
In 2013, H&W debuted a brand new course on Rehabiltation for the Breast Oncology Patient. This coming year, we are thrilled to be offering this course on the West Coast, in San Diego in April. Pelvic Rehab Report talked to course author and instructor Susannah Haarmann, PT, CLT, WCS about what she learned from teaching this course for the first time and what she looks forward to sharing with participants this year.
PRR: You developed and started teaching this course for the first time in 2013. What did you learn from your first time teaching this course?
SH: I learned that the breadth of topics that ought to be covered in order to present a holistic approach to rehabilitation and breast oncology is gigantic! I was inspired to teach this course because, from my perspective, in most clinics and hospitals, the vast concerns of breast survivors regarding physical well-being and quality of life are not being addressed. I turned to mentors for guidance, but their knowledge had holes. I probed the research, but the information pertaining to rehabilitation seemed disjointed. I sought out continuing education, however, the topics covered were not as complete and detailed as I would have preferred.
In summary, I learned teaching in 2013 that I bit off a lot to chew! Feedback from the course was largely optimistic, however, I have made huge modifications. The course material has been reorganized from a 3-day to 2-day course. Although the course is still steeped in research, the content has been stream-lined. I have also included more labs with pertinent case scenarios for didactic learning and skills development.
Were there any surprises? How did feedback from participants inform the evolution of this course as you prepare to teach in 2014?
I was surprised by the variability in course participants! There were physical therapists and occupational therapists, women’s health practitioners, travelling physical therapists and certified lymphedema therapists, outpatient practitioners and acute care therapists…the perspectives that we had during the debut course was incredible! I treat breast cancer survivors on an outpatient basis, but feedback from the acute care therapists helped me address post-surgical and inpatient issues. Furthermore, I am a certified lymphedema therapist (CLT) trained by the Norton School of Lymphedema, however, there were also Leduc trained CLTs present as well. Interacting with these practitioners broadened my awareness of lymphedema treatment approaches.
Finally, the labs included in this course are broad in scope; they require us to pull from our basic knowledge of cardiopulmonary, integumentary and neuromuscular systems knowledge. Many participants were glad to sharpen their skills in orthopedic testing of the shoulder or vitals assessment and interpretation. In order to be experts, sometimes we have to perfect the basics- Be prepared to call on your generalist wisdom!
What were the most common questions asked by participants during the course? How does the course address frequent questions/misconceptions therapists might have about this topic?
I would say that many of the therapists were inspired by the idea of a health care team that became familiar with the client from the time of diagnosis through the ‘re-entry’ phase into long-term survivorship. Participants wanted to know how to facilitate the practice of the prospective surveillance model in their communities and develop relationships with physicians.
I think that a frequent misconception about breast oncology rehabilitation is that it just addresses lymphedema. In most cases, all bodily systems are affected by treatments related to breast cancer; some rear their heads during the acute phase, whereas other side effects become noticeable with the aging process. We as rehabilitation professionals are able to work with various body systems across the continuum of care. If you take this course be prepared to learn about treating post-surgical side effects such as lymphatic cording, muscle imbalances and post-mastectomy pain syndrome. Get ready to dig into treating side effects of chemotherapy such as peripheral neuropathy, fatigue, osteoporosis and dyspareunia. Learn about rehabilitation considerations pertaining to radiation such as integumentary and potential cardiopulmonary changes. But, we won’t stop there! Behind every ‘body’ is a person; you will also be exposed to what the research says about how medical interventions can affect the psyche and how methods such as mindfulness based stress reduction can not only improve personal well-being, but also affect cancer outcomes.
Want to learn more from Susannah? Check her out in San Diego, April 12-13!
A recently published review about peripartum management of gestational diabetes mellitus (GDM) confirms that use of recommended guidelines, testing, and follow-up "…seems suboptimal at best and arbitrary at worst." Despite the fact that during pregnancy, a mother and her fetus experience health risks related to gestational diabetes, screening remains low across countries and study settings. Once a woman is diagnosed with GDM, she is at risk for developing postpartum Type II diabetes. The necessary follow-up testing is also not consistently completed, and many new mothers are challenged by recommended lifestyle modifications.
