Mental Health is a very serious global concern! As a health care provider, I have seen my patients anxious, scared, confused, tearful, depressed, and sometimes in sheer panic with debilitating anxiety and pain. As they express these emotions, they look for a glimmer of hope and look up to me with the trust that I as their provider will be able to “fix” all their concerns. I have felt the immense burden they carry and many times their emotions cross over and affect me too.
At that moment, the only thought racing through my mind was how could I decrease their physical and psychological distress to help them “feel better.” How could I decrease the burden they carry not just physically, but mentally and emotionally, and how could I empower them with the tools and strategies to build both physical and mental resilience?
The American Physical Therapy Association (APTA) supports interprofessional collaboration at the organizational and individual levels to promote research, education, policy, and practice in behavioral and mental health to enhance the overall health and well-being of society consistent with APTA’s vision. Physical, behavioral, and mental health are inseparably interconnected with overall health and well-being. It is within the professional scope of physical therapist practice to screen for and address behavioral and mental health conditions in patients, clients, and populations. This includes appropriate consultation, referral, or co-management with licensed health services providers in the prevention and management of behavioral and mental health conditions (1) through its position statement HOD P06-20-40-10.
The APTA also endorses evidence-based complementary and integrative interventions (HOD P06-18-17-47) underscores the importance of incorporating Integrative medicine practices within physical therapy. At the State level, as a member of the American Physical Therapy Association of New Jersey (2), I have been actively involved in Co-Charing the new Integrative Physical Therapy (IPT) Special Interest Group. IPT blends traditional physical therapy methods with holistic practices that address the whole person—physically, mentally, emotionally, and spiritually. This initiative aims to enrich therapists' capabilities in delivering Integrative Physical Therapy by leveraging a variety of methodologies, including Yoga, Mindfulness, Tai Chi, Hydrotherapy, Acupuncture, Acupressure, Zero Balancing, Reiki, Nutrition and Energy medicine to name a few.
According to the National Center of Complementary & Integrative Health (NCCIH), a branch of the National Institutes of Health (NIH), Mental health problems are common. In the United States, they affect about one-fourth of adults in any given year. According to the World Health Organization, mental illnesses account for more disability in developed countries than any other group of illnesses. Anxiety and mood disorders are the most common mental health problems. Researchers are investigating complementary and integrative health approaches for a variety of mental health problems, including anxiety & depression (3).
Anxiety disorders are one of the most common mental health concerns with a major contribution to the global burden of disease. Pharmacology and psychotherapy stand for the conventional treatment for anxiety disorders but these present limited efficacy, especially in the case of chronic anxiety, with high relapse rates often causing adverse side effects (4).
Anxiety is a natural part of the human experience, often serving as a protective mechanism in response to potential threats. However, when symptoms become chronic, disproportionate, or uncontrollable, anxiety can escalate into a clinical disorder. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), anxiety disorders vary in presenting symptoms and may include excessive worry, panic attacks, restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbances. Beyond these distressing psychological and emotional disturbances, the sequelae of anxiety extend into the realm of physical health. Research has pointed to a correlation between anxiety and increased pain responses, as well as the exacerbation of musculoskeletal disorders (5).
 Anxiety disorders have profound implications on both mental and physical health.
Anxiety disorders have profound implications on both mental and physical health.
There is growing interest in manual therapy modalities, with emerging research to alleviate related symptoms (5). A systematic review by West et al (2024) found that individuals receiving manual therapy interventions displayed a statistically significant reduction in anxiety intensity. The use of Acupressure for Anxiety is a common practice in Integrative Medicine, and the literature supports Acupressure as an effective and feasible alternative treatment for decreasing anxiety. A systematic review and meta-analysis published by He et al. (2019) found moderate evidence that Acupuncture and/or Acupressure was significantly associated with reduced cancer pain and decreased use of analgesics.
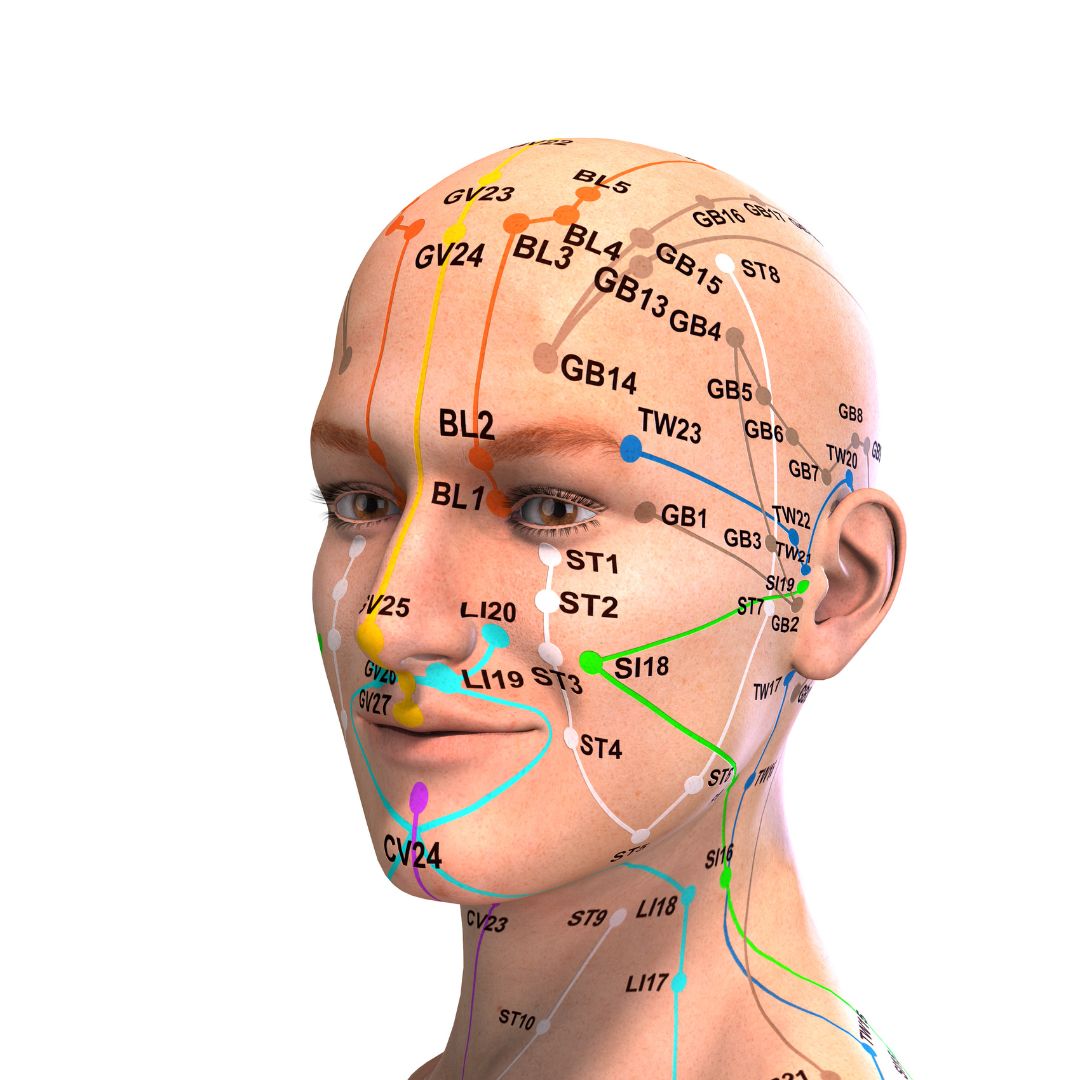
