This is a common question that faculty member, Mercedes Eustergerling, is asked. To paraphrase this question – why does H&W (a pelvic rehabilitation institute) offer a breastfeeding course – Breastfeeding Conditions? Well, if you consider that new parents who are breastfeeding have just experienced a birthing event then the answer is – it has plenty to do with pelvic rehabilitation.
Most pelvic therapists have exposure to patients who have given birth and are experiencing a range of postpartum pelvic issues including painful intercourse, prolapse, and incontinence. Have you considered how breastfeeding affects these issues? After giving birth the body’s levels of estrogen drop and the levels of prolactin rise. Prolactin is the hormone responsible for stimulating milk production and will remain elevated during breastfeeding. Thus, estrogen levels remain low during this time and can result in vaginal dryness, delayed menses, low libido, and painful sex.
Women or any person who has experienced childbirth, with pelvic organ prolapse (POP) are often told that the condition will improve after breastfeeding. While many do see improvement after weaning their child there is no correlation between breastfeeding slowing the healing of pelvic floor muscles or worsening POP long-term (1). POP has been linked with sleep quality (2). Which anyone with a newborn can tell you is in short supply. Not surprisingly, sleep is important for your body to recover from birthing, managing postpartum mood disorders, and of course, staying awake to take care of your baby. For breastfeeding parents, sleep deprivation is a way of life as they are waking up every 2-3 hours to feed their baby and establish a strong milk supply. It may be beneficial at this point for the new parent to work with a lactation consultant. These professionals can guide new parents through latching, feeding, milk supply issues, breast pump use, and can help reduce stress and promote optimal rest and recovery postpartum.
Mercedes pointed out in a past interview that “Anytime we talk about breastfeeding we are talking about two people working together, the mother and the baby, it's a team effort. As physiotherapists, we can help with issues or conditions that arise on the maternal (breast) side of things, and on the infant side of things. When it comes down to it, the physiotherapist's role is not about what or how much (nutrition) gets into the baby’s belly, but rather how it gets in (mechanics).” Fast milk flow can make the task of suckling more difficult for babies with an uncoordinated suck/swallow/breathe pattern. If the mechanics or timing is off, the infant will prioritize airway protection and may appear to go on and off the breast throughout the feed.
Another common concern for postpartum parents is urinary incontinence, aka bladder leaking. Breastfeeding does not make incontinence worse, but there is research showing that breastfeeding triggers intense thirst in relation to plasma vasopressin, oxytocin, and osmoregulation (3). The connection is that drinking more water due to this thirst will increase your urge frequency and possible urine leakage.
Mercedes Eustergerling’s remote course Breastfeeding Conditions provides a thorough introduction to the physiology of the lactating breast, dysfunction, treatment interventions, and further discusses the pelvic rehab therapist’s role in breastfeeding and pumping support. As a rehab therapist, it is within the scope of practice to assess and treat breast inflammation and pain such as mastitis, blocked ducts, milk blebs, and cracked nipples. However, Mercedes also discusses when it is important to refer to other health care professionals.

Mercedes sat down with The Pelvic Rehab Report this week to talk about herself and her course.
Tell me a little bit about yourself and your practice.
I studied physical therapy to work with athletes and quickly developed an interest in chronic pain and complex health conditions. As I worked with these populations, I found that I wasn’t able to fully evaluate or treat them without a better understanding of pelvic health, so I took continuing education in pelvic health, and my skills as a physical therapist expanded tremendously.
Then I had a baby and encountered every infant feeding hurdle you can imagine. At our lactation appointments, I was fascinated by it all and realized that I could not provide whole-person physical therapy without understanding the physiology and conditions that are unique to lactating individuals.
In my practice today, I work as a part of a team that provides physical therapy and mental health occupational therapy for chronic pain, trauma, pelvic health, breast health, and infant feeding. We teach courses and workshops, and we do research in chronic pain and breast health.
How do you incorporate physical therapy principles when helping parents meet feeding goals?
At its core, physical therapy is about optimizing a person’s function. What makes physical therapy for infant feeding interesting is that we consider the functional goals and limitations for two individuals: the parent and the infant. In this course, the focus is on the parent’s function. Physical therapists already have the knowledge and skills necessary to manage inflammation, pain, and skin integrity. We apply a biopsychosocial, trauma-informed approach to concerns such as musculoskeletal overuse injuries, ergonomics, breast inflammation, and nipple wounds. Physical therapists are especially helpful for individuals with existing musculoskeletal, neurological, or cardiorespiratory conditions because of our extensive knowledge in these areas
What made you want to create this course?
I was asked to create a course for physical therapy in lactation and infant feeding after attending a women’s health course and discussing it with a colleague. At the time, I was in a solo practice and seeing patients with breast inflammation. They would go onto their parenting groups on Facebook and advise other parents to seek physical therapy for blocked ducts, mastitis, etc. The problem was that I was the only physical therapist in the country providing this service! As physical therapists received requests from their patients to help with these conditions, they started looking for continuing education opportunities.
A lot of our information on lactation comes from oral history that is passed down from one generation to the next. This is a beautiful thing from a cultural perspective. However, one of my goals in creating this course was to provide evidence-based information for health professionals so we could deliver the best care possible. For lactating individuals, there is no shortage of advice or opinions on every topic. I dove into the literature to compile information for a research-informed course and I continue to review the literature and update the course often.
If you could get a message out to practitioners about bodyfeeding and lactation what would it be?
This is a population that is underserved and needs care. In all studies done on the subject, pain is consistently one of the top three reasons for stopping chest/breastfeeding. Physical therapists have unique training and backgrounds that make us a valuable resource for these individuals. It is not difficult to apply our existing knowledge and skills once we gain some understanding of the anatomy, physiology, and sociocultural context of lactation.
