Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 has a personal interest in various eastern holistic healing traditions, and she noticed that many of her chronic pain patients were using complementary health care approaches including acupuncture and yoga. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
There is worldwide concern over the increasing rates of pharmacologically induced labor, opioid use, and operative birth. Women are seeking holistic non-pharmacologic options to avoid medical and surgical interventions in childbirth which has led to the popularity of Complementary and Alternative Medicine (CAM) therapies. Despite CAM existing outside of conventional heath systems, a substantial number of women have been found to use CAM to manage their health during pregnancy1.
Among CAM therapies, Acupuncture and Acupressure have been found to be helpful for pregnancy-related symptoms such as nausea, breech presentation, and labor induction with post-partum recovery considerations as well. Acupressure has roots in Acupuncture and is based on more than 3000 years of Traditional Chinese Medicine (TCM). TCM supports Meridian theory and meridians are believed to be energy channels that are connected to the function of the visceral organs. Acupoints located along these meridians transmit Qi or the bio-electric energy through a vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera.
A systematic review published by Smith et al2 looked at the use of Acupuncture or Acupressure for pain management during labor. They noted that the pain women experience during labor can be intense, with body tension, anxiety, and fear making it worse. The data included a total of 3960 women and found that Acupressure may reduce pain intensity in women experiencing labor pain.
Another RCT published by Levett et al included 176 nulliparous women with low-risk pregnancies, attending hospital-based antenatal clinics. They incorporated six evidence-based complementary medicine techniques: Acupressure, visualization and relaxation, breathing, massage, yoga techniques, and facilitated partner support. Randomization occurred at 24–36 weeks’ gestation, and participants attended a 2-day antenatal education program plus standard care, or standard care alone.
The study found a significant difference between the two groups with the study group having decreased epidural use (23.9%) compared to the standard care group (68.7%). The study group participants also reported a reduced rate of cesarean section and length of the second stage among other measures.
An article published by Debra Betts3 discusses several key considerations for promoting physiological Labor with Acupuncture. Multiple studies have cited the effectiveness of Acupressure by stimulating these powerful Acupoints as well. The author states that the suggestion of Acupoints cited below are based on both her clinical practice and midwifery feedback and are by no means an exhaustive list. The practitioner is encouraged to explore Traditional Chinese Medicine to promote efficient physiological labor in women.
Key considerations for promoting natural physiological labor include:
Is the baby in an optimal anterior position? The author states “Women can become involved in their own treatment by learning proactive positioning. This involves a woman keeping her knees lower than her hips when sitting, in order to assist gravity in moving her baby into the best possible position. Bucket‑type seats such as car seats and comfy sofas, therefore, need to be abandoned in favor of birthing balls, sitting astride chairs (with the arms resting on the back).” Key acupuncture points that can be stimulated include Bladder 60 ( BL 60), Spleen 6 (Sp 6), and Bladder 67 (BL 67). Bladder 60 (BL 60) is considered an empirical induction point. Midwifery feedback suggests that this is a useful point for promoting an optimal position of the baby for birth. Bladder 67 (BL 67) is considered an extremely important point if the baby is not in an anterior position.
Is the woman emotionally prepared for labor? While most women have some level of underlying anxiety or fear about the approaching birth, it is essential to address any significant emotional disharmony. The hormone oxytocin is released several weeks prior to labor, initially stimulating uterine contractions at night, with increasing production then aiding the transition into labor. Stress hormones such as adrenaline and noradrenaline have a direct inhibiting effect on natural oxytocin release, and therefore play a very significant role in inhibiting contractions2. Key acupuncture points that can be stimulated include Kidney 1 (KD 1), Liver 3 (Liv 3), and Pericardium 6 (P6) among others. Kidney 1 (K1) is useful for women who are experiencing fear of induction or childbirth itself. Liver 3 (Lv 3) is helps in improving Liver chi. Pericardium 6 (P6) is helpful for nausea, regulating the heart and calming.
Is the woman physically prepared for labor? Women may be physically exhausted or have pre-existing physical conditions that, once addressed, will help to promote physiological labor2. Key acupuncture points that can be stimulated include Bladder 43 (BL 43) and Stomach 36 (St 36). Bladder 43 ( BL 43) is A point that tonifies and nourishes the Lung, Heart, Kidneys, Spleen, and Stomach. Stomach 36 (ST 36) is a useful point to reinforce if the woman is exhausted, due to its qi-tonifying and blood-nourishing properties.
