Ashley Rawlins is a Dallas-based doctor of physical therapy (DPT) with advanced certification in pelvic health and obstetric health. She practices at Origin, leading provider of virtual and in-person physical therapy for women. Dr. Rawlins's areas of specialization include pelvic pain, sexual dysfunction, pregnancy-related pain, postpartum recovery, and bowel and bladder dysfunction. She is a passionate author and educator and enjoys creating educational materials and teaching classes for patients, students, and fellow physical therapists.
I may be biased, but pelvic health is arguably one of the most important specialties in physical therapy. It's well known that pelvic floor muscle dysfunction affects individuals across every age group, life stage, sex, and gender, and can contribute to pain and dysfunction in many other areas of the body. According to research, 23.7% of women have at least one pelvic floor disorder and this percentage only increases with age. (1) So, why aren’t more physical therapists specializing in pelvic health?
A cross-sectional survey completed in 2018 found that the biggest barriers to entering this specialty are “lack of awareness, mentorship, and continued education.” (2) An alarming 59% of physical therapists have received little to no information on pelvic health physical therapy when graduating from their entry-level program. (2)
If you’re a physical therapist reading this, you’ve probably received a peppering of instruction on topics including lymphedema, osteoporosis, pregnancy, and maybe urogenital dysfunction. When I was a student, I only had two lectures covering topics related to pelvic health, plus one afternoon dedicated to observation of the prosected female sex anatomy. Luckily, those lectures and that one afternoon were so fabulous, they got me hooked on this specialty, but it was hardly enough education, given the prevalence of pelvic floor dysfunction.
More awareness of and education on pelvic health is needed so that physical therapists can better care for their patients. At Origin, we’re helping to fill this need by supporting physical therapy students who are interested in pursuing a career in pelvic health, but who may not be able to get the required experience.
Pathways to Pelvic Physical Therapy
There isn’t one specific path to becoming a pelvic physical therapist. Some students will complete a post-professional residency in pelvic health. Some will independently take continuing education courses and pursue certifications or board certifications in pelvic health. Whichever path you take in getting the knowledge and hands-on skills that are critical for safely diagnosing and treating this patient population, one thing is true: It can be both expensive and nerve-wracking!
If you are lucky enough to get a pelvic health clinical rotation, you’ll likely need to complete an advanced training course on pelvic health first. This is so you’re familiar with examination and treatment frameworks. These courses are costly for students in physical therapy school and can make these opportunities an impossibility for those with fewer economic resources.
In addition to being expensive to prepare for, clinical rotations for pelvic health in physical therapy school are intimidating. Yes, it’s exciting to finally be out in the “real world” after being stuck in a classroom for months. But even if you’re didactically prepared, walking through the doors of a new clinic with little more than the name of your clinical instructor (CI) can be terrifying. My clinical rotations felt more like boot camp, at times — I was dropped into the waters of patient care and made to sink or swim, based on my CI’s rules. Looking back, I know this was really more of how it felt versus the reality, but I longed for a rotation that was collaborative and curated to improve my clinical competence.
Educating & Mentoring Students in the Clinical Setting
At Origin, we don’t want finances to be a barrier for those pursuing a career in pelvic health, nor do we want students to feel underprepared or unsupported. We value creating opportunities, providing education, and mentoring those wanting to enter this area of specialty. Much like the patient care standards at Origin, we have worked to create an elevated student clinical experience. Below are some of the ways that we are providing this education and experience in our pelvic health clinics.
Onboarding: We start each clinical rotation with thorough onboarding so every student feels prepared. Prior to the first day in the clinic, students get a Student Handbook which details everything they need to feel prepared in their clinical rotation, from what to wear, to information on our company’s values, mission, and policies. We also take the time to train students on our EMR system, billing practices, telehealth services, and our model of care.
Learning Modules Depending on the length of the clinical rotation, we have developed various training modules for each of the students to complete with their CI. Important topics related to orthopedic and pelvic health physical therapy include infection control, informed consent, internal and external pelvic floor muscle examination, as well as a thorough training on some of the more common conditions that we treat in our clinics—weekly student “check-ins” help to inform the curriculum organization and tailor each student’s experience.
Simulation Experiences: Taking a course in pelvic health in advance of the clinical will set students up for a more in-depth rotation in pelvic health, but if getting this training is a barrier to starting in pelvic health, we’ve developed simulation experiences for the student. Once the students have completed the appropriate learning modules, we pair students to practice on each other, or help in getting volunteer pelvic models. Additionally, skills labs, team Learning and Development meetings, and student in-service assignments help to reinforce concepts learned throughout the clinical rotation.
At Origin, part of our mission to expand access to healthcare includes expanding the community of knowledgeable and expert pelvic health physical therapists. We feel that by improving the student experience and initiating the path to specialization in pelvic health, we can proactively change the status quo of pelvic floor care.
References:
1. Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–1316. doi:10.1001/jama.300.11.1311.