Acupressure is part of Traditional Chinese medicine (TCM), which is a comprehensive science that studies human health and disease. A central relational element of TCM is Yin and Yang, which refer to opposites, mutually exclusive yet complementary substances within the human body and the outside world. Based on the theory of the balance of Yin and Yang and the interaction of five elements (五行) (metal, wood, water, fire, and earth), TCM analyzes changes in the five Zang organs (五脏) (liver, heart, spleen, lung, and kidney), six Fu organs (六腑) (gallbladder, stomach, large intestine, small intestine, bladder, and triple energizer), extraordinary Fu-organs (奇恒之腑) (brain, marrow, bone, pulse, gallbladder, uterus, and ovary), meridians (the channels of basic substances transportation and connecting inside and outside of the human body), and qi-blood-body fluid (the basic substances constituting and maintaining the human life activities) (6).
A recent study by Yang et al (2021) cited several key Acupressure points that can help with Anxiety & fatigue (Heart 7, Spleen 6), chemotherapy-induced nausea, vomiting and anxiety in women with breast cancer ( Pericardium 6), primary dysmenorrhea ( Liver 3 ), anxiety & pain in cancer patients (Large Intestine 4, Heart 7), pre-operative cesarean section anxiety (Yintang EX-HN 3 and Heart 7), anxiety from the anticipation of surgery or treatment (Yintang EX-HN3, Heart 7 & Pericardium 6).
The literature also provides robust scientific evidence supporting Acupressure as an effective non-pharmacological therapy for the management of a host of conditions such as insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions to name a few.
Case Study Clinically, our ability to target the nervous system to make a change in a patient’s pain and anxiety is extremely valuable from a pain neuroscience perspective. Recently a patient in her early 60s walked into the clinic with high anxiety and rectal pain rated 15/10. She reported that she spoke to her best friend and her friend who had found relief for anxiety with urinary retention with Acupressure had urged her to see me. She said, “I have tried everything, and you are my last hope!”
Clinically, our ability to target the nervous system to make a change in a patient’s pain and anxiety is extremely valuable from a pain neuroscience perspective. Recently a patient in her early 60s walked into the clinic with high anxiety and rectal pain rated 15/10. She reported that she spoke to her best friend and her friend who had found relief for anxiety with urinary retention with Acupressure had urged her to see me. She said, “I have tried everything, and you are my last hope!”
This patient had been to the ER twice over a span of 3 months and had undergone extensive testing with no diagnostic pathology. The only position she could find relief was in a side-lying but she was so distressed at the thought of “spending the rest of my life on the couch” that she refused to lie down in that position during the day, even if it meant relief from her excruciating pain.
The first thing I taught her was to notice how shallow her breath was, and how to use her breath deeply and actively to decrease her pain and anxiety by using two key Acupressure points Central Vessel 17 (CV 17), located at the center of her chest and Yintang EX-HN3, located between the eyebrows. CV17 is known to be a point for emotional healing while Yintang (EX-HN 3) is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM). Within a few minutes, the patient felt very calm and relaxed and felt that she now had some control over her symptoms.
She was now able to focus and actively listen to me as I explained to her that we needed to work not just on the physical body, but also the mental, emotional, and energy body. I guided her to accept the “positional preference” of her body and “align” herself mentally and physically with what makes her “feel better.” So instead of feeling bad every time she thought about lying down to decrease her pain, I taught her to feel empowered that she had one position that she could use to break the cycle of her pain. This shift in how she approached her pain, as well as the potent Acupressure points to alleviate pain and anxiety, were a tremendous relief to her. I sent her home with a breathwork practice, a pelvic girdle stretching program, and an Acupressure program that targeted key Acupoints for self-regulation. The patient returned the next visit and reported that her pain was down from 15/10 to 5/10.
Over the course of the next few visits, using a combination of Acupressure as a self-regulation tool, targeted stretching of the lower back & pelvic girdle musculature, manual therapy, self-care, and breath work and awareness, this patient gained complete control over her anxiety and pain. She felt much calmer and empowered to have a physical self-regulation Acupressure practice which she could use to improve both her physical and mental health.
As a holistic pelvic health practitioner, who is psychologically informed with an Integrative physical therapy clinical practice, I recognize the deep-rooted mind-body connections and the need to address the “whole” person. In all the ancient and modern Energy healing practices, the breath is the key to working with the physical, mental, emotional, and the energy body. Acupressure is a powerful evidence-based energy healing practice that can be combined with breathing to heal the body in multiple dimensions. When a patient can “breathe better” and “feel better,” they can be steered easily towards building both physical and mental resilience.
