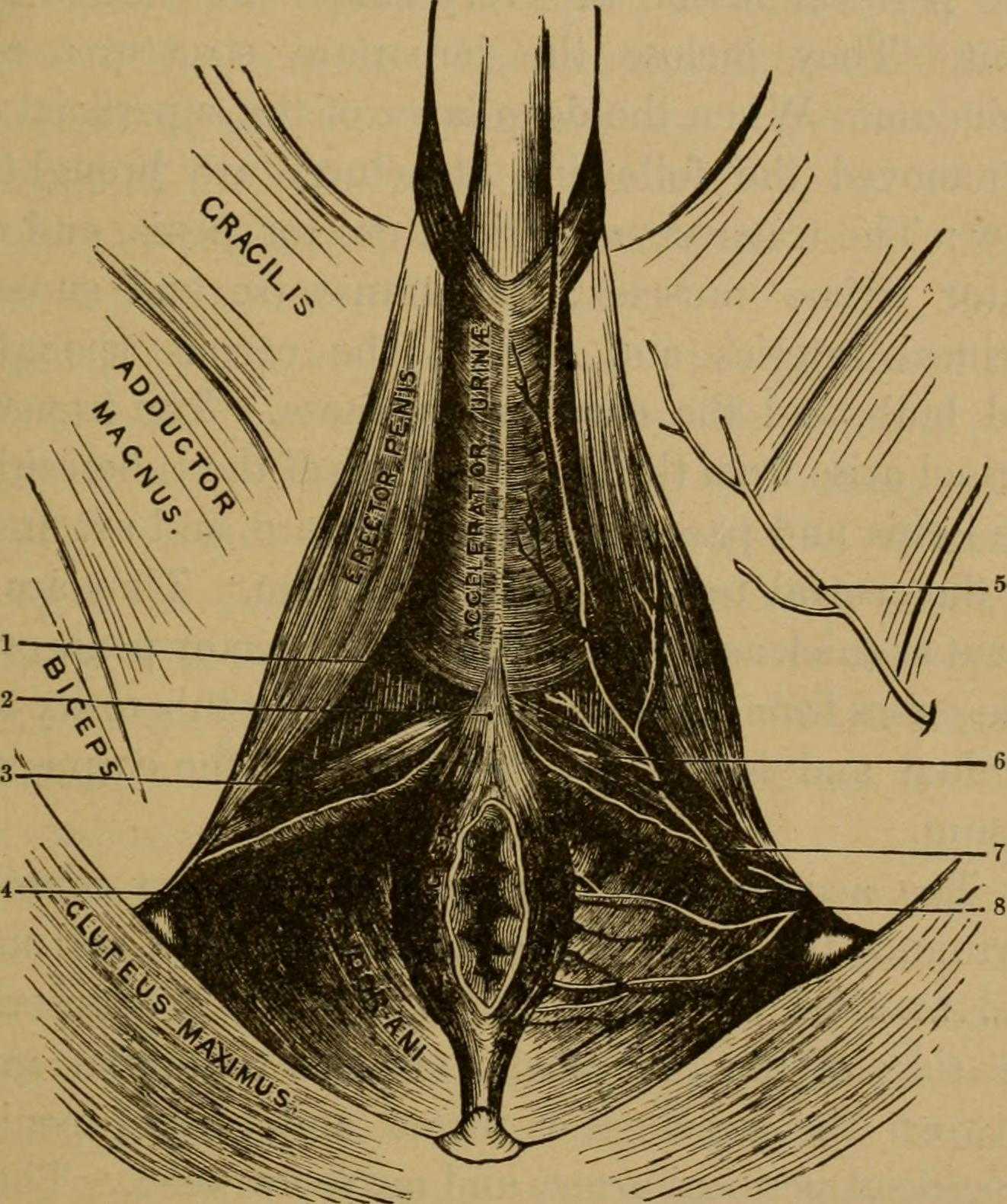
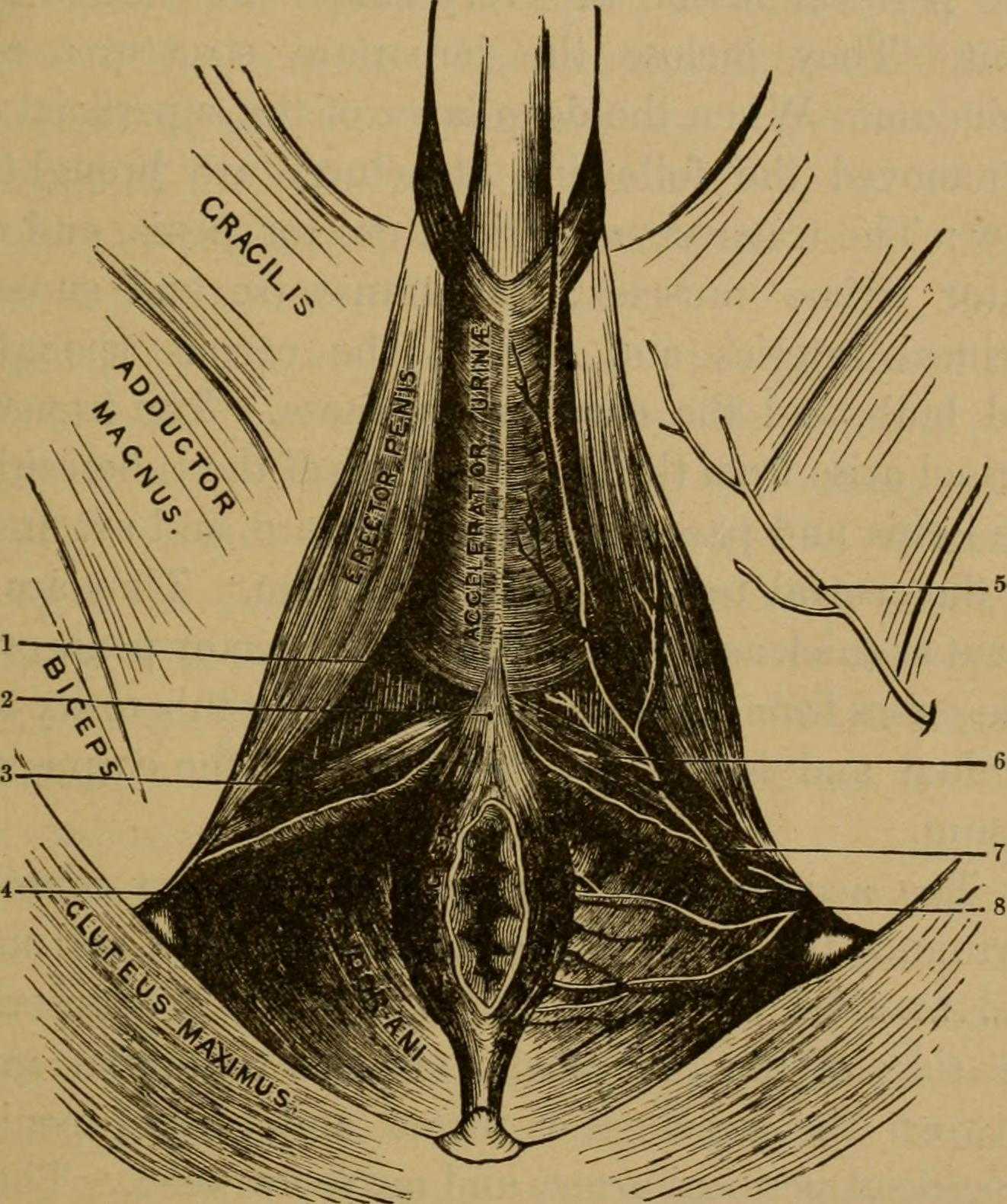
 Many therapists transition to treating men with the knowledge and training from female patients. When therapists apply this knowledge, for the most part, it works. When we spend some attention on learning what is a bit different, we might be drawn to the superficial muscles of the perineum. This old anatomy image does a wonderful job of "calling it like it is" or using anatomical terms that describe an action versus naming only the structure. In the image we are looking from below (inferior view) at the perineum and genitals. Just anterior to the anus we can see the anterior muscles within the urogenital triangle, with the base of the shaft of the penis located just anterior to (above in this image) the anus and perineal body. Notice that at the midline, we see muscle names the "accelerator urine". Modern textbooks refer to this muscle as the bulbocavernosus, or bulbospongiosus. Taking the name of accelerator urine, we can understand that this muscle will have an effect on aiding the body in emptying urine. It does this through rhythmic contractions, most often noted towards the end of urination, when the typical spurts of urine follow a more steady stream. This assistance with emptying can take place because the urethra is located within the lower part of the penis, the portion known as the corpus spongiosum. Because the bulbocavernosus muscle covers this part of the penis, and the inferior and lateral parts of the urethra are virtually wrapped within the bulbocavernosus, the muscle can have an effect on emptying the urine in the urethra.
Many therapists transition to treating men with the knowledge and training from female patients. When therapists apply this knowledge, for the most part, it works. When we spend some attention on learning what is a bit different, we might be drawn to the superficial muscles of the perineum. This old anatomy image does a wonderful job of "calling it like it is" or using anatomical terms that describe an action versus naming only the structure. In the image we are looking from below (inferior view) at the perineum and genitals. Just anterior to the anus we can see the anterior muscles within the urogenital triangle, with the base of the shaft of the penis located just anterior to (above in this image) the anus and perineal body. Notice that at the midline, we see muscle names the "accelerator urine". Modern textbooks refer to this muscle as the bulbocavernosus, or bulbospongiosus. Taking the name of accelerator urine, we can understand that this muscle will have an effect on aiding the body in emptying urine. It does this through rhythmic contractions, most often noted towards the end of urination, when the typical spurts of urine follow a more steady stream. This assistance with emptying can take place because the urethra is located within the lower part of the penis, the portion known as the corpus spongiosum. Because the bulbocavernosus muscle covers this part of the penis, and the inferior and lateral parts of the urethra are virtually wrapped within the bulbocavernosus, the muscle can have an effect on emptying the urine in the urethra.
Notice that if you follow the fibers of the accelerator urine muscle towards the top of the image, where the penis continues, you will notice fibers of the muscle wrapping around the sides of the penis. These fibers will continue as a fascial band that travels over the dorsal vessels of the penis. This allows the muscle to also have a significant action during sexual activity, in which blood flow (getting blood into, keeping blood in, and letting blood out of the penis) is paramount.
On either side of the penis we can see what is labeled the erector penis. As these muscles cover the legs, or crura which form the two upper parts of the penis, when the muscles contract, blood is shunted towards the main body of the penis. This of course helps with penile rigidity, as the smooth muscles in the artery walls of the penis allow blood to fill the spongy chambers.
Once we discuss the usual functions of these muscles, we can then imagine the dysfunctions potentially created by less than optimal activity. Consider the difficulty that these muscles will create in contracting or relaxing if they are either too weak, or too tense. These issues can create difficulty emptying well the urethra, often leading to post-void dribble. Blood flow and therefore penile rigidity with erections may be negatively impacted by inability of these muscles to contract or stay contracted, and blood flow leaving the penis may be impaired if the muscles cannot relax. When we work with patients who have genital pain, pelvic floor muscle weakness, dyscoordination, or tension, we can often improve sexual function, bladder emptying, and tasks that might otherwise be affected by pain.