What lesson have you learned that has stayed with you and impacted your practice?
When I met one of my first patients with mastitis, she was curled up on the exam table and the lights in the room were off. Her partner answered all my questions because she felt too ill to talk. Two days later, she came to her appointment with makeup on and smiling. She said she was feeling like herself again. I have a great deal of sympathy for anyone experiencing the acute symptoms of breast inflammation and I take care to consider their psychosocial impacts instead of treating it as a purely physical condition.
What do you find is the most useful resource for your practice?
There is a phenomenal community of lactation professionals in my city of Calgary, Canada. We are fortunate to have physicians who specialize in lactation and infant feeding, and they value collaborative care. I shadowed with them in their clinics for 500+ hours and gained a great deal of skills and knowledge from a medical perspective. Now, we continue to collaborate and I am able to refer patients for an evaluation or to check any possible red flags. I encourage all physical therapists entering this practice area to connect with lactation professionals and physicians in their area.
What books or articles have impacted you as a clinician?
The works of Donna Geddes and Maya Bolman have changed my understanding of breast anatomy, physiology, and inflammation. Similarly, the World Health Organization’s publication on mastitis was a great introduction to the pathophysiology and available literature.
A book that I have read several times and recommend to those who are interested in the pediatric side of things is Supporting Sucking Skills in Breastfeeding Infants by Catherine Watson Genna. And in 2021, a book on breastfeeding and public health was published with a chapter on the role of physical therapists, which I wrote. That book is called Lactation: A Foundational Strategy for Health Promotion by Suzanne Hetzel Campbell. The chapter on physical therapy for lactation and infant feeding can be helpful to understand our role and communicate how this practice area fits into our scope of practice.
Breastfeeding Conditions is a two-day remote course and is scheduled for:
This course may be of interest to you if you have taken any other the other H&W peripartum courses including:
- · Pregnancy Rehabilitation
- · Postpartum Rehabilitation
- · Pregnant and Postpartum Rehabilitation Special Topics
- · Doula Services and Pelvic Rehab Therapy
- · Medical Perspective in Peripartum Care
- · Perinatal Mental Health: The Role of Pelvic Rehab Therapist
- · Pregnancy and Postpartum Considerations for High-Intensity Athletics
References:
- Iris S, Yael B, Zehava Y, et al. The impact of breastfeeding on pelvic floor recovery from pregnancy and labor [published online ahead of print, 2020 May 19]. Eur J Obstet Gynecol Reprod Biol. 2020;251:98-105. doi:10.1016/j.ejogrb.2020.04.017
- Ghetti C, Lee M, Oliphant S, Okun M, Lowder JL. Sleep quality in women seeking care for pelvic organ prolapse. Maturitas. 2015;80(2):155-161. doi:10.1016/j.maturitas.2014.10.015
- James RJ, Irons DW, Holmes C, Charlton AL, Drewett RF, Baylis PH. Thirst induced by a suckling episode during breastfeeding and relation with plasma vasopressin, oxytocin, and osmoregulation. Clin Endocrinol (Oxf). 1995;43(3):277-282. doi:10.1111/j.1365-2265.1995.tb02032.x

Mia Fine, MS, LMFT, CST, CIIP is the creator of the remote course, Sexual Interviewing for Pelvic Health Therapists. This course is for pelvic rehab therapists who want to learn tools and strategies from a sex therapist’s toolkit who works with patients experiencing pelvic pain, pelvic floor hypertonicity, and other pelvic floor concerns. Mia (they/she) is a student of Queer Theory, Intersectionality, and Social Justice and offers holistic, anti-oppressive, and trauma-informed therapy in the Seattle area.
As a Licensed Marriage and Family Therapist, Certified Medical Family Therapist and trained AASECT Certified Sex Therapist, Mia has clocked hundreds of hours in direct client contact, supervision, and consultation. She has also attended numerous sex therapy trainings, continuing education opportunities, and trains incoming sex therapists on current modalities and working with vulnerable client populations.
Sexuality is core to most human beings’ identity and daily experiences. Human beings are hard-wired for connection, intimacy, and pleasure. When there are concerns relating to our sexual identity, sexual health, and capacity to access our full potential, it affects our quality of life and holistic well-being. Practitioners who work with folks on issues of sexual health and decreasing sexual dysfunction are in the position to encourage awareness and healing. Mia shares, “Imagining a world where human beings don’t walk around holding shame or traumatic pain is imagining a world of health and happiness.”
Unwanted sexual pain often goes unaddressed because culture does not teach the interactions between feelings, relationships, and the body. Our society often tells us that there is something wrong with us, that we are defective, for wanting a healthy sex life and for addressing our human needs/sexual desires. People are not taught that sex should not be painful and that pain is our body giving us information that something is going on. It’s not uncommon that most people who experience sexual pain often feel as if they are broken. Mia’s favorite thing to say is that “No person is broken. Each and every one of us are uniquely special beings worthy of being loved and nurtured.”
Providers must be aware of their own biases and be introduced to the various sexual health resources available to providers and patients. Mia further stresses, "Always listen to your patient to understand what they are saying and feeling. Do not respond defensively. Remember that this can feel like a threatening situation for patients. It is vital that providers working with pelvic floor concerns have the necessary education and training to work with patients on issues of sexual dysfunction."
From a business standpoint, happy patients are more likely to return to your practice in the future, recommend your practice to their friends, and pay their bills on time and in full. Patients want to have quality interactions with a healthcare provider who cares about them. As a practitioner, your satisfied patient is more likely to make follow-up appointments and maintain their prescribed treatment plan, which can lead to more positive outcomes.
Sexual Interviewing for Pelvic Health Therapists offers current and empirically-founded sex therapy and sex education resources for both the provider as well as the patient. Mia will broaden your scope of competence in working with patients who experience forms of sexual dysfunction and who hope to live their full sexual lives. This course will add the extensive skills of interviewing for sexual health. It also offers the provider a new awareness and self-knowledge on their own blind spots and biases.