Unfortunately, women who develop gestational diabetes may not have any symptoms. Medical providers typically screen for GDM with an oral glucose tolerance test between weeks 24-28, or earlier if risk factors are present. According to Medline Plus, excessive thirst or increased urination may be present as a symptom. Blurred vision, fatigue, weight loss despite increase in appetite, frequent infections, or nausea and vomiting may also occur. A common challenge of diagnosing women with disease conditions during the peripartum period is that symptoms such as fatigue, nausea, or changes in hunger and thirst may occur as a typical part of pregnancy or the postpartum period, so a woman may not report all symptoms to her provider. Risk factors for patients in developing gestational diabetes can include age over 25, having a family history of diabetes, giving birth to a child weighing greater than nine pounds, having high blood pressure, or a high body mass index (BMI) prior to pregnancy.
What is the potential impact for pelvic rehabilitation providers who work with women during the prenatal or postpartum period? Because women who develop GDM often have larger babies, there may be an increased risk of a cesarean section, or injury to the pelvis during childbirth. While pregnant, a woman with GDM may have elevated blood pressures. In the postpartum period, the risk for developing Type II diabetes increases, yet may not develop for 5-10 years. Medical providers and patients each experience barriers to screening and follow-up, as described in the open access article available here. Barriers for health care providers can include not seeing the patient during the screening period, not having appropriate resources available for testing, lack of coordination between different providers, and patient refusal of the test. Even if a woman is identified early as having gestational diabetes, and is informed about appropriate diet and exercise modifications that will reduce the risk of developing Type II diabetes in the postpartum period, poor self-efficacy and social support may limit a woman from achieving her desired goals.
As is often asked regarding review of articles in this blog, what is the role of the pelvic rehabilitation provider? If a rehab provider is aware of the risks for the condition, we can respectfully inquire if the patient has been screened, and encourage her to follow-up during the 24-28 week window as needed. If a woman complains of fatigue or blurred vision, or changes in her habits that "don't seem right" to the provider or the patient, a referral to the managing medical provider can be made. During the postpartum period, providing community education, health and wellness screening, or clinical screening can be completed. It is necessary for rehab therapists to assist in identifying barriers to exercise and proper nutrition, and coordinate with a patient's resources as able. Having a support team such as nutritionists, exercise therapists, and social services can have a positive impact, as many women are focused on the daily acts of raising a child and have too little focus on their own health.
If you are interested in learning more about the prenatal period, the postpartum recommendations for gestational diabetes, and exercise prescription, find out which of the Perinatal Series of continuing education courses fits into your schedule. (These courses do not need to be taken in any particular order. )Therapists will find a blend of evidence-based support related to peripartum issues as well as evaluation and intervention techniques to apply in the clinic. The next Care of the Pregnant Patient takes place in April in Maywood (near Chicago Care of the PostpartumPatient is in Oakland, CA, in March, and the next Peripartum Special Topics course happens in Texas in October.
Throughout the Guidelines on Chronic Pelvic Pain created by the European Association of Urology, the recognition of anxiety and depression as a concomitant symptom of chronic pelvic pain is made. Various types of pelvic dysfunctions have been demonstrated to have an association with anxiety and depression, including urethral pain, chronic pelvic pain, anorectal disorders, and sexual dysfunction. While a first line of medical treatment for patients who complain of neuropathic pain type, according to the Guidelines, is the prescribing of antidepressants, there are other interventions identified in the literature for alleviating anxiety and stress related to chronic pain. One of the studied interventions for pain, anxiety, and stress is yoga.
In a systematic review and meta-analysis for yoga and low back pain (which is also a common comorbidity of pelvic pain) yoga was found to have "…strong evidence for short-term effectiveness and moderate evidence for long-term effectiveness…" and the study concludes that yoga can be recommended for patients who have chronic low back pain. In this review of ten randomized controlled trials including 967 subjects with chronic low back pain, no serious adverse events were reported. A report in the journal Alternative Medicine Review states that yoga, which may be considered an adjunct therapy for stress and anxiety, is supported by good compliance among patient populations and a lack of drug interactions. The same study states that better research is needed before strongly recommending yoga for the specific purposes of reducing anxiety and stress. The current research is plagued with common statistical challenges: lack of a control group, variations in studied physiological markers, lack of validated scales, and heterogenous study populations.