If you are interested in learning more about how to assess and treat these muscles, you have one more opportunity this year to attend the 3-day Male Course instructed by Holly Tanner. Holly has been teaching this course for over 10 years when she co-wrote the first course with colleague and faculty member Stacey Futterman. The course has been updated and turned into a 3-day course to include more manual therapy techniques. Hurry to grab one of the remaining spots in the October 27-29 course in Grand Rapids!
At a hair salon, I once saw a plaque that declared, “I’m a beautician, not a magician.” This crossed my mind while reading research on radical prostatectomy, as knowing the baseline penile function of men before surgery seemed challenging. Restoring something that may have been subpar prior to surgery can be a daunting task, and it can cause discrepancies in results of clinical trials. Despite this, two recent studies reviewed the current and future penile rehabilitation approaches post-radical prostatectomy.

Bratu et al.2017 published a review referring to post-radical prostatectomy (RP) erectile dysfunction (ED) as a challenge for patients as well as physicians. They emphasized the use of the International Index of Erectile Function (IIEF) Questionnaire to establish a man’s baseline erectile function, which can be affected by factors such as age, diabetes, alcohol use, smoking habits, heart and kidney diseases, and neurological disorders. The higher the IIEF score preoperatively, the higher the probability of recovering erectile function post-surgery. The experience of the surgeon and the technique used were also factors involved in ED. Radical prostatectomy is a trauma to the pelvis that negatively affects oxygenation of the corpora cavernosum, resulting in apoptosis and fibrotic changes in the tissue, leading to ED. Minimally invasive surgery allows a significantly lower rate of post-RP ED with robot assisted radical prostatectomy (RARP) versus open surgery. The cavernous neurovascular bundles get hypoxic and ischemic regardless of the technique used; therefore, the authors emphasized early post-op penile rehabilitation to prevent fibrosis of smooth muscle and to improve cavernous oxygenation for the potential return of satisfactory sexual function within 12-24 months.
Clavell-Hernandez and Wang2017 [and Bratu et al., (2017)] reported on various aspects of penile rehabilitation after radical prostatectomy. The treatment with the most research to support its efficacy and safety was oral phosphodiesterase type-5 inhibitors (PDE5Is), which help relax smooth muscle and promote erection on a cellular level. Sildenafil, vardenafil, avanafil, and tadalafil have been studied, either used on demand or nightly. Tadalafil had the longer half-life and was considered to have the greatest efficacy. Nightly versus on-demand for any PDE5I was variable in its results. Intracavernosal injection (ICI) and intraurethral therapy using alprostadil for vasodilation improved erectile function, but it caused urethral burning and penile pain. Vacuum erection devices (VED) promoted penile erection via negative pressure around the penis, bringing blood into the corpus cavernosum. There was no need for intact corporal nerve or nitric oxide pathways for proper function, and it allowed for multiple erections in a day. Intracavernous stem cell injections provided a promising approach for ED, and they may be combined with PDE5Is or low-energy shockwave therapy. Ultimately, the authors concluded early penile rehabilitation should involve a combination of available therapies.
Restoring vascularity to healing tissue is a primary goal in rehabilitation, and the sooner the better. Disruption of cavernous nerves and penile tissue post-RP demands rehabilitation, and some methods have more supporting clinical evidence than others. Newer approaches require more exposure and clinical trials for efficacy and long term outcomes. Clinicians should pay attention to updated research and consider taking continuing education courses such as Post-Prostatectomy Patient Rehabilitation or Oncology and the Male Pelvic Floor.
Bratu, O., Oprea, I., Marcu, D., Spinu, D., Niculae, A., Geavlete, B., & Mischianu, D. (2017). Erectile dysfunction post-radical prostatectomy – a challenge for both patient and physician. Journal of Medicine and Life, 10(1), 13–18.
Clavell-Hernández, J., & Wang, R. (2017). The controversy surrounding penile rehabilitation after radical prostatectomy. Translational Andrology and Urology, 6(1), 2–11. http://doi.org/10.21037/tau.2016.08.14
Speaking with a runner friend the other day, I mentioned I was writing a blog on yoga for pelvic pain. She had the same reaction many runners do, stating she has doesn’t care for yoga, she never feels like she is tight, and she would hate being in one position for so long. Ironically, neither of us has taken a yoga class, so any preconceived ideas about it are null and void. I told her yoga is being researched for beneficial health effects, and one day we just might find ourselves in a class together!
 Saxena et al.2017 published a study on the effects of yoga on pain and quality of life in women with chronic pelvic pain. The randomized case controlled study involved 60 female patients, ages 18-45, who presented with chronic pelvic pain. They were randomly divided into two groups of 30 women. Group I received 8 weeks of treatment only with nonsteroidal anti-inflammatory medication (NSAIDS). Group II received 1 hour, 5 days per week, for 8 weeks of yoga therapy (asanas, pranayama, and relaxation) in addition to NSAIDS (as needed). Table 1 in the article outlines the exact protocol of yoga in which Group II participated. The subjects were assessed pre- and post-treatment with pain scores via visual analog scale score and quality of life with the World Health Organization quality of life-BREF questionnaire. In the final analysis, Group II showed a statistically significant positive difference pre and post treatment as well as in comparison to Group I in both categories. The authors concluded yoga to be an effective adjunct therapy for patients with chronic pelvic pain and an effective option over NSAIDS for pain.