Stimulating contractions: Debra Betts also notes that key points of the Bladder meridian that are located on the sacrum are crucial in initiating contractions. While Traditional Chinese Medicine (TCM) does consider some Acupuncture points like Large Intestine 4 (LI 4), Gall Bladder 21 (GB 21), and Spleen 6 (Sp 6) should not be stimulated in pregnant women, the opposite is true when we want to initiate labor and these points can be additionally used to assist in stimulating contractions.
Acupressure can also be used in the post-partum period for overall generalized well-being, promoting a sense of bonding with the baby, calm, and relaxation.
Acupressure can be used to stimulate key energy points also known as Acupoints in various meridians and as hands-on musculoskeletal specialists, we can use and teach this modality to our patients. Acupressure requires no equipment, is easy for clinicians to teach and for patients to self-administer when taught correctly, and is an empowering self-care tool to promote optimal health outcomes.
The course Acupressure for Optimal Pelvic Health focuses on powerful Acupressure points in key Meridians including the Kidney, Bladder, Spleen, and Stomach meridians. It also explores Yin Yoga as an integrative intervention with Acupressure. Yin Yoga, a derivative of Hath Yoga is a wonderful complimentary practice to Acupressure. Yin Yoga is a slow and calm meditative practice that uses seated and supine poses that are held for three to five minutes with deep breathing. It stimulates the energy flow through the meridian channels by creating tension along specific meridian lines.
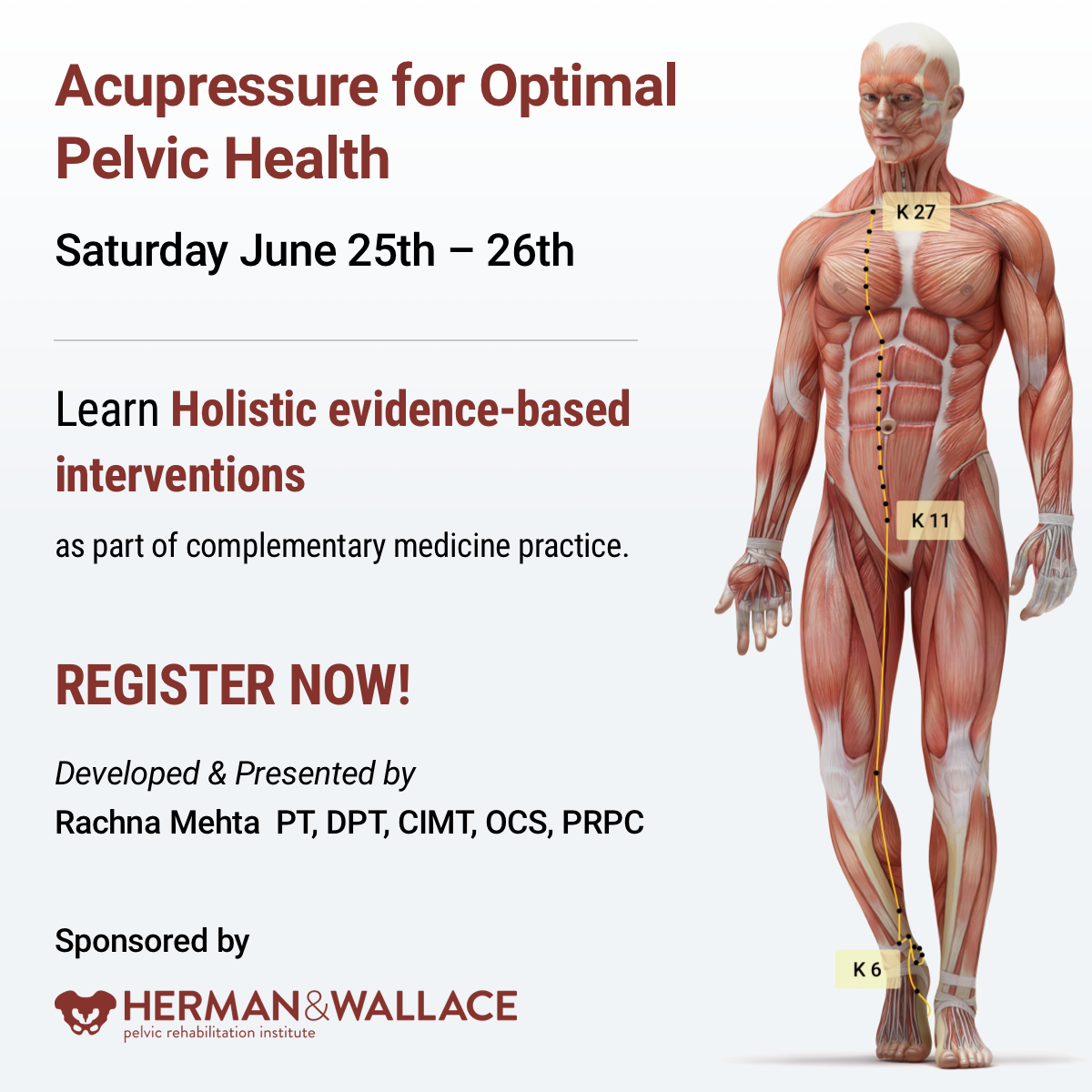
This course is curated and taught by Rachna Mehta. To learn how to integrate Acupressure into your clinical practice, join the next scheduled remote course on June 25- 26, 2022.