For the pelvic rehabilitation provider, having a working knowledge of common yoga terminology and postures can assist in modification or adaptation of a patient's current routine. In addition, learning to apply yoga concepts and postures such as breathing, trunk and pelvic coordination, soft tissue lengthening within a patient's comfort can add to a pelvic rehab provider's toolbox. There is room for you to join Dustienne Miller, physical therapist and yoga instructor, in California at the Yoga for Pelvic Pain course. Contact the Pelvic Rehabilitation Institute if you have any questions about this continuing education course.
For patients who are diagnosed with constipation, functional anorectal testing is often completed prior to referral for physical therapy. A recent study concluded that clinical examination of pelvic floor muscle function is critical for identifying a rectocele or pelvic muscle overactivity, and that anorectal function tests should be reserved for selected cases. Pelvic rehabilitation therapists are able to perform tests of the pelvic muscles and function during a patient's attempts to contract, relax, and bear down through the pelvic floor. These tests are easy to repeat and a patient can be instructed in corrective muscle techniques to improve the ability to empty the bowels.
Consider the patient who presents to the clinic after experiencing a defecography. In this test, a patient undergoes an imaging study while sitting on an elevated toilet seat. The patient is asked to bear down to evacuate a bolus of material that is placed inside the rectum. It is easy to understand why a patient finds this test to be "embarrassing." Following this test, when a patient is diagnosed with dyssynergia (when the puborectalis muscle contracts rather than lengthening and relaxing during attempt to defecate) he or she is frequently referred to pelvic rehabilitation. A pelvic rehab therapist can observe and palpate the same phenomena in the clinic: when asked to bear down or drop the pelvic floor muscles, if a patient instead contracts or is unable to lengthen the muscles, re-training can be implemented.
I have often wondered why a patient would need to complete this type of testing for constipation-related pelvic muscle dysfunction if the same patient could reverse a dysfunctional muscle pattern with a brief bout of pelvic rehabilitation. The research by Lam and Felt-Bersma (full-free text article linked above) appears to confirm this thought, concluding that anorectal functional testing contributes little to information that can be gained in clinical examination in women who have idiopathic constipation.
The authors studied 100 women who were diagnosed with idiopathic constipation and who fit the Rome III criteria. A prospective evaluation included an extensive questionnaire regarding complaints, abdominal, rectal, and vaginal examination, and anorectal function tests such as anorectal manometry (ARM)and anal endosonograpy (AUS). Exclusion criteria included inflammatory bowel disease, fissures, or fistula, and endocrine disorders orcolonic obstruction were ruled out. Of these 100 women, 25% were found to have hypertonia and dyssynergia of the pelvic floor, and 15% presented with a rectocele. During anorectal manometry, the authors also noted that women had difficulty relaxing during straining. In the group studied, 37 women complained of impaired evacuation, and interestingly, 40% of these women had a rectocele, yet no rectoceles were identified in the women who did not complain of impaired evacuation.
While medical screening for patients who complain of constipation is important, this research identifies a group of patients (those diagnosed with idiopathic constipation) for whom ARM or AUS testing does not contribute significantly to the evaluative process. The study is very valuable reading for pelvic rehabilitation providers as the authors clearly understand the role of rehabilitation and articulate the value ofpelvic floor muscle function in meaningful ways throughout the report. If you are interested in learning how to evaluate and treat patients who have constipation, there are 3 seats remaining in the PF2A continuing education course at the end of this month in Fairfield, California (right next to Napa, in case that interests you!) The PF2A course covers bowel dysfunction such as constipation, fecal incontinence, and other colorectal conditions, and also offers on Day 3 an Introduction to Male Pelvic Floor function and dysfunction related to pelvic pain and urinary dysfunction. Following the West coast PF2A, there are East coast and Midwest dates, click here to find the course information. Sign up early as this course always sells out!
