the little things for granted or sweat them anymore. I am grateful for not feeling that horrible, hellish sensation any longer. I appreciate having my mind pain and panic free. I speak my mind while respecting my own desires instead of belittling them. I am currently in school to become a Physical Therapy Assistant as through this process I learned that I’m actually much smarter than my middle school guidance counselor thought. I understand the mind is incredibly powerful, and fear rarely has the same power over me.
How do you handle flare ups?
I now handle brief flare ups with deep breaths, meditation, and/or just taking a step back and trying to zero in on what is really bothering me. At least now I can clearly think without debilitating pain and am able to function.
What would you like to say to other people who are struggling with chronic pelvic pain?
Oh, man. For the initial duration, I would say find a safe place where you can feel as comfortable as possible until the pain lessens. When it is bad, you sort of have to give in to it. However, part of this recovery is the physical mechanics of muscle and fascia. Physical Therapy is essential in the process of recovery to release this tension. I would tell them not to give up hope. You will not find many health professionals or websites that will tell you that you can beat this and recover 100%. But I will tell you, you can recover, 100%. You can. But for now, your full-time job is to work on recovery, and that includes lots of self-care, facing possible emotional pain, and physical therapy.
If you would like to learn more about addressing the mind body connection with patients please join us for Holistic Intervention and Meditation: Boundaries, Self-Care and Dialog in January. We will be exploring ways to help our patients heal to their fullest potential as well as keeping ourselves emotionally healthy in the process. Treating patients with persistent pain can be challenging for the best of us. Please come for this three-day course where you will leave feeling refreshed, renewed and reinvigorated to treat even your most complex patient.
Additional resources:
https://www.tamethebeast.org/#home
https://www.youtube.com/watch?v=jIsF8CXouk8
http://www.sciencedirect.com/science/article/pii/S1356689X11000737
http://www.noigroup.com/en/Home
https://bodyinmind.org/who-are-we/
Recently my coworkers and I celebrated a male patient’s recovery from a long and difficult journey with persistent pelvic pain. “Ben’s” case had many elements of what we normally see in our patients: chronic muscle holding, restricted fascia, allodynia, hyperalgesia, castrophizing and kenisiophobia. Ben was also very upfront about how his pain impacted his emotional well-being and vice versa. His healing process taught us a lot about the biopsychosocial aspects of treating persistent pain. Along his journey we dreamed of the day we could write a blog together and help other people learn from the experience. Ben also decided to make a career change entering school to become a PTA so that he could help others in pain. Here is my interview with this brave patient.
 1. Tell us about how your pain started
1. Tell us about how your pain started
My pain started with urethral burning. Tests showed there was no infection. In retrospect, the cause of pain could have been the beginning of tension on pudendal nerve branches from extreme stress and a series of traumatic incidents that happened within weeks of each other. They included a very embarrassing and stressful summer of unemployment, a father who had heart failure and triple bypass in the fall, and a girlfriend who gave me an ultimatum when I was too stressed to get an erection.
2. What medical tests or treatments were done?
When the pain started, I first thought it was a basic urinary tract infection. I went to the med center and was prescribed an antibiotic. After 3 days without change, I went back in and although they still found no sign of infection, they prescribed an additional antibiotic. The urethral pain never stopped and seemed to get worse. Following a series of visits to numerous doctors and urologists, I repeated tests on the prostate fluid, blood tests, and more bacterial tests. No infection. My PCP also made a fairly large overture of testing me repeatedly for HIV. For five months I had a blood test every month, all came back negative. This was damaging to my psyche. For those months I was terrified my life was over. In retrospect, that doctor was out of line, I changed doctors.
3. What were your thoughts when your doctor suggested physical therapy?
When the doctor suggested pelvic floor physical therapy, I was a little skeptical because I was still convinced that something was wrong in a chemical or infectious way (as is typical for most men with pelvic floor dysfunction). However, desperate to take away the constant pain, I followed the advice.
Stay tuned for part two of our conversation with Ben, coming up in our next post on the Pelvic Rehab Report!
