When we think of pelvic floor dysfunction, our minds often go straight to adults. We may even consider toddlers or children struggling with conditions like constipation or bedwetting. A population I frequently find missed is the infant! Many providers don’t realize that the pelvic floor issues that show up in infancy don’t have to be waited out.
As pediatric pelvic health providers, we have a unique and powerful role to play in helping babies who struggle with common challenges like reflux, colic, constipation, feeding difficulties, and even motor delays. At the root of many of these concerns lies the pelvic floor—an area often overlooked in traditional pediatric care. These parents will go to their providers, and they’ll be offered advice like “hold them upright for 20 minutes after feeding” or “try a lactation consultation,” but what happens if these interventions are not enough, OR what happens if a rehab provider wants to provide more support to a struggling family.
You may be thinking, “I don’t do pediatrics.” If that is your stance, I recommend you keep reading. You don’t have to be a dedicated pediatric therapist to provide families struggling with cranky or uncomfortable babies. Even if you don’t want to provide specific recommendations and treatment, you can still screen and offer referrals for support and even this step will create improvement in the quality of life of your families.
Understanding the Infant Pelvic Floor: More Than Just Diaper Changes
The abdominal canister in infants is still developing and is deeply interconnected with multiple systems in the body:
- The digestive system (contributing to reflux, gas, and constipation)
- The nervous system (especially for babies with difficulty calming or regulating)
- The musculoskeletal system (torticollis, body tension, abnormal movement patterns)
- The oral-motor system (especially in cases of tethered oral tissues or poor latch)
When these systems are under stress or not functioning in sync, the baby will likely be showing difficulty in performing regular functions, causing them to be uncomfortable. All babies express their discomfort differently, but this can lead to stressful symptoms such as crying, fussing, gassiness, constipation, reflux, and vomiting, leading to abnormal posturing and gross motor delays due to these adverse symptoms.
What Infant Pelvic Floor Dysfunction Looks Like
Pelvic floor issues in babies don’t always look like they do in adults. Instead, rehab providers may notice:
- Chronic straining to poop or lack of bowel movement coordination
- Irregular bowel habits, bloating, and gas
- Body tension that affects feeding or limits comfortable tummy time
- Shallow or inefficient breathing patterns
- Arching or clenching behaviors in response to gas or discomfort
- Difficulty tolerating changes in position or touch
These signs are often dismissed as “just colic” or “something they’ll grow out of,” but we know that targeted therapy can make a significant difference—not just in comfort, but in functional development.
 The Role of Rehab Providers: PTs and OTs Working Together
The Role of Rehab Providers: PTs and OTs Working Together
Both physical therapists and occupational therapists play essential roles in assessing and treating infant pelvic floor dysfunction.
Physical therapists focus on:
- Core and pelvic floor coordination
- Alignment and tension patterns affecting bowel/bladder mechanics
- Breathing mechanics and diaphragm coordination
- Tummy time, head shape, and early motor development
Occupational therapists bring expertise in:
- Feeding and oral-motor function
- Sensory integration, especially around elimination and body awareness
- Nervous system regulation and co-regulation strategies for parents
- Positioning to support optimal arousal and digestion
Together, this integrative approach addresses the whole baby, not just their symptoms.
Why This Matters: Long-Term Impacts Start Early
We’re not just aiming to reduce fussiness or help with pooping (although that’s often where we start!). We’re helping to lay the foundation for:
- Healthy bowel and bladder habits
- Confident motor skill development
- Positive body awareness and sensory processing
- Easier transitions to solids and potty training down the road
Early therapy can prevent compensatory patterns and teach families tools that make everyday care easier and more connected.
A Tool for Your Toolbox: Pediatric Pelvic Floor Play Skills
To help bridge the gap between pelvic health and pediatric development, we offer a class called Pediatric Pelvic Floor Play Skills. It’s designed for rehab professionals to learn specific play skills and actionable treatment techniques for each age group of the pediatric client, from the infant to the teen/tween.
For each age category we cover:
- Age-specific considerations, tips, and tricks
- Play-based strategies to support pelvic floor coordination for each age
- How to support pelvic health treatment
- Case studies and hands-on tools for both PTs and OTs
- Problem solving for more difficult cases and situations
If you're looking to expand your skill set, collaborate across disciplines, or just get more confident in treating your littlest patients - this class is for you. Join me next weekend on May 4th!
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating pelvises and ages with a variety of Pelvic Health dysfunctions. There is not much she has not treated since beginning this journey, and she is always happy to further her education to better help her patients meet their goals.
Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating pelvises and ages with a variety of Pelvic Health dysfunctions. There is not much she has not treated since beginning this journey, and she is always happy to further her education to better help her patients meet their goals.
Dr. Pluchino strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at present. In 2020, she opened her own practice called Practically Perfect Physical Therapy to help meet the needs of more clients. She has been a guest lecturer for Rutgers University's Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.

If you saw Ethical Considerations for Pediatric Pelvic Health and thought “Why are they making ANOTHER ethics class?” please let me take a moment to explain its origin and purpose in the Herman and Wallace course offerings. I wrote my Pediatric Pelvic Floor Play Skills course when I had colleagues asking for ways to play with their patients. When I started teaching this class, some of the most common questions that came up seemed like ETHICAL questions. How do we handle pediatric care in different settings? How do we get consent from minors? If a child says no but their legal guardian wants the assessment done, what does the provider do?
Pediatric Pelvic Floor Play Skills is a class written to help providers take the pelvic health knowledge they have, and learn activities they can perform with different ages of children to help work on their pelvic floor function. One of the tricky parts of working with children is including the child in their care plan and coordinating with caregivers. In this course, talk about specific concerns and considerations by age, as well as strategies to bring to a provider's practice. This class is for the provider who does not have a lot of experience treating pediatric patients and wants to learn how to make sessions enjoyable and effective. While in Ethical Considerations for Pediatric Pelvic Health, we review the different overall milestones, as well as what age-appropriate expressions of sexuality may look like as children develop toward adulthood.