As healthcare providers, we share this mental and emotional burden with our patients, and we must empower them with the tools and strategies to live healthy pain-free and anxiety-free lives.
To learn more about Acupressure, please join us for the upcoming remote course Acupressure for Optimal Pelvic Health scheduled for Feb 1st & 2nd. The course will introduce course participants to the basics of Traditional Chinese Medicine (TCM), Acupuncture & Acupressure. Of the 12 major Meridians or energy channels, this course will focus on the Bladder, Kidney, Stomach, and Spleen meridians. In addition, there are other important Meridian points that stimulate the nervous system and can be used for self-regulation to manage Anxiety, pain, and a host of other symptoms. The course also offers two potent Acupressure home exercise and wellness programs.
This course explores Yin yoga as a powerful holistic practice with Acupressure and will offer an evidence-based perspective on how Yin poses within each meridian can channelize energy through neurodynamic pathways with powerful integrative applications to facilitate healing in multiple dimensions.
References
- The Role of the Physical Therapist and the American Physical Therapy Association in Behavioral and Mental Health: Position statement https://www.apta.org/apta-and-you/leadership-and-governance/policies/role-pt-apta-behavioral-mental-health
- American Physical Therapy Association of New Jersey: Integrative Physical Therapy Special Interest Group https://aptanj.org/page/IPTSIG
- National Center of Complementary & Integrative Health (NCCIH) https://www.nccih.nih.gov/health/anxiety-and-complementary-health-approaches
- Amorim D, Amado J, Brito I, et al. Acupuncture and electroacupuncture for anxiety disorders: A systematic review of the clinical research. Complement Ther Clin Pract. 2018;31:31-37. doi:10.1016/j.ctcp.2018.01.008
- West KL, Huzij T. A systematic review of manual therapy modalities and anxiety. J Osteopath Med. 2024;124(11):487-497. Published 2024 Jun 24. doi:10.1515/jom-2024-0001
- Yang J, Do A, Mallory MJ, Wahner-Roedler DL, Chon TY, Bauer BA. Acupressure: An Effective and Feasible Alternative Treatment for Anxiety During the COVID-19 Pandemic. Glob Adv Health Med. 2021;10:21649561211058076. Published 2021 Dec 12. doi:10.1177/21649561211058076
- He Y, Guo X, May BH, et al. Clinical Evidence for Association of Acupuncture and Acupressure With Improved Cancer Pain: A Systematic Review and Meta-Analysis. JAMA Oncol. 2020;6(2):271-278. doi:10.1001/jamaoncol.2019.5233
- Zhang SQ, Li JC. An introduction to traditional Chinese medicine, including acupuncture Anat Rec (Hoboken). 2021;304(11):2359-2364. doi:10.1002/ar.24782
- Abbott R, Hui EK, Kao L, et al. Randomized Controlled Trial of Acupressure for Perception of Stress and Health-Related Quality of Life Among Health Care Providers During the COVID-19 Pandemic: The Self-Acupressure for Stress (SAS) Trial. Am J Med Open. 2023;10:100056. doi:10.1016/j.ajmo.2023.100056
- Chen SR, Hou WH, Lai JN, Kwong JSW, Lin PC. Effects of Acupressure on Anxiety: A Systematic Review and Meta-Analysis. J Integr Complement Med. 2022;28(1):25-35. doi:10.1089/jicm.2020.0256
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
Author Bio
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
 Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has since been working in outpatient hospital and private practice settings with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has since been working in outpatient hospital and private practice settings with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna currently practices in an outpatient setting. Her clinical practice has focused on an Integrative physical therapy approach blending traditional physical therapy methods with holistic practices that address the whole person - physically, mentally, emotionally, and spiritually. She specializes in working with pelvic health patients who have bowel and bladder issues with high pelvic pain which sparked her interest in Eastern holistic healing traditions and complementary medicine. She has spent many hours training in holistic healing workshops with teachers based worldwide. She is a member of the American Physical Therapy Association and a member of APTA’s Academy of Orthopaedic Physical Therapy and the Academy of Pelvic Health Physical Therapy.
Rachna also owns TeachPhysio, a PT education and management consulting company. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
An Ancient Science with a Modern Evidence-Based Approach
A 15-year-old patient walked into the clinic with her mom presenting with symptoms of constipation, lower abdominal spasms, and pain with bowel movements. Over the course of the visit, I learned that she was on medication for depression and was also suffering from chronic anxiety. Anxiety pervaded every aspect of her life, from things happening during the day to her near and far future. Her symptoms were worse when her anxiety was high and she struggled to relax her body and mind.
So, in addition to teaching her a program with breathing exercises, self-abdominal massage, pelvic girdle stretching, and the use of a squatty potty, I also taught her perineal self-acupressure at the acupoint Central Vessel 1 (CV 1) for constipation and two self-regulation points Central Vessel 17 (CV 17) and Yintang (EX-HN 3) for alleviating her anxiety.