References
- Steel A, Adams J, Sibbritt D, Broom A. The Outcomes of Complementary and Alternative Medicine Use among Pregnant and Birthing Women: Current Trends and Future Directions. Women’s Health. May 2015:309-323. doi:10.2217/WHE.14.84.
- Smith CA, Collins CT, Levett KM, et al. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020;2(2): CD009232.
- Betts, Debra. Inducing Labour with Acupuncture–Crucial Considerations. Journal of Chinese Medicine. 2009;90: 20-25.
- Atkins KL, Fogarty S, Feigel ML. Acupressure and Acupuncture Use in the Peripartum Period. Clin Obstet Gynecol. 2021;64(3):558-571. doi:10.1097/GRF.0000000000000636.
- Levett, Kate M., Smith, C.A., Bensoussan, A. & Dahlen, H.G. Complementary therapies for labour and birth study: a randomized controlled trial of antenatal integrative medicine for pain management in labour. BMJ Open, 2016 Jul 12;6(7):e010691. DOI: 10.1136/bmjopen-2015-010691.
- Schlaeger JM, Gabzdyl EM, Bussell JL, et al. Acupuncture and Acupressure in Labor. J Midwifery Women's Health. 2017;62(1):12-28. doi:10.1111/jmwh.12545.
Acupressure for Optimal Pelvic Health
Instructor: Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
Price: $450
Experience Level: Beginner
Contact Hours: 12.5
Course Dates: June 25-26, 2022 and October 15-16, 2022
Course Description:
This continuing education course is a two-day seminar that offers participants an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, and stress and bringing the body back to a state of physiological balance are integrated throughout the course.
Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channel energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
Special Considerations and Lab materials
The labs for this course will involve external whole-body palpation and mapping of acupressure points. Please wear fitted t-shirt and leggings or yoga pants for acupressure point mapping. Participants should buy a pack of 1-inch diameter white circle stickers to be used in Labs for mapping acupressure points.
Participants are encouraged to use a Yoga mat if available and any other props they may have at home including yoga blocks, small blankets, towels and pillows to be used in the guided Yin Yoga Lab portion of the course.
Recommended resources: It is recommended that participants purchase an Acupressure Point Chart for ease of following the course work and labs in this course. Since the accuracy of points and content may vary on different charts, it is recommended to buy a copy at https://acupressure.com/products/acupressure-charts/
Target Audience:
This continuing education seminar is targeted to rehabilitation professionals who use manual therapy as a treatment modality. Knowledge of acupressure points with specific anatomical landmarks will enable clinicians to add to their toolbox skills for treating a variety of pelvic health conditions related to the bowel, and bladder and treatment of pelvic pain.
Prerequisites:
It is recommended that the participants have a working knowledge of the functional anatomy of pelvic floor muscles as well as various associated pelvic health conditions. Pelvic Floor 1 through Herman & Wallace is strongly recommended.