Check out Mia's interview with Holly Tanner on the Herman & Wallace YouTube Channel for more information on the course.
Sexual Interviewing for Pelvic Health Therapists - Remote Course
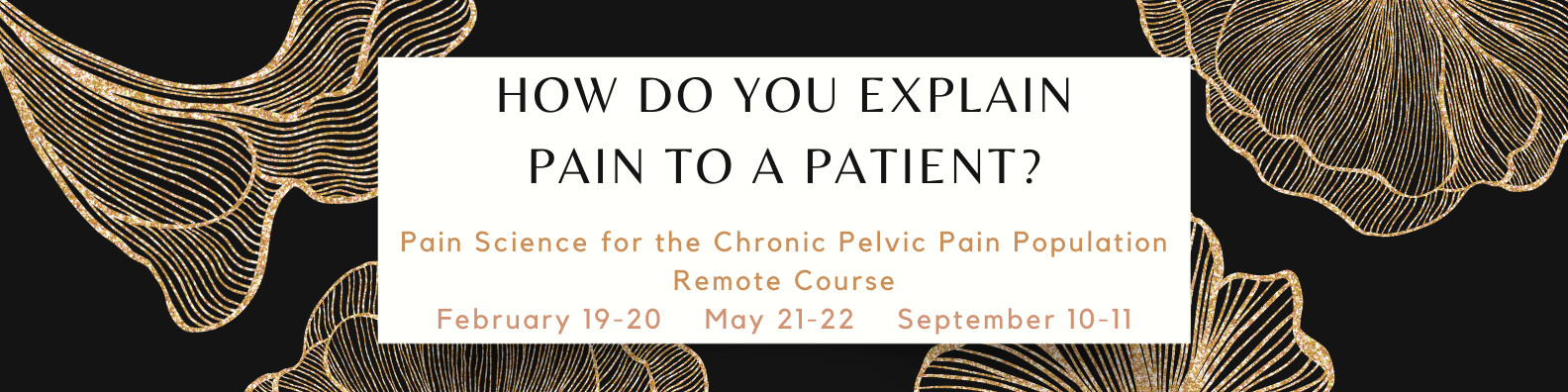
How do you explain pain to a patient? How do you reeducate the nervous system to be less sensitive? These are the questions that Tara Sullivan, PT, DPT, PRPC, WCS, IF, and Alyson N Lowrey, PT, DPT, OCS address in their new course Pain Science for the Chronic Pelvic Pain Population. The chronic pain population is often dismissed or misled that they have something drastically wrong with them, or worse, nothing wrong with them at all. Alyson and Tara share that “this population often has the most functional deficits and the worst clinical outcomes. We want to change that.”
Tara has specialized exclusively in pelvic floor dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012. Alyson became involved with pelvic rehabilitation through working in a clinic with Tara Sullivan. She is a board-certified orthopedic specialist and primarily works with the ortho patient population. When Tara came into the clinic she brought along the pelvic floor population and they joined forces. Alyson, with her ortho perspective, is better able to recognize that in some of her orthopedic patients, a lot of their pain was coming from the pelvic floor. The pelvic pain patient population crosses over from physical therapy to the orthopedic and occupational therapy worlds. By treating their patients wholistically Tara and Alyson have been able to make a huge difference to both of their practices.
By focusing specifically on the topic of pain science in their new course, Tara and Alyson delve into the true physiology of pain including the topics of central and peripheral sensitization. Pelvic specialists that can benefit from this course are those whose patients have chronic pelvic pain including endometriosis, interstitial cystitis, irritable bowel syndrome, vaginismus, vestibulodynia, primary dysmenorrhea, and prostatitis. The biggest thing is to learn how to recognize if there is a sensitization component to your patient’s pain.
Alyson shares that being able to recognize chronic pain in the patient is huge, that this is “not your regular patient who has a peripheral injury and we just need to rehab them through that process. It’s a whole different ballgame when we’ve got our nervous system in a hypersensitive state.” She continues, “a huge part of the treatment is educating your patient about pain and trying to decrease the fear around movement…and how we use our words to decrease fear is huge.” This course also discusses how to desensitize the nervous system through dry needling, diaphragmatic breathing, sleep hygiene, and bowel and bladder retraining.
Pain Science for the Chronic Pelvic Pain Population is scheduled for February 19-20, May 21-22, and September 10-11. This course is targeted to physical therapists, occupational therapists, physical therapist assistants, occupational therapist assistants, registered nurses, nurse midwives, and other rehabilitation professionals. The full interview with Tara Sullivan and Alyson Lowery is available on the Herman & Wallace YouTube channel.

Elena Teare, the Communications Lead from Open Arms Perinatal Services sat down with The Pelvic Rehab Report to discuss their organization and annual fundraiser Labor of Love.
For our practitioners who are not familiar with Open Arms, can you tell me the organization?
Open Arms is the leading independent, community-based program in Washington State providing wraparound perinatal services to low-income families. We serve nearly 300 families every year and our award-winning program is not hospital-directed or based. Our trusted, community-centered approach always prioritizes the unique cultural, linguistic, and emotional needs of each client free of charge.
We provide services across four program areas: birth doulas, community-based outreach doulas (who provide in-home support up to two years of age), family support services, and lactation support peer counseling. We also train emerging birth workers to serve families in their own communities.
Our communities of focus are Black/African American, Somali, Latinx, and American Indian/Alaska Native communities of King, Snohomish, and Pierce counties. 87% of our clients are of color.

Can you share a success story?
