Mora Pluchino, PT, DPT, PRPC sat down this week with Holly Tanner in an interview to discuss her new courses, Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens. She is a pelvic therapist who works in an outpatient clinic, has her own side company (Practically Perfect PT), has written 2 books available on Amazon, and is a senior TA and faculty member with Herman & Wallace. Mora joins the Herman & Wallace faculty with her new course series in ethics: Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens.
What are your core values as a pelvic health practitioner? Depending on your practitioner license these may include (1):
- Accountability - Active acceptance of the responsibility for the diverse roles, obligations, and actions of the physical therapist and physical therapist assistant including self‐regulation and other behaviors that positively influence patient and client outcomes, the profession, and the health needs of society.
- Altruism - The primary regard for or devotion to the interest of patients and clients, thus assuming the responsibility of placing the needs of patients and clients ahead of the physical therapist’s or physical therapist assistant’s self‐interest.
- Collaboration - Working together with patients and clients, families, communities, and professionals in health and other fields to achieve shared goals. Collaboration within the physical therapist‐physical therapist assistant team is working together, within each partner’s respective role, to achieve optimal physical therapist services and outcomes for patients and clients.
- Compassion and Caring - Compassion is the desire to identify with or sense something of another’s experience; a precursor of caring. Caring is the concern, empathy, and consideration for the needs and values of others.
- Duty - The commitment to meeting one’s obligations to provide effective physical therapy services to patients and clients, to serve the profession, and to positively influence the health of society.
- Excellence - The provision of physical therapist services occurs when the physical therapist and physical therapist assistant consistently use current knowledge and skills while understanding personal limits, integrating the patient or client's perspective, embracing advancement, and challenging mediocrity.
- Integrity - Steadfast adherence to high ethical principles or standards, being truthful, ensuring fairness, following through on commitments, and verbalizing to others the rationale for actions.
- Social Responsibility - The promotion of mutual trust between the profession and the larger public that necessitates responding to societal needs for health and wellness.
Annual CEU requirements for license renewals don’t just look at hands-on skills. Many states also require a number of ethics credits including California, Georgia, Illinois, New Jersey, and Utah (2). In her interview, Mora Pluchino explains that one day she and her colleague were at lunch talking about course options for their ethics CEU requirement. They had taken the same course over and over at Stockton University and wanted to do something different this time. This led to Mora reaching out to Herman & Wallace and Holly Tanner who helped her start writing the course. Mora’s new courses focus on this ethics requirement, provide 6 contact hours, and registration is $175.00 for each:
- Ethical Concerns for Pelvic Health Professionals – June 18th
- Ethical Considerations from a Legal Lens – December 10th
What should you expect from an ethics course? Mora breaks down the Ethical Concerns for Pelvic Health Professionals course and shares that there is about an hour of pre-course video lectures to watch, then the live course involves “a little bit of lecture in relation to pelvic health and ethics, and then there will be some case studies and group work. After this, an ethical expert will come in and do live question/answers with us.”
These courses are to really make practitioners comfortable with these ethical and moral issues. Mora explains, “I really want practitioners who take this course to understand and know where to find information about those issues that come up with their boss, their organization, their patients, or themselves. A lot of times, ethical situations just make us just know instinctively that something doesn’t feel right.” Holly follows up with “Sometimes these situations can make us feel embarrassed, and maybe we contributed or didn’t contribute in the right way to a scenario. We don’t always bring them up to other people out of this embarrassment, or we just don’t know which pathway to take.”
A lot of common questions have an ethical component such as “How do I bill for this,” “How do I tell my boss I can’t do this,” or even “Can I reuse a biofeedback sensor?” Mora shares, “Sometimes, as a practitioner you can feel pressured to do (or not do) something, and you don’t know how to say no. With these courses, you will be able to give clear reasons such as it’s in my guidelines, in my practice act, and core values as being a PT or OT.” She further expands on this, “We have all of these people working for us in the APTA and AOTA that are creating all of these ethical guidelines and all of this information to give us the support.”
The ethics topics are broken down into two courses, with the first course Ethical Concerns for Pelvic Health Professionals focused specifically on people who treat pelvises scheduled for June 18, 2022. The second course, Ethical Considerations from a Legal Lens, is scheduled for December 10, 2022, and deals with the legalities and rights of health care providers. Some questions that are touched on during lectures include abandonment of care and discrimination. Mora also shares that a lot of the ethics courses she has taken are “from the perspective of therapists that are abusing their patients, but when you work in pelvic health world you realize it can go the other way too, or it can be a back and forth kind of thing.”
To learn more, and fulfill that ethics CEU requirement, join H&W and Mora Pluchino this summer in Ethical Concerns for Pelvic Health Professionals on June 18th or this winter in Ethical Considerations from a Legal Lens scheduled for December 10th.
Resources:
- APTA. Core Values for the Physical Therapist and Physical Therapist. HOD P06‐19‐48‐55. 9/20/2019. https://www.apta.org/siteassets/pdfs/policies/core-values-endorsement.pdf. Accessed 5/30/2022.
- Fraticelli, T. PT Progress. Physical Therapy Continuing Education: PT CEU Requirements by State. October 8, 2018. https://www.ptprogress.com/physical-therapy-continuing-education-requirements-by-state/. Accessed 5/30/2022.
Additional Resources:
o Counselors / Psychologists: https://www.apa.org/about/apa-jobs/values
Sarah Clampett, PT, DPT, is Head of Clinical Operations at Origin, a leading provider of pelvic floor and whole-body physical therapy with a special focus on pregnancy and postpartum. After studying Kinesiology and Psychology at the University of California, Sarah stayed on to earn her Doctorate of Physical Therapy. As a clinical leader at Origin, she’s as passionate about helping PTs love the work they do as she is helping patients feel good in their bodies.

Shortly after I started physical therapy school, I realized that being a physical therapist is a fantastic conversation starter. People’s eyes tend to light up when they hear I’m a PT because almost everyone has had an experience with physical therapy — and even if they haven’t, they’ve had an injury. They want to tell me about the physical therapy they did in high school for their scoliosis or that time they tore their ACL skiing. They even seek advice for that pesky low back pain that hasn’t fully resolved since throwing their back out six months ago.
I love to hear people’s stories and genuinely enjoy engaging in casual conversations about injuries. When I’m done explaining that core strength is important when dealing with back pain, I go on to say that while I started my career in ortho, I’m now a pelvic floor PT. That’s when one of two things happens: 1) They stare at me blankly, then quickly change the subject, or 2) Their eyes light up even brighter and they start asking questions. That’s when the conversation gets really fun. “What exactly do you do?” “What do you treat?” and “How did you get into that?”