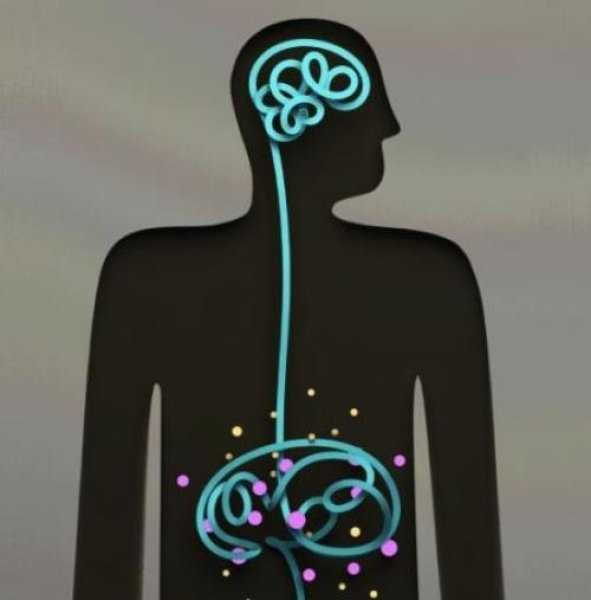
Recently I had a patient referred to me for fecal incontinence. She looked so familiar to me and we realized she had seen me before, years ago, for bladder issues. She was a sweet 60 something single woman who had raised 6 kids on her own after her husband left her. We laughed as she remembered something funny I had said back then. Then we got down to business. In recent years my patient “Inez” had been diagnosed with both diabetes and Crohn’s disease. She was managing the Crohn’s very well but her sugars were much harder for her to get under control. When I asked her about her current complaints and symptoms she reported that most days her bowels were perfect. She reported one or two soft easy to pass stools per day. But when she had to leave the house for a doctor appointment, she would have explosive diarrhea. This didn’t happen if she went to the grocery store or to visit a friend. Upon further questioning she realized she was really anxious about her diabetes and her interactions with her medical provider regarding her diabetes had not been positive. She felt frustrated, scared, and powerless. 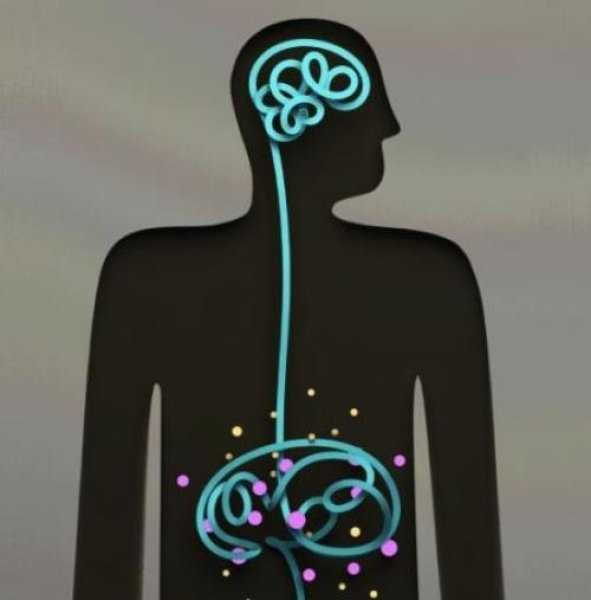
As a pelvic health PT I could have treated Inez in a variety of ways. With my initial exam I did not see any glaring musculoskeletal issues. I suggested to Inez the possibility that her nervous system was sending the wrong kind of signals to her bowels when she got anxious and that we could address this in PT. Inez agreed that she would like to try this approach. We decided that we would reevaluate after four visits to see if we needed to change the plan. Over four visits I used craniosacral therapy protocols to address nervous system upregulation and tension. I taught Inez relaxation techniques and encouraged 10 or 15 minutes of daily relaxation practice. Inez opened up about her relationship with her kids and how they tended to be takers but not givers. She would get frustrated and feel a bit used at times. We had conversations about boundaries and saying “no” and I shared some of my own experiences and struggles as well. Lastly we talked about how what we think can affect how we feel and what we do. Inez’s faith was important to her. She found a few bible verses that were meaningful to her about fear and anxiety and would repeat those during her daily relaxation time. On her fourth visit, Inez was all smiles. She brought me a jar of her homemade salsa as a graduation present. As we sat down to talk she reported to me that she saw her doctor yesterday. She had no bowel issues. And more than that, as her doctor began to talk over her she said to him, “No. Stop. You are always talking and never listening. I need you to listen to me today.” She went on to explain to him how it worried her that she was not able to control her diabetes well and she didn’t think he was doing enough to help her. Her physician did stop and listen and asked Inez, “what would you like me to do for you?” She asked for a referral to a specialist and he obliged. Inez was thrilled that she was able to manage her anxiety in a way that helped her bowels and to find the courage to confront her doctor to get the care she felt she needed.
