Male Pelvic Pain: What Therapists Can Do to Help End the Desperation
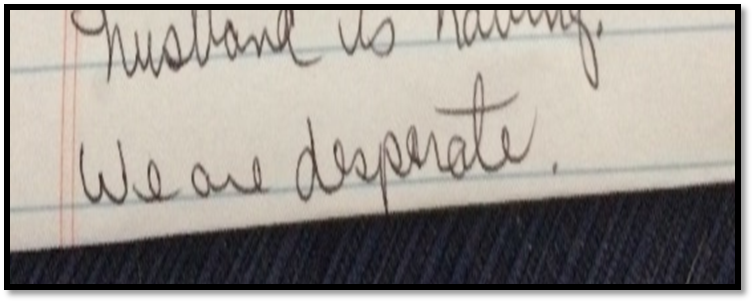
Recently, a note was left at my doorstep by the wife of an older gentleman who had chronic male pelvic pain. His pain was so severe, he could not sit, and he lay in the back seat of their idling car as his wife, having exhausted all other medical channels available to her, walked this note up to the home of a rumored pelvic floor physical therapist who also treated men. The note opened with how she had heard of me. She then asked me to contact her about her husband’s medical problem. It ended with three words that have vexed me ever since…we are desperate.
Unlike so many men with chronic pelvic pain, he had at least been given a diagnostic cause of his pain, pelvic floor muscle dysfunction, rather than vaguely being told it was just a prostate issue. However, the therapists that had been recommended by his doctor only treated female pelvic dysfunction.
“We are desperate”: A Call to Action for All Therapists to become Pelvic Floor Inclusive
My first thought after reading the note was, “I bet shoulder or knee therapists don’t get notes like this on their doorstep.” My next thought, complete with facepalm, “THIS HAS TO STOP! Pelvic floor rehab has got to become more accessible”.
Pelvic floor therapists see men and women and even transgenders. They treat in the pediatric, adult, and geriatric population. They treat pelvic floor disorders in the outpatient, home health and SNF settings. They treat elite athletes and those with multiple co-morbidities using walkers. They can develop preventative pelvic wellness programs and teach caregivers how to better manage their loved one’s incontinence. This is due to one simple fact: No matter the age, gender, level of health or practice setting, every patient has a pelvic floor.
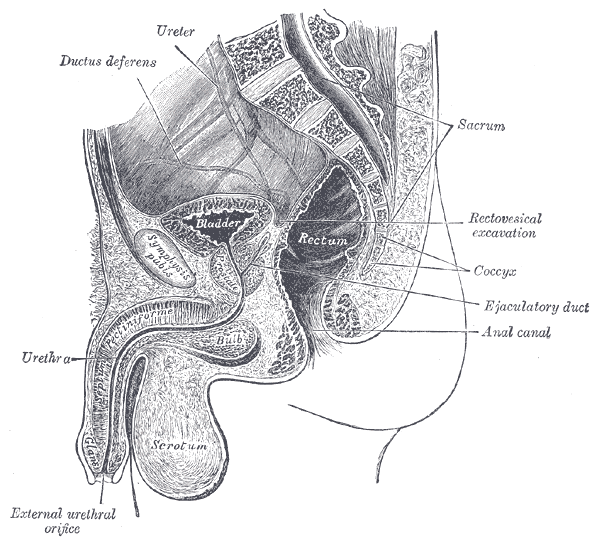
The pelvic floor should not be regarded as some rare zebra in clinical practice when it is the workhorse upon which so many health conditions ride. It interacts with the spine, the hip, the diaphragm, and vital organs. It is composed of skin, nerves, muscles, tendons, bones, ligaments, lymph glands, and vessels. It is as complex and as vital to function and health as the shoulder or knee is, and yet students are lucky if they get a “pelvic floor day” in their PT or OT school coursework.
I call for every therapist, specialist, and educator to learn more about the pelvic floor. Here are some steps you can take today toward eliminating the need for such a note to be written.
If you are a pelvic floor therapist who treats men, shout it from the rooftops!
Contact every PT clinic, every SNF, every doctor, every nurse, every chiropractor, every acupuncturist, every massage therapist, every personal trainer, every community group and let them know! If you have already told them, tell them again. Send a one page case study with your business card. Host a free community health lecture at the library or VFW hall. Keep the conversation going. Reach out to your local rehab or nursing school programs and volunteer to speak to the students. Feature pelvic health topics in your clinic’s social media stream. Get on every single therapist locator that you can so people can find you. Click here to go to the Herman and Wallace Find a Practitioner site.