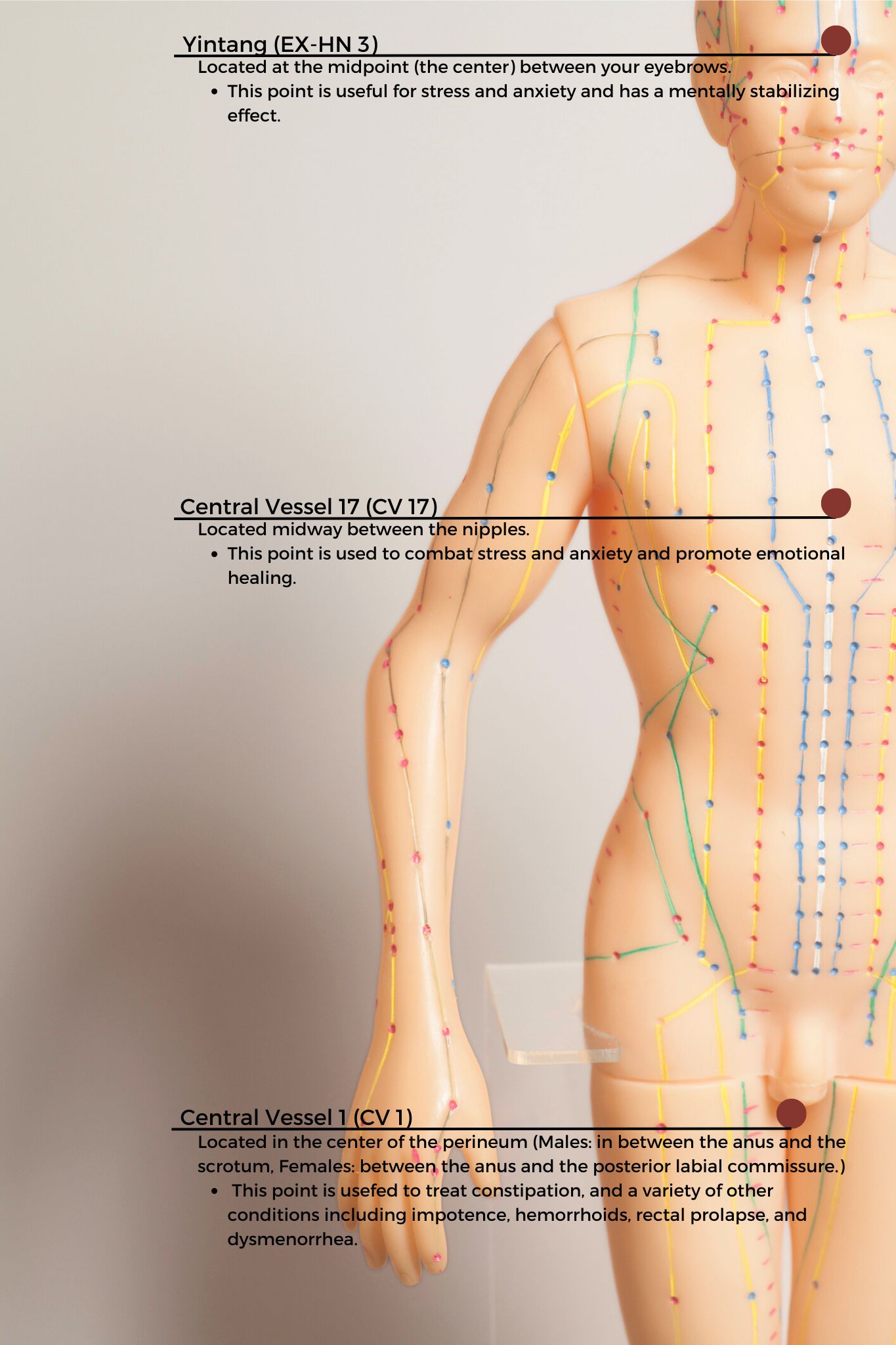 CV1 also known as Huiyin is located at the perineum. A study by Abbott et al. reported that the perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. CV17 is located at the center of the chest and is known to be a point for emotional healing while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM).
CV1 also known as Huiyin is located at the perineum. A study by Abbott et al. reported that the perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. CV17 is located at the center of the chest and is known to be a point for emotional healing while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM).
The patient returned the next visit and reported that her abdominal spasms were 50% better and she no longer had pain with bowel movements. She also reported that she felt calmer and was able to use the perineal self-acupressure technique to evacuate very quickly. Over the past several years, I have found that adding Acupressure to my clinical practice has added so much value as an Integrative holistic tool to complement traditional care.
Evidence-based Integrative health and medicine practices blend traditional physical therapy methods with holistic practices that address the whole person-physically, mentally, emotionally, and spiritually (Justice et al). Acupressure is considered an Integrative medicine practice and is based on traditional Chinese meridian theory in which acupuncture points are pressed to stimulate the flow of energy or Qi. Acupuncture meridians are believed to form a network throughout the body, connecting peripheral tissues to each other and to the central viscera. This tissue network is also continuous with more specialized connective tissues such as periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (Kaptchuk).
There is robust scientific evidence supporting acupressure as an effective non-pharmacological therapy for the management of a host of conditions such as anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions to name a few.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety (Monson et al).
To learn more about Acupressure, join the upcoming remote course Acupressure for Optimal Pelvic Health scheduled for October 12th-13th. This course introduces practitioners to the basics of traditional Chinese medicine (TCM), acupuncture & acupressure, and provides an introduction to Yin yoga. Of the 12 major Meridians or energy channels, the focus is on the majority of acupoints in the Bladder, Kidney, Stomach, and Spleen meridians. In addition, there are other important meridian points that stimulate the nervous system and can be used for self-regulation, improving the flow of Qi the life force energy to improve the physiological functioning of the organs. The course also explores Yin poses within each meridian to channelize energy through neurodynamic pathways with powerful integrative applications across multiple systems. If you are not able to attend the October course date, then check out the website for the options scheduled for 2025.
References
- Chen SR, Hou WH, Lai JN, Kwong JSW, Lin PC. Effects of Acupressure on Anxiety: A Systematic Review and Meta-Analysis. J Integr Complement Med. 2022;28(1):25-35. doi:10.1089/jicm.2020.0256
- Abbott R, Ayres I, Hui E, Hui KK. Effect of perineal self-acupressure on constipation: a randomized controlled trial. J Gen Intern Med. 2015;30(4):434-439.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.