Saxena et al.2017 published a study on the effects of yoga on pain and quality of life in women with chronic pelvic pain. The randomized case controlled study involved 60 female patients, ages 18-45, who presented with chronic pelvic pain. They were randomly divided into two groups of 30 women. Group I received 8 weeks of treatment only with nonsteroidal anti-inflammatory medication (NSAIDS). Group II received 1 hour, 5 days per week, for 8 weeks of yoga therapy (asanas, pranayama, and relaxation) in addition to NSAIDS (as needed). Table 1 in the article outlines the exact protocol of yoga in which Group II participated. The subjects were assessed pre- and post-treatment with pain scores via visual analog scale score and quality of life with the World Health Organization quality of life-BREF questionnaire. In the final analysis, Group II showed a statistically significant positive difference pre and post treatment as well as in comparison to Group I in both categories. The authors concluded yoga to be an effective adjunct therapy for patients with chronic pelvic pain and an effective option over NSAIDS for pain.
In the Pain Medicine journal, Huang et al.2017 presented a single-arm trial attempting to study the effects of a group-based therapeutic yoga program for women with chronic pelvic pain (CPP), focusing on severity of pain, sexual function, and overall well-being. The comprehensive program was created by a group of women’s health researchers, gynecological and obstetrical medical practitioners, yoga consultants, and integrative medicine clinicians. Sixteen women with severe pelvic pain of at least 6 months’ duration were recruited. The group yoga classes focused on lyengar-based techniques, and the subjects participated in group classes twice a week and home practice 1 hour per week for 6 weeks. The Impact of Pelvic Pain (IPP) questionnaire assessed how the participants’ pain affected their daily life activities, emotional well-being, and sexual function. Sexual Health Outcomes in Women Questionairre (SHOW-Q) offered insight to sexual function. Daily logs recorded the women’s self-rated pelvic pain severity. The results showed the average pain severity improved 32% after the 6 weeks, and IPP scores improved for daily living (from 1.8 to 0.9), emotional well-being (from 1.7 to 0.9), and sexual function (from 1.9 to 1.0). The SHOW-Q "pelvic problem interference" scale also improved from 53 to 23. The multidisciplinary panel concluded they found preliminary evidence that teaching yoga to women with CPP is feasible for pain management and improvement of quality of life and sexual function.
Whatever treatment we provide for our patients, we need to consider the individual and their often biased opinions or perceptions. Providing research and educating each patient on the efficacy behind the proposed therapy will likely impact their outcome. The Yoga for Pelvic Pain course can enhance a clinician’s understanding and allow them to better implement a potentially life-changing therapy for their clients.
Saxena, R., Gupta, M., Shankar, N., Jain, S., & Saxena, A. (2017). Effects of yogic intervention on pain scores and quality of life in females with chronic pelvic pain. International Journal of Yoga, 10(1), 9–15. http://doi.org/10.4103/0973-6131.186155
Huang, AJ, Rowen, TS, Abercrombie, P, Subak, LL, Schembri, M, Plaut, T, & Chao, MT. (2017). Development and Feasibility of a Group-Based Therapeutic Yoga Program for Women with Chronic Pelvic Pain. Pain Medicine. http://doi.org/10.1093/pm/pnw306
In the world of pelvic health, we are constantly meeting patients who are surprised to learn about the scope of what we do. Oftentimes, it is because we mention the pelvic muscles’ roles in sexual health that a patient will offer up symptoms with their sexual health, or ask a few more questions. Outside of pelvic health professionals asking about sexual function, do men bring up these issues with anyone? Not usually. In Fisher and colleagues 2-part “Strike up a conversation” study (2005), the authors reported that men who have erectile dysfunction (ED) are worried about their partner’s reaction, don’t want to admit to having a chronic problem, and frankly, just don’t even know where to start. Unfortunately, the partners of men who have ED have the same concerns. In addition, partners are worried about bringing it up and “making their partners feel worse about it.” When men did bring up sexual concerns with their physician, although they reported feeling nervous and embarrassed, they also reported feeling hopeful and relieved.
 This issue was highlighted in a recent interview and article published on National Public Radio. The article shares that for war veterans, sexual intimacy is often affected, and yet, is often ignored. A Marine who suffered PTSD after a head injury and shrapnel to the head and neck describes how he had to go to the doctor several times just to work up the nerve to ask for help for his sexual dysfunction. He also shared how it was difficult to talk about “…because it contradicts a self-image so many Marines have.” Apparently you don’t have to be a Marine to feel the same intense pressure related to talking about sexual issues. I have spent more time in the past year trying to better understand why men don’t discuss these issues, with a best friend or partner, and each time, my question of “what would that be like if you brought it up?” is met with near bewilderment, as if revealing this issue were akin to revealing your deepest, darkest secret. Apparently, it is. Telling a buddy you have erectile dysfunction, for men, seems to be like showing your enemy where the chink in your armor is, or like setting yourself up to be the center of every “getting it up” joke for the remainder of your life.
This issue was highlighted in a recent interview and article published on National Public Radio. The article shares that for war veterans, sexual intimacy is often affected, and yet, is often ignored. A Marine who suffered PTSD after a head injury and shrapnel to the head and neck describes how he had to go to the doctor several times just to work up the nerve to ask for help for his sexual dysfunction. He also shared how it was difficult to talk about “…because it contradicts a self-image so many Marines have.” Apparently you don’t have to be a Marine to feel the same intense pressure related to talking about sexual issues. I have spent more time in the past year trying to better understand why men don’t discuss these issues, with a best friend or partner, and each time, my question of “what would that be like if you brought it up?” is met with near bewilderment, as if revealing this issue were akin to revealing your deepest, darkest secret. Apparently, it is. Telling a buddy you have erectile dysfunction, for men, seems to be like showing your enemy where the chink in your armor is, or like setting yourself up to be the center of every “getting it up” joke for the remainder of your life.