If you only treat pelvic dysfunction in women, please consider expanding your specialty to include men.
The guys really need your help. You literally may be the only practitioner around that has the skills to treat these types of problems. Yes, the concerns you have about privacy and feeling comfortable are valid. But, you are not alone in this. Smart people like Holly Tanner have figured all that stuff out for you and can guide you on how to expertly treat in the men’s health arena. Sign up for Male Pelvic Floor or take an introductory course online at Medbridge. If you have only taken PF1, it’s time to sign up for Pelvic Floor Level 2A: Function, Dysfunction and Treatment: Colorectal and Coccyx Conditions, Male Pelvic Floor, Pudendal Nerve Dysfunction. Reach out to other pelvic floor therapists that treat men and ask for mentorship.
If you are general population therapist, consider taking a pelvic floor course.
Good news! Not every pelvic floor course requires you to glove up and donate your pelvis to science, so to speak. Yes, there are several external only courses you can take that do not have an internal examination lab. Click here and look under “course format” to see a list of external only courses. If you treat in the outpatient, ortho, or sports medicine arena, consider taking Biomechanical Assessment of the Hip & Pelvis: Manual Movement Therapy and the Myofascial Sling System or the Athlete and the Pelvic Floor .
If you treat in the Medicare age population, work in skilled nursing, or home health, join me in New York on May 21-22 for Geriatric Pelvic Floor. It is an external course and we cover documentation and self-care strategies extensively for incontinence and pelvic pain in older adults across multiple settings. Older adults with pelvic pain, like the man in the back seat, are at risk for being diagnostically ignored. We will address biases, such as “prostato-centric” thinking, ageism, and the ever-present “no fracture no problem” prognosis given to seniors who sustain a fall, but are left with disabling soft tissue dysfunction.
If you are a PT or OT school educator, eliminate “Pelvic Floor Day”.
Sorry, but it sounds silly. It’s like saying you offer a “Knee Day” in your program. Replace it by including the pelvic floor into Every. Single. Class…anatomy, ther ex, neuro, peds, geriatrics, and even cardiopulmonary!
As the baby boomer population grows, pelvic floor disorders are expected to rise significantly (download a free white paper on pelvic floor trends here). Are you preparing your doctorate students to be competent screeners of pelvic floor dysfunction? Pelvic floor rehab is becoming the gold standard of first line treatments for pelvic dysfunction. Are you giving your students the skills to be competitive in a job market that recognizes pelvic floor rehabilitation as standard of care? Bias is learned. Excluding the pelvic floor in your student’s coursework or presenting it as a niche specialty subtly reinforces this bias.
Reach out and ask your local pelvic floor therapists to guest lecturer throughout the program. Send your instructors to pelvic floor courses. Encourage your students to take Pelvic Floor Level 1 in their last 6 months of coursework. Offer a clinical rotation in pelvic floor rehabilitation. Include case studies and patient perspectives on pelvic dysfunction, such as A Patient’s Pelvic Rehab Journey.
The Silver Lining
Thanks to the champions of pelvic floor rehab education, we’ve come a long way. The good news in this story is that this man’s doctor recognized early that he had pelvic floor muscle dysfunction and recommended that he see a pelvic floor physical therapist. The bad news-it took 2 years before he could find one. The ball is in our court, therapists. Let’s do better. Until there are no more men in the back seat, we still need to #LearnMoreAboutThePelvicFloor.
In the world of pelvic health, we are constantly meeting patients who are surprised to learn about the scope of what we do. Oftentimes, it is because we mention the pelvic muscles’ roles in sexual health that a patient will offer up symptoms with their sexual health, or ask a few more questions. Outside of pelvic health professionals asking about sexual function, do men bring up these issues with anyone? Not usually. In Fisher and colleagues 2-part “Strike up a conversation” study (2005), the authors reported that men who have erectile dysfunction (ED) are worried about their partner’s reaction, don’t want to admit to having a chronic problem, and frankly, just don’t even know where to start. Unfortunately, the partners of men who have ED have the same concerns. In addition, partners are worried about bringing it up and “making their partners feel worse about it.” When men did bring up sexual concerns with their physician, although they reported feeling nervous and embarrassed, they also reported feeling hopeful and relieved.