Where My Passion for Ortho Started
I decided to go to PT school for a couple of reasons. I’ve always loved sports and consider sports a large part of my upbringing. (Fun fact: I only listened to AM sports radio until I was about 13). And, like many PTs, I discovered physical therapy as a patient. In my case, it was after injuring myself in high school playing volleyball.
I loved going to PT, not only because I was getting better — I loved seeing all the other patients getting better around me. It was a very sports-oriented PT clinic and my first and only experience with PT, so when I declared Kinesiology as my major and started my pre-PT coursework in college, I had my heart set on being a sports/ortho PT. It felt like the perfect fit at the time. I was a student athletic trainer for 2.5 years in college to learn as much as I could about the sports rehab world before heading into PT school.
Fast forward to my final semester and clinical rotation at PT school: I was at an ortho clinic with a large population of athletes. I loved it. After I graduated, I was hired as a PT at that same clinic and started my career as a working PT. I began working a few days a week to build my caseload with the plan to transition to full-time as my schedule filled. That clinic happened to also own a women’s health clinic that treated primarily prenatal and postpartum patients. A few weeks after starting, I was asked if I wanted to work additional days by filling in at the women’s health clinic. As a new grad who needed to pay rent, I said yes because more days meant more money. It was supposed to be temporary.
My Journey to Becoming a Pelvic Floor PT
As soon as I walked into the women’s health clinic, something clicked. I fell in love with the patient population and helping them feel better. I remember early on, a patient with such severe pelvic pain that they could barely walk to the bathroom. At their next visit, they said they could walk without pain again. The ability to help people going through pregnancy and postpartum felt especially meaningful. I spent a year and a half working in both clinics and then transitioned to treating women’s health full time.
After working in women’s health for a couple of years, I eventually got tired of referring my patients with pelvic floor conditions to colleagues who treated pelvic floor and decided it was time to start treating it myself. To be honest, I was hesitant at first and definitely nervous about taking my first course. But as soon as I started treating the pelvic floor, something clicked again.
Even more so than in the past, I connected deeply with my patients and their goals. Giving someone the confidence to leave the house without wearing a maxi-pad or carrying extra underwear because they’re no longer worried about leaking was amazing. So many people suffer in silence from pelvic floor disorders and are resolved to just live with them. I’m lucky enough to provide a safe space to talk about it and assure them that it can get better. How cool is that?
Advice for an Ortho PT Curious About Pelvic floor
Take a course! Just because you take the course does not mean you are committing to a career change. Even if you decide it’s not the right time to switch or you didn’t enjoy it as much as you thought you would, you’ll still learn valuable information that you can immediately incorporate into your practice. That overworked, stressed patient with lingering hip pain might need pelvic floor lengthening to get that last bit of pain to resolve.
Most ortho PTs who make the shift are nervous they won’t be able to use their ortho skills when treating the pelvic floor, and that simply isn’t true. My time in ortho has definitely shaped the pelvic floor PT I am today.
In ortho, you treat the whole body. If your foot hurts, you look at the knee, the hip, the low back, and how everything works together to figure out what’s causing the foot pain. Pelvic floor PT is no different. You must look at the whole body and figure out how all the parts are working together to get the results you need. I continue to use many of the same exercises now that I used back when I was working as an ortho PT.
Lastly, the pelvic floor is a group of muscles. If it’s weak, it needs to strengthen. If it’s overactive, it needs to lengthen. If it’s uncoordinated, it needs to be retrained. Yes, treating pelvic floor dysfunction requires special training, but at the end of the day, muscles are muscles.

I have always enjoyed working with the peripartum population. However, the longer I worked in pelvic rehabilitation the more I heard the same story over and over when interviewing patients. For example, when working with a patient with urinary incontinence or prolapse, I would say: “when did this start” and some of my elderly patients would laugh and say “when Johnny was born” and I would say “how old is Johnny” they would reply “40!” Many of the pelvic patients I was treating had symptoms originating around the time of childbirth and they had been suffering for decades. So, I figured, let’s get to the root of the problem and focus on earlier intervention.

What is the root of the problem? In my opinion, it is the lack of postpartum care. Pregnant patients are often inundated with birth education programs and information about pregnancy and childbirth. Additionally, there is a battery of prenatal visits, prenatal testing, and preparations for birth. All of which are wonderful to help prepare for birth. Conversely, the resources and guidance to help with physiological and musculoskeletal healing postpartum are lacking. Patients are counseled about serious signs and symptoms, but clear guidance to help to return to daily functional activities including recreation and exercise is often not provided. As musculoskeletal and exercises experts we are in a wonderful position to help patients reduce pain and improve function following the birth of a child.
Prior to 2018, the first post-partum checkup was six weeks following birth. Barring any severe problems, this was often the last contact with a medical provider for the parent. Patients were not provided specific guidance on how to return to daily activities, let alone higher-level activities such as running, exercising, and/or lifting weights.
In 2018, the American College of Obstetrics and Gynecology (ACOG) revised its guidelines, which now support earlier and more frequent postpartum visits. It is recommended that the first contact between patient and obstetric care provider occur in the first three weeks following birth and that subsequent visits are scheduled as needed in an ongoing fashion1. This is important, as many consider the patient is still healing from birth up to 12 weeks (definitions vary). Depending on their knowledge and experience, a patient may not immediately realize they have a musculoskeletal problem. A new parent is busy adapting to their role as a care provider and may not be thinking about themselves. Additionally, they may not know what “normal” is for their body postpartum, including vaginal, abdominals, and/or bowel, and bladder functions. For example, the patient may be experiencing urinary incontinence (UI) which they “think” is normal postpartum, therefore, they may not bring it up to their provider. Patients often seek advice from family and friends who may even joke about peeing their pants when they sneeze or laugh or play with their children. Urinary incontinence is not ever “normal”, however, is it common in the postpartum period. Availability of vetted resources and a relationship with a healthcare provider are essential to cure these misconceptions.
According to a systematic review, the prevalence of urinary incontinence is 33% at three months postpartum2 and remains at 29% four years postpartum3. This means about one-third of women have urinary incontinence postpartum and remain that way without intervention. We also know the prevalence of urinary incontinence is strongly related to increasing age and underreported. This example highlights a common misconception: pelvic dysfunction is a normal part of the after-birth stage. However, with intervention, these problems can be alleviated, and we can improve the quality of life for these patients.
According to the American College of Physicians (ACP) clinical practice guidelines for non-surgical management of UI there is high-quality evidence that strongly recommends pelvic floor muscle training as the first-line treatment for stress incontinence.4
So why isn’t pelvic assessment and rehabilitation recommended for all people who birth in our country? In several European countries, pelvic rehab is standard postpartum care for anyone who births. Over the last two decades, I do see more postpartum patients referred for rehabilitation for their musculoskeletal impairments. However, I still think we need more skilled providers assisting these patients and spreading the word about the interventions rehabilitation professionals provide. These can range from common orthopedic complaints (e.g neck or back pain from repetitive baby care) to specific bladder and/or bowel dysfunction, such as leakage and/or constipation, abdominal separation (Diastasis Rectus Abdominus-DRA), prolapse, pelvic pain, perineal tearing, and/or pain with intercourse.