- Justice C, Sullivan MB, Van Demark CB, Davis CM, Erb M. Guiding Principles for the Practice of Integrative Physical Therapy. Phys Ther. 2023;103(12):pzad138. doi:10.1093/ptj/pzad138
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Abaraogu UO, Igwe SE, Tabansi-Ochiogu CS. Effectiveness of SP6 (Sanyinjiao) acupressure for relief of primary dysmenorrhea symptoms: A systematic review with meta- and sensitivity analyses. Complement Ther Clin Pract. 2016;25:92-105
- He Y, Guo X, May BH, et al. Clinical Evidence for Association of Acupuncture and Acupressure With Improved Cancer Pain: A Systematic Review and Meta-Analysis. JAMA Oncol. 2020;6(2):271-278. doi:10.1001/jamaoncol.2019.5233
AUTHOR BIO
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
 Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna currently practices in an outpatient setting. The majority of her clinical orthopedic practice has focused on treating musculoskeletal, neurological, pre- and post-operative surgical conditions to name a few. She specializes in working with pelvic health patients who have bowel & bladder issues with high pelvic pain which sparked her interest in Eastern holistic healing traditions and complementary medicine. She has spent many hours training in holistic healing workshops with teachers based worldwide. She is a member of the American Physical Therapy Association and a member of APTA’s Academy of Orthopaedic Physical Therapy and Academy of Pelvic Health Physical Therapy.
Rachna also owns TeachPhysio, a PT education and management consulting company. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC, RTY 200 is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions.
As I walked into the room to greet a new patient, I quickly glanced at the prescription for Pelvic Floor Physical Therapy in her chart. The words “urinary retention” caught my attention. As I gathered her history, I learned that this patient had a history of high anxiety and had been to the ER twice within a few weeks with symptoms of urinary retention. She was now taught to self-catheterize herself to manage her symptoms. After comprehensive testing by her urologist ruled out obstructive and neurological causes, she was referred to pelvic floor therapy with a diagnosis of pelvic floor muscle tension and inability to relax her pelvic floor muscles.
Urinary retention, or the inability to voluntarily void urine, is one of the most prevalent presenting urologic complaints in the emergency department. Voluntary urination requires close coordination between muscles of the pelvic floor, bladder, and urethra, as well as the nerves innervating them.
Female urinary retention is either acute or chronic and can be categorized according to the International Continence Society as:
- Complete (full retention) or partial (high post-void residuals)
- Acute or chronic
- Symptomatic or asymptomatic
- Mechanism (obstructive or non-obstructive)
Two of the most common causes of chronic urinary retention in women are bladder muscle dysfunction and obstruction. The condition is important as it can lead to significant clinical problems if left untreated, such as bladder decompensation, hydronephrosis, renal failure, vesicoureteral reflux, nephrolithiasis, and urinary tract infections, as well as symptoms including suprapubic pain, feelings of incomplete emptying, weak urinary stream, urgency, and incontinence1.
The patient was anxious and worried and could not step out more than an hour away from her home as she feared she would need to return home to void. She could only void at her own home and her social life was extremely limited due to these voiding restrictions. Given her high anxiety, I initiated Acupressure points for Anxiety in her program as an evidence-based holistic practice.
Acupressure is widely considered to be a powerful Complementary & Alternative Medicine (CAM) therapy and is gaining acceptance within the medical community as part of an Integrative medicine approach. It draws its roots from Acupuncture which is part of Traditional Chinese Medicine (TCM) believed to be over 3000 years old. TCM is based on Meridian theory where key Acupressure points (or Acupoints ) lie along specific meridian lines and are connected to the visceral functions of vital organ systems.
Research shows that Acupressure points have been used with Emotional Freedom Techniques (EFT) as well as for the management of pain, anxiety, nausea, fatigue, urinary incontinence, constipation, and symptom management. Studies over the past few decades have found that Acupressure points transmit energy or the vital Qi (life force energy ) through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety2.
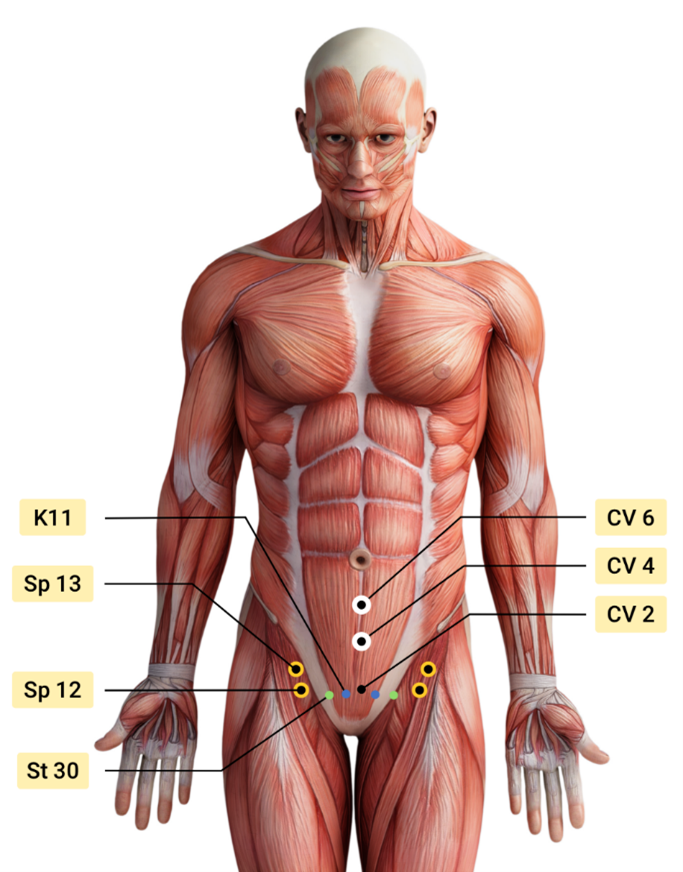
Over the next few weeks, the patient was treated by a multidisciplinary team including her Primary Care Physician, Psychologist, Acupuncturist, and Pelvic floor Physical Therapist. Integrating Acupressure along with manual therapy, behavioral modifications, exercises, breath work and stretching, key potent points in the Central Channel, Kidney, Stomach, Spleen, and Bladder meridians were utilized to down-regulate her nervous system and improve the physiological functioning of her vital organs.