While my dad was visiting Michigan, we had the day to ourselves as my kids were in school. I was so excited to have quality time with my dad. Unfortunately it was pouring down rain. We decided on a leisurely brunch and then a movie. Dad chose the movie, “Wind River.” While not a movie I would normally pick, I was happy to go along. A little more than half way through…there was a horribly violent scene against a young women. I panicked, plugged my ears and closed my eyes. Unfortunately some images were burned into the back of my mind. When the movie was over, I remained seated and tears just came. My dad held me while I cried. I was able to calm down and leave the theater, but the images continued to bother me. During the next few days, I made it a priority to care for myself and allow my nervous system to process and heal.
 What happened to me? I have never had any traumatic personal experience. Why did I react so strongly? I talked with my therapist about it and she suggested I might have experienced secondary traumatic stress. We know, as pelvic health therapists, we need extra time to hear the “stories” of new patients. We do our best to create a safe space for them so they can trust us and we can help them discover pathways to healing. Yet no one has taught us what we are supposed to do with the traumatic stories our patients share. How are we to cope with holding space for their pain? How do we put on a happy face as we exit the room to get the next patient?
What happened to me? I have never had any traumatic personal experience. Why did I react so strongly? I talked with my therapist about it and she suggested I might have experienced secondary traumatic stress. We know, as pelvic health therapists, we need extra time to hear the “stories” of new patients. We do our best to create a safe space for them so they can trust us and we can help them discover pathways to healing. Yet no one has taught us what we are supposed to do with the traumatic stories our patients share. How are we to cope with holding space for their pain? How do we put on a happy face as we exit the room to get the next patient?
Teaching Capstone over the last few years, Nari Clemons and I have talked with many of you who were feeling emotionally overloaded especially when treating chronic pelvic pain and trauma survivors. Some of you were experiencing job burnout, others were deciding maybe it was time for a career shift, away from the pelvis. We realized something needed to be done as our field was losing talented pelvic health therapists. We have also struggled ourselves with various aspects of our profession.
There are no studies that directly look at job burn out, secondary traumatic stress, and compassion fatigue among pelvic health physical therapists. Yet these problems are common among social workers, physicians and other people groups in health care. There are individual as well as institutional risk factors that lead to the development of each. The solution, as one self-help module puts it, is developing resilience. A large part of this skill is making self-care a priority. The basics such as adequate sleep, nutrition, and exercise are foundational. Meditation, mindfulness, therapy, and spiritual practices, as well as supportive friends/groups are also imperative.
Nari and I realized that training to develop resilience in therapists was missing. Initially we equipped ourselves to have better boundaries, ground ourselves with meditation, mindfulness and exercise, which enhanced our skills in dealing with complex, chronic patients. We compiled what we have learned and want to share it with you. We would like to invite you to attend Holistic Interventions and Meditation: Boundaries, Self-Care, and Dialogue. We have designed this 3 day course to be partially educational and absolutely experiential. We are going to dig deeper into ways to calm our patient’s and our own nervous systems, explore and practice the latest recommendations on treatment of persistent pain, we will mediate and learn about mediation, play with essential oils, learn some new hands on techniques, and support and encourage one another as we build communication skills. We want you to leave feeling refreshed and equipped to continue to treat patients without losing yourself in the process. We want to invest in you so you can continue the investment you have made in your career and avoid job burnout, compassion fatigue and secondary trauma. We invite you to develop the resilience you need for a rewarding career in pelvic health physical therapy by joining us in Tampa this January.
Cieslak, R., Shoji, K., Douglas, A., Melville, E., Luszczynska, A., & Benight, C. C. (2014). A meta-analysis of the relationship between job burnout and secondary traumatic stress among workers with indirect exposure to trauma. Psychological services, 11(1), 75.
Meadors, P., Lamson, A., Swanson, M., White, M., & Sira, N. (2010). Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress. OMEGA-Journal of Death and Dying, 60(2), 103-128.
Sodeke-Gregson, E. A., Holttum, S., & Billings, J. (2013). Compassion satisfaction, burnout, and secondary traumatic stress in UK therapists who work with adult trauma clients. European journal of psychotraumatology, 4(1), 21869.
Stearns, S., & Benight, C. C. (2016). Organizational Factors in Burnout and Secondary Traumatic Stress. In Secondary Trauma and Burnout in Military Behavioral Health Providers (pp. 85-113). Palgrave Macmillan US.
Today we pick up on Jennafer Vande Vegte's interview with her patient, "Ben", about his experience overcoming chronic pelvic pain syndrome. Ben's quality of life improved so much that he has returned to school in order to become a PTA, with a focus on pelvic rehabilitation!