When developing this four-course postpartum series, I wanted rehabilitation providers to have more advanced skills to provide examination and treatment to this special population. This includes techniques to assess and treat the abdominals and pelvis, as these areas are physiologically impacted by pregnancy and birth over a relatively short amount of time. To effectively treat this population, one needs to be familiar with physiological changes from pregnancy, and stages of labor and birth to understand the journey of your patient. There is so much we can do to help these patients over a range of complaints, from acute breast and perineal care to DRA and pelvic dysfunctions. As with any special population, postpartum patients have unique red flags and concerns to monitor, and due to our more frequent patient contact, it is imperative to be proficient in screening for these conditions. These topics and more are included in the course series.
I am grateful and appreciative of this collaboration between Herman & Wallace and Medbridge to provide a platform for clinicians to progress their knowledge. Hopefully, this improves access to postpartum care and increases referrals for rehabilitation services to improve the function and quality of life for parents. Together we can reduce chronic impairments stemming from the childbirth period.
Resources:
- Accessed on 5/9/2022: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/05/optimizing-postpartum-care
- Thom, D. H., & Rortveit, G. (2010). Prevalence of postpartum urinary incontinence: a systematic review. Acta obstetricia et gynecologica Scandinavica, 89(12), 1511-1522.
- Gartland, D., MacArthur, C., Woolhouse, H., McDonald, E., & Brown, S. J. (2016). Frequency, severity and risk factors for urinary and faecal incontinence at 4 years postpartum: a prospective cohort. BJOG: An International Journal of Obstetrics & Gynaecology, 123(7), 1203-1211.
- Qaseem, A., Dallas, P., Forciea, M. A., Starkey, M., Denberg, T. D., Shekelle, P., & Clinical Guidelines Committee of the American College of Physicians*. (2014). Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians. Annals of internal medicine, 161(6), 429-440.
|
Postpartum Patient: General Examination Instructor: Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES
Postpartum Patient: General Treatment Instructor: Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES |
Abdominals in the Postpartum Patient: Evaluation and Treatment Instructor: Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES
Pelvic Floor in the Postpartum Patient: Evaluation and Treatment Instructor: Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES |
The popularity of yoga continues to rise with over 36 million yogis living in the United States of America and over 300 million practitioners worldwide. Yoga has several therapeutic effects that make it a beneficial addition to home exercise programs for practitioners and personal practice.
Dustienne Miller discussed some of the benefits of yoga in her March blog (March 8, 2022 - A yoga practice can change your neuroanatomy!). These benefits extend beyond the musculoskeletal system and include improved mood and depression, changes in pain perception, improved mindfulness and associated improved pain tolerance, and the ability to observe situations with emotional detachment.
The physical benefits are well documented in several research studies and include improved flexibility, strength, and stability as well as enhanced respiratory and cardiovascular function. Supporting documentation also shows that yoga can help alleviate the symptoms of chronic pain. Dustienne Miller shared that in a study by Villemure et al, they determined “that the insula-related interoceptive awareness strategies of the yoga practitioners being used during the experiment correlated with the greater intra-insular connectivity...concluding that the insular cortex can act as a pain mediator for yoga practitioners.”
Restorative yoga shares the many benefits seen in other styles of yoga and can also be a great addition to home programs for pelvic rehab practitioners. Kate Bailey shared in her interview with The Pelvic Rehab Report (August 31, 2021 – Faculty Interview: Kate Bailey) that restorative yoga “focuses on the lesser-known aspects of the yoga platform: breath, restorative practice, and a bit of meditation. I have clients all the time who struggle with meditation because their nervous systems aren’t ready for it. So we look at breathing and restorative yoga both as independent alternatives, but also as a way to get closer to meditation.. giving the clinicians another skill for their own rest practice can be useful when feeling tired, overwhelmed, or burned out. “
But what does this mean? Let’s look at some of these aspects a bit closer:
Improving mood and sleep: This includes depression, anxiety, and even stress or other mood disorders. Consistent yoga practice can lead to significant increases in serotonin levels coupled with decreases in the levels of monoamine oxidase, an enzyme that breaks down neurotransmitters and cortisol(1). Yoga can inhibit the areas in the brain responsible for fear, aggressiveness, and rage (posterior or sympathetic area of the hypothalamus) – while simultaneously stimulating the rewarding pleasure centers in the median forebrain and other areas leading to a state of bliss and pleasure. This inhibition results in lower anxiety, heart rate, respiratory rate, blood pressure, and cardiac output (2).
Think about it. Deep breathing calms the nervous system. This promotes relaxation. The more relaxed you are then the better the chance of having a good night’s sleep. Consistent yoga practice can also assist sleep quality by increasing melatonin and reducing hyperarousal (3). Pratyahara, or a turning inward of the senses, allows downtime for the nervous system and can be encouraged by yoga poses such as savasana (corpse pose) and pranayama (breathing exercises/control.
Reduced Chronic Pain: Asana and meditation have been shown to reduce chronic pain including reduced pain from arthritis, back pain, and other chronic conditions while also improving balance and increasing proprioception(1). Yoga sessions can take our joints through a full range of motion. This squeezes and soaks areas of cartilage not often used and provides fresh nutrients, oxygen, and blook to the joints. Otherwise neglected areas of cartilage in the joints would wear out, exposing bone, which can lead to arthritis and chronic pain. At the same time, yoga is gentle on the body and consistent practice can strengthen the connective tissues that surround the bones and joints.
Effects on Cancer Patients: Yoga cannot cure cancer, but it can reduce stress and improve physical, emotional, and spiritual wellness. There is supporting research that the growth of cancerous tumors can be exacerbated by stress(4). This same study found that consistent yoga practice could decrease post-chemotherapy-induced frequency and intensity of nausea and the intensity of anticipatory nausea and vomiting. In 2018 Lin et al provided new research showing that restorative yoga can decrease depression in cancer survivors; improve symptoms of anxiety, depression, and pain symptoms in cancer patients; and help patients manage the toxicity of cancer treatments (5). In addition, yoga has a fundamental emphasis placed on mindfulness and acceptance of your body and its limitations.
Kate Bailey likes to joke about lying on the floor, but really, it is not a joke at all. Lying on the floor for 15 minutes is savasana. She shares that “Savasana is a wakeful resting and a practice of relaxation response. It seems easy: you always have access to a floor. You don’t need anything fancy. Aside from the neuroregulatory benefits of rest, savasana also gives the postural muscles a break. It allows the hip flexors to re-lengthen and the cervicothoracic junction to realign.”