 This issue was highlighted in a recent interview and article published on National Public Radio. The article shares that for war veterans, sexual intimacy is often affected, and yet, is often ignored. A Marine who suffered PTSD after a head injury and shrapnel to the head and neck describes how he had to go to the doctor several times just to work up the nerve to ask for help for his sexual dysfunction. He also shared how it was difficult to talk about “…because it contradicts a self-image so many Marines have.” Apparently you don’t have to be a Marine to feel the same intense pressure related to talking about sexual issues. I have spent more time in the past year trying to better understand why men don’t discuss these issues, with a best friend or partner, and each time, my question of “what would that be like if you brought it up?” is met with near bewilderment, as if revealing this issue were akin to revealing your deepest, darkest secret. Apparently, it is. Telling a buddy you have erectile dysfunction, for men, seems to be like showing your enemy where the chink in your armor is, or like setting yourself up to be the center of every “getting it up” joke for the remainder of your life.
This issue was highlighted in a recent interview and article published on National Public Radio. The article shares that for war veterans, sexual intimacy is often affected, and yet, is often ignored. A Marine who suffered PTSD after a head injury and shrapnel to the head and neck describes how he had to go to the doctor several times just to work up the nerve to ask for help for his sexual dysfunction. He also shared how it was difficult to talk about “…because it contradicts a self-image so many Marines have.” Apparently you don’t have to be a Marine to feel the same intense pressure related to talking about sexual issues. I have spent more time in the past year trying to better understand why men don’t discuss these issues, with a best friend or partner, and each time, my question of “what would that be like if you brought it up?” is met with near bewilderment, as if revealing this issue were akin to revealing your deepest, darkest secret. Apparently, it is. Telling a buddy you have erectile dysfunction, for men, seems to be like showing your enemy where the chink in your armor is, or like setting yourself up to be the center of every “getting it up” joke for the remainder of your life.
The bottom line is that we can be part of the solution to this problem, because men must be certain that their medical provider knows about any emerging or worsening erectile dysfunction. Loss of libido, or changes in erectile function can be associated with heart issues, with diabetes, or with other major medical concerns. Research such as the referenced “strike up a conversation study” has demonstrated that health care providers or partners may positively influence a patient’s access to care. Once medical evaluation has been completed, the role of the pelvic health provider is critical in improving sexual health for men with dysfunction. If you are interested in learning more about the role of the pelvic health provider for erectile dysfunction or pain related to sexual function, the Male Pelvic Health continuing education course will be offered 3 times this year through the Herman & Wallace Pelvic Rehabilitation Institute. Your next opportunity to learn about urinary and prostate conditions, male pelvic pain, sexual health and dysfunction is next month in Portland, Oregon.
Chang, A. (2016). For veterans, trauma of war can persist in struggles with sexual intimacy. Retrieved from http://www.npr.org/sections/health-shots/2017/01/01/507749611/for-veterans-trauma-of-war-can-persist-in-struggles-with-sexual-intimacy
Fisher, W. A., Meryn, S., Sand, M., Brandenburg, U., Buvat, J., Mendive, J., ... & Strike Up a Conversation Study Team. (2005). Communication about erectile dysfunction among men with ED, partners of men with ED, and physicians: The Strike Up a Conversation Study (Part I). The journal of men's health & gender, 2(1), 64-78.
Fisher, W. A., Meryn, S., Sand, M., & Strike up a Conversation Study Team. (2005). Communication about erectile dysfunction among men with ED, partners of men with ED, and physicians: the Strike Up a Conversation study (Part II). The journal of men's health & gender, 2(3), 309-e1.
“Please stress the need to examine men…For some reason, most female PT`s shy away from a male’s private parts totally. It would be great if females were taught that it's important to go there…And treat us as equals in this arena.”
 This is an excerpt from a recent email we received at Herman & Wallace headquarters, and it highlights a common theme, that of patient access to care. While there are many factors driving patient access to pelvic health, availability of therapists trained in various conditions is certainly one major issue. By the time any patient is referred to pelvic rehabilitation, they have already overcome the challenge of many providers not being aware that there is help for pelvic health issues, and insurance or payment hurdles that can also cause a patient to delay or avoid recommended treatment. Many physical therapy programs have done an outstanding job in developing and marketing women’s health programs, with men’s health programs addressing post-prostatectomy care or male pelvic pain coming along almost as an afterthought.