The patient was also taught to use perineal acupressure points for the management of intermittent constipation. The patient learned and practiced daily an Acupressure Anxiety points regimen along with traditional rehabilitation exercises, and became calmer and more mindful with complete resolution of urinary retention symptoms. She could now step outside her home and use public bathrooms which socially was a big achievement for her.
The course Acupressure for Optimal Pelvic Health next offered on Feb 4th -5th 2023 explores Acupressure as an evidence-based modality for the management of Anxiety, Stress, Pain, and Symptom management. The course also teaches two programs with specific potent points for Anxiety and for Daily Wellness and introduces Yin Yoga as a complementary practice to Acupressure. This course is curated and taught by Rachna Mehta PT, DPT, CIMT, PRPC, RYT 200. Rachna has integrated Acupressure as part of her rehabilitation toolbox for several years now bringing holistic healing and wellness to her patients.
References
- Leslie SW, Rawla P, Dougherty JM. Female Urinary Retention. [Updated 2022 Nov 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538497/
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of acupressure on anxiety: a systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
- Son CG. Clinical application of single acupoint (HT7). Integr Med Res. 2019;8(4):227-228.
- Kwon CY, Lee B. Acupuncture or Acupressure on Yintang (EX-HN 3) for Anxiety: A Preliminary Review. Med Acupunct. 2018;30(2):73-79.
- Abbott, R., Ayres, I., Hui, E. et al. Effect of Perineal Self-Acupressure on Constipation: A Randomized Controlled Trial. J GEN INTERN MED30, 434–439 (2015).
Acupressure for Optimal Pelvic Health
Course Dates:
February 4-5, June 3-4, October 14-15
Price: $450
Experience Level: Beginner
Contact Hours: 12.50
Description: This continuing education course is a two-day seminar that offers participants an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, stress, and bringing the body back to a state of physiological balance are integrated throughout the course.
Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung, and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 is Board certified in Orthopedics, a Certified Integrated Manual Therapist, and a Herman & Wallace certified Pelvic Rehab Practitioner. Rachna has a personal interest in various eastern holistic healing traditions and she noticed that many of her chronic pain patients were using complementary health care approaches including acupuncture and yoga. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
A patient walks into the clinic 30 minutes late for their appointment with me, brimming with anxiety and apologizing profusely. “I’m so sorry,” they say, “I kept driving around in circles and could not find a single parking spot.” Another patient, a teacher, reports that her anxiety and pelvic pain progressively worsens as her day progresses and peaks when she gets home with her own two young children at the end of a long day. A third patient with a 15-year history of pelvic pain with unexplained infertility who has failed every conventional ART treatment suddenly conceives her miracle child naturally with acupuncture. She shares, “My anxiety was always so high, I could never relax. They stimulated acupuncture points all over my body, and it worked. My anxiety was so much under control this time.”
Here are the things running through my mind as I work with these patients:
- What could be the most effective hands-on clinical intervention I could use to calm them down?
- Could I teach them daily acupressure self-care and wellness regimens to alleviate anxiety?
- Could I foster a feeling of self-control in them to manage anxiety in stressful situations?
- How does acupuncture really work for infertility, and why does it use points all over the body?
- Can acupressure be used to stimulate key potent acupoints for anxiety?
- Is there a physical practice of yoga that is calm and meditative and is complementary to acupressure?
These questions led to researching the currently available evidence, and I found that there has been a rising clinical interest in complementary holistic practices over the last several decades for anxiety & chronic stress management. Current research supports both acupressure and yin yoga as powerful tools in the realm of energy medicine.
Acupressure is based on 3000 years of Traditional Chinese Medicine (TCM) that believes in Meridian Theory and energy channels which are connected to the function of the visceral organs. There is emerging scientific evidence of acupoints transmitting Qi energy through the vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera with potentially powerful integrative applications across multiple systems. This network is also continuous with more specialized connective tissues such as the periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (1). Fascia and connective tissue literally pervade every anatomic dimension in the body.
Helene Langevin (2) and colleagues proposed an anatomical/ physiological parallel to explain some of the key concepts of TCM.
- Qi: Sum of all body energetic phenomena (e.g. metabolism, movement, signaling, information exchange)
- Meridian Qi: Connective tissue biochemical/bioelectrical signaling
- Blockage of Qi: Changed connective tissue matrix composition leading to a change in signal transduction
- Restoration of the flow of Qi: Cellular activation/gene expression leading to restored connective tissue matrix composition and signal transduction
Modern acupressure charts map the principal 12 meridians connected to the physiological functions of key organs. The key meridians to focus on in pelvic health patients would be the bladder, kidney, spleen, and stomach meridians. Acupressure is systemically effective for a host of conditions including anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions. Each acupressure point has many internal connections to the visceral organs. Stimulating these points by using acupressure assists the body’s self-regulating mechanisms and facilitate healing and neurophysiological quieting.
A recent study by Elizabeth Monson (3) and colleagues retrospectively analyzed 519 acupressure treatments on hospitalized patients, nurses, and the general public across six US states. They followed a specific acupressure protocol and looked at pre- and post-treatment in conjunction with self-rated pain and anxiety scores, where 0 represented no pain or anxiety, and 10 represented the worst pain and anxiety. They found that:
- Hospitalized patients demonstrated a 4 point ↓ in pain scores and 5 point ↓ in anxiety scores
- Nurses demonstrated a 3 point ↓ in pain scores and 4 point ↓ in anxiety scores
This study concluded that acupressure is a highly satisfactory complementary therapy that can demonstrate a clinically significant decrease in self-rated pain and anxiety scores (2).
A robust body of research also attests to yoga being a powerful integrative health practice for alleviating daily anxiety and stress. Yoga is an umbrella term for various physical, mental, and spiritual practices originating in ancient India. Hath Yoga is the most popular form of Yoga in western society. Yin Yoga, a derivative of Hath Yoga, is a much calmer meditative practice that uses seated and supine postures, held three to five minutes while maintaining deep breathing. Its focus on calmness and mindfulness makes Yin Yoga a tool for relaxation and stress coping, thereby improving psychological health (4).