Treating patients who have chronic pelvic pain is challenging for many reasons. The nature of chronic pain in any body site often means that the patient has a multifactorial presentation that requires a team approach to interventions. And because the pelvis also contains the termination of several body systems such as the urologic, reproductive, and gastrointestinal, there exists potential for addressing a musculoskeletal issue that is masking a medical issue which requires intervention by a medical provider. The phrase "When you have a hammer, everything looks like a nail" can be applied to patient care for any discipline. When a patient presents with chronic pelvic pain, pelvic rehabilitation therapists can usually find tender pelvic muscles to treat. Is the pelvic muscle tenderness from guarding due to visceral pain or infection?
In a 2013 article in the journal General Practitioner, Dr Croton describes red flag symptoms in acute pelvic pain. These include pregnancy, pelvic or testicular masses, and vaginal bleeding and/or pain in postmenopausal women. During the history taking, patients can be asked about menstrual patterns, possibility of pregnancy, and sexual history. Further medical evaluation may include a pregnancy test, ultrasound, laparoscopy, and urine tests to rule out infection. While the above is not an exhaustive list, it reminds the pelvic rehabilitation provider to always keep in mind the potential for medical evaluation and intervention. Once a patient has been deemed to have "only chronic pelvic pain," a new, equally challenging list emerges: is the pain generated by an articular issue, myofascial dysfunction, neuropathy, psychological stress, or postural pattern? Is the pain local, such as in the pubis symphysis or in the sacroiliac joint ligaments, or are the symptoms referred from a nearby structure, such as the abdominal wall or the thoracolumbar junction? And what are the best methods to examine in a systematic way the various theories about the origins of a patient's pain?
Peter Philip has created a course to provide answers to the above questions. He combines skills in both orthopedics and manual therapy, and pulls from an extensive knowledge about pelvic pain and differential diagnosis which was the research topic of his Doctor of Science degree. Peter's course provides clearly instructed techniques in anatomical palpation, spinal and joint assessment, and he also instructs in how the nervous system and cognition can impact a patient's perception of pain. The course will be offered at the end of this month in Seattle- don't miss this chance to refine skills in differential diagnosis for chronic pelvic pain!
As I looked through this post by an accomplished yoga instructor on the "Top 10 Yoga Postures for Strength," I tried to look at the words and images through the eyes of our typical patients. The chosen postures made the list as they contained foundational "alignment and strength needed to master many more advanced postures." While this may be true for some, I can easily imagine the trouble that most of my patients would find by attempting to cruise through the demonstrated techniques. With jump backs, headstands, handstands, and one arm side planks, there is little caution made about hyper extensibility, about "gripping" postures as Diane Lee explains so well, or about compensatory patterns that can cause strain or injury.
The yoga instructor is not to be blamed- any magazine, blog post, or website that sells fitness or wellness attempts to package information to the public in attractive and efficient methods. An impressively toned, graceful, and high-level yoga practitioner is perfect for such a marketing goal. Unfortunately, any person reading an instructor's guide to finding your physical strength does not have said instructor giving the required feedback about joint position, compensations, and necessary modifications or starting postures.
Patients everywhere espouse the benefits of a yoga practice, and we all have likely met someone whose life was drastically changed for the better after finding yoga. Can yoga also be the cause of an injury? I recall entering a new yoga class at a gym (where the instructor had created a "guru" type following) and I was horrified at the instructor's lack of restraint in guiding a room of 70 or more students through very advanced poses that they were simply expected to push themselves through. The students wore their suffering like a badge, telling each other to "stick it out" as they would keep getting stronger. The instructor then approached me and, without knowing anything about me or my body, twisted me aggressively into a posture that I quickly unraveled as soon as she moved away. As if students cannot find enough ways to push the body outside of a comfort zone, having an instructor violate basic safety principles (was I returning to yoga after a spinal surgery?) adds to the potential for injury.
In a systematic review of adverse events associated with yoga, Cramer, Krucoff & Dobos describe musculoskeletal injuries such as fractures, ligament tears, joint injuries, disc annular tears, and several cases related to breathing techniques. Headstands were a common method for acquiring a yoga-related injury. The authors suggest that for patients who have physical or mental ailments, yoga can be adapted to a patient's "…needs and abilities and performed under the guidance of an experienced and medically trained yoga teacher."