In 2019, Asha was experiencing homelessness when pregnant with her second child. She heard about Open Arms through her shelter and soon was matched with Suad Farole, a Community-Based Outreach Doula. Originally from Somaliher through pregnancy, birth, and her daughter for two years. When Asha became pregnant with her son in late 2020, she knew she wanted Suad to be with her. In Asha’s words, “When I first decided to get a doula, I didn’t expect what I received. Suad was a true gift that not only oversaw the safety of my child as she came into this world, but she truly cared for my well-being and helped me to become the mother that I am now.”
What is the importance of the yearly Labor of Love event?
Labor of Love is our most important fundraising event of the year! It is a chance for us to engage our community and highlight the extraordinary outcomes our families achieve. When community members invest in the work that we do, they provide Open Arms with the flexibility to allocate dollars to any part of the organization that needs extra support. Given the uncertainty in today’s world, it’s important that we have the ability to respond quickly to the changing circumstances of our client families.

What makes you, the staff, volunteers, and the community passionate about this organization?
Our approach is evidence-informed, culturally appropriate, and community-centered and is effective in reducing medical interventions and the costs of perinatal care. By prioritizing the emotional needs of birthing people, our staff and volunteers set the stage for new mothers and parents to be strong and confident advocates for their children and families. By removing the cultural barriers to perinatal care by providing culturally competent care, we facilitate better community linkage to the health care system.
Our doulas and lactation consultants, as well as community of midwives, are committed to improving the health outcomes for birthing people and children of systematically underserved communities. Our families’ outcomes exceed those of Washington state and the country. As of 2021, 95% of our families give birth at full term and healthy birth weight, 85% avoid unplanned cesareans, and 82% are still breast/chestfeeding at six months.[i]
How do persons in need find your organization and what partnerships do you have?
Many of our families are referred from other organizations and service providers, and others find us through word of mouth in the community. Through our Perinatal and Lactation Support Collaborative, we have strong partnerships with the organizations like the Center for Indigenous Midwifery, Generations Midwifery Services, Global Midwifery Services, The Pacific Islander Health Board of Washington, and Rainier Valley Midwives. Additionally, the Program for Early Parenting Support (PEPS) and the Tubman Center for Health and Freedom are additional partnerships we have.

What is the awareness level in the community of Open Arms?
Open Arms clients are referred from other community partners and agencies who trust us to provide the best possible, culturally sensitive care. Over 30% of our referrals are from previous clients who seek our services again or refer friends and family.
How can people who are interested in supporting Open Arms donate or support the organization?
Interested supporters can make a gift to Open Arms online at https://www.openarmsps.org/get-involved/donate/make-gift-today/. To make an even bigger difference in the lives of the families we serve, community members can join our Baby Whisperers Monthly Giving Circle with a sustaining monthly gift. We also value gifts of time and welcome volunteers to assist with some of the behind-the-scenes logistics of the organization. People can stay up to date with our work and opportunities to get involved by heading to our site and subscribing to our newsletter or following our social media channels.

[i] Compared to King county’s rates: 91% of people give birth at full term; 93% are at a healthy birth weight, and 39% are breast/chestfeeding at six months.

Elijah Sharrieff is the content writer for My Community Health Network. MYCHN is a full-service healthcare provider in Houston Texas, that provides accessible health care in multiple Houston Communities. Elijah specializes in blogs that educate patients on relevant topics such as: prenatal care, mental health, the importance of diet and exercise, and dental care. Elijah’s holistic approach to health care blogging stems from his background in education. Elijah taught preschool, middle school, and tutored college and high school students. Teaching allowed Elijah to realize the interconnected nature of health as it relates to the mind and body.
Cervical Health Awareness
Cancer is among the leading causes of death in America. Despite this, cancer is one of those things that you don't think will happen to you. We like to think we are healthy individuals, but cancer is unpredictable and complicated.
Around 300,000 women are diagnosed with cervical precancers in America. MYCHN has created a list of prevention tips to ensure a healthy cervix!
What Causes Cervical Cancer?
Cervical Cancer typically develops when healthy cervix cells grow and multiply continuously. In other words, they don't die like normal cells. Instead, these continually replicating cells form a mass, also known as tumors.
In many cases, HPV can lead to cervical cancer. However, an HPV diagnosis doesn't mean you will be diagnosed with cervical cancer.
What are Cervical Cancer Risk Factors?
Risk factors can increase your cancer risk. There are multiple risk factors for cervical cancer; some of them may surprise you.
- Sexual history: Your sexual history can put you more at risk for cervical cancer.
If you are sexually active at a young age (18 years old and under)
- Diet: If you do not consume a balanced diet, you could be at higher risk for cervical cancer
- Cervical Cancer in the family: If you have family members who have cervical cancer, your chances of developing cervical cancer are higher than if no one in your family has it. In some cases, this is because of rare inherited conditions that make it harder for some women to fight HPV.
- Smoking: It's a difficult habit to quit. However, smoking has been shown to harm the body. Women who smoke are twice as likely to develop cervical cancer.
Tobacco by-products have been found in the cervical mucus of women who smoke. Some studies have shown that the chemicals in cigarettes can damage the DNA of cervix cells. This occurrence can lead to the development of cervical cancer.
How can you Have a Healthy Cervix?
Prevention is going to be vital to lowering your risk of cervical cancer. What are some cervical cancer prevention methods?
- Pap Smear:
A pap smear is a screening that looks for abnormal changes that could lead to cancer. Luckily, cervical cancer doesn't develop overnight, so regular pap smears are useful in cervical cancer prevention.
- Following up with your health care provider:
Following up with your health care provider is crucial to cervical health. Health care providers provide access to pap smears and other preventative measures.
- Get the HPV Vaccine:
The HPV vaccine protects against sub strains of HPV that lead to cervical cancer.