Yin Yoga is also a wonderful complimentary practice that can be combined with Acupressure. Yin Yoga engages the physical, emotional, and energy body. Yin postures supportively align the body to stress connective tissues along specific meridian lines that activate potent acupressure points along those meridians. The Acupressure for Optimal Pelvic Health remote course explores Yin postures within key meridians and integrates acupressure and Yin Yoga with modifications into rehabilitation interventions. Anxiety and daily wellness self-care program is also a key part of the course.
As pelvic health therapists and medical providers, we can empower our patients to recognize the mind-body-energy interconnections and how they affect multiple systems, giving them the tools and self-care regimens to live healthier anxiety and pain-free lives. Combining our orthopedic skills with mindfulness-based holistic interventions also complements our best evidence-based practices.
The course Acupressure for Optimal Pelvic Health is an evidence-based journey of holistic healing and empowerment curated and taught by Rachna Mehta. To learn how to integrate acupressure and Yin Yoga into your practice, join the next scheduled remote course on October 23-24, 2021.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.2.
- Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec. 2002;269(6):257-265. doi:10.1002/ar.10185
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521. doi:10.1089/acm.2018.0422
- Daukantaitė D, Tellhed U, Maddux RE, Svensson T, Melander O. Five-week Yin Yoga-based interventions decreased plasma adrenomedullin and increased psychological health in stressed adults: A randomized controlled trial. PLoS One. 2018;13(7)
- Hmwe NTT, Browne G, Mollart L, Allanson V, Chan SW. An Integrative review of Acupressure interventions for older people: A focus on sleep quality, depression, anxiety, and agitation. Int J Geriatr Psychiatry. 2019;34(3):381-396. doi:10.1002/gps.5031
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of Acupressure on Anxiety: A Systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
In a previous post on The Pelvic Rehab Report, Sagira Vora, PT, MPT, WCS, PRPC explored the impact that pelvic floor exercises can have on arousal and orgasm in women. Today we hear part two of the conversation, and learn what factors can impact a woman's ability to achieve orgasm.
 “An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
“An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
Wow, that sounds like paradise! The question is--how to get there? Many of our cohorts and many our female patients have not experienced this or orgasm happens for them rarely. Findings from surveys and clinical reports suggest that orgasm problems are the second most frequently reported sexual problems in women. Some of the reasons cited for lack of orgasm are orgasm importance, sexual desire, sexual self-esteem, and openness of sexual communication with partner by Kontula el. al. in 2016. Rowland found that most commonly-endorsed reasons were stress/anxiety, insufficient arousal, and lack of time during sex, body image, pain, inadequate lubrication.
One factor that comes up consistently, is the ability of women to focus on sexual stimuli. This point has been brought up by various studies and presented in different ways. Chambless talks about mindfulness training and improvements in orgasm ability noted equally in women who practiced mindfulness vs. women who engaged in Kegels and mindfulness. Rosenbaum and Padua note in their book, The Overactive Pelvic Floor, “women who do not have a low-tone pelvic floor and who seek to enhance sexual arousal and more frequent orgasms have not much to gain from pelvic floor muscle training. Actually, a relaxed pelvic floor and mindful attention to sexual stimuli and bodily sensations seem a more effective means of enhancing sexual arousal and orgasm.” Various studies specifically studying the effect of mindfulness training have demonstrated both improved arousal and orgasm ability in women who practiced mindfulness. Brotto and Basson found their treatment group, which consisted of 68 otherwise healthy women, who underwent mindful meditation, cognitive behavioral training and education, improved in sexual desire, sexual arousal, lubrication, sexual satisfaction, and overall sexual functioning.
Cognitive-behavioral therapy appears to play a significant role in improving sexual function in women. Meston et. al. notes, “cognitive behavioral therapy for anorgasmia focuses on promoting changes in attitudes and sexually relevant thoughts, decreasing anxiety, and increasing orgasmic ability and satisfaction. To date there are no pharmacological agents proven to be beneficial beyond placebo in enhancing orgasmic function in women.”
Alas, there are no magic pills to create the above described “state of altered consciousness,” allowing women a sense of “well-being and contentment.” However, mindfulness training and cognitive behavioral therapy are both accessible and attainable for women who want to improve their ability to enjoy this much desired state. Many Pelvic floor therapist incorporate cognitive behavioral and mindfulness approaches in their practice.