This is an excerpt from a recent email we received at Herman & Wallace headquarters, and it highlights a common theme, that of patient access to care. While there are many factors driving patient access to pelvic health, availability of therapists trained in various conditions is certainly one major issue. By the time any patient is referred to pelvic rehabilitation, they have already overcome the challenge of many providers not being aware that there is help for pelvic health issues, and insurance or payment hurdles that can also cause a patient to delay or avoid recommended treatment. Many physical therapy programs have done an outstanding job in developing and marketing women’s health programs, with men’s health programs addressing post-prostatectomy care or male pelvic pain coming along almost as an afterthought.
So what is really limiting the care of men who wish to overcome urinary, pain, or sexual dysfunction? For many locations around the country, there simply is not enough awareness of the scope of pelvic rehab, the nearest pelvic rehab provider may be far away geographically (or have a months-long waiting list), or the clinic may limit pelvic healthcare to women. If the clinic chooses to only provide care to women, what are we being discriminating about? The word “discriminate” has at least two rather distinct definitions, one that is more negative, and meaning that we are acting in an unjust or prejudicial manner, and another that simply means we are recognizing a difference between patient groups. If we choose to discriminate against treating men in a pelvic health setting, it’s easy to understand that if a therapist has never been instructed in how to examine a male patient, it may be prudent to avoid such evaluation until training is completed. We can find examples of this situation in other aspects of clinical care: if I have never taken proper training in evaluation of the vestibular system, for example (a condition that historically has not always been comprehensively instructed in school), then it’s in my best interest (and that of the patient) to only provide such care once I have taken appropriate training.
If our care of male pelvic health conditions is due to lack of specific training, what is our professional responsibility for acquiring training in conditions such as post-prostatectomy urinary incontinence, male genital pain, or erectile dysfunction? If we are to serve the pelvic health populations well, our training should progress to include lifespan issues for all ages and all genders. If we actively choose to avoid treating a population or condition, is that fair to the community seeking care? The ethics of choosing not to treat patients of a particular gender or condition are interesting to consider, but are not the scope of this post. On the other hand, the business side of being able to market to and welcome male patients in our clinics is very positive, and of course, all of our patients tend to be grateful for what we offer.
If you are interested in learning more about male pelvic healthcare, the Institute has several courses that can help you do so. These courses include an introduction to men at the Pelvic Floor Level 2A course, the Male Pelvic Floor: Function, Dysfunction and Treatment course (3 days dedicated to evaluation and treatment of urinary, sexual, and pain dysfunction), the Post-Prostatectomy course, as well as several manual therapy courses such as our myofascial courses. It is understandable that pelvic health for men may be less familiar territory for many of us based on our graduate training and experiences. If fear or discomfort is holding us back, at least attending a training course can help provide strategies and tools for gaining more comfort in treating men. We are at an exciting time in the pelvic health field when treating men is gaining more ground. If you are not already, join this exciting movement by signing up for one of the many classes available to you!
Peyronie’s disease is a condition in which there are fibrotic plaques (sometimes calcified) that can cause a curvature in the penis, most notable during erection. Pain as well as urinary and sexual dysfunction may occur with Peyronie's disease. Increased attention has been given in recent years to the relationship between male hormones, erectile dysfunction, and Peyronie's disease. According to the Mayo Clinic, testosterone, the predominant hormone affecting male physical characteristics, peaks during adolescence and early adulthood. Testosterone gradually decreases about 1% per year once a man reaches age 30-40. Some men experience symptoms from the decline in testosterone and these symptoms can include decreased sexual function, sleep disturbances changes in bone density and muscle bulk, as well as changes in cognition and depression. Because other factors and conditions can cause similar symptoms, patients with any of these changes should talk to their medical provider to rule out diabetes, thyroid dysfunction, depression, sleep apnea, and medication side effects, according to Mayo.
 In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
The larger question about Peyronie’s disease is what a patient can do to improve the symptoms of the condition. Therapists who treat male patients are increasingly interested in this question, and many are working with their patients to address the known soft tissue dysfunction. Interventions may include teaching patients to perform soft tissue mobilizations and stretches to the restricted tissue, and educating the patient in what the available literature tells us about rehabilitation of this condition. Hopefully, as male pelvic rehabilitation continues to grow in popularity, more therapists will contribute case studies and participate in higher levels of research so that more men can add conservative care of Peyronie’s to their list of treatment options.