- Limit your sexual partners:
Unfortunately, HPV is easily spread. It is relatively easy to become exposed to HPV. The virus spreads through skin-to-skin contact, so it can be spread without having sex. The American cancer society has stated that HPV can be spread through hand to genital contact.
With the aforementioned in mind, limiting the number of sexual partners could put you at a lower risk of HPV.
- Stop smoking:
Smoking is a tough habit to shake. However, the consequences of smoking are severe for the body's health in the long term. Many cigarettes and tobacco products have harmful cancer-causing chemicals. In addition, smoking weakens your immune system.
A weakened immune system makes it harder for your body to fight viruses like HPV. Just a gentle reminder, HPV can lead to cervical cancer.
Pap Smear Near Me
According to The World Health Organization, cervical cancer is the fourth most common cause of cancer in women. Pap Smears are an excellent cervical cancer prevention method. MYCHN offers pap smears and other women's health services. We have 11 locations in the metropolitan Houston area.
CHN Cares for patients with private insurance, Medicaid, Medicare, and uninsured! Visit https://mychn.org/services/womens-health/ for more.
Bottom Line
Cervical cancer is common cancer for women and, in many cases, can be deadly. Thankfully, there are prevention methods to prevent the disease. For example, regular Pap smears can be used to prevent Cervical cancer.
Eating a balanced diet and not smoking can also be excellent prevention methods.
My Community Health Network. MYCHN is a full-service healthcare provider in Houston Texas, that provides accessible health care in multiple Houston Communities.
References:

Sarah Haran PT, DPT, OCS, CF - L2 earned a BS in exercise science from Gonzaga University and a DPT from the University of Washington. She has been practicing in Seattle for almost 15 years and opened her private practice, Arrow Physical Therapy in 2016. Her specialties include dance medicine, the CrossFit and weightlifting athlete, and conditions of the hip and pelvis such as femoroacetabular impingement and labral tears. In 2017, she began coaching other PTs who wanted to start their own practices and from there, she co-founded Full Draw Consulting with her partner Dr. Kate Blankshain. Together, they offer coaching, consulting, and several 8-week online business courses for Physical Therapy entrepreneurs. Sarah Haran instructs Weightlifting and Functional Fitness Athletes, next scheduled for February 26th, 2022.
As a physical therapist who works with CrossFit® athletes, I want to address a persistent problem we have in our professional community. Many PTs don’t know what to do with CrossFit® athletes.
When CrossFit® first came on the scene, a lot of PTs would encounter athletes who had injuries or dysfunctions related to their sport. Perhaps shoulder pain from kipping pull-ups or low back pain from deadlifts or kettlebell swings, maybe stress incontinence from box jumps.
Whatever it was, it seemed like we were seeing Crossfitter after Crossfitter in our practices. Was it that they were injuring themselves more than other athletes? Was it that their sport was bad and full of terrible ideas and awful coaching? I think what we were seeing was the quick growth of a popular sport (lots of people participating) and a community of people who not only were pushing themselves in the gym but who were interested in getting better and back into the gym quickly (ie. seeking rehab quickly). And then we were seeing rehab professionals who didn’t know how to help and were overwhelmed by the complexity of the sport.
And while there are some folks in healthcare who would like to see CrossFit® lose popularity, the reality is that it is here to stay and you will likely be faced with treating these athletes in some capacity. But what do we do with them? How do we keep our patients healthy when they want to continue to participate in CrossFit®??
The 3 primary duties of the physical therapist:
- Work to understand the sport
- Educate ourselves about where in the body these injuries commonly occur and how they happen
- Design rehab programs:
- ○ which address training volume just as we would in any other sport
- ○ that are functional to these athletes
- ○ that supplement CrossFit® workouts with accessory work to:
-
- ■ drill positions
- ■ strengthen weaknesses
- ■ mobilize tightness
- ■ improve endurance for these positions/movements

The messaging we need to communicate to our CrossFit® patients:
- Form and technique need to come first… then volume, weight, difficulty, and intensity.
- Mobility is not just flexibility; we also need to emphasize stability through a range of motion.
- Scaling and modifying is critical to all athletes at some point in their career. Work with your PT and coach to make appropriate decisions.
- CrossFit® is here to stay. Let’s keep our athletes in this sport for the long haul.
Treating CrossFit® athletes has been a primary passion of mine for many years and it is very exciting to be able to offer a course with Herman & Wallace that introduces the sport to other PTs. You do not have to be a CrossFit® athlete or specialist to want to help these patients and we want all the fabulous PTs out there to be able to impact the CrossFit® community effectively.
Weightlifting and Functional Fitness Athletes will review the history and style of Crossfit exercise and Weightlifting, as well as examine the role that therapists must play for these athletes. Common orthopedic issues presented to the clinic will be examined.
Check out the Herman & Wallace YouTube Channel for the full interview with Dr. Yeni
Dr. Oluwayeni Abraham stumbled into the niche field of fertility. She shares, "I had all of these women who would come in with painful periods that would have significant post-surgical problems and would end up having fertility concerns. As I was picking up my visceral mobilization techniques, I started to see that I was able to help women conceive and help women who maybe have experienced reoccurring miscarriages actually carry to term. That's when I said, "I think I'm doing something here that could be something else." That's when I tried to hone in on the specific skills that were influencing and maximizing the results and outcomes.
In Dr. Yeni's course, Fertility Considerations for the Pelvic Therapist, she shares manual therapy techniques and a lot of data on hormones, the endocrine system, and other pieces of the puzzle. The language in the fertility world is based on these building blocks. Specific fertility-related diagnoses are discussed that help you formulate a pathway in treatment. Another important thing Dr. Yeni teaches is how to collaborate and work with these other providers that are going to be on this journey with your patients.