Let's talk about Pediatric Care
When we say “pediatric” this can span from infants to teenage age groups. Dealing with a crying baby will be different decision-making versus a toddler in a tantrum or a defiant teen. The pediatric population is a vulnerable group because they can’t advocate for themselves, their own interests, and their health to protect themselves from harm. When we consider decision-making with a child, a therapist should consider things like their development, family structure, competence, and education levels. Children develop in a variety of areas including their fine and gross motor skills, language, cognitive, social, emotional, and behavior.
In pediatric care, obtaining informed consent has two parts because it requires therapists to secure consent from caregivers and to seek assent from the child. Once they have obtained the parent’s permission, therapists should explain the procedures, potential benefits, and risks in an age-appropriate manner to the child. Therapists have to make sure the child feels comfortable and involved in their care at each step.
Pelvic health providers should establish clear guidelines about what information will be shared with caregivers and what will remain confidential when working with children, especially tweens and teens. This helps the therapist to build trust with the patient and encourages open communication with the patient. We must also consider what the caregivers are entitled to hear about their child’s life and medical care. For example, if a tween wants to talk to you about sex, do you feel equipped with the ethical implications for yourself in your practice? What about if a child discloses a sexual assault at school? What about if a teenager tells you they are pregnant but hasn’t told their parents? This class will give some guidelines to make these decisions and provide a peer “think tank” to further discuss.
One of the easiest ways to be an effective pediatric provider includes communication with the patient and their support system. Make sure to review topics like the condition, treatment options, and expected outcomes to empower them to make informed decisions. Keep your communication clear and provide educational materials that are accessible and understandable. Make sure to check with caregivers about what words and pictures they are comfortable with the child seeing and hearing. Some children or caregivers may have personal, religious, or cultural implications that may limit what education they want the child to be exposed to.
Every child is unique, and their treatment should reflect their individual needs, preferences, and circumstances. Therapists should listen to the child and their support network, and incorporate their feedback into the plan of care. Consider their life and routine to make sure their care and homework fit into their daily schedule. Advocating for the needs and rights of pediatric patients is a critical aspect of ethical care. Therapists may need to recommend resources, treatments, and accommodations, and promote awareness and education about pediatric pelvic health issues within the broader community. This may include coordinating with a child’s daycare, school, or other medical providers.
What course is right for you?
- Ethical Considerations for Pediatric Pelvic Health on October 13th - Learn more about the ethical challenges pediatric pelvic health practitioners may experience including consent, managing situations of trauma and abuse, and managing autonomy for minors. If you work with pediatric patients on a regular basis, this class can be an additional step in your practice. It will review topics like consent, abuse, education, communication, and diagnoses that tend to have more ethical considerations with pediatric patients. Join us to review background information and then discuss, as a group, different cases and ethical situations to help further your pediatric clinical practice.
- Pediatric Pelvic Floor Play Skills on October 20th - This is a beginner-level course and is a good fit for providers who do not have a lot of experience treating pediatric patients and want to learn how to make sessions enjoyable and effective. In this course, we discuss specific concerns and considerations by age, strategies to bring to a provider's practice, sample home programs, equipment purchase lists (with a budget in mind), tips for helping get families on board with the implementation of care, and resources such as outcomes measures, developmental milestone checklists, and recommendations things parents ask for like how to talk about periods and sex.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC
 I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.
Dawn is debuting a new course, Pediatric Postural Development, with Herman & Wallace on September 29, 2024.
Most physical and occupational therapists learn about one diaphragm in school: the respiratory diaphragm. But did you know that Osteopathic Manipulative Medicine recognizes 5 different diaphragms within the body? They include tentorium cerebelli, tongue, thoracic outlet, respiratory diaphragm, and pelvic floor. (1)
The intricate myofascial connections between all these diaphragms are fascinating! But as a pediatric pelvic floor therapist, what’s the significance of these connections when you look at kids’ functional mobility and strength?
The pelvic floor and respiratory diaphragm are the two main structures that we’ll be discussing today. You’ll learn how they develop during infancy and childhood and how their functional relationship affects your assessment and treatment for kids with bowel and bladder dysfunction.
Development Of The Pelvis, Spine, And Diaphragm During Infancy
Pelvic Structure At Birth
 Pelvic structure and spinal curvatures develop based on the activities of infants and young children. The educational role that you have as a pediatric therapist is significant during a child’s first years of life, especially for children with congenital or developmental delays. Doing your best to help them achieve these developmental goals will greatly affect their life in later years.
Pelvic structure and spinal curvatures develop based on the activities of infants and young children. The educational role that you have as a pediatric therapist is significant during a child’s first years of life, especially for children with congenital or developmental delays. Doing your best to help them achieve these developmental goals will greatly affect their life in later years.
At birth, the pelvis of the baby is funnel shaped and the respiratory diaphragm is oblique. You can observe a neonate with a wide rib cage, which only allows for a short descent of the ribs. You can hear evidence of this as a newborn’s cry is very short. At this time, their pelvic floor has no posture.
Cervical Lordosis
The first curve to develop in an infant is cervical lordosis. Neck control improves as the head is challenged against gravity. In an upright position, the neck is challenged to maintain a neutral position. In prone, the neck is challenged to extend and re-enforces a lordotic curve.
Tummy time is important to begin at a young age. Not only do kids develop neck and core strength, but extending the neck in a prone establishes proper cervical lordosis for later in life.
Thoracic Kyphosis And Ribcage
Thoracic kyphosis develops when a child begins sitting. Again, thinking about sitting from a trunk control perspective is important, but establishing proper kyphotic alignment should not be overlooked. A mild degree of kyphosis is normal, but congenital deformities can exaggerate children’s kyphosis and increase the difficulty of achieving good sitting posture.
Independent sitting is an important milestone itself and further affects: (2)
- object perception
- language development
- spatial memory
- visual processing
- overall cognition
When treating infants, let’s remember to teach how important the skill of independent sitting is. We will discuss this further in the last section and how it relates to pelvic floor function.