While yoga does not need to be discouraged, we may need to consider the patient's abilities and challenges, and be familiar with our community resources prior to suggesting that a patient begin yoga. If you are more interested in advancing your own practice and in learning how to apply yoga principles and postures to your patient populations, the Institute has several means to accomplish this. For patients who have pelvic pain, Dustienne Miller will teach Yoga for Pelvic Pain in March, where you can learn how to tailor specific yoga techniques for specific patient presentations and conditions. You can also check out Ginger Garner's live and on-line yoga courses by clicking here (scroll down to Yoga as Medicine).
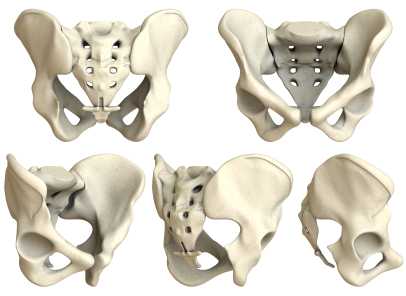
Are sacroiliac joint injections useful for our patient population? A 2013 review article, available here, concludes that current literature "…is unable to fully conclude the effectiveness of the modality and provide adequate comparison against surgical treatment." The above linked article provides a description of fluoroscopy-guided sacroiliac joint injections that can be used for both diagnostic and for therapeutic purposes.
According to the article, a guided injection may be indicated in a patient who has known sacroiliac joint pathology, a history of trauma, or referred symptoms into the buttock or lower extremity. Contraindications can include pathology of coagulation, pregnancy (due to radiation effects), systemic or local skin infection, or patient allergies to medication. During the procedure, a local anesthetic is utilized, and the patient is minimally sedated so that he or she is able to answer questions about pain. Both a pain-reducing medication and an anti-inflammatory are typically utilized; however, in patients who have received a maximum level of steroids, only an analgesic may be injected.
Results of an injection may include provocation of symptoms and/or immediate relief, which provides diagnostic value, i.e., that the structures injected may have, in fact, been causative to the patient's symptoms. For many patients, pain relief occurs within 24 hours. The long-term benefits of sacroiliac joint injections is not well-documented, so the ability to predict length of benefit is challenging.
In regards to rehabilitation of the patient who has undergone a sacroiliac joint injection, following a procedure, the patient is usually instructed to rest for 3-4 days and to follow-up with the referring medical provider within 2-3 weeks. The level at which a patient should resume physical activity, therapeutic exercises, and participation in physical therapy is determined by the medical provider. Level of activity in rehabilitation should therefore be coordinated with the patient's medical provider and potentially with the interventionist who performed the injection.
For more information about sacroiliac joint injections, check out this MedScape article about the topic, or clickhereto view a video of an SIJ injection. To learn clinical information about SIJ evaluation, mobilization, and stabilization activities, check out the next Sacroiliac Joint & Pelvic Ring Dysfunctioncontinuing education course taught by Pelvic Rehabilitation Institute faculty member Peter Philip. This course will be offered two times this year; coming up in early February on the West coast (Santa Barbara, CA) and in July on the East coast (Baltimore, MD.) Click here to learn more about the course objectives and schedule.
At the end of this month, Herman & Wallace instructor Michelle Lyons, BSc Physio, PT, MISCP will be teaching our Pelvic Floor Level One course at Coventry University in the United Kingdom.
H&W teamed up with Gerard Greene, MSc (Manip Physio), MMACP, MCSP, PG Cert HEd to put on this course. Below is a guest blog from our friend across the pond, Gerard, about his experience putting on an H&W PF1 event:
There has been a lot of buzz and excitement in UK Physiotherapy circles about the first Herman & Wallace PF1 course.
The majority of Physiotherapists attending this course will be from England, but we also have participants flying in from Northern Ireland, Portugal and Cypress. The participants have a range of clinical backgrounds, including working in the UK National Health Service (NHS), private hospitals and private practice. There will also be some University- based Physiotherapy lectures. What will really make the PF1 course unique will be the attendance of some Midwifery Lecturers. It is hoped that the Physiotherapy/ Midwifery synergy on the course will lead to some joint projects in 2014, which will only further improve patient care and outcomes.