When working with fertility it's important to ask ourselves how do we bring value to this puzzle? How do we bring value after someone has had multiple failed IVF cycles? We can't just say we're going to do a bunch of manual work. We also have to speak the language and understand the body in its entirety and how it's playing a role in being able to maximize fertility outcomes.
When asked what sparks her passion and keeps her so excited about working with this population Dr. Yeni stated, "the outcomes! We're still therapists, and we love to see results."
Fertility Considerations for the Pelvic Therapist - Remote Course
This course requires each registrant to have a live model. Due to the nature of labs, please be sure your model or partner is not pregnant and does not have an IUD for safety. Additionally, those with hydrosalpinx will not be able to participate in uterine mobility techniques but can still attend the course.
Katie McGee, PT, DPT, (they/them) is a pelvic health physical therapist based in Seattle. Katie received their Doctor of Physical Therapy from the University of Washington in 2014 and their board certification as a Women’s Health Clinic Specialist (WCS) in 2018. Their practice, B3 Physical Therapy, centers on transgender care and perinatal rehabilitation. Join H&W and Katie to learn about perinatal mental health in Perinatal Mental Health: The Role of Pelvic Rehab Therapist - Remote Course scheduled for February 5, 2022.
Due to the COVID-19 pandemic, rates of perinatal mental health conditions—such as anxiety and posttraumatic stress disorder—have risen sharply1. Around 70% of pregnant people are now reporting psychological distress1. With many families under increased stress and financial worry, the odds of developing postpartum depression have jumped from one in seven to one in five(1)!
Fortunately, pelvic rehabilitation therapists can make a difference in the mental health of their perinatal clients. In fact, many pelvic rehab therapists are reducing the risk of perinatal mental health issues without even knowing it! Simply supporting clients in keeping up with physical activity and reducing bodily pain are proven strategies for lowering the risk of perinatal mental health issues (2,3). Pelvic rehab providers can go even further in supporting their perinatal clients’ mental health with some simple actions:
1. Ask – Many birthing people feel shame around negative feelings and thoughts related to pregnancy and postpartum. Asking perinatal clients about their emotional challenges can help break through that shame. A good ice breaker for talking about perinatal mental health is letting your clients know that a mood disorder is the number one complication of pregnancy. Be sure to listen attentively and avoid interruption whenever someone discloses their mental health challenges.
2.Screen – Screening for mental health conditions can guide pelvic rehab therapists to know when it’s time to refer clients to specialized care, such as medication and/or therapy. Pelvic rehab therapists are qualified to use several screening tools in the perinatal period, including the Edinburgh Postnatal Depression Scale, the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7. Best of all, these tests are free to use and easy to administer.
3. Gather resources – When a client discloses that they have thoughts of self-harm or are experiencing violence in their home, you want to be prepared with the next steps to help. Collecting resources ahead of time can go a long way in turning what would have been a fumbling offer to help into a confident action plan. Looking to grow your resource list? Check out these three links:
- Perinatal Mental Health Resources: https://www.postpartum.net/
- Intimate Partner Violence Resources: https://www.rainn.org/
- Substance Use Resources: https://www.samhsa.gov/
4. Connect – Racism leads to People of the Global Majority birthing in the United States to experience increased rates of preterm birth and low infant birth weights (4). Both these outcomes have been tied to worse postpartum mental health (5). Research shows that when People of the Global Majority are connected to culturally congruent birth doulas, rates of preterm birth and low infant birth weights fall (6). Other research similarly supports the concept that when people are paired with culturally congruent providers, health outcomes improve (7). Whenever possible, think about how you can offer your clients resources/referrals that match their identity and background to support their mental wellbeing.
5. Learn – Join Katie McGee, PT, DPT (they/them) for the Herman & Wallace course, Perinatal Mental Health: The Role of Pelvic Rehab Therapist - Remote Course scheduled for February 5, 2022. By participating in this remote learning class, you will:
- Develop a basic understanding of perinatal mood and anxiety disorders
- Bolster your listening skills for working with perinatal clients
- Gain additional tips for screening for perinatal mental health issues
- Learn how to help clients create perinatal wellness plans
- Expand your toolbox of coping skills to teach clients
Don’t miss this opportunity to truly change the lives of your perinatal clients!
References
- Yan H, Ding Y, Guo W. Mental Health of Pregnant and Postpartum Women During the Coronavirus Disease 2019 Pandemic: A Systematic Review and Meta-Analysis. Front Psychol. 2020;11:617001.
- Mathur VA, Nyman T, Nanavaty N, George N, Brooker RJ. Trajectories of pain during pregnancy predict symptoms of postpartum depression. Pain Rep. 2021;6(2):e933.
- Marconcin P, Peralta M, Gouveia ÉR, et al. Effects of Exercise during Pregnancy on Postpartum Depression: A Systematic Review of Meta-Analyses. Biology (Basel). 2021;10(12):1331.
- Andrasfay T, Goldman N. Intergenerational Change in Birthweight: Effects of Foreign-born Status and Race/Ethnicity. Epidemiology. 2020;31(5):649-58.
- Anderson C, Cacola P. Implications of Preterm Birth for Maternal Mental Health and Infant Development. MCN Am J Matern Child Nurs. 2017;42(2):108-14.
- Thomas MP, Ammann G, Brazier E, Noyes P, Maybank A. Doula Services Within a Healthy Start Program: Increasing Access for an Underserved Population. Matern Child Health J. 2017;21(Suppl 1):59-64.
- Towning EJ, Purohit A. Black babies cared for by black doctors less likely to die in the US: revolutionize medical education to tackle the problem in the UK. BMJ. 2020;370:m3783.