Let’s take a moment to close with a savasana (did you know that a 5-minute savasana is recommended for every 30 minutes of yoga?). This pose can calm the central nervous system, aid the digestive and immune systems, reduce headaches, fatigue, and anxiety while lowering blood pressure and calming the mind, and reducing stress.
Take a moment and lay on the floor with your arms and legs open wide and relaxed (starfish style), supported by a bolster, or you may want to place your hands gently over your chest or your stomach. Now gently still your body. Release your breath and be present. Be completely aware of the moment. Let your mind and body go for a few moments.
Namaste.
References:
- McCall T. New York: Bantam Dell a division of Random House Inc; 2007. Yoga as Medicine.
- Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. International journal of yoga, 4(2), 49–54. 2011. doi: 10.4103/0973-6131.85485
- Wang W-L, Chen K-H, Pan Y-C, Yang S-N, Chan Y-Y. The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):195. doi:10.1186/s12888-020-02566-4
- Carson, J. W., Carson, K. M., Porter, L. S., Keefe, F. J., Shaw, H., & Miller, J. M. (2007). Yoga for women with metastatic breast cancer: results from a pilot study. Journal of pain and symptom management, 33(3), 331–341.
- Lin P-J, Peppone LJ, Janelsins MC, et al. Yoga for the management of cancer treatment-related toxicities. Curr Oncol Rep. 2018;20:5. doi:10.1007/s11912-018-0657-2
 Restorative Yoga for Physical Therapists with instructor Kate Bailey
Restorative Yoga for Physical Therapists with instructor Kate Bailey
This course will provide the basis for experiencing and integrating restorative yoga into physical therapy practice. Restorative yoga is an accessible practice that can teach patients (and practitioners) how to rest systematically, for short periods of time, on a regular basis to encourage the parasympathetic nervous system to balance with the sympathetic nervous system for improved neuroregulation. Topics include the difference between meditation and restorative yoga, and how they can support each other in order to support the ability to drop into relaxation. Restorative postures, each taking 20-30 minutes are offered prior to the live meeting so that participants can experience what a patient might experience when restorative yoga is a component of their home program. Then in the live course participant experiences, questions, and strategies on how to reduce barriers to relaxation so that patients can integrate this practice into their lifestyle will be discussed. There will also be live labs for breathing techniques and specific meditations that may be helpful to patients working with an unregulated nervous system.
 Yoga for Pelvic Pain with instructor Dustienne Miller
Yoga for Pelvic Pain with instructor Dustienne Miller
This course offers an evidence-based perspective on the value of yoga for patients with chronic pelvic pain by focusing on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) - and how they can be applied for patients who have hip, back and pelvic pain. A variety of pelvic conditions will be discussed including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Lecture topics include the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.

This article was originally posted on the Medbridge Blog site: https://www.medbridgeeducation.com/blog/2021/11/six-actionable-ways-to-be-a-better-lgbtq-ally/.
Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians. Brianna owns and operates Empower Physiotherapy, a private practice in Seattle. As a competitive powerlifter, Brianna enjoys working with strength athletes who experience pelvic floor dysfunction, especially stress incontinence. She is passionate about providing care to individuals in the LGBTQ+ community, including those undergoing hormonal/surgical transition. Brianna's additional clinical interests include prenatal/postpartum care for trans and gender-nonconforming folx and pelvic floor care for patients that are intersex. Brianna curated and teaches LGBTQ+ cultural competency for practitioners in her course - Inclusive Care for Gender and Sexual Minorities.
LGBTQIA2S+. Does it seem like that acronym is ever-growing? That’s because it is!
As our society evolves, more people are feeling safe and comfortable to live as their authentic selves, and every day there is more evidence to support that.
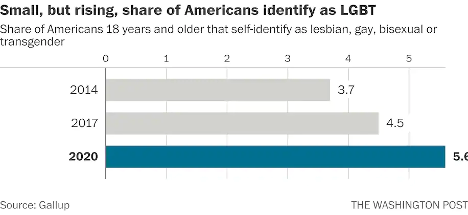
According to Gallup polls, the percentage of people in the U.S. that identify as lesbian, gay, bisexual, or transgender has increased to 5.6 percent.3 That is three times the entire population of Colorado! These numbers are even higher amongst younger generations—up to 20 percent in Gen Z and millennials by some estimates. In 2019, nearly 80 percent of surveyed Americans state that they personally know someone who identifies as LGBTQIA2S+ or queer.2 And while the word “queer” has a nasty history as a derogatory slur, it is increasingly used by folks in the LGBTQIA2S+ community to describe those who do not identify as cisgender or heterosexual.
What Is the Importance of Sexual Orientation or Gender Identity in Healthcare?
Recent years have provided a groundswell of awareness building around this community—from representation in entertainment, discussion about participation in athletics, and changes occurring at the legislative level. However, one area of society in which awareness is still lacking is in modern-day medicine, so let’s explore the significance of sexual orientation and gender identity (SOGI) as it pertains to healthcare.
As a medical professional, you may wonder “Can’t I simply treat all people the same?” While this idea may be filled with good intentions, the unfortunate reality is that we do not yet have access to this utopian future. There are real, measurable differences in the health of all marginalized communities, including gender and sexual minorities (GSM).
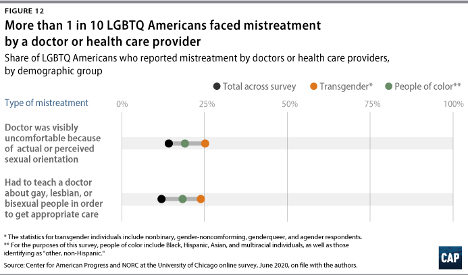
In 2020, 1 in 10 LGBTQIA2S+ Americans faced some form of mistreatment from a healthcare professional.1 These negative experiences strongly correlate with postponing or altogether avoiding medical care in the future, further contributing to the collective LGBTQIA2S+ fear of discrimination. The statistics are even worse when specifically looking at queer and trans people of color.
What Can You Do as a Healthcare Provider?
While the system and the education that trains our clinicians could benefit from a renovation, here are six actionable steps you can take now to facilitate a safer space for your LGBTQIA2S+ patients:
1. Recognize your own potential to cause harm.
As healthcare professionals, we have some degree of inherent privilege. With this privilege comes the capacity to inflict harm, intentional or not. While intentions matter, they do not supersede the impact your words or actions have on another. Assumptions matter, too. While assumption making is common and normal—an evolutionarily advantageous adaptation of the brain—they are not facts, and they are not harmless. Erroneous assumptions about a person’s gender or sexual identity by a medical professional can lead to behaviors that cause discomfort in and discrimination towards LGBTQIA2S+ patients and clients, even if inadvertently.