As an infant increases their activity in the quadruped position, the diaphragm angle gets steeper inside the ribcage. This angle also increases through weight-bearing positions and with the development of the scapular stabilizers around the ribcage.
Lumbar Lordosis And Sacrum
Standing influences lumbar lordosis. Once again, standing challenges core stability and develops strength. But also recognize how standing helps the child establish proper lordotic lumbar posture.
Furthermore, in standing, the diaphragm orientation changes. The diaphragm becomes more parallel to the pelvic floor. As the diaphragm establishes a more horizontal orientation with standing and walking, the muscular tone increases as it responds to the vertical pressure and pull of the viscera.
This upright position also develops the pelvic floor to counteract the pressure of the viscera being pulled down by gravity. Counternutation of the sacrum protects the pelvic floor from full visceral pressures.
Let’s take a look at the functional relationship as the diaphragm and pelvic floor develop.
Functional Relationship Of Diaphragm And Pelvic Floor During Childhood
 When the diaphragm and pelvic floor are developed in their horizontal orientations, they begin moving together during breathing. When inhaling, the diaphragm and pelvic floor descend as the ribcage and abdominal cavity expand. When exhaling, the diaphragm and pelvic floor ascend. The continued alternating movement mobilizes the viscera and creates a lymphatic pump.
When the diaphragm and pelvic floor are developed in their horizontal orientations, they begin moving together during breathing. When inhaling, the diaphragm and pelvic floor descend as the ribcage and abdominal cavity expand. When exhaling, the diaphragm and pelvic floor ascend. The continued alternating movement mobilizes the viscera and creates a lymphatic pump.
This relationship between the diaphragm and pelvic floor is why it’s so important to look at breathing mechanics in kids. Ribcage mechanics and good diaphragm strength and tone affect the mobilization of the viscera, including the stomach and intestines. This is especially relevant when treating kids with constipation.
If you watch constipated children breathe, you will notice that they often breathe more anteriorly through their bellies instead of up and down. You will also notice minimal or no expansion of the ribcages.
Additionally, when the viscera descend, this cues the pelvic floor to activate and continue developing. Around ages 2-3, the pelvic floor develops enough stretch to react to bowel and bladder function. This is the age when children typically develop urinary continence.
Although therapists usually use the term pelvic “floor”, it’s important for you to consider this as a “diaphragm”. The pelvic “diaphragm” is a dynamic partition that serves to adjust pressures and pump fluids within the body.
Lymphatics throughout the trunk, head, and limbs are all regulated by the pumping of the body’s five diaphragms. The diaphragms work together to regulate pressures, pulling fluids and toxins into the lymph system to detoxify the body. The colon has a great lymphatic network, so this is especially important in kids with bowel issues.
Now you understand how the respiratory diaphragm and pelvic floor influence function in typically developing children. What about kids with impaired functional mobility or impaired gross motor delays? Let’s dive into these considerations.
Pediatric Postural Impairments And Gross Motor Developmental Delays
 Children with physical developmental delays will have delayed pelvic floor control as well. As you learned earlier in this blog, establishing control in positions including prone, sitting, quadruped, and standing, develops a baby’s spinal curvatures.
Children with physical developmental delays will have delayed pelvic floor control as well. As you learned earlier in this blog, establishing control in positions including prone, sitting, quadruped, and standing, develops a baby’s spinal curvatures.
If children have conditions such as spina bifida or cerebral palsy, those developmental positions may be delayed or sometimes never reached.
Improper spinal curvature early in life will affect a child’s ability to attain or maintain postural positions required for voiding and defecation. This will also delay the development of the relationship between the diaphragm and pelvic floor control.
Start looking at these milestones not only from your perspective of postural control and gross motor function but also to help improve their bowel and bladder function:
- holding head up in prone
- sitting independently
- quadruped reaching and crawling
- standing independently
- walking
If a child never stands or walks, they will struggle to develop diaphragm and pelvic floor control because gravity will not challenge this system. Spending time in upright positions by using assistive devices such as standers or walkers will help develop respiratory capacity and pelvic floor control.
When you have this treatment outlook, you can help parents shift their perspectives too. Parents of children with disabilities are often overwhelmed and tired. Help them to understand the benefits of continued work in practicing and attaining developmental postural and motor skills.
 The new course, Pediatric Postural Development debuts on September 29, 2024 and focuses on the role of the pelvic floor, diaphragm, and core. This one-day course is designed to help therapists understand the development of the diaphragm and pelvic floor muscles (PFM) as they relate to core function and continence in children. Learn how to connect the ribcage, the diaphragm, and the pelvic floor for proper core activation, as well as receive instruction in anatomy and development of the diaphragm and its relationship to the pelvic floor/core. The information presented in the course applies to children who have been diagnosed with Cerebral Palsy, Down syndrome, ASD, Hypotonia, and more.
The new course, Pediatric Postural Development debuts on September 29, 2024 and focuses on the role of the pelvic floor, diaphragm, and core. This one-day course is designed to help therapists understand the development of the diaphragm and pelvic floor muscles (PFM) as they relate to core function and continence in children. Learn how to connect the ribcage, the diaphragm, and the pelvic floor for proper core activation, as well as receive instruction in anatomy and development of the diaphragm and its relationship to the pelvic floor/core. The information presented in the course applies to children who have been diagnosed with Cerebral Palsy, Down syndrome, ASD, Hypotonia, and more.
References:
- Bordoni B. The Five Diaphragms in Osteopathic Manipulative Medicine: Myofascial Relationships, Part 1. Cureus. 2020 Apr 23;12(4):e7794. doi: 10.7759/cureus.7794. PMID: 32461863; PMCID: PMC7243635.
- Kretch, K. S., Marcinowski, E. C., Hsu, Y., Koziol, N. A., Harbourne, R. T., Lobo, M. A., & Dusing, S. C. (2023). Opportunities for learning and social interaction in infant sitting: Effects of sitting support, sitting skill, and gross motor delay. Developmental Science, 26(3), e13318. https://doi.org/10.1111/desc.13318
Special thanks to Dawn for allowing The Pelvic Rehab Report to reprint her article, originally published on her website at kidsbowelbladder.com.