To learn more about what the literature tells us about Peyronie’s and other male pelvic rehabilitation conditions, the Male Pelvic Floor continuing education course is taking place in Seattle in November, and you won't want to miss it!
Varicoceles are enlarged veins that occur in the scrotum. They can be common in adolescent boys and men, with an incidence rate of approximately 15%. Because up to 1/3 of men dealing with infertility have a varicocele, a repair of this venous herniation may be a first line treatment for male fertility. Varicoceles are sometimes referred to as feeling like a "bag of worms" due to the distended veins that coil through the area (the U.S. National Library of Medicine provides a useful illustration). Although varicoceles may be painless, they are thought to be symptomatic in up to 10% of men. Symptoms can be dull, aching, throbbing, and can worsen with physical activity. Conservative care includes scrotal support, limiting physical activity, and using anti-inflammatory medications.

Pelvic rehabilitation providers may work with a male patient who complains of scrotal pain, and who has a known diagnosis of a varicocele. If the patient is unsure of such a diagnosis, questioning the patient about prior discussions with his medical providers may reveal that he was told about “enlarged veins in the scrotum” or similar description. Visual inspection may reveal the tell-tale appearance of distended veins inside the scrotum, and palpation may reveal a significant difference among sides (unless both sides are involved of course.) Physical examination for a varicocele is usually completed in supine and standing positions and may be palpable with or without Valsalva maneuver. Keeping in mind that the differential diagnosis for pain in the scrotum can include medical conditions such as testicular torsion, epididymitis, inguinal hernia, testicular tumor, hydrocele, epididymal cyst, or sperm granuloma, patients who have complaints must see an appropriate medical provider to rule out such conditions. It is also possible for a patient’s condition to change or worsen if a period of time has passed, with communication with the referring provider recommended. Post-surgical complications that should also be considered are inguinal hernia repair for nerve entrapment or vasectomy.
Because of the nerves traveling in the same pathway as the involved veins, we can also consider the neural tension potentially created from the increased venous distension creating either (or both) compression and drag. Surgical options may be discussed by the medical provider, and these might include a microsurgical ligation or a varicolectomy. According to Park & Lee (2013) “A varicocelectomy should be considered in patients with no alleviation of their pain after conservative management, including resting, scrotal elevation, and nonsteroidal anti-inflammatory analgesics.” Conservative management is exactly where we can fit in as providers of pelvic rehabilitation. Including a condition such as a varicocele in our differential diagnosis and treating planning can further our success with patients.
Herman & Wallace offers it's popular Male Pelvic Floor Function, Dysfunction and Treatment course next month in Denver, CO. See you there!
References
Park, Y. W., & Lee, J. H. (2013). Preoperative predictors of varicocelectomy success in the treatment of testicular pain. The world journal of men's health, 31(1), 58-63.
Shridharani, A., Lockwood, G., & Sandlow, J. (2012). Varicocelectomy in the treatment of testicular pain: a review. Current Opinion in Urology, 22(6), 499-506.

What are you saying when giving directions to men during pelvic floor muscle training, and how do those instructions affect the effectiveness of a contraction? These questions are tackled in a study that is very interesting to therapists working in pelvic dysfunction. 15 healthy men ages 28-44 (with no prior training in pelvic floor training) were instructed to complete a submaximal effort pelvic muscle contraction. Tools utilized to acquire data in the study include those below:
| Assessment tool | Measuring |
| Transperineal ultrasound | displacement of pelvic floor landmarks |
| Surface EMG (electromyography) | abdominal, anal sphincter muscle activation |
| Nasogastric transducer | intra-abdominal pressure (IAP) |
| Fine wire electromyography (3 participants only) | puborectalis, bulbocavernosus muscles |
Participants sat upright on a plinth (backrest reclined at ~20 degrees with their knees extended). Directions for the submaximal efforts were given by telling the men to produce a level 3/10 effort with 10 being a maximal contraction. The men were instructed to hold the contraction for 3 seconds, and they were given 10 seconds rest between each of the 4 contractions using different verbal cues. (This series of 4 contractions was repeated with randomization for verbal cues, with a 2 minute rest in-between.) Verbal instructions were intended to target specific contractile tissues as described below- some of this theory could be validated via the fine wire EMG.