The bottom line is that we can be part of the solution to this problem, because men must be certain that their medical provider knows about any emerging or worsening erectile dysfunction. Loss of libido, or changes in erectile function can be associated with heart issues, with diabetes, or with other major medical concerns. Research such as the referenced “strike up a conversation study” has demonstrated that health care providers or partners may positively influence a patient’s access to care. Once medical evaluation has been completed, the role of the pelvic health provider is critical in improving sexual health for men with dysfunction. If you are interested in learning more about the role of the pelvic health provider for erectile dysfunction or pain related to sexual function, the Male Pelvic Health continuing education course will be offered 3 times this year through the Herman & Wallace Pelvic Rehabilitation Institute. Your next opportunity to learn about urinary and prostate conditions, male pelvic pain, sexual health and dysfunction is next month in Portland, Oregon.
Chang, A. (2016). For veterans, trauma of war can persist in struggles with sexual intimacy. Retrieved from http://www.npr.org/sections/health-shots/2017/01/01/507749611/for-veterans-trauma-of-war-can-persist-in-struggles-with-sexual-intimacy
Fisher, W. A., Meryn, S., Sand, M., Brandenburg, U., Buvat, J., Mendive, J., ... & Strike Up a Conversation Study Team. (2005). Communication about erectile dysfunction among men with ED, partners of men with ED, and physicians: The Strike Up a Conversation Study (Part I). The journal of men's health & gender, 2(1), 64-78.
Fisher, W. A., Meryn, S., Sand, M., & Strike up a Conversation Study Team. (2005). Communication about erectile dysfunction among men with ED, partners of men with ED, and physicians: the Strike Up a Conversation study (Part II). The journal of men's health & gender, 2(3), 309-e1.
Unfortunately one of the most common things we hear in pelvic rehab is “I hope you can help me, you’re my last hope.” In severe cases, this translates to the patient having little hope of surviving their life with pelvic pain. In severe but not necessarily life-threatening cases, being a patient’s last hope can also mean “please help me have sex in my relationship or my partner is going to leave me.” This situation places a lot of pressure on the patient and also on the therapist. How long did it take this patient to find her way to pelvic rehab? Research tells us that most women have been through multiple physicians, under- or misdiagnosed, and that many have failed attempts at intervention with medications or procedures.
 It’s clear to women that they are being judged when they go to medical appointments complaining of pelvic pain or pain with intercourse. Although it seems really old school to hear that a provider said “It’s all in your head.” or “How much do you like your partner?” or “Well, you’re getting older, sex isn’t that important.” these dismissive phrases are still used. A study by Nguyen et al., 2013 reported that women who reported chronic pain were more likely to perceive being stereotyped by doctors and others. Interestingly, among the group of women who had chronic vulvar pain, the women who sought care for their condition reported feeling more stigmatized. Because the support a woman perceives may influence her willingness to seek out help for chronic vulvar pain, we need to keep educating our peers, the public, and the providers about the real challenges women face, and the power of rehabilitation in overcoming those challenges.
It’s clear to women that they are being judged when they go to medical appointments complaining of pelvic pain or pain with intercourse. Although it seems really old school to hear that a provider said “It’s all in your head.” or “How much do you like your partner?” or “Well, you’re getting older, sex isn’t that important.” these dismissive phrases are still used. A study by Nguyen et al., 2013 reported that women who reported chronic pain were more likely to perceive being stereotyped by doctors and others. Interestingly, among the group of women who had chronic vulvar pain, the women who sought care for their condition reported feeling more stigmatized. Because the support a woman perceives may influence her willingness to seek out help for chronic vulvar pain, we need to keep educating our peers, the public, and the providers about the real challenges women face, and the power of rehabilitation in overcoming those challenges.
Vulvodynia is a common pelvic pain condition, and one that typically is associated with painful intercourse, or dyspareunia. (Arnold et al., 2006) It's estimated that by the age of 40, as many as 8% of women will have or have had a diagnosis of vulvodynia (Harlow et al., 2014), and this is clearly a significant quality of life issue.
Physical therapy has been shown to be successful in treating vulvar pain and pain with intercourse, including as part of a multidisciplinary approach. (Brotto et al., 2015) That's why Herman & Wallace is so eager to help empower more therapists to help patients live a life free of vulvar pain and dyspareunia. You can learn more about our courses and other resources at https://www.hermanwallace.com/continuing-education-courses.
Arnold, L. D., Bachmann, G. A., Kelly, S., Rosen, R., & Rhoads, G. G. (2006). Vulvodynia: characteristics and associations with co-morbidities and quality of life. Obstetrics and gynecology, 107(3), 617.
Brotto, L. A., Yong, P., Smith, K. B., & Sadownik, L. A. (2015). Impact of a multidisciplinary vulvodynia program on sexual functioning and dyspareunia. The journal of sexual medicine, 12(1), 238-247.
Harlow, B. L., Kunitz, C. G., Nguyen, R. H., Rydell, S. A., Turner, R. M., & MacLehose, R. F. (2014). Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. American journal of obstetrics and gynecology, 210(1), 40-e1.
Nguyen, R. H., Turner, R. M., Rydell, S. A., MacLehose, R. F., & Harlow, B. L. (2013). Perceived stereotyping and seeking care for chronic vulvar pain. Pain Medicine, 14(10), 1461-1467.