AUTHOR BIO:
Dawn Sandalcidi PT, RCMT, BCB-PMD
 Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn is a national and international speaker in the field, and she has gained so much from sharing experiences with her colleagues around the globe. In addition to lecturing internationally on pediatric bowel and bladder disorders, Dawn is also a faculty instructor at the Herman & Wallace Pelvic Rehab Institute. Additionally, she runs an online teaching and mentoring platform for parents and professionals.
In 2017, Dawn was invited to speak at the World Physical Therapy Conference in South Africa about pediatric pelvic floor dysfunction and incontinence. Dawn is also Board-Certified Biofeedback in Pelvic Muscle Dysfunction (BCB-PMD). She has also been published in the Journals of Urologic Nursing and Section of Women’s Health.
In 2018, Dawn was awarded the Elizabeth Noble Award by the American Physical Therapy Association Section on Women's Health for providing Extraordinary and Exemplary Service to the Field of Physical Therapy for Children.

The HW admin team has been hard at work filling speaker spots, building breakout sessions, and creating fun new experience ideas for the upcoming 2025 conference.
If you're into pelvic health then this is the conference for you. HWConnect was created to provide a top-tier networking event for pelvic rehabilitation practitioners that focuses on providing a safe environment for professional development, exposure to new products, and sharing inspiration for all things pelvic health.
HWConnect features keynote speakers, breakouts, labs, and educational sessions. Topics range from pediatrics with Dawn Sandalcidi to gender-affirming care with Ken McGee. HWConnect is all about connection - the name says it all. Network. Learn. Grow. Repeat. 
Registering is as easy as 1, 2, 3!
- Complete online registration.
- Book travel and lodging. HWConnect will be held at the Hilton Seattle Airport & Conference Center and HW has special pricing set up for attendees.
- Show up, and don't forget to stop by and say hello to all of your favorite HW team members!
Need More Information?
- Keynote Speakers are the indomitable Dawn Sandalcidi, PT, RCMT, BCB-PMD (she/her), Nancy Norton, RN (she/her), and Leticia Nieto, PsyD, LMFT, TEP (she/her).
- Speakers include Ken McGee, PT, DPT (they/he), Dr. Cindy Mosbrucker (she/her), Meryl Alappattu, PT, PhD (she/her), and Carole High Gross, PT, DPT, PRPC (she/her).
- Breakout sessions, workshops, and labs include yoga, meditation, rehabilitative ultrasound imaging, squat analysis, and MORE - all led by your favorite HW faculty including Dustienne Miller, Nari Clemons, and Allison Ariail.
- HW proudly welcomes second-time conference sponsor CMT.
- Vendor Hall featuring exhibitors including Intimate Rose, Slippery Stuff, and Raise the Pelvic Floor.
- Non-profit booths feature the Kenya Scholarship Foundation and Open Arms Perinatal Services. Read this past blog to learn more about the Kenya Scholarship Foundation.
- Special Podcast Guests feature Callie and Rachel from Pelvic Service Announcement (PSA) and Courtney from Raise the Pelvic Floor.
For more information and a full lineup check out the HWConnect 2025 page!
Already Coming to HWConnect?
That's amazing!
Herman & Wallace would love your help spreading the word about HWConnect 2025 and the chance to connect with the amazing people in our community. Check out this page where you can review and share all the programming we’ve booked thus far. https://hermanwallace.com/connect-2025
We look forward to seeing you at HWConnect 2025!

Imagine you’re a provider who has foundational information about the pelvic floor. Maybe you’ve just started taking coursework for adults, you may have taken a pediatric pelvic health class or maybe you’ve been treating adults for years. You know the anatomy, the physiology, and the general treatment practice guidelines.
- Your clinic gets a call about a baby with colic and your supervisor asks you if you could treat it. Do you accept the evaluation?
- You see a post on a “mommy Facebook group” asking for potty training tips for a child who is withholding stool during potty training. Do you tag your business/practice as a resource that can help?
- You have a family friend with a child struggling with voiding during the school day and they ask you for advice as a pelvic health provider. Do you have ideas on how to guide them?
- A patient you are seeing for pelvic floor issues asks you to start treating their teenager because they have “the same issues.” Does this seem scary to you?
Pediatric Pelvic Floor Play Skills is a class written to be a supplement to other pelvic health education classes a pelvic floor therapist has likely taken. This class helps providers take the pelvic health knowledge they have, and learn activities they can perform with different ages of children to help work on their pelvic floor function. The class shows videos of actual treatment sessions of different children in different age groups showing how to integrate stretching, strengthening, coordination, and other fun activities into a therapy visit.
One of the tricky parts of working with children is including the child in their plan of care and coordinating with caregivers. Pediatric Pelvic Floor Play Skills talks about specific concerns and considerations by age, as well as strategies to bring to a provider's practice. This class is for the provider who does not have a lot of experience treating pediatric patients and wants to learn how to make sessions enjoyable and effective.
This class includes sample home programs, equipment purchase lists (with a budget in mind), tips for helping get families on board with the implementation of care, and resources such as outcomes measures, developmental milestone checklists, and recommendations things parents ask for like how to talk about periods and sex.
The next Pediatric Pelvic Floor Play Skills remote course is scheduled for June 29th, come spend a day learning how to integrate what you already know into a playful session for your tiniest of clients to your angstiest teenager.
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.
Dawn Sandalcidi, PT, RCMT, BCB-PMD can be found online at https://kidsbowelbladder.com/. Dawn is a long time instructor with Herman & Wallace and has generously shared her recent blog with The Pelvic Rehab Report. "Stool Withholding And Core Activation" can be found in its original post on her website here: https://kidsbowelbladder.com/stool-withholding-and-core-activation/.
What do they have in common?
About 9-12% of children suffer from functional constipation, which is the vicious cycle of retained stool causing rectal distention and subsequent loss of sensation and urge to defecate, which results in further stool retention. The exact physiologic causes for functional constipation are not completely understood.