| Verbal cue | Targeting |
| "tighten around the anus" | anal sphincter |
| "elevate the bladder" | puborectalis |
| "shorten the penis" | striated urethral sphincter |
| "stop the flow of urine" | striated urethral sphincter, puborectalis |
Displacement, IAP, and abdominal/anal EMG were compared for the different verbal instructions. The greatest dorsal displacement of the mid-urethra and striated urethral sphincter activity was noted with the instruction to "shorten the penis." "Elevate the bladder" encouraged the greatest increase in abdominal EMG and IAP, while "tighten around the anus" induced the greatest anal sphincter activity. Displacement of pelvic landmarks correlated with EMG readings of the muscles thought to produce the targeted movement. The authors conclude that the therapist's choice of verbal instructions can influence the muscle activation and urethral movement in men. They suggest "shorten the penis" and "stop the flow of urine" for optimal activation of the striated urethral sphincter. They also point out the fact that by using the fine wire EMG and correlating muscle activation to observations with the transperineal ultrasound, the study validates the use of the less invasive method. If you are ready to jump into more education about male pelvic rehabilitation, join us in Denver in early August, or Seattle in November.
Physical therapist, educator, researcher, and clinical instructor Daniel Kirages, who was mentioned in Do Male Therapists Belong in Pelvic Rehab: Part I, shares his viewpoint from the perspective of his various roles.

“As a male, how did you get involved in pelvic rehab?” This is a question I have been asked countless times and the answer can be pretty simple, I usually say “It’s really not much different than any other musculoskeletal related issue. I’m just not afraid of working below the belt.” Working within the domain of neuro-musculo-skeletal physical therapy offers an endless supply of opportunities. Pelvic rehab is just one subcategory amongst many and this can be further subdivided into several categorizations as well – incontinence, voiding dysfunction, pain, etc. Despite a heavy dose of specialized knowledge necessary for these topics, ultimately we view the patient/client using a similar lens as any neuro-musculo-skeletal condition. This would include the need to examine and intervene for identified deficits in motor coordination, mobility, flexibility, strength, awareness and knowledge. Therefore, all PTs are primed to enter the world of pelvic rehab and they should consider “uploading the mental software” of pelvic specific knowledge by taking courses and finding a mentor to get started.
Being a male within what is typically considered a female related health domain never really bothered me. It just made me witness what a great opportunity it is and how I can be somewhat unique with my practice because there was and still is a need for more male PTs to be involved in pelvic rehab. Early on in my career I would see more females than I do now because our clinic needed the coverage and I wanted to use all aspects of the pelvic related knowledge I acquired. There was never an issue because the patients were willing to work with me; it was not a big deal to them because most of the time a male physician referred them to me in the first place. I would protect myself from any concerns by having a female aide or student be my chaperone in the room. This way a witness was present. It was not a burden on the clinic in any way, and actually the chaperones reported feeling very enlightened about what I do and I believe having a chaperone comforted the patient as well. The male patients I treat are so grateful and many express how they would be uncomfortable with a female therapist although they would go "if they had to". Of course, we as the practitioners know that the care offered by a PT of any gender will be therapeutic and professional, but the patient would not know until they had a positive experience. Some of my patients have avoided going to PT for their pelvic dysfunction until they discovered they can see a male PT. Unfortunate, but true.
The sheer number of people experiencing pelvic health related disorders speaks to the need for competent PTs to help them, but we have competition from urologic nurses, occupational therapists, Pilates instructors, personal trainers amongst others. However, we as PTs are most equipped to serve this population because of our educational backgrounds in manual therapy, exercise physiology, systems physiology and the priceless ability to take time to educate our patients. So the door is open for all of us to get involved and join the world of pelvic rehab which is why I try to make a push to incorporate pelvic rehab topics within entry-level DPT programs. We are making some gains in select programs, but without the PT board exam or the school credentialing agencies seeing value in pelvic rehab it will not change rapidly. The last several years there has been at least one male student applying each semester for a 16-week clinical affiliation with me for a hybrid ortho/male pelvic health experience. As long as there are more PTs offering this exposure to male students we will soon be populating the pelvic rehab world with a bit more testosterone, which can only be a good thing.

Earlier this week a blog post asked the question "Do male therapists belong in pelvic rehab?" With increased frequency, male therapists are participating in pelvic rehab coursework and practices. Some of the male therapists are even attending coursework as students. I asked Justin Stambaugh, a student from Duke University (who very much impressed me with his command of the material, and his calm, curious, and competent demeanor), a few questions about his path into pelvic rehab. Below are his responses.