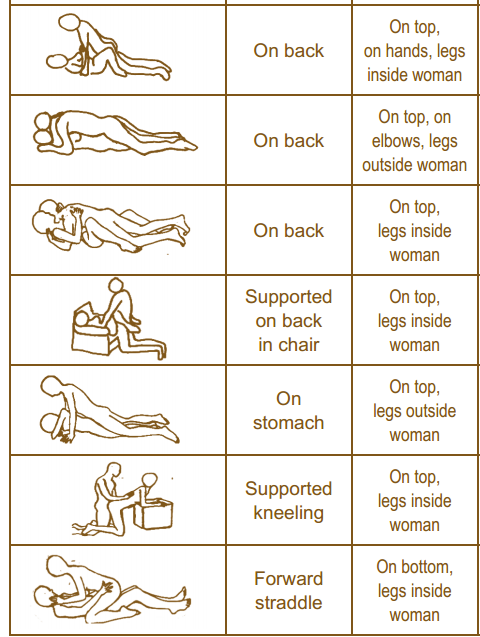
As pelvic rehab providers, we may find it easy to talk to our patients about sexual function when it is a patient who comes to us with a sexually relevant problem or directly related diagnosis, such as dyspareunia or limited intercourse participation due to prolapse symptoms. However, are we talking to our other patients about sexual function? Are they talking to us about it? What about our orthopedic patients - are we routinely asking them about how their problem can affect their sexual function? Some recent studies found that 32% of patients planning to undergo a Total Hip Replacement (THR) had reported concerns about difficulties with sexual activityBaldursson, Wright. Was the fact that they could not participate in sexual activity due to the hip pain a driving factor when considering the hip replacement, maybe? Just because a patient doesn’t ask, does not mean that they don’t want to know how their orthopedic injury affects sexual function. Resuming sexual function is an important quality of life goal that is included on few outcome assessment forms, however, there are some that address this subject such as the Oswestry Disability Index for Low Back Pain. Discussion of this topic should be addressed more routinely than it is.
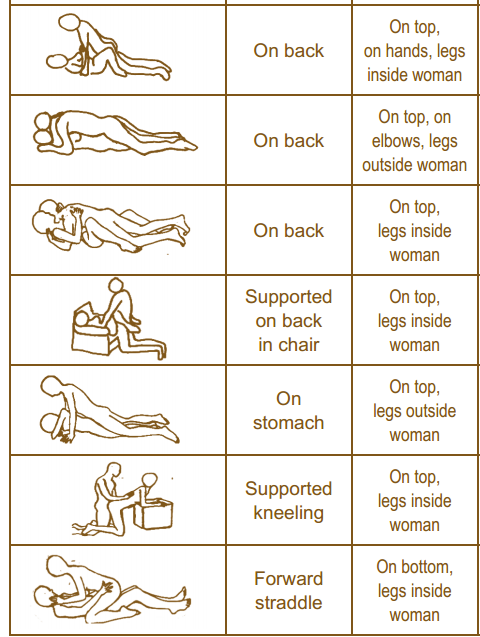
It is important to remember that just because a patient is not in our office for a directly related sexual problem, it is still important to at least open up the dialogue about sexual health. One study in 2013 had patients complete a questionnaire on their sexual function after undergoing a total hip or total knee replacement and 90% reported improved overall sexual functionRathod, et al.. We should try to make the conversation part of our routinely delivered information for a total joint replacement, for example when telling our THR patient, you can resume driving at 3-6 weeks (or when cleared by surgeon), you have Range of Motion precautions of avoiding internal rotation, hip flexion past 90 degrees, and hip adduction (crossing the legs) for the length specified by your surgeon (if it was a posterior approach THR), and you can resume sexual function at 3-6 weeks (or when cleared by the surgeon), or when you feel ready after that. It is important to give the patient some kind of guideline about when they can expect to resume sexual activity, however, always emphasize that it should be resumed when the patient is ready so they don’t feel pressured before they are ready. Also as pelvic rehab practitioners we can offer them guidance about what positions may be best for them when returning to sexual activity to put less strain on the prosthesis and hip as well as help them be comfortable. To continue with our example for THR (posterior approach) their precautions are likely to restrict hip flexion past 90 degrees, hip internal rotation, and adduction, so for a man or woman following THR lying on their back would be a safe position.
As physical therapists it is our job to provide guidance. Instead of telling people what not to do, helping them find a safe way to do things they want to do to maintain function should always be our goal. Sexual activity participation is definitely an important function for quality of life that is often overlooked and not discussed, so talk to your patient about it, they will likely appreciate it.
One useful tool to learn more about positioning for sexual activity is the Herman & Wallace product “Orthopedic Considerations for Sexual Activity.” It provides a great list of positions with pros and cons of each position, and is a helpful visual aid for your patients to help them return to sexual function safely with consideration of their respective injuries.
Baldursson, H., & Brattström, H. (1979). Sexual difficulties and total hip replacement in rheumatoid arthritis. Scandinavian journal of rheumatology, 8(4), 214-216.
Wright, J. G., Rudicel, S. A. L. L. Y., & Feinstein, A. R. (1994). Ask patients what they want. Evaluation of individual complaints before total hip replacement. Journal of Bone & Joint Surgery, British Volume, 76(2), 229-234.
Rathod PA, Deshmuka AJ, Ranawat AS, Rodriguez JA. Sexual function improves significantly following total hip and knee arthroplasty: a prospective study. Program and abstracts of the 2013 meeting of the American Academy of Orthopedic Surgeons; March 19-23, 2013; Chicago, Illinois. Poster P023.