We know the bowel absorbs water constantly. The longer stool sits in the rectum, the harder it becomes. For some children, this leads to very large stools that are uncomfortable or difficult to eliminate. In turn, these children may practice something called stool withholding (which may be the reason stool was sitting in the rectum too long in the first place).
There are many other reasons a child may withhold their stools beside the standard issues that functional constipation presents. Some other reasons for stool withholding include:
- Inability to generate intraabdominal pressure
- Availability, likes, and dislikes of the toilet
- Fear of having a bowel movement
- Perineal sensation issues
- Psychological concerns
- Pain with defecation
- Dietary contribution
- Illness or infection
- Medications
- And more
No matter how or why a child began withholding stools, it’s vital to treat the problem as soon as possible. When withholding and constipation go untreated, they can cause lifelong issues. In this article, we will explore the relationship between constipation and core control, specifically the child’s ability to generate intraabdominal pressure.
What are the Symptoms a Child May have When Practicing Stool Withholding?
Normally, when enough stool enters the rectum and it’s time for a bowel movement, the rectum will send messages to the brain to make you aware that it’s time to have a poop. Ideally, when you receive this message and become aware of your body’s need to defecate, you find a toilet and do so.
When a child regularly withholds stools, the stool may become retained in the rectum and cause rectal distention and a subsequent loss of sensation. Because the rectum isn’t able to sense its fullness, the messages are never sent to the brain, and the sense of urge to poop disappears.
Although children who withhold stools may not have the urge to poop, they can have other physical symptoms if their stool withholding causes stool retention.
Physical symptoms of stool retention include:
- Abdominal pain
- Offensive body odor
- Stools that clog the toilet
- Decreased appetite
- Urinary incontinence or frequency
- And more
Children who withhold stools do not always have retention, however, and sometimes will simply withhold stools due to their environment (such as being at school during the day), and poop as soon as they get home.
How Might Core Strength Relate to Stool Withholding?
I treated a 6-year-old child once who had a bowel movement every single day, but only after he fell asleep in his parents' arms. His parents hadn’t been able to transition him out of diapers because of this. His bowel movements were so predictable that his parents would wait for him to poop, then clean him up and put him back to bed.
This child was also autistic and did have issues with low tone. I discovered during examination of the child that he had a difficult time voluntarily contracting his core muscles. Rotational and balance activities were difficult for him to perform as well due to his lack of core control.
You may be wondering what the core has to do with constipation, or stool withholding specifically. For starters, you need adequate core strength in order to sit upright on the toilet. Without proper core control, children may develop poor toileting postures which can lead to difficulty with defecation.
Correct toileting posture involves first being able to have enough hip extension, back extension, and side-to-side control to balance in a seated position on the toilet seat. Seats of differing heights add to the complexity of good toileting posture.

Proper Body Position for Toileting
Ideally, your feet should be supported, not dangling (which is a common occurrence for our children using adult-sized toilets). Forearms should be resting on the thighs, and the hips should be bent to at least 90 degrees of flexion. The spine should be in a neutral position (no posterior pelvic tilt).
This position allows for the pelvic floor muscles to relax appropriately, and for the core muscles to activate enough in order to produce appropriate intraabdominal pressure.
Without appropriate intraabdominal pressure generation, it will be difficult for a child to push out their poop. This is precisely what we discovered with my patient who was withholding until she got into bed. When in her parents' arms she was flexed, it was easier for her to generate enough intraabdominal pressure to poop, and so she did!
Knowing the reason for his withholding allowed us to target treatment planning where he needed it the most.
How to Address Core Strength in Children who Withhold Stools
Once you’ve determined that core activation is a root issue, you’ll need to address it in order to see any change with your patient’s bowel habits. Parents are usually at their wit’s end and are looking to you for answers. Your physical exam is your best tool in identifying root causes of stool withholding.
Many children attending physical and/or occupational therapy do suffer from low tone. As we’ve learned, this can compound constipation issues and even lead to stool withholding.
With the child above, we worked on core activation exercises first in supine, then in prone on an incline, and gradually added challenge to his exercises until she was able to generate enough intraabdominal pressure to poop on the toilet independently.
Even if your patient does not suffer from low tone, core activation and training may still be indicated. Some children have difficulty with coordinating or timing appropriate muscle contraction and relaxation. Be sure to evaluate the core when treating patients who suffer from constipation and stool withholding.
These children may have difficulty crossing midline as well. Age-appropriate exercises to engage the core while also incorporating diagonal and midline-crossing motions will be beneficial for those patients.
Additionally, you’ll want to assess the rib cage. Oftentimes I find children who have difficulty with core control also have a wider rib angle and hence need upper abdominal engagement exercises.
Lastly, many of the children you’ll treat will need help with rotation. This is a common finding during examination and without addressing rotation, you’ll see much slower progress.

Treating Stool Withholding and Core Issues is Possible
So many children with constipation will not receive appropriate treatment during childhood and their problems will persist into adulthood. It’s our job as pediatric therapists to identify children in need of help. Many children with bowel and bladder problems will be seen in your clinics for other issues, and unfortunately never even bring up the bowel or bladder concerns.
I put together a list of 5 Screening Questions you can ask your patients to determine whether they might be suffering from bowel or bladder issues and not even know it. This is a quick and easy way to identify patients in need of pediatric pelvic floor therapy.
It’s a great idea to get in touch with your local pediatric pelvic floor specialist to be able to easily refer these patients. You can also become a pediatric pelvic floor therapist yourself by taking my online courses! I believe this patient population is severely underserved and have made it easier than ever to learn how to best support these children.
My courses are held live in various locations around the world throughout the year, but I also offer online options for you to be able to work at your own pace from the comfort of home. Inside my online courses, there is space in every module to leave comments or ask questions and they go directly to me.
Sign Up For the Pediatric Functional Gastrointestinal Disorders Remote Course.
I’ve also created a group online where those who have taken my courses can collaborate, receive my mentorship, and discuss any issues that come up along their pediatric pelvic floor therapy journey. The group is called KBB Professional Village.