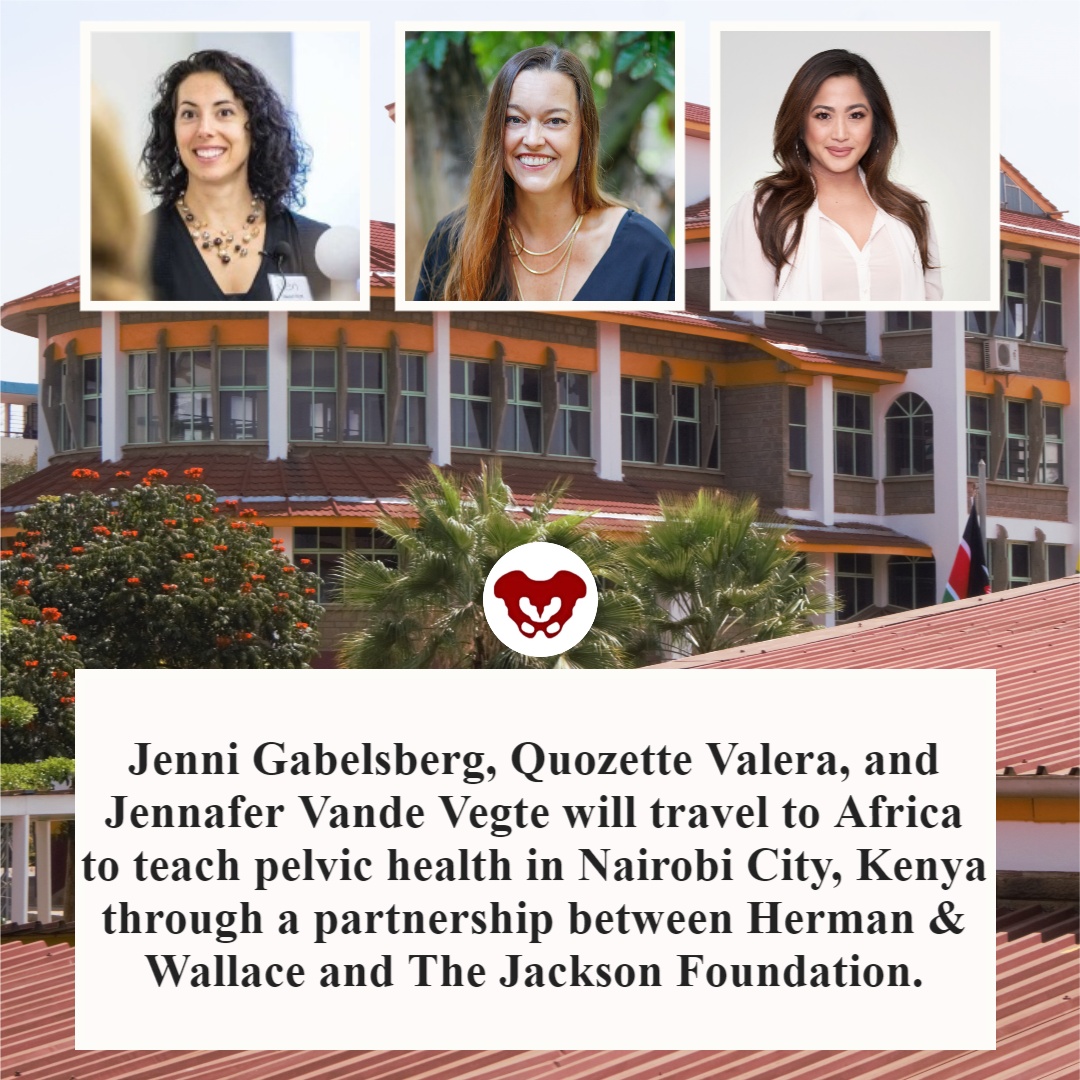
Faculty members Jenni Gabelsberg DPT, WCS, MSc, MTC and Jennafer Vande Vegte, PT, BCB-PMD, PRPC along with senior Teaching Assistant Quozette Valera PT, DPT will travel to Africa to teach pelvic health in Nairobi City, Kenya through a partnership between Herman & Wallace and The Jackson Foundation. These instructors will be teaching two modules of comprehensive pelvic health training with the goal of creating a self-sustaining, continuous education program taught and offered locally. In addition to training a cohort of physiotherapists in assessing and treating the pelvic floor, these American faculty members will be mentoring local Kenyan therapists to teach these courses in an ongoing manner. We at the Institute are proud and thrilled to be a part of spreading this knowledge and skillset in this currently-underserved region.
The courses offered will comprise H&W's Pelvic Floor Series, with the addition of content relevant to Kenya, including obstetric fistula and female genital mutilation. According to the Worldwide Fistula Fund, there are ~ 2 million women and girls suffering from fistulas. Estimates range from 30 to 100 thousand new cases developing each year; 3-5 cases/1000 pregnancies in low-income countries. A woman may suffer for 1-9 years before seeking treatment. For women who develop fistula in their first pregnancy, 70% end up with no living children.
Have you ever had a dream hidden so deep in your heart you never even spoke it aloud?
The dream for me, to someday teach internationally will come to fruition in February 2022. Jenni Gabelsberg DPT, WCS, MSc, MTC; Quozette Valera PT, DPT; and I will travel to Africa to teach pelvic health in Nairobi City, Kenya through a partnership between Herman & Wallace and The Jackson Foundation.
Richard Jackson, a prominent clinician, educator, and businessman himself (The Jackson Clinics, Richard Jackson Seminars, and The Jackson Foundation), had his own dream to build the quality of physical therapy in Africa by educating and empowering clinicians through an evidence-based curriculum developed by Richard and taught by his staff. Richard served two years in the Peace Corps in Kenya in the late 70s. He taught PT at Kenya Medical Training College. In 2010 a former colleague of his moved from the US back to Ethiopia to address and equip PT education and educators in the country. This led to a partnership where Richard helped develop the first DPT program in Africa. “We were in Ethiopia for seven years. We started a residency program that turned into a doctoral program in physical therapy. In December 2017, we graduated 17 DPTs and now we are out. It is sustainable. It’s up to them to carry on and they have the curriculum and the skills,” said Richard in this article.