Women’s Health in the UK has been getting increasing profile in both the media and the professional literature with two key publications recently on NICE guidelines for Stress Incontinence and a Cochrane review for management of Pregnancy related pelvic and LBP.
As the course organiser, I was able to generate a lot of energy and momentum around the course through the use of social media such as Twitter, Facebook and Linkedin. Although the Twitter community around pelvic rehab and women’s health physiotherapy is well established in the USA and Australia, it is in it’s infancy in the UK.
Patterson Medical, the biggest supplier of Physiotherapy and rehab equipment in the UK, will be supplying the EMG devices so that participants can learn to use this modality.
Michelle and I also share an Irish connection, as we both graduated from Physiotherapy School in Dublin, Ireland in 1994; Michelle from University College Dublin and me from Trinity College Dublin. Although both Universities were seen as traditional rivals, in the Physiotherapy world this common ground has been a real bonus in the development of our professional relationship. Michelle is a recognized expert in Women’s Health Physiotherapy and she and I have worked closely in organizing the UK course, as well as further plans for the development of Women’s Health Physiotherapy education and training in the UK in 2014. Working with instructor Michelle Lyons, and H&W team members Siv Prince and Derek Huff has been a very positive and energizing experience, and I’m already looking forward to the next joint event.

Gerard has a musculoskeletal physiotherapy background and has taught and delivered Physiotherapy courses in Ireland, N Ireland, England, Scotland, Wales, Turkey and Jordan. Gerard is looking forward to doing some further teaching in the Middle East and the USA next year. He also lectures on the MSc Manual Therapy Programme in Coventry University which has a national and international reputation for excellence. H&W is very much looking forward to working with him on this course and in the future!
A recent study asked if transcutaneous electrical nerve stimulation (TENS) can be a helpful treatment for men who have refractory chronic pelvic pain. 60 men completed pain diaries and the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) at baseline, after 12 weeks of TENS treatment, and at last known follow-up. The mean age of the subjects was 46.9 years. TENS was measured as an effective treatment in nearly half of the men, and the benefits of the treatment were sustained during a mean follow-up of 43.6 months in 21 of 29 patients. The primary measurement tool for pain, the Visual Analog Scale, or VAS, significantly decreased from 6.6 to 3.9. Quality of life measurement was also improved, with more men feeling mostly satisfied, pleased, or delighted versus dissatisfied, unhappy, or terrible.
What's the take home message? Regardless of the limitations of the study (non-randomized, non-placebo), TENS was found to be a safe and effective treatment without any adverse responses within this study. As a means of neuromodulation, which we know is critical in conditions of chronic pain, the application of electrotherapy is inexpensive, low-risk, and is a useful tool in the healing process. That healing process should include therapies that the patient can apply himself, so that he recognizes his own capacity and necessity for participating in recovery of function.
As there are few studies that address electrotherapy only for chronic pelvic pain, this research is useful in adding some weight to our clinical choices in modality use. Does a patient need to utilize TENS for 12 weeks to determine efficacy? Probably not, but this is an easy modality that can be trailed in the clinic, and utilized as a home program tool if recorded as beneficial for the patient.

Following H&W founder Holly Herman's amazing presentation at the North American Menopause Society's Annual Meeting, Holly sat down with Dr. Mache Seibel to talk pelvic rehab and the role of the PT in treating patients with bladder, bowel and sexual dysfunction.
You can watch the interview HERE
According to NAMS, the attendance at the annual meeting was over 70% physicians and 13% nurses. Physical therapists and "other professionals" made up only 8% of attendace, so kudos to Holly for spreading the gospel about the important role of the PT in women's health!
Want to catch more Holly? She'll be teaching Pelvic Floor Level One, Pelvic Floor Level Three, Care of the Pregnant Patient, Care of the Postpartum Patient, and Peripartum Special Topics in 2014!
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./











