Learn More about KBB Professional Village.
Pediatric Functional Gastrointestinal Disorders
Course Dates:
November 12-13, 2022
May 20-21, 2023
November 4-5, 2023
Price: $600
Experience Level: Intermediate
Contact Hours: 15
Description: This two-day, remote course is offered on Zoom and is the next step for therapists who focus on the pediatric pelvic floor patient population. It is designed to expand your knowledge of the development of normal bowel patterns in children, introduce the new Rome IV criteria (Zeevenhoovenet al. 2017), and review the anatomy and physiology of the GI system with emphasis on Pediatric Functional Gastrointestinal Disorders (FGID).
This course will delve into the most common types of functional constipation and the tests and measures used to assess it. Special emphasis on constipation with the coexistence of fecal incontinence (Nurko, Scott. 2011) and the psychological effects of these disorders will also be presented. Additionally, participants who have not yet been trained will learn external and internal anorectal PFM evaluation of the pediatric perineum. Indications for rectal balloon training and determining the appropriate patient will be instructed with lab. Functional defecatory positions for breathing and PFM relaxation, manual therapy techniques of the abdominal wall and viscera will be taught.
Dawn Sandalcidi PT, RCMT, BCB-PMD is known as the go-to expert in the field of pediatric pelvic health. She has been practicing for 40 years this May and has concentrated on the pediatric pelvic floor for 29 of those. When it comes to pediatric pelvic floor issues, there is so much more than bedwetting, and often the practitioner needs to look beyond the pelvic floor.
Despite the growing number of pelvic rehab specialists treating men and women with PF dysfunction, children in this patient population remain woefully under-served. This can cause undue stress for the child and family, as well as the development of internalizing and externalizing psychological behaviors. Many of the techniques used in pediatric pelvic therapy can be translated to the adult population. The question is ‘who’s the driver?’ In pediatrics, it is typically a bowel issue.
The Standard American Diet involves food that is high in calories, saturated fats, trans fats, added sugars, and sodium. It is also lacking in the intake of essential nutrients for the body like fiber, calcium, potassium, and vitamin D. This lack of dietary fiber can cause issues with the digestive tract as well as the colon leading to constipation. Bowel dysfunction including constipation can contribute to urinary leakage and urgency (1). Constipation accounts for approximately 5% of visits to pediatric clinics (2) proving that there is a need for practitioners to know how to treat these pediatric issues.
Dawn focuses much of her pediatric knowledge on her two courses: Pediatric Incontinence and Pelvic Floor Dysfunction (PEDs) and Pediatric Gastrointestinal Disorders (PEDsG). Pediatric pelvic floor basics are covered in PEDs, including instruction in anatomy, physiology, development of normal voiding reflexes and urinary control, and learning how to talk with child patients. Biofeedback and ultrasound (which Dawn fondly calls jelly belly) are also covered and can be helpful as less invasive procedures for children.
PEDsG goes beyond the pelvic floor and opens up the door to look at the big picture of the whole child. Dawn shares that almost 80% of her kiddos with chronic constipation present with diastasis rectus abdominus. They can also have hyperextension in the thoracic spine, and the rib cage is postally rotated – where the kids don’t know how to bring it down.
Dawn is also on the threshold of writing a pediatric pelvic pain course that she expects to be ready later this year. Pediatric pelvic pain is becoming more prevalent, and it can’t be treated the same way as in adults. Dawn explains that “children don’t understand, so we’re actually creating a pediatric pain neuroscience protocol. It is a bio-psycho-social approach, and we use fun things.”
Research tells us that 15% of kids per year will outgrow bedwetting. Children who suffer from bedwetting can feel ashamed and embarrassed, have self-esteem issues, or even act out. There are 5 basics of where you start with a pediatric patient that are taught in PEDs. Dawn also shares 5 basics in her e-book, BEDWETTING BOOTCAMP(3):
- Avoid things that can irritate the bladder
- Avoid drinking anything just before bed
- Drink throughout the day
- Empty your bladder throughout the day
- Avoid constipation and straining
Everything in Pediatric Incontinence and Pelvic Floor Dysfunction builds into Pediatric Gastrointestinal Disorders, and everything in PEDsG builds into Pediatric Pelvic Pain. The more practitioners who learn about the pediatric pelvic floor means that more kids get treated and the fewer adults that will have pelvic floor dysfunction. To learn more about treating pediatric pelvic health register for one of Dawn Sandalcidi’s upcoming courses:
Pediatric Incontinence and Pelvic Floor Dysfunction: August 27-28th
Pediatric Gastrointestinal Disorders: May 14-15, November 12-13
References:
- Sandalcidi (Spring 2018). Paediatric incontinence and pelvic floor dysfunction. Journal of Pelvic, Obstetric and Gynaecological Physiotherapy, 122, 5–8.
- Thibodeau B. A., Metcalfe P., Koop P. & Moore K. (2013) Urinary incontinence and quality of life in children. Journal of Pediatric Urology 9 (1), 78–83.
- Dawn Sandalcidi PT, RCMT, BCB-PMD. BEDWETTING BOOTCAMP Frustrated by Bed Wetting? The 5 Ways to Speed Starting Up Dry Tonight! www.kidsbowelbladderPMD.com. https://cdn.fs.teachablecdn.com/YfP5rUfiRtOJxXZSZUso

Amanda Moe, DPT, PRPC specifically treats women, men, and children with disorders of the pelvis and pelvic girdle. Amanda earned her Pelvic Rehabilitation Practitioner Certification (PRPC) in 2015 to distinguish herself as a highly qualified and specialized practitioner in the field of pelvic health and worked at Texas Children's Hospital in Houston, TX. There Amanda assisted with the development and expansion of the pediatric pelvic physical therapy program treating children with a variety of diagnoses such as bowel and bladder dysfunction, constipation, encopresis, coccydynia, abdominal/groin pain, as well as other disorders related to the pelvic girdle. Amanda enjoys assistant teaching with the Herman & Wallace Pelvic Rehabilitation Institute in her free time as well as working out, practicing yoga, and spending time with her family.