By recognizing the power differential that exists in the patient/provider relationship and the implications that come with it, we are likely to be more aware of our words and actions when they come up, and more willing to address them when they do. And by taking a position of genuine care and curiosity rather than assumption, we can affirm the relationship between the person whom we are helping and their body.
2. Update your language.
Always use the correct pronouns and name of the person with whom you are working. One easy way to do this is simply by mirroring the language they use when describing themself. However, if you are meeting someone for the first time, you may unintentionally use language that is not in line with your patient or client’s identity. For example, you may use someone’s dead name (the name assigned to them at birth) which may still be listed on their legal and medical documentation.
You can preempt this kind of unintentional harm by including areas for clarification on intake paperwork. This will allow you the opportunity to affirm the pronouns of the person in your care upon your first interaction. While pronoun affirmation may seem like a small action, it has shown to be effective in reducing suicidal ideation and depression.4 Another way to update your language for greater inclusivity is by using the term “spouse” or “partner” when inquiring if a patient has someone at home that can help with their activities of daily living or rehabilitation. Additionally, when referring to pregnancy, birthing, and postpartum care, practice saying “pregnant person” or “birthing parent” rather than “pregnant woman” or “mother.”
3. Speak up….even if the LGBTQIA2S+ person or target of the harm isn’t present.
Shaming someone’s behavior is unlikely to result in positive change or self-reflection. Instead, we can follow the steps of stopping, educating, and being proactive to foster learning in our colleagues. This kind of dialogue offers the opportunity for the individual to participate in the discussion by learning about their behavior, rather than feeling pushed out of the conversation which could limit their chance to grow.
- First, STOP the discussion or action taking place by intervening with “Those words can be hurtful.”
- Next, EDUCATE in lieu of asserting judgment. Proceed from a lens of curiosity. Asking the person “Do you know what those words mean?” or genuinely inquiring about their intention and understanding. Doing this will facilitate conversation and enhance one’s knowledge of their damaging actions, reducing the chance that they will repeat the harmful behavior.
- Finally, BE PROACTIVE by following up with resources for further learning such as GLMA, WPATH, or The Fenway Institute.
It is important to note the significance of taking this action even if the LGBTQIA2S+ person was not present for the encounter. This breaks the notion that harmful language is acceptable so long as the subject of the harm is not privy to it. If the LGBTQIA2S+ person is present for the encounter, it is best to first pull them aside to check in with them, make sure they are alright, and ask if they want your help. Some folks prefer to avoid drawing attention to themselves. It is also a skill of allyship to know when not to talk.
4. Be receptive to feedback.
When an LGBTQIA2S+ person, or a person from any marginalized group for that matter, corrects your language or behavior, practice saying “thank you” rather than “sorry” and avoid explaining yourself. It is a privilege to learn about oppression rather than to experience it for yourself. When someone corrects you, not only are they bravely honoring their authentic identities, but they are doing emotional labor on your behalf, and in the age of freely available information, it is never the responsibility of marginalized folks to educate others for free. These interactions are opportunities for personal growth—don’t let them pass you by!
5. Suggest practical changes to make the workplace more inclusive.
Does your workplace have gender-neutral bathrooms? Many LGBTQIA2S+, queer, and trans people avoid using public restrooms to avoid harassment and violence. Such aggressions can have very tangible consequences to their physical health, such as pelvic floor dysfunction. If there aren’t any inclusive restrooms in your workplace, make a suggestion to change that.
How inclusive are the brochures in your waiting room? Do the patient education materials that you provide to a patient after evaluation use language and imagery that include the LGBTQIA2S+ community? These are areas that can be improved upon with the suggested language updates we discussed above in action step two.
Are there symbols or graphics that will welcome GSM, such as safe space signs, flags depicting an upside-down rainbow triangle, or “all-gender” verbiage in lieu of gender-specific? Both would make easy additions that signal to patients they are in an inclusive space. However, it is important to distinguish the difference between saying a space is safe, and actually making a space safe. A space can only be safe if the entire team of providers and office staff are on board. Labeling a space as safe when it is not has the propensity to cause further harm. Be sure before these indicators are put up in your practice, everyone is ready to support such efforts.
6. Be prepared to mess up—but don’t let that deter you from trying.
Any etymologist will tell you that languages are living things that are constantly evolving. Developments such as these can make it challenging to stay current on which terminology is most beneficial to our growing society. Sometimes just the fear of making a mistake can be intimidating enough to discourage people from trying. What is most important is not how well you use updated language but that you are trying. Your effort matters, and it is what will move the needle in the right direction. Cultural responsiveness is not knowing every nuanced detail of every demographic group. Cultural responsiveness is being willing to reflect and modify your viewpoints when presented with information that differs from what you previously held to be true. Try to accept that just with learning any new skill, mistakes are bound to happen. When they do be prepared to learn, and then move forward with that new knowledge in mind.
References:
- Cusick Director, J., Seeberger Director, C., Woodcome, T., Oduyeru Manager, L., Gordon Director, P., Shepherd, M., Parshall, J., Santos, T., Medina, C., Gruberg, S., Mahowald, L., Bleiweis, R., Graves-Fitzsimmons, G., & Zhavoronkova, M. (2021, November 7). The State of the LGBTQ Community in 2020. Center for American Progress. Retrieved November 23, 2021, from https://www.americanprogress.org/article/state-lgbtq-community-2020/.
- Ellis, S. K. (2019). GLAAD Accelerating Acceptance 2019 Executive Summary. GLAAD.
- Jones, J. M. (2021, November 20). LGBT identification rises to 5.6% in latest U.S. estimate. Gallup.com. Retrieved November 23, 2021, from https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx.
- Russell, S. T., Pollitt, A. M., Li, G., & Grossman, A. H. (2018). Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. Journal of Adolescent Health, 63(4), 503–505. https://doi.org/10.1016/j.jadohealth.2018.02.003
Additional resources:
- Schmidt, S. (2021, February 26). 1 in 6 Gen Z adults are LGBT. and this number could continue to grow. The Washington Post. Retrieved November 23, 2021, from https://www.washingtonpost.com/dc-md-va/2021/02/24/gen-z-lgbt/.
- Who Are We? Consortium. (n.d.). Retrieved November 23, 2021, from https://www.consortium.lgbt/intersex-inclusive-flag/.
Inclusive Care for Gender and Sexual Minorities
with instructor Brianna Durand, PT, DPT
When it feels overwhelming and nuanced, it can be tempting to avoid uncomfortable topics altogether. However, attendees for this course can expect to be gently guided into the sometimes confusing realm of gender and sexual orientation, and identity. This course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice. Although this course will cover pelvic floor physical therapy specifically, it is appropriate and useful for any medical professional as we all have patients in the LGBTQ+ community.