Holly: How did your path lead towards pelvic rehab in general?
Justin: Pelvic rehab really necessitates an openness and sense of comfort regarding issues that can be seen as very personal, private, and even taboo. I was drawn to pelvic rehab because I am the type of person who doesn’t believe that individuals should have to suffer in silence because of fear or embarrassment of addressing their issues. I want people to know that they can and should seek treatment for their pelvic health issues, and that physical therapy can be a valuable resource in this regard.
I also value the complexity of pelvic rehab. In addition to the clinical aspect of care there is also the psychosocial element that adds to the scope and depth of treatment. I appreciate that pelvic rehab requires the clinician to continuously evaluate and adapt their approach in order to be proficient.
Additionally I find that often times many physicians, patients, and other physical therapists don’t realize the extent of what we are capable of treating, and how great of an impact we can have on someone’s life. I get excited about educating and promoting this side of the profession.
Holly: What is your viewpoint on how you will be perceived as a male therapist in treating pelvic rehab with a female patient?
Justin: As a male therapist in the pelvic rehab setting I understand that there are some female patients who will be hesitant to work with me solely because of my gender. I think this is an unfortunate fact, however it simply requires me to be a bit more industrious as a practitioner. Patients who may initially be uncomfortable with me due to my gender are really just asking me to prove to them that I know what I’m doing and that I am trustworthy. It is completely understandable that I need to win their trust before moving forward with any type of treatment. I respect my patients and ultimately just want what’s best for them. We can work together on achieving this goal, and find the correct path that suits each patient’s needs based on their comfort level. Often times I think of the phrase “to a man with a hammer, everything looks like a nail”. Although I am capable of performing an internal pelvic floor exam and subsequent treatment, there are also external approaches that may work just as well for an apprehensive patient depending on their presentation. This may also help gain their trust in order to implement more effective care in future sessions.
Holly: How do you think your generation differs from those before you in addressing the entire issue of gender?
Justin: I would like to think that my generation is more open regarding issues of sex and gender. However I think there are still many hurdles left to climb in this regard. I feel that socially my generation is part of an evolution in tolerance and empathy towards diversity with respect to issues such as gender, gender identity, sexual orientation etc. All of these qualities define some part of all of us and are constantly being communicated and evaluated. If we look back through history we see the dynamics of social inequality based on gender. Today we continue to see broad discussions regarding sex and gender. I feel that each generation continues to grow from these conversations and socially we persist in advancing our understanding and comfort regarding this topic.
Holly: Where do you see us (on the continuum) as a profession in normalizing the experience of having treatment directed to the pelvis by any gendered therapist to any gendered patient?
Justin: It would be my hope that in the future more institutions will instruct pelvic health with patient models that allow students to interact and conduct treatment based therapies in a clinical manner. I feel that in order to alleviate some of the gender based fears and apprehension regarding pelvic rehab from a professional perspective, all students should get to experience this aspect of physical therapy before deciding if its for them. I do feel it’s unfortunate that there are not more males who are interested in pelvic rehab. Oftentimes people are afraid of what they don’t know. It seems that perhaps pelvic rehab has remained somewhat enigmatic in that many individuals don’t get to experience this type of patient care, and therefore never approach it. It is such a great benefit to be able to work with this population of patients. I feel that the more exposure and normalization pelvic rehab gets to the patient population as well as to the professionals in the field of physical therapy the more we will see an increase in gender representation within the profession.
If the work of pelvic rehab is in the hands of students like Justin, we have so much to look forward to in our field. Thank you to Justin for being willing to articulate his thoughts and experience so that we can continue to explore issues of gender in pelvic rehabilitation.
This question is one that, a decade ago, may have made more sense to ask, as very few male therapists were engaged in the world of pelvic rehabilitation. Most pelvic rehabilitation practices still stem from programs developed in "Women's Health" so it's logical to see more female patients being treated, usually by female therapists. We are at an exciting time in the healing professions, and particularly in pelvic rehabilitation, when choice of provider may come to be based more on experience, personality and qualifications of the treating therapist than on the provider's or patient's gender. At the Institute's most recent entry-level Pelvic Floor 1 (PF1) courses, 2 male therapists were in attendance at 2 different PF1 courses on opposite sides of the nation. This shift (we tend to have an occasional male therapist within the pelvic floor series courses) has been noticed, and at the Institute, we have committed efforts at exploring if and how this shift affects our coursework. For example, are the instructors comfortable, are the female participants cool with it, and do the men feel welcomed? To find out a little more about the subject, I bring your attention to a few of the men who are currently representing the field of pelvic health.