Before the Book
I started off my career in Pelvic Physical Therapy treating adult women and men as do many physical therapists entering the pelvic niche. My local children’s hospital discussed a need for pelvic physical therapy in children which, with the help of Herman and Wallace’s Adult/Pediatric courses as well as mentoring from my local Gastroenterology department, I devoted the next few years of my career to.
I aided in program development and expansion of Pediatric Pelvic Physical Therapy services at Texas Children’s Hospital in Houston, Texas. After moving out of state, I then collaborated and expanded Pediatric Pelvic Physical Therapy services in Pittsburgh, Pennsylvania—working closely with both the Urology and Gastroenterology Department at UPMC’s Children’s Hospital of Pittsburgh. While treating children with pelvic dysfunctions is similar to treating those in adults, there is much to be considered when providing education to children, parents, and even referring providers about pelvic floor dysfunction and Pediatric Pelvic Physical Therapy.
The NEED for this Book
When educating children, parents, or even referring practitioners about pelvic floor dysfunction and physical therapy, I grew frustrated with the lack of “simplified” or “child-friendly” models, illustrations, or depictions available. Specifically, I saw a need for:
- the depiction of pelvic girdle muscles and organs in a “child-friendly” format for BOTH boys and girls
- pictures of what a child’s pelvic muscle “role” or “activity” is during peeing or pooping
- what common muscle dysfunctions in children “look like” in easy-to-understand pictures
Additionally, I longed for a book or resource that described common conditions and symptoms treated in Pediatric Pelvic Physical Therapy (or Occupational Therapy) as well as what the Pediatric Pelvic PT/OT evaluation and treatment may look like. In 2021, I decided to do something about this which lead to me writing my first book: Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children.
Book Features
Do you have parents, patients, referring physicians, or other medical providers wondering exactly what Pelvic Physical Therapy for children is like—look no further! In Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children, I explain the basics all in a rhyming, child-friendly format. This book introduces the collaborative nature in resolving children’s potty or pelvic troubles and describes how Pediatric Pelvic PT/OT often works closely with gastroenterologists, urologists, pediatricians, or other providers to remedy a child’s complaints. Pelvic PT for ME has many unique features pertaining to Pediatric Pelvic Physical Therapy, some of which are highlighted below:
- Common Conditions Treated
- I discuss typical conditions that are treated in Pelvic PT such as pee leaks, poo problems (constipation, poo leaks/smears), nighttime bedwetting, pelvic pain, and many others.
- Child-Friendly Anatomy Illustrations
- Age-appropriate anatomical illustrations of muscles and organs in the pelvic girdle are utilized throughout the book to aid in explaining bowel, bladder, and pelvic functioning.
- Pelvic Floor Muscles during Peeing or Pooping
- Pelvic floor muscle anatomy, functioning, and dysfunction—as they relate to potty troubles—are discussed through the use of child-friendly images to enhance not only child but also parent and referring provider understanding.
- Common Evaluation Techniques and Treatment Interventions
- The Pediatric Pelvic Physical Therapy evaluation, as well as typical treatment interventions, are discussed and illustrated to make both children and parents excited to seek treatment!
- Inclusion of Occupational Therapy
- While the field of Pediatric Pelvic Physical Therapy in of itself is new, I briefly discuss the inclusion of Occupational Therapists also providing Pediatric Pelvic Therapy services.
Where to Purchase
My primary goal behind the creation of this book was to develop an affordable resource for every Pelvic PT/OT who treats children. Secondarily, my goal was to increase knowledge and understanding of our services to parents, children, and potential referral sources or colleagues. Pelvic PT for ME encourages parents and children to refuse the notion that potty troubles “go away with age” and empowers children to be active participants in their Pelvic PT (or OT) experience. Enjoy this comprehensive yet simple storybook explanation of Pediatric Pelvic Physical Therapy, available on Amazon for $15.
Contact
Contact me or check out my website for more information: www.pelvicphysicaltherapyandmore.com
IG/Facebook: amandampelvicpt
This week The Pelvic Rehab Report sat down with senior teaching assistant and author, Mora A Pluchino, PT, DPT, PRPC, to discuss her new book “The Poop Train”. Mora works at the Bacharach Institute for Rehabilitation and in 2020, she opened her own "after hours" virtual practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016, as well as a TA with Herman and Wallace since 2020 with over 150 hours of lab instruction experience!
What or who inspired you to write this book?
My nine-year-old daughter has had issues with constipation since she was two. Our household is no stranger to talking about poop and all things related to poop to manage her tummy issues. I always tried to explain to her the purpose of habits like eating fiber and drinking water, as well as how poop moves through the body. One day my daughter started telling me that her “poop train wasn’t ready to leave the station” and I got the idea for the story!
Can you tell me about your book and the title?
I wanted a title that would be silly but interesting to a child. My goal was to create a book to be easy to read and understand the story about how food enters and leaves our body with resources within and after the book for parents to help manage their child’s bowels. I wanted it to be something that would be fun to read while on the potty, preparing for potty training or if a child is having an issue.
What does your daughter think of “The Poop Train”?
I just asked her and she took my computer over to answer. “I think that you are crazy and you talk about poop way too much! I also think that your book is super cute and even kind of funny. Kids and adults alike are going to love it because it talks about all the parts it needs to but it is not creepy or embarrassing.” - Nina P.
What’s your favorite thing about your book?
I am honestly in love with the illustrations. I had this idea for a few years and couldn’t do anything with it because I’m not good at drawing. I finally connected with the sister of a dear friend who shares my love poop talks and happens to be a talented artist. She brought my idea to life in adorable, inclusive, and simple images!
How do you think writing this book has impacted you as a PT and parent?
Taking Pelvic Floor Level 1 changed my life as a parent. This career path gave me the tools to help my daughter manage her constipation and resultant pelvic floor issues like post-void dribbling and bed-wetting. I wrote this book to help other parents who had similar struggles.
Were there any surprises along this book journey?