This week The Pelvic Rehab Report sat down with new faculty member, Emily McElrath PT, DPT, MTC, CIDN, to discuss her pelvic rehab journey and her new course, Pregnancy and Postpartum Considerations for High-Intensity Athletics. Emily is a native of New Orleans, is highly trained in Sports and Orthopedics, and has a passion for helping women achieve optimal sports performance. Emily is also certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and Crossfitter and has personal experience modifying these activities during pregnancy and postpartum.

Hi Emily! Can you tell us a little bit about yourself and your clinical practice?
My name is Emily McElrath, and I am an orthopedic and pelvic floor PT. I spent the early years of my career in sports medicine and primarily worked with high school and collegiate athletes, as well as weekend warriors. I myself am a distance runner and Crossfitter and have always had a love for sports. After the birth of my second child, I had a hard time returning to Crossfit due to significant pelvic floor dysfunction and pain. At that time, I became a pelvic floor patient and quickly realized how valuable this specialty was. This began my journey to becoming a pelvic PT.
Since that time almost 4 years ago, I have been blending my orthopedic and pelvic health knowledge and skillset to help women return to the sports they love without pain and pelvic floor dysfunction. My main goal as a clinician is to educate and empower my patients to feel in control of their own bodies, and to feel confident in daily and recreational activities.
What has your educational journey as a pelvic rehab therapist looked like and how did you get involved in the pelvic rehabilitation field?
It was really a matter of personal experience leading me to the field of pelvic health. I knew the specialty of pelvic health existed, but until I was a patient I did not truly appreciate how valuable it was. Seeing firsthand how significantly pelvic floor physical therapy could improve the quality of a patient’s life gave me a desire to become a pelvic PT. Once I got into my course work with Herman & Wallace, I realized that my background as an orthopedic PT would blend well with pelvic PT. It also gave me a lot of perspective into how significant of a role the pelvic floor plays in the entire kinetic chain. I would even say that my pelvic floor education has helped me be a more thorough orthopedic clinician. It has helped me think outside the box and enabled me to be more thorough in my critical thinking when evaluating patients.
What patient population do you find most rewarding in treating and why?
I have two patient populations that I find most rewarding. The first is HIIT athletes. I find this population so fun to work with. They are some of the most dedicated and compliant patients I have. Their love of their sport is often a driving force for them to get and stay healthy. Many of these athletes will even come to my clinic without having pain or dysfunction. They are strictly coming for education and prevention, which I love. After all, PTs as a profession are huge proponents of wellness and prevention. I also love teaching a patient that they can, in fact, continue doing exercises they may have been previously told were not safe to do during pregnancy or postpartum. Giving them hope that they can continue doing what they love after they were afraid they may not is very rewarding.
The second population I love working with is my childbirth prep patients. I LOVE education. I feel like these sessions really highlight that part of physical therapy. These sessions not only address any current concerns a patient is having but also provide education to give them the confidence to birth the way they want. I review everything from what to expect during labor, to different positions for pushing, and how to push. I even have partners come to the sessions so they can learn how to best support the patient during delivery. Hearing from patients that their birth experience was beautiful and just as they had hoped always gives me a lot of joy. I feel honored to be able to be a part of that journey.
What do you find is the most useful resource for your practice?
I find other practitioners the most valuable resource in my practice. There is so much that can be gained from collaborating with other pelvic PTs, doulas, midwives, OB/GYN, sex therapists, etc. Pelvic rehab is so multifaceted, that I believe it truly requires a collaborative approach to provide the best patient outcomes.
What books or articles have impacted you as a clinician?
There was a recent article that came out about the prevalence and significance of Levator Ani avulsion tears. This was an interesting article because I have seen this more and more clinically, but there is very little research on the matter. My favorite books as a clinician are: “The Body Keeps the Score”, “Come As You Are”, and “Pelvic Pain Explained”.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
I think the biggest thing I have learned is that the objective findings of our evaluations are only a small part of the puzzle. Pelvic rehab is an intimate type of physical therapy, and many of our patients may have had trauma that is still raw to them. If most of your evaluation is spent talking with the patients to ensure they feel comfortable, that’s ok. I have realized that it’s ok if I don’t get to every objective test and measure in the first session. In this line of work, patient comfort is most important. Building a rapport with your patient must take precedent.

What made you want to create this course, Pregnancy and Postpartum Considerations for High-Intensity Athletics?
I wanted to create this course because I saw a need in the Crossfit community for more education on how to safely train pregnant and postpartum athletes, and I feel physical therapy is a great place to start, after all, PTs are experts in the musculoskeletal system. We are seeing more and more of these HIIT athletes becoming moms and wanting to maintain their athleticism throughout pregnancy & postpartum, and I think that’s great!
With that being said, I think there are nuances to training this athletic population. There are so many hormonal, anatomical, and structural changes to consider during pregnancy & postpartum, and that may affect how well an athlete can tolerate strain. However, most of these changes are not contraindications to training. Therefore, we as rehab practitioners and physical therapists need to fully understand the demands of HIIT, as well as the specific considerations for this population so that we can keep them safely and effectively doing what they love.
What need does your course fill in the field of pelvic rehabilitation?
By and large, people do not fully understand the demands of HIIT activities like Crossfit unless they personally partake in these activities. This includes healthcare professionals like physical therapists. However, many of our pregnant and postpartum athletes will require the care of a PT (especially pelvic) at some point throughout their pregnancy, and postpartum journey.
My course, Pregnancy and Postpartum Considerations for High-Intensity Athletics bridges the gap between education and experience, for those healthcare professionals who do not personally participate in HIIT to understand the demands of the sport. It also helps those physical therapists who do not specialize in pelvic health to understand the unique demands of this athlete population from a pelvic health perspective.
Who, what demographic, would benefit from your course?
Any PT, PTA, PT student, OT, COTA, or OT student who is looking to better understand the demands of HIIT, the special considerations for pregnant and postpartum athletes who participate in HIIT, and how to safely train and treat these athletes to help them continue to do what they love.
If you could get a message out to physical therapists about pelvic rehab what would it be?
Oh man, where do I start? There are so many things I want to shout from the mountain tops about pelvic PT. It truly is a gem in the field of physical therapy, and I think is often a missing link in traditional physical therapy care. Pelvic rehab is so much more than urinary leakage and kegels. It can be so impactful to the quality of life of a patient. There is no other area of the body that is critical to so many functions but is also so vastly overlooked and undertreated. The need for research, education, and development in this field is critical if we are going to have a true “whole body” approach to treatment.