Herman & Wallace Institute faculty member, Peter Philip, has treated both men and women in his practice for years. This treatment involves internal assessment and intervention when needed, and Peter approaches all of his patients with the same matter-of-fact, clearly defined consent. As a private practice owner, it makes sense that Peter is able to retain his patients regardless of the condition for which they are seeking care. Having to refer a patient to another therapist or clinic would negate the ability for a therapist to provide comprehensive care. On his website you will find a listing of women's health issues described next to sports, work, and other lifestyle injuries.
I posed the following question to Jake Bartholomy , physical therapist in Seattle, Washington: "Why is it so important for a male therapist to be involved in pelvic rehab, regardless if the goal is to focus on working with male or female or other gendered patients?" Jake's response reflects the value of offering choices to the patients he serves: "I believe it's important for people to have a choice in their therapist. Many people are shy and nervous to discuss their pelvic issues and if male or transgendered patients are more comfortable working with a male therapist, I'm proud to offer that service in the Seattle area."
I recall meeting Daniel Kirages, physical therapist and clinical instructor at the University of Southern California, at a male pelvic floor course years ago. When he introduced himself to the group, he joked that he was there as the token male "to break up the girl party." While this joke has stuck with me, it also drives home the point that it takes courage to show up at coursework which has previously been dominated by female therapists. Daniel has been involved in research, teaching in the classroom and online, and lecturing nationally about pelvic rehab.
In my experience as an instructor, the male therapists who attend pelvic rehab courses are exceptionally grounded, open-minded, and exude a quiet confidence that seems necessary for working with sensitive issues surrounding pelvic rehabilitation. Just for the record, we absolutely do believe that male therapists belong in pelvic rehabilitation coursework and practice, and we at the Institute are going to continue to explore how we can support all genders working in this much-needed, and good work. If you are interested in learning more about the course series or any specialty topics courses, check out our course listings here.
Among the challenges in research for chronic pelvic pain is the lack of consensus about diagnosis and intervention. Prominent researchers and physicians J. Curtis Nickel and Daniel Shoskes describe a methodology for classification of male chronic pelvic pain using phenotyping, which can be simply described as “a set of observable characteristics.” The authors point out in this article that men with complaints of pelvic pain have historically been treated with antibiotics, even though now it is known that most cases of “prostatitis” are not true infections. With most patients having chronic pelvic pain presenting with varied causes, symptoms, and responses to treatment, Nickel and Shoskes acknowledge that traditional medical approaches have not been successful.
In an attempt to improve classification of patients and subsequent treatment approaches, the UPOINT system was developed. The domains of the system include urinary, psychosocial, organ specific, infection, neurological/systemic conditions, and tenderness of skeletal muscles, and are listed below. Within each domain, the clinical description has been adapted from the original study (which can be accessed full text at the link above.)
UPOINT Domains
-Urinary: CPSI urinary score > 4, complaints of urinary urgency, frequency, or nocturia, flow rate , 15mL/s and/or obstructed pattern
-Psychosocial: Clinical depression, poor coping or maladaptive behavior such as catastrophizing, poor social interaction
-Organ specific: specific prostate tenderness, leukocytosis in prostatic fluid, haematospermia, extensive prostate calcification
-Infection: exclude patients with evidence of infection
-Neurological/systemic conditions: pain beyond abdomen and pelvis, IBS, fibromyalgia, CFS
-Tenderness of skeletal muscles: palpable tenderness and/or painful muscle spasm or trigger points in perineum or pelvic muscles
Within the initial research utilizing the UPOINT classification system, the authors report that most patients fall into more than one domain, and that the more domains a person is identified with, the more severe the symptoms. The domains leading to the highest impact are the psychosocial, neurological/systemic, and then the tenderness domain. The referenced article points out that the most impactful domains are the ones that are non-prostatocentric, or focused on dysfunction within the prostate itself. Phenotyping may indeed lead to improved classification of and treatment of male chronic pelvic pain. If you are interested in learning more about male chronic pelvic pain, there are still two opportunities to take the Male Pelvic Floor continuing education course this year. In August of this year, the course will take place in Denver, and in November, the male course will return to Seattle.