 Sexual dysfunction is a common negative consequence of Multiple Sclerosis, and may be influenced by neurologic and physical changes, or by psychological changes associated with the disease progression. Because pelvic floor muscle health can contribute to sexual health, the relationship between the two has been the subject of research studies for patients with and without neurologic disease. Researchers in Brazil assessed the effects of treating sexual dysfunction with pelvic floor muscle training with or without electrical stimulation in women diagnosed with multiple sclerosis (MS.) Thirty women were allocated randomly into 3 treatment groups; 20 women completed the study. All participants were evaluated before and after treatment for pelvic floor muscle (PFM) function, PFM tone, flexibility of the vaginal opening, ability to relax the PFM’s, and with the Female Sexual Function Index (FSFI). Rehabilitation interventions included pelvic floor muscle training (PFMT) using surface electromyographic (EMG) biofeedback, neuromuscular electrostimulation (NMES), sham NMES, or transcutaneous tibial nerve stimulation (TTNS). The treatments offered to each group are shown below.
Sexual dysfunction is a common negative consequence of Multiple Sclerosis, and may be influenced by neurologic and physical changes, or by psychological changes associated with the disease progression. Because pelvic floor muscle health can contribute to sexual health, the relationship between the two has been the subject of research studies for patients with and without neurologic disease. Researchers in Brazil assessed the effects of treating sexual dysfunction with pelvic floor muscle training with or without electrical stimulation in women diagnosed with multiple sclerosis (MS.) Thirty women were allocated randomly into 3 treatment groups; 20 women completed the study. All participants were evaluated before and after treatment for pelvic floor muscle (PFM) function, PFM tone, flexibility of the vaginal opening, ability to relax the PFM’s, and with the Female Sexual Function Index (FSFI). Rehabilitation interventions included pelvic floor muscle training (PFMT) using surface electromyographic (EMG) biofeedback, neuromuscular electrostimulation (NMES), sham NMES, or transcutaneous tibial nerve stimulation (TTNS). The treatments offered to each group are shown below.
| sEMG biofeedback | Sham NMES | Intravaginal NMES | TTNS | |
| Group 1 (n=6) | X | X | ||
| Group 2 (n=7) | X | X | ||
| Group 3 (n=7) | X | X |
The following factors made up the inclusion criteria for the study: age at least 18 years, diagnosis of relapsing-remitting MS, and a 4 month history of stable symptoms. All of the participants were sexually active and were found to be able to contract pelvic floor muscles correctly. Group 1 patients were treated with “sham” electrical stimulation using surface electrodes placed over the sacrum at a pulse width of 50 ms and a frequency of 2 Hz. Patients in Group 2 used an internal (vaginal) electrode at 200 ms at 10 Hz. Group 3 were given transcutaneous tibial nerve stimulation at 200 ms and 10 Hz. All groups followed these treatments with pelvic floor muscle exercises using a vaginal sensor and biofeedback.
The authors concluded that pelvic floor muscle training alone or in combination with intravaginal neuromuscular electrostimulation or transcutaneous tibial nerve stimulation is effective in treating sexual dysfunction in women who have MS. Improvements were noted in these groups in sexual arousal, vaginal lubrication, satisfaction, and in the Female Sexual Function Index. While the numbers in the respective intervention groups is not large enough to determine the best option for patients who have multiple sclerosis, the research reminds us that neurostimulation in conjunction with pelvic muscle training may be very valuable.
Research published in a Nursing journal highlights the need for pelvic rehab providers to assess for sexual dysfunction in women before, during, and after pregnancy. 200 women were interviewed about their return to sexual activity after pregnancy and childbirth, and the results demonstrate that women can (and do) have limitations in their sexual function around the entire peripartum period.
![By Nina Matthews (Flickr: head to head) [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/thumb/8/86/Silhouette_or_a_pregnant_woman_and_her_partner-14Aug2011.jpg/492px-Silhouette_or_a_pregnant_woman_and_her_partner-14Aug2011.jpg) The results of the survey concluded that before pregnancy 33.5% of the women reported sexual dysfunction, and this number increased to 76% during pregnancy, and to 43.5% following delivery. The types of sexual dysfunction included dyspareunia, vaginismus, and decreased desire and orgasm. The authors of the study correlated dysfunctions with Catholic religion, vaginal delivery without suture, dyspareunia during pregnancy, vaginismus before pregnancy, and with working more than 8 hours per day.
The results of the survey concluded that before pregnancy 33.5% of the women reported sexual dysfunction, and this number increased to 76% during pregnancy, and to 43.5% following delivery. The types of sexual dysfunction included dyspareunia, vaginismus, and decreased desire and orgasm. The authors of the study correlated dysfunctions with Catholic religion, vaginal delivery without suture, dyspareunia during pregnancy, vaginismus before pregnancy, and with working more than 8 hours per day.
The information collected in this study raise important points with a variety of topics related to sexual function. How we as providers aim to address these topics with women can have a critical impact on the health of a woman and her family. Let’s look at some action items this research can lead us to:
- Include methods of asking about sexual health in your written and verbal evaluations
- Educate colleagues about bringing up sexual health with women throughout the lifespan
- Avoid assuming that a woman would not want to be sexually active during pregnancy
- Recognize that personal beliefs (including religion) play a role in sexual health, and that a patient can be encouraged to talk to her spiritual advisor or a trusted professional if concerns arise
- Talk about healthy workloads, options for modifications at work, and strategize with patients about rest breaks or decreasing work hours if financially able
This type of research can lead to many more questions, such as how religious beliefs impact sexual function during pregnancy, what the effect of physiologic changes versus fatigue can have on libido, or if women who have intervention for dyspareunia prior to pregnancy have decreased sexual dysfunction after pregnancy. Most of us were not instructed in how to dialog about these types of questions, and of course some topics, like religion, are potentially very sensitive to bring up with our patients.