Describe your physical therapy experience. Talk about your recovery process. Include the physical, mental and emotional components.
 For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
Over the course of many months of PT though we couldn’t pinpoint what started the pain, we knew my nervous system was keeping it going. Sensory signals had somehow been rerouted through pain centers in the delicate and complicated highway interstate of the nervous system. It was as if the Fed Ex truck that was supposed to carry a package from Miami to Denver got rerouted to New York, stuck in traffic in Manhattan, flipped off by cab drivers, beaten up by gang members, contents of the truck shaken up by the driver trying to flee the city, and then finally finding the way out of New York to the true destination of Denver – with damaged goods, and shaking with anxiety. As to who the idiot dispatcher was who re-routed the truck to New York, well, he’s really good at keeping himself secret and innocent-looking. Jerk!
Physical therapy, over time, began to work for me. It released trigger points which are the first step in the long process of recovery. As we know, chronic tension must be addressed in tissues and nerves, and the mind must relearn how to remain in neutral. I found that as I gained periods of relief I could see that there truly was a mind-body connection beyond what I could imagine. My physical therapist and I both knew that nerves are the slowest recovering tissue in the body, and when you combine that with an anxious mind, you have a complicated puzzle to solve. There is definitely a closed circuit that develops with chronic pelvic pain. Pain causes anxiety, anxiety causes pain and circularly they feed one another.
During my physical therapy I joined a male pelvic pain message board online. I began understanding that most men who develop pelvic pain also have experienced traumatic emotional stress. And a large part of chronic pelvic pain is rooted in a mind-body dysfunction. I had to learn how to stop thinking catastrophically, especially during flare ups. I had to trust that my body would heal and think positively. I had to learn how to relax, take care of myself, eat well, stretch and exercise daily.
When I started physical therapy, I hoped to escape the pain. My first 5 month phase of physical therapy helped to loosen the chronically tightened pelvic sphincter muscles. However, I still had allodynia. In my second phase of physical therapy I began experiencing reduction of pain for a longer duration of time. After about a year of therapy, I finally got to a point where I could see there was significant improvement, even though some intermittent pain and anxious symptoms stubbornly persisted. In late spring of 2017, I finally felt like I had conquered the pain by 98%. Occasionally flares would still come, but they were brief and nothing like before physical therapy.
How has your experience with chronic pelvic pain changed you?
CPPS has profoundly changed me. I don’t take the little things for granted or sweat them anymore. I am grateful for not feeling that horrible, hellish sensation any longer. I appreciate having my mind pain and panic free. I speak my mind while respecting my own desires instead of belittling them. I am currently in school to become a Physical Therapy Assistant as through this process I learned that I’m actually much smarter than my middle school guidance counselor thought. I understand the mind is incredibly powerful, and fear rarely has the same power over me.
How do you handle flare ups?
I now handle brief flare ups with deep breaths, meditation, and/or just taking a step back and trying to zero in on what is really bothering me. At least now I can clearly think without debilitating pain and am able to function.
What would you like to say to other people who are struggling with chronic pelvic pain?
Oh, man. For the initial duration, I would say find a safe place where you can feel as comfortable as possible until the pain lessens. When it is bad, you sort of have to give in to it. However, part of this recovery is the physical mechanics of muscle and fascia. Physical Therapy is essential in the process of recovery to release this tension. I would tell them not to give up hope. You will not find many health professionals or websites that will tell you that you can beat this and recover 100%. But I will tell you, you can recover, 100%. You can. But for now, your full-time job is to work on recovery, and that includes lots of self-care, facing possible emotional pain, and physical therapy.
If you would like to learn more about addressing the mind body connection with patients please join us for Holistic Intervention and Meditation: Boundaries, Self-Care and Dialog in January. We will be exploring ways to help our patients heal to their fullest potential as well as keeping ourselves emotionally healthy in the process. Treating patients with persistent pain can be challenging for the best of us. Please come for this three-day course where you will leave feeling refreshed, renewed and reinvigorated to treat even your most complex patient.
Additional resources:
https://www.tamethebeast.org/#home
https://www.youtube.com/watch?v=jIsF8CXouk8
http://www.sciencedirect.com/science/article/pii/S1356689X11000737
http://www.noigroup.com/en/Home
https://bodyinmind.org/who-are-we/