Join H&W and Emily McElrath on May 21st to learn more about this patient demographic in Pregnancy and Postpartum Considerations for High-Intensity Athletics
Hi Kate, can you tell us about the course you have designed Restorative Yoga for Physical Therapists?
My name is Kate Bailey and I am a pelvic floor physical therapist. I’ve been a pelvic floor PT going on4-5 years now. Before that, I’ve been a pilates instructor for 20 years and taught yoga for over a decade. This course is a culmination of all of my experiences both with the yoga, pilates, and the pelvic floor population from kiddos through adulthood. It allows us to use the techniques from the yoga and pilates philosophies to support people in their healing process from pelvic pain and also just in their bodies.
What can participants expect to learn when they come to the course?
I wrote this course when the pandemic started. My whole intention was to make the didactic information self-paced and watch the videos as often as you want kind of course. This way, when we have dedicated time together it’s a lot more about discussion and me guiding people through the labs, and in turn, they can guide their colleagues or patients. It is designed so I’m not spending a lot of time lecturing to a screen and our time dedicated to each other is more about a conversation. I want people to learn about the information in their own time, marinate in it a little bit, and then come with questions.
How do you feel that restorative yoga fits in with the care we provide to our patients with pelvic health conditions?
The restorative yoga component to me is really special because it’s one of the only times we prioritize rest, and not doing, and sitting with ourselves. Not necessarily trying to get strong, or trying to get more flexible. It’s really about allowing our bodies to be. Sometimes that is being in a little bit of discomfort. Sometimes that is just being with the exhaustion that I think we all have a little bit of. Just learning how to be with ourselves for 8, to 12, to 15 minutes and see that as a really productive part of our treatment plan.
How does trauma-informed care influence your course?
One of the things that I highlight in the course is how much trauma occurs in and around the home. So when we’re asking patients to do a home program one of the discussion points we have in the course is “what if the home is inherently triggering or unsafe?” How can we use concepts of graded exposure to get someone from needing a lot of sensory things, like lights on, windows locked, facing the window, eyes open to slowly getting people toward a little bit more safety. If that is not a possibility, finding another location and strategizing how we can prioritize our own safety and our own ability to relax rather than saying I must relax.
The other component of trauma in the course is the unveiling of how prevalent trauma is. In pelvic health, we talk a lot about sexual trauma because we are dealing a lot with the pelvic floor region and the genitals. One of the things I think we sometimes might be able to speak to more is the little subversive types of trauma. Whether it is emotional trauma, whether it is neglect, whether it is transgenerational trauma or intersectionality trauma…
There’s this other component in yoga that is coming out now that is the trauma that has been handed down through the yoga lineages. What I think is not understood is that a lot of people who practice yoga in a deep way have significant trauma from yoga. The question then is how do we reclaim a practice that is so lovely, done with care and kindness and non harming, for people who have maybe experienced it in a very harmful way – and introduce it as a non-harming, caring, compassionate method for people who haven’t experienced it. The whole idea is about how do you be in rest in your body and in empowerment.
Can you give an example of how a pelvic PT or OT would fit restorative yoga into their practice?
As PTs and Ots we are starting to bring mindfulness in, a lot, to our programming in terms of some of the work from Jon Kabat Zen on how great meditation is for so many things. There is still a question of “How do I put this in my plan of care?” The great thing about this class is that we can speak directly to this. Let's say that you are in a hospital-based scenario, you can give restorative yoga to someone n a hospital bed very easily. They’re not going anywhere and what a great thing to give them: a breathing practice, a concentration practice, and a rest practice.
For someone in private practice, such as orthopedics, this is the type of practice where maybe you’re not giving pelvic floor strengthening if someone has a large degree of overactivity in their pelvic floor. But they still need something to do at home, or they need something to do at the office. Maybe restorative yoga is a little bit too far out there for the patient. Maybe they don’t have a space they can lie down on the floor. That’s when we can say, ok how can we then transfer a pelvic floor restorative yoga posture to a desk situation? Can you cross your legs on your chair and lean forward, and modify it that way.
Then there is this component of the class that is all about breathing. I think we know in pelvic health how wonderful and how great breath-work can be and so some of these techniques can be used as ‘secret exercises’ in your everyday life in addition to being a dedicated practice. We talk about all of that in class.
Watch the full interview with Kate Bailey at the Herman & Wallace YouTube Channel:
Join Kate to learn more about including restorative yoga into your practice with Restorative Yoga for Physical Therapists this year. Courses are scheduled for:
Kate Bailey, PT, DPT, MS, E-RYT 500, YACEP, Y4C, CPI owns a private practice in Seattle that focuses on pelvic health for all genders and ages and works under a trauma-informed model where patient self-advocacy and embodiment are a priority. In addition to being a physical therapist, I’ve been teaching Pilates for nearly 20 years and yoga for over 10. Kate’s course, Restorative Yoga for Physical Therapists, combines live discussions and labs with pre-recorded lectures and practices that will be the basis for experiencing and integrating restorative yoga into physical therapy practice. Kate brings over 15 years of teaching movement experience to her physical therapy practice with specialties in Pilates and yoga with a focus on alignment and embodiment.
Yoga is a common term in our current society. We can find it in a variety of settings from dedicated studios, gyms, inside corporations, online, on Zoom, at home, and on retreat. The basic structure of a typical yoga class is a number of flowing or non-flowing postures, some requiring balance, some requiring going upside down, and many requiring significant mobility to achieve a certain shape. At the end of these classes is a pose called savasana, corpse pose (or sometimes translated for comfort as final resting pose). In this pose, which is often a treat for students after working through class, students lie on the ground, eyes closed, possibly supported by props, and rest. It is perhaps the only other time in the day when that person is instructed to lie on the floor in between sleep cycles.
Savasana is one of many restorative yoga postures. In the work created and popularized by Judith Hanson Lasater, PT, PhD1, restorative yoga has taken a turn away from the active physical postures, breath manipulations, and meditations that are commonplace in how we think of yoga. She has focused on rest and the need for rest in our current climate of productivity, poor self-care, and difficulty managing stress and pain.
In a dedicated restorative yoga class (not a fusion of exercise then rest, or stretch then rest… which are really lovely and have their own benefits), a student comes to class, gathers a number of props, and is instructed through 3 to 5 postures, all held for long durations to complete an hour or longer class. Consider what it would look like to do 3 things over one hour with the intent of resting. It is quite counter-culture. Students have various experiences with this type of practice, but over time many begin to feel the need for rest (or restorative practice) in a similar way that one feels thirsty or hungry.