In 2012 the program Richard stated reproduced and blossomed in Nairobi, Kenya. Let’s talk for a second about what the field of PT is like in Kenya. In a country of almost 54 million people, there are about 2,000 PTs. Thirty-five percent (700) are women, as reported by the Kenya Society of Physiotherapists. The degree is a diploma that takes 3 years to earn, and there are 9 programs available.
There is a women’s health section along with other specialty sections. Medical care has both private and public facilities which can have a wide variation in amenities. After offering specialty training in orthopedics and neurology, Richard recognized the need to expand training to pelvic health. Thus, a partnership between Herman & Wallace, The Pelvic Health and Rehab Center, and The Jackson Foundation was born. In 2019 three cohorts of teachers: Nancy Cullinane PT, MHS, WCS, Kathy Golic PT, and Terri Lannigan PT, DPT, OCS taught module one; Kathy Golic, Casie Danenhauer, and Sherine Aubert fielded a second module; and then educated and equipped the first class of 35 pelvic health graduates. The foundation of the Kenyan Pelvic Health Program thus laid; the future looked bright!
Then…covid brought everything to a screaming halt.
Almost three years later, the program will eagerly resume in Nairobi City.
One can imagine in a country with so few therapists, so few female therapists, and even fewer (think under 50!) pelvic health therapists, the desperate need for pelvic health training and treatment is difficult to fathom. Add to that the strain of a rather patriarchal society where women's health may not be readily accepted or addressed.
In her blog about her experience in Kenya, Sherine Aubert reflects, “To me, this two-week course was way beyond teaching pelvic floor physical therapy - it was truly empowering women to speak up for themselves and each other in the medical community. It provided a voice for anyone suffering from pelvic floor issues to seek help.”
As for Jenni, Quozette, and I, we are beyond humbled and excited to be a part of this experience. Per Richard, "Everyone has come back from these experiences profoundly changed."
If you would like to support this program, we are open to your ideas, expertise, and connections. You can also make a tax-deductible donation to The Jackson Foundation here.
If you have connections to help us bring donations of pelvic health supplies, please contact one of us at This email address is being protected from spambots. You need JavaScript enabled to view it. or This email address is being protected from spambots. You need JavaScript enabled to view it.
For further information:
Read about Richard Jackson.
- https://www.middleburglife.com/world-class-care-at-the-jackson-clinics/
- https://www.orthopt.org/uploads/content_files/files/Jackson.pdf
- https://www.teachandtreat.org/
Read about the 2019 pelvic health training in Kenya:
- https://hermanwallace.com/blog/pelvic-floor-level-1-is-heading-to-kenya
- https://hermanwallace.com/blog/week-one-at-kenya-medical-training-college-in-nairobi-kenya
- https://hermanwallace.com/blog/the-second-course-module-in-nairobi-kenya
Read more about PT in Kenya:
This article was submitted by Aparna Rajagopal and LeeAnn Taptich. Both practitioners are based out of the Henry Ford Macomb Hospital in Michigan where Aparna Rajagopal, PT, MHS is the lead therapist of their pelvic dysfunction program, and Leeann Taptich DPT, SCS, MTC, CSCS leads the Sports Physical Therapy team. Michigan. They work very closely together at the hospital which gives them a very unique perspective of their patients. Aparna and LeeAnn instruct the Breathing and the Diaphragm course. This remote course explores how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes.
COVID-19 has been a part of our vocabulary for almost 2 years now and has changed the world we live in. COVID-19 is a virus that affects the cardiovascular, digestive, urinary, and respiratory systems. We still do not have adequate evidence to guide our treatment of COVID -19 patients in their sometimes prolonged recovery phase. Research continues to be made available about the short and long-term effects of the virus on our bodies.
An example of a post-COVID-19 patient was a female with complaints of difficulty taking in a deep breath. She also reported that the physical act of breathing felt like a lot of work/effort. She had undergone all sorts of respiratory and cardiac testing and had been cleared from a medical standpoint. Upon talking to the patient, it was discovered that she wasn't complaining of shortness of breath/dyspnea.
Instead, this patient was complaining about having to expend a lot of energy to perform the mechanical action of breathing. She reported that this had started after she had experienced moderate COVID - 19 symptoms for about a month. The patient did extremely well with a plan of treatment aimed at improving mobility in the soft tissues and joints of the thorax while working on establishing a breathing pattern with a focus on improved overall expansion. An incidental benefit of her treatment was a dramatic reduction in her symptoms of urinary urgency which she had developed during her COVID-19 recovery stage.
Recently, a clinical commentary in the Journal of Women’s Health Physical Therapy talked about the possibilities of pelvic floor dysfunction developing on account of COVID-19 (1). Since COVID 19 affects the respiratory system, we can postulate that something involving the respiratory system will possibly have an effect on the pelvic floor due to the unique relationship shared between the pelvic floor and the diaphragm.
Recovering COVID 19 patients may have changes in their musculoskeletal system. These changes may include increased accessory muscle use, decreased chest wall mobility (including the associated joints and muscles), and altered breathing mechanics due to both the disease process and possibly the immobility of bed rest.
The upcoming Breathing and the Diaphragm course helps practitioners understand the connection of dysfunction pertaining to respiration and how it can affect the pelvic floor. In this course, Aparna Rajagopal and LeeAnn Taptich will instruct you to look at the body as a whole while assessing and treating for mobility deficits, motor control deficits in terms of breathing dysfunction presented by these patients.
References:
1. Siracusa C, Gray A. Pelvic floor considerations in COVID-19. Journal of Women’s Health Physical Therapy. 2020; 44(4): 144-151.