As we grow in the knowledge of how the human body works it seems like all roads lead back to the nervous system. All of our treatments and interactions with patients affect the nervous system in one way or another. In our fast paced, stressed out world, finding ways to be intentional in addressing the nervous system can be a game changer for patients (as well as for ourselves). If this is an area you would like to grow in, please consider a new course being offered this January in Tampa, Florida. Participants taking Holistic Interventions and Meditation will experience and explore evidence-based information on strategies to address the nervous system. Topics covered include practical meditation, use of essential oils, supplements, yoga, calming and centering manual techniques and instruction in how to best dialogue with patients struggling with pain, anxiety and the effects of trauma. Nari Clemons and I hope to see you there.
Faurot, K. K. R., Gaylord, S., Palsson, O. S., Garland, E. L., Mann, J. D., & Whitehead, W. E. (2014). 715 Mindfulness Meditation Has Long-Term Therapeutic Benefits in Women With Irritable Bowel Syndrome (IBS): Follow-Up Results From a Randomized Controlled Trial. Gastroenterology, 146(5), S-124.
Kearney, D. J. (2012). Mindfulness meditation for women with irritable bowel syndrome–evidence of benefit from a randomised controlled trial. Evidence-based nursing, 15(3), 80-81.
Keefer, L., & Blanchard, E. B. (2001). The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behaviour research and therapy, 39(7), 801-811.
Mindful eating requires slowing down and paying attention to the present moment experience of eating. Rather than mindlessly put food into your mouth and not really taste what you’re eating, you deliberately notice the appearance, smell, texture and taste of the food and pay attention to your thoughts, feelings, and physical sensations. Eating mindfully can interrupt habitual eating behaviors and promote greater self-regulation of food choices.1 Warren and colleagues conclude mindful eating has the potential to help address maladaptive eating behaviors and the difficulties many face with controlling food intake.2
 Although mindful breathing, body scan and movement are the core skills I teach patients with persistent pain, I introduce mindful eating as another strategy to cultivate present moment awareness. Patients can have surprising shifts in their relationship to food and frequently comment, “If I ate more mindfully, I would enjoy my food more and eat less!”
Although mindful breathing, body scan and movement are the core skills I teach patients with persistent pain, I introduce mindful eating as another strategy to cultivate present moment awareness. Patients can have surprising shifts in their relationship to food and frequently comment, “If I ate more mindfully, I would enjoy my food more and eat less!”
Lucie Khadduri, PT, DPT, PRPC clinician and Adjunct Professor at the University of Puget Sound School of Physical Therapy, took my course last spring and describes her patient’s experience with mindful eating:
I have been meaning to email for some time to thank you for the April 2017 course on Mindfulness for Rehab Professionals. Your class really impacted my daily PT practice in a positive way. I wanted to share with you one story in particular to illustrate the power that these new tools you have given me have helped others.
I have this male patient who is about 35 years old who struggled with chronic constipation, bloating and anxiety related to his intense fecal urges that were then followed by an inability to defecate. When he started PT, he had just left his job and took a job working from home just so that he could have consistent, stress free bathroom access.
I spoke to him about diaphragmatic breathing and mindfulness and its impact on the autonomic nervous system. What helped him the most, though, was the mindful eating exercise. He has since started applying these concepts to when he eats. He told me on his discharge visit that in the past, he would eat 4 slices of pizza very quickly, without thinking about it and then have horrible pain afterward. Now, he says it is easy to eat 1 slice and have a salad not because he knows salad is better for him, but because his mouth and mind crave different textures and colors in his food. Mindful eating gave him the ability to slow down, focus on the physical sensations of eating and he found that this has changed his relationship with food. As a result, his constipation is much better managed and his anxiety and stress are much better.
Thanks again for an excellent class. I often encourage patients to go to your website for your free 10 minute meditations.
Thank you, Lucie, for sharing this story. It reflects one of the many ways patients benefit from training in mindful awareness. I look forward to introducing colleagues to mindful eating and additional experiential mindful exercises and current research in my upcoming class, Mindfulness-Based Pain Treatment, at Loyola University Stritch School of Medicine, Maywood, Il, September 30 and October 1.
1. Miller CK. Mindful eating with diabetes. Diabetes Spectr. 2017 May;30(2):89-94.
2. Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviors: effectiveness and associated potential mechanisms. Nutr Res Rev. 2017 Jul 18:1 – 12.
Image courtesy of California Institute of Technology