Funny story, I proofread my book multiple times along with my husband and a friend. My daughter read the book for the first time and found a TYPO! At that point, it was too late so my book became practically perfect. Hint - the typo is in the resource section!
What advice do you have for other PTs who are interested in writing?
I’d encourage anyone interested in writing something to go for it. Take your idea and nurture it until you can create it! Talk to others if you get stuck. I did this and found the illustrator of my dreams shortly after. And proofread a million times!
Do you think you’ll write another book?
I am finalizing the manuscript for my second pelvic health book. I was so happy with how Elizabeth Wolfe was able to capture the style I wanted that I asked her to work on a second project a few days after we finished our first. “Practically Perfect Pelvic Health 101: A Visual Tour of the Pelvic Floor” will be going to print soon!
How do I get a copy of this book?
“The Poop Train” is available in paperback on Amazon! I am also happy to send copies to fellow pelvic health professionals at a discount. I can be contacted by email at This email address is being protected from spambots. You need JavaScript enabled to view it.!
Mora Pluchino (She/Her)
Deb Gulbrandson, PT, DPT, along with Frank J Ciuba DPT, MS, is the author and instructor for a new course on osteoporisis that is launching remotely this month. Join Deb in Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals!
Osteoporosis is a disease of increasingly porous bones that are at greater risk for fracture. The normal “bone remodeling” of breaking down and building up bone as we age is out of balance. Similar to a bank account with withdrawals outpacing deposits, as time goes on there is more breaking down than building back up. This leaves the bone more vulnerable for fracture.
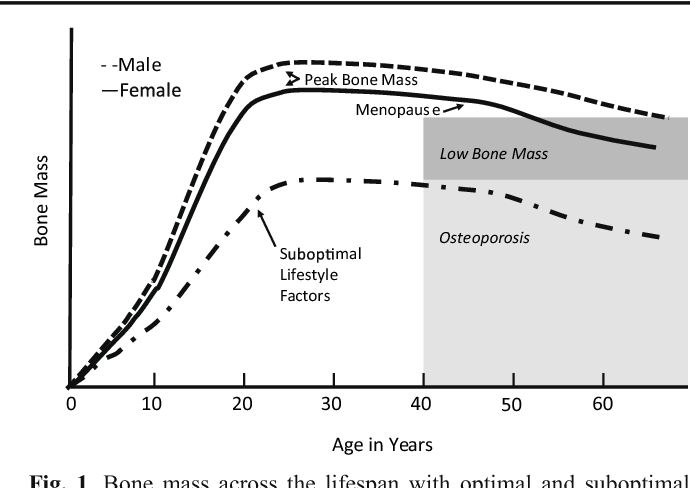
We tend to think of Osteoporosis as an old person’s disease and in fact age is certainly a risk factor. We see a sharp decline in bone density the first few years following menopause; a withdrawal from the “bone bank account.” But let me share a startling statistic. At the age of 20 we have 98% of the bone density we will ever achieve. We achieve Peak Bone Mass by age thirty when our bones have reached their maximum strength and density.
Factors affecting Peak Bone Mass include both Non-modifiable and Modifiable. Among the non-modifiable factors are gender (peak bone mass is higher in men), race (peak bone mass is higher in African Americans), and hormonal factors (early onset of menstruation and use of oral contraceptives tend to have higher peak bone mass). A family history of osteoporosis is another important factor.
Modifiable factors include nutrition (adequate calcium in the diets of young people), physical activity during the early years (specifically weight bearing and resistance exercises). Poor lifestyle behaviors (smoking, high alcohol intake, and sedentary lifestyle) have all been linked to low bone density in adolescents.
The American Physical Therapy Association website includes a section on “Container Baby Syndrome” (CBS). CBS is the name used to describe a range of physical, cognitive, and developmental conditions caused by a baby or infant spending too much time in containers such as baby carriers, strollers, and Bumpo seats. Bone mass can certainly be affected by reduced movement and weight bearing activities. Due to the SIDS scare, many young parents are fearful of allowing their children to spend time on their abdomens. Educate and share the “Supine to Sleep, Prone to Play” mantra.
The graph below shows a comparison of the Peak Bone Mass of males to females and to individuals with suboptimal lifestyle factors. You can see that the suboptimal group never catches up and enters the osteoporosis stage at around age 40.
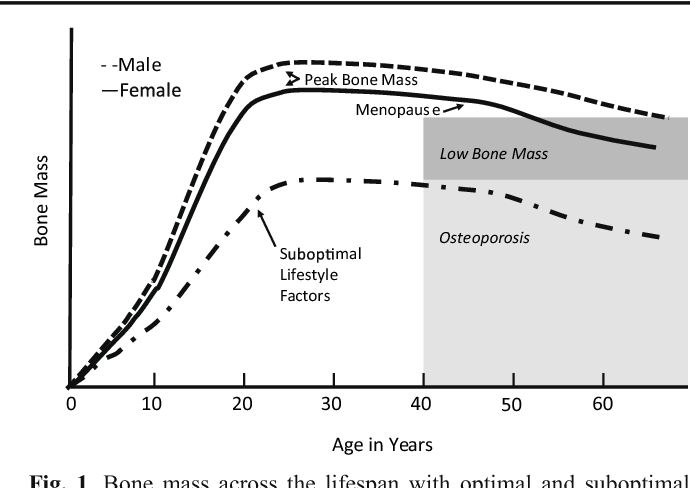
According to the Department of Human Services “Osteoporosis is a pediatric disease with geriatric consequences. Peak bone mass is built during our first three decades. Failure to build strong bones during childhood and adolescent years manifests in fractures later in life.”
What can we do?
• Start early: Encourage young children (and their parents) to move more and sit less.
• Spread the word: Speak to Young Mothers’ Clubs, Girl Scout Troops; anywhere to influence adolescent and teens about the importance of proper exercise and good nutrition.
• Write a blog: Share this information in newspapers, social media, and on your website. Get the word out! Because the bones of our future generation depend on it.
NIH Osteoporosis and Related Bone Diseases National Resource Center
Department of Human Services
American Physical Therapy Association