The studies above mention pain as one of the factors for inability to experience arousal and orgasm. Hucker and Mccabe even noted that their mindfulness treatment group demonstrated significant improvements in all domains of female sexual response except for sexual pain. Dealing with sexual pain is a daily battle pelvic floor therapist face each day. So, how do women with sexual pain dysfunction differ from women who are experiencing sexual dysfunction but not pain? Let’s explore this in our next blog…
Chambless DL, Sultan FE, Stern TE, O’Neill C, Garrison S. Jackson A. Effect of pubococcygeal exercise on coital orgasm in women. J Consult CLin Psychol. 1984; 52:114-8
Bratto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women Behav Res Ther. 2014 Jun; 57:43-5
Hucker A. Mccabe MP. Incorporating Mindfulness and Chat Groups Into an Online Cognitive Behavioral Therapy for Mixed Female Sexual Problems. J Sex Res. 2015;52(6):627-33
Kontula O., Mettienen A. Determinants of female sexual orgasms. Socioaffect Neurosci Psychol. 2016 Oct 25;6:31624. doi: 10.3402/snp.v6.31624. eCollection 2016
Meston CM1, Levin RJ, Sipski ML, Hull EM, Heiman JR. Women’s orgasm. Annu Rev Sex Res. 2004;15:173-257. Review
Rosenbaum, Talli Y., Padoa, Anna. The overactive Pelvic floor. 1st ed. 2016
Roland DL, Cempel LM, Tempel AR. Women’s attributions on why they have difficulty reaching orgasm. J. Marital Therapy. 2018 Jan 3:0
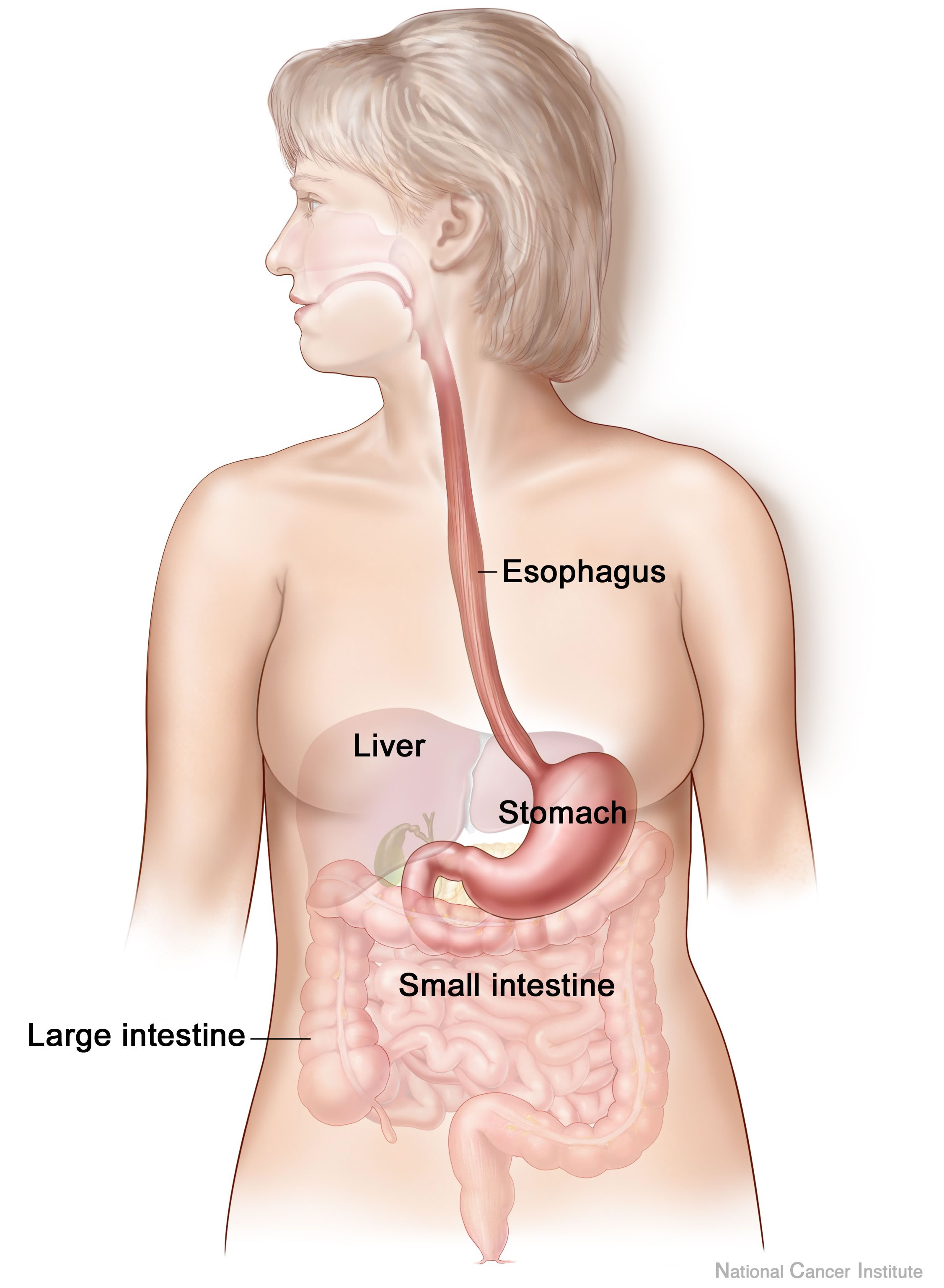
Anxiety and depression are frequently encountered co-morbidities in the clients we serve in pelvic rehabilitation. This observation several years ago in clinical practice is one of many that prompted me down the path of exploring the connection between the gut, the brain, and overall health. In answering the question about these connections, I discovered many nutritionally related truths that are being rapidly elucidated in the literature.
A recent study by Sandhu, et.al. (2017) examines the role of the gut microbiota on the health of the brain and it’s influence on anxiety and depression. The title of the study, “Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry” gives us pause to consider the impact of our diets on this axis and in turn, on the health of our nervous system. The authors state:
It is diet composition and nutritional status that has been repeatedly been shown to be one of the most critical modifiable factors regulating the gut microbiota at different time points across the lifespan and under various health conditions.
With diet and nutritional status being the most critical modifiable factors in the health of this system, it becomes our responsibility to seek to understand this system and its influencing factors. We need to learn how to nourish the microbiota-gut-brain axis.
While anxiety and depression are common co-morbidities we encounter, we also commonly detect imbalance between the sympathetic and parasympathetic nervous system in our patients leading to, for example, pelvic floor muscle tension. In light of this study we must first and foremost ask: what is the microbiota? How can it influence our nervous system? How does this correlate to anxiety and depression? The answers to these questions provide clinical insight with far-reaching impact. We also consider: which circumstances disrupt the health of this system and which improve it? Finally, could understanding of this axis, among other nutritional correlates, provide a novel approach to bowel dysfunction, bladder dysfunction, chronic pelvic pain?
Be a part of the paradigm shift to integrative understanding as we explore these and many other burning questions. Please join us for insightful discussion in White Plains, NY March 31-April 1, 2017 for our next offering of Nutrition Perspectives for the Pelvic Rehab Therapist.
Sandhu, K. V., Sherwin, E., Schellekens, H., Stanton, C., Dinan, T. G., & Cryan, J. F. (2017). Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res, 179, 223-244. doi:10.1016/j.trsl.2016.10.002