If you would like more practical advice about the clinical implications for sexual medicine across the lifespan and among all genders, consider a trip to San Diego this November to learn from Herman & Wallace co-founder Holly Herman at Sexual Medicine for Men and Women: A Rehabilitation Perspective!
Holanda, J. B. D. L., Abuchaim, E. D. S. V., Coca, K. P., & Abrão, A. C. F. D. V. (2014). Sexual dysfunction and associated factors reported in the postpartum period. Acta Paulista de Enfermagem, 27(6), 573-578.
Peyronie’s disease is a condition in which there are fibrotic plaques (sometimes calcified) that can cause a curvature in the penis, most notable during erection. Pain as well as urinary and sexual dysfunction may occur with Peyronie's disease. Increased attention has been given in recent years to the relationship between male hormones, erectile dysfunction, and Peyronie's disease. According to the Mayo Clinic, testosterone, the predominant hormone affecting male physical characteristics, peaks during adolescence and early adulthood. Testosterone gradually decreases about 1% per year once a man reaches age 30-40. Some men experience symptoms from the decline in testosterone and these symptoms can include decreased sexual function, sleep disturbances changes in bone density and muscle bulk, as well as changes in cognition and depression. Because other factors and conditions can cause similar symptoms, patients with any of these changes should talk to their medical provider to rule out diabetes, thyroid dysfunction, depression, sleep apnea, and medication side effects, according to Mayo.
 In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
The larger question about Peyronie’s disease is what a patient can do to improve the symptoms of the condition. Therapists who treat male patients are increasingly interested in this question, and many are working with their patients to address the known soft tissue dysfunction. Interventions may include teaching patients to perform soft tissue mobilizations and stretches to the restricted tissue, and educating the patient in what the available literature tells us about rehabilitation of this condition. Hopefully, as male pelvic rehabilitation continues to grow in popularity, more therapists will contribute case studies and participate in higher levels of research so that more men can add conservative care of Peyronie’s to their list of treatment options.
To learn more about what the literature tells us about Peyronie’s and other male pelvic rehabilitation conditions, the Male Pelvic Floor continuing education course is taking place in Seattle in November, and you won't want to miss it!
The research on pelvic pain and specifically on sexual dysfunction has focused on heterosexual women, leaving a large gap in the clinically-based evidence. A study published last year in the Journal of Sex & Marital Therapy aimed to narrow this gap by studying the characteristics of vulvar pain in women in a variety of relationships. The associations between qualities such as love and communication were evaluated in relation to the participants' perceptions of how pain influenced their relationships. Within the research report, the authors establish that pelvic pain commonly causes pain and limitation with sexual function, and that queer women (defined in their work as women who identify as something other than heterosexual) also experience pain with sexual function.
"Of the 839 women, 31% reported genital pain, with 12% of the women with genital pain in a same-sex relationship, 67% in a mixed-sex relationship, and 21% being single"
The women in the study provided information about demographics, experiences of genital pain and pain characteristics. They completed surveys including the Dyadic Trust Scale (measures trust in a close relationship), the Rubin Love Scale (assesses level of romantic love), and the Communication Subscale of Evaluation and Nurturing Relationship Issues, Communication and Happiness Marital Satisfaction Scale (measures level of communication). Participants' average age was 25, and of the 77% who were in a relationship, most (60%) were in a mixed-sex relationship. Average length of relationships was 3 years, with nearly 84% of the women being white with some level of higher education.
Of the 839 women, 31% reported genital pain, with 12% of the women with genital pain in a same-sex relationship, 67% in a mixed-sex relationship, and 21% being single. Of the 260 women reporting genital pain, 39% identified as heterosexual, 15% identified as lesbian, and 46% identified as bisexual. The most common pain locations reported were inside the vagina (48%), in the pelvis or abdomen (45%), at the vaginal opening (39%), and 21% of the women reported global vulvar pain. From the data, the authors also report that women in same-sex relationships were likely to report that tampon insertion was painful.
The authors point out that challenges to healing for women who identify outside of heterosexual are many, and can include:
- homonegativity and heterosexism at a medical provider's office
- failure to disclose sexual identity due to fear of negative interaction
- fear that a symptom is linked to a sexual practice
- being in an unsupportive relationship or having poor adjustment within relationship
The limited research on sexual pain in women in same sex relationships has highlighted strengths within the relationships as well. Women in same sex relationships have been noted to have more effective communications skills, which may in turn foster better understanding of conditions such as pelvic pain. The authors concluded that while the characteristics of vulvar pain were similar across groups, there was a difference in the perception of pain impact on relationships. Better communication for same-sex couples and more love for mixed-sex couples was positively associated with impact on relationship. Of the women reporting pain, nearly half of the participants indicated that the pain negatively impacted their relationship in general, and 64% reported that the pain interfered with sexual health.
This type of research provides insight for pelvic rehabilitation clinicians and adds to our data base of considerations when working with women. The truth is that most of us were not provided adequate training in how to evaluate and manage issues of sexual health, nor were we provided with the means to value our own sexuality as a normal and healthy part of being. This lack requires education to fill in our own gaps, so that we can be of best service to our patients. If we are able to be present and nonjudgmental, our patients can in turn share openly and provide information that can direct best care. Holly Herman, co-founder of the Pelvic Rehabilitation Institute, offers a 2-day course in Sexual Medicine, so that providers can learn more about healthy sexuality as well as how to dialog with our patients.