We know the benefits of rest: being able to access the ventral vagal aspect of the parasympathetic nervous system is what Dr. Stephen Porges2 suggests supports health, growth, and restoration. There is the impact on the ventral vagal complex in the brainstem that regulates the heart, the muscles of the face and head, as well as the tone of the airway. To heal, we need access to this pathway. To manage stress, we need to access this pathway. To be able to choose our actions rather than be reactionary, we need to access this pathway. Restorative yoga is an accessible method that may be a new tool in a patient’s toolbox to help manage their nervous systems.
Join Kate Bailey to learn more about restorative yoga in Restorative Yoga for Physical Therapists this year. Courses are scheduled for:
1. Relax and Renew: Restful Yoga for Stressful Times by Judith Hanson Lasater PT, PhD
2. Polyvagal Theory by Stephen W Porges PhD

H&W is proud to be able to present a new remote course on ethics from new faculty member, and Sr. TA, Mora Pluchino, PT, DPT, PRPC. Mora is a graduate of Stockton University with a BS in Biology (2007) and Doctorate of Physical Therapy (2009). She has been working at Bacharach Institute for Rehabilitation ever since graduation and has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training.
Mora began treating Pelvic Health patients in 2016 and has experience treating women, men, and children with a variety of Pelvic Health dysfunction. In 2020, she opened her own "after hours" virtual practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients and has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules and has been a TA with Herman & Wallace since 2020 with over 150 hours of lab instruction experience. Mora authored and instructs Ethical Concerns for Pelvic Health Professionals.
● You are a new graduate, and your employer sends you to Pelvic Floor Level 1 and expects you to start up a Pelvic Health Program at the facility. Your first scheduled patient is a diagnosis you didn’t learn about and don’t feel comfortable treating, but your student loan payments have started, and you need this job.
● The word has gotten out and referrals are flowing into your clinic after hearing what a life-changing service your Pelvic Health program provides. You have a 6 month long waiting list and your front desk person asks you how to organize the list. Options include prioritizing based on the severity of issues, first come/ first serve, based on past history with the facility, etc.
Put yourself in these situations and reflect. How would you feel? What would you do? All of the situations above have a common theme. They present Ethical Concerns for Pelvic Health Professionals. Ethical situations are very common in day-to-day practice for any health care professional. Treating in the pelvic region can add additional complications due to the level of intimacy and vulnerability in this care.
Ethics by definition is “the division of philosophy concerned with how a person should behave in a matter that is considered morally correct or good” that gives us standards, virtues, and rules (Boone, 2017). The professional code of ethics for each professional category and is grounded in virtue ethics. Virtue ethics includes four main concepts including balance of harms and benefits, doing no harm, justice, and autonomy (Kirsch, 2005)
Whether a practitioner is a physical therapist/ physical therapist assistant, occupational therapist, psychologist, social worker, nurse, doctor, or physician’s assistant, their governing professional organization will have a code of ethics and conduct to help guide these practitioners in good decision making. There are many ethical decision-making models to help guide an individual through the process of identifying, defining, examining, and then problem solving any ethical occurrence.
The RIPS Model, originally presented by Arlanian, Swisher & Davis in 2005, presents an ethical framework to help guide practitioners through the steps needed to address ethical concerns. The world of ethical decision-making is typically one of many options, typically being more “gray area” than simply “black” and “white.” Ethical Concerns for Pelvic Health Professionals is designed to help make these decisions easier to define, examine, discuss, and address so we can have these tough conversations!
Ethical Concerns for Pelvic Health Professionals is a one-day remote course that covers ethical considerations for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day-to-day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety, and compliance. The purpose of this class is to explore the ethical challenges Pelvic Health practitioners may experience including consent, managing trauma and abuse, and preventing misconduct. To learn more join us in Ethical Concerns for Pelvic Health Professionals on June 18, 2022!
Research:
Boone, B. (2017). Ethics 101: From altruism and utilitarianism to bioethics and political ethics, an exploration of the concepts of right and wrong. Adams Media.
Kirsch, N. (2005). Ethics in Physical Therapy: A Case-Based Approach. McGraw Hill Publications. American Physical Therapy Association.
Kristina Koch, PT, DPT, is a board-certified women’s health physical therapist and certified lymphedema therapist who is the author/instructor of the remote course Pharmacologic Considerations for the Pelvic Health Provider. She has been treating pelvic health dysfunction in all ages and genders since 2001. Kristina works in private practice in Colorado Springs, CO, and has served as a guest lecturer for the pelvic health content at Regis University in Denver and the University of Colorado.
Did you know that the median length of time a primary care provider spends with a patient is 15 minutes? This breaks down to approximately 5 minutes for the patient to talk about their health concerns and 5 minutes for the health care provider to speak, with the rest being applied toward paperwork (1). After this appointment, the patient may not be seen again for several months or even a year. Medication side effects that impact the patients’ quality of life, or create new symptoms, can be easily overlooked.
I created the course, Pharmacologic Considerations for the Pelvic Health Provider because, with direct access to physical and occupational therapy services, a greater responsibility has been placed upon the therapist to take on more of a role as a primary care provider. We must ensure that all factors contributing to a patient’s signs and symptoms are considered. This includes reviewing and assessing if medications or supplements may be causative.
As therapists, we typically spend more time with our patients than their primary care providers. We are seeing them for longer periods during a treatment session and will see them numerous times throughout a month or longer. As a result, our patients have a greater opportunity to discuss their signs and symptoms with us versus their physician or primary care provider. Therefore, understanding how medications may be impacting a patient is essential. Being able to educate the patient about the side effects of the medications they are taking and how the medications may be contributing to their complaints can enhance the value of the treatment session.
By possessing this knowledge and understanding of the medications that are prescribed to treat pelvic health, therapists can have educated conversations with our patients and other health care providers involved in their care. The ability to discuss the most recent medications and supplements or complementary alternatives, that may minimize side effects or have fewer impacts on quality of life and enhance function, is an integral part of patient care.
Join Kristina to dive into Pharmacologic Considerations for the Pelvic Health Provider. This one-day, virtual course will discuss the importance of understanding pharmacology and review commonly prescribed medications. Kristina also spends time explaining current research pertaining to the pharmacologic treatment of numerous pelvic and reproductive health conditions, medication side effects, drug interactions, and non-pharmacologic alternatives. Medications discussed include those for constipation and GI dysfunction, pelvic pain conditions (including vulvodynia, chronic prostatitis, and endometriosis), as well as medications and side effects in Gender-Affirming Care for patients who are transitioning.
Upcoming 2022 course dates for Pharmacologic Considerations for the Pelvic Health Provider include:
References:
- Tai-Seale, M., McGuire, T. G., & Zhang, W. (2007). Time allocation in primary care office visits. Health Services Research. 42(5), 1871-1894. Doi:10.1111/j.175-6773.2006.00689.x
- Ciccone, C. D. (2007). Pharmacology in Rehabilitation. (4th). F.A. Davis Company.