2. Dockter M, Benson S, Zhang Y, Anderson C, Le D. Factors influencing physical therapists to enter into women's health specialty practice. Journal of Women's Health Physical Therapy. 2018; 42(3): 154-164. doi: 10.1097/JWH.0000000000000107.

Allyson Shrikhande, a board-certified Physical Medicine and Rehabilitation specialist, is the Chair of the Medical Education Committee for the International Pelvic Pain Society. She is a leading expert on pelvic health and a respected researcher, author, and lecturer. Dr. Shrikhande is a recognized authority on pelvic pain diagnosis and treatment and is the author and instructor of the remote course Working with Physiatry for Pelvic Pain. Her course discusses the synergistic nature of pelvic physiatry with pelvic floor therapy.
Chronic Pelvic Pain Syndrome (CPPS) is a condition that causes pain or discomfort in the lower abdominal and pelvic region including the buttocks, lower back, hips, groin, perineum, and deep pelvic structures which last longer than six months. The symptoms of CPPS often affect the function of organs such as the bladder and bowel. It can cause difficulty sleeping and pain with sitting or sexual intercourse. It may also result in mobility issues which can impede your ability to manage basic daily tasks. The symptoms of CPPS should be taken seriously and deserve the attention of a healthcare professional.
What causes CPPS?
CPPS often has no singular root cause but is rather rooted in a combination of multiple different issues. Some of the many common risk factors are:
- Hormonal changes, which may occur naturally, throughout a woman’s lifetime (such as during menopause or pregnancy), or because of a glandular imbalance
- Gynecological disorders like fibroids, endometriosis, adenomyosis, polycystic ovarian syndrome, pelvic inflammatory disease, pelvic congestion syndrome, vulvodynia, and lichen sclerosus
- Infections, including yeast infections, urinary tract infections, and bacterial vaginosis
- Urological causes such as bladder pain syndrome or interstitial cystitis
- Musculoskeletal causes including hip, sacroiliac joint, or spine pathology, Myofascial Pain syndromes, and pelvic floor muscle tightness or spasticity
- Gastrointestinal causes like hemorrhoids, irritable bowel syndrome (IBS), Crohn’s disease, and ulcerative colitis
- Neurologic disorders such as herpes simplex or migraines
- Rheumatological disorders such as Ehlers Danlos Connective Tissue hypermobility disorders, rheumatoid arthritis
We also need to acknowledge how important mental factors like stress, anxiety, and emotional trauma often are in contributing to pelvic floor muscle tension. There also may be hereditary factors that cause an upregulated nervous system, which often contributes to increased pain sensitivity.
What makes CPPS so difficult to diagnose?
The causes of CPPS are complex. It’s a condition that often involves multiple organs as well as the nervous, myofascial, and skeletal systems. Some of the most common risk factors for CPPS, including endometriosis and neuromuscular dysfunction, are hard to accurately diagnose. These conditions may not appear on x-rays, ultrasounds, or other imaging tests. Proper identification of CPPS requires a pelvic pain specialist to make an informed analysis of the patient’s medical history and symptoms.
How would you describe a physiatrist's role in working with other specialists to treat CPPS?
Physiatrists are the “quarterback” of CPPS patient care. This is because physiatrists are not trained in just one organ system, we’re trained to examine the interplay of the different organ systems with each other, as well as with the muscles and nerves. This makes physiatrists uniquely qualified to “quarterback” a CPPS patient’s healthcare team. We take a holistic look at each patient, including mind-body connections. This helps us understand each individual person’s primary pain generators and predisposing factors to having pelvic pain.
To learn more about working with physiatry, join Allyson Shrikhande at her course, Working with Physiatry for Pelvic Pain, scheduled for January 11, 2022. Her course will review the core elements, including diagnosis and non-operative treatment options, for a successful pelvic floor therapy and pelvic physiatry relationship for non-operative management of Chronic Pelvic Pain (CPPS) patients.
This article is contributed by faculty members Tiffany Lee and Jane Kaufman. Their course, Biofeedback for Pelvic Floor Muscle Dysfunction, is scheduled for December 4-5, 2021 provides a safe space for clinicians to learn and practice this valuable tool.
Rarely do practitioners see a topic so argued in pelvic rehabilitation as the use of surface EMG biofeedback. There are practitioners who boldly state they are for or against it on their social media accounts and clinic pages. Therapists are not questioning the use of biofeedback with neurologic or orthopedic applications, so why is it such a polarizing topic in pelvic health? The Pelvic Rehab Report sits down with faculty members Tiffany Lee and Jane Kaufman to discuss the tool they love. This month they published a Special Issue article in the Biofeedback Journal for the Association for Applied Psychophysiology and Biofeedback. These two instructors have over 50 years of combined experience using biofeedback.(*)
Biofeedback provides visual and auditory feedback of muscle activity and is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function, enabling the patient to learn how to alter the physiological process through verbal and visual cues. Jane Kaufman explains that "many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients to hone in on body awareness and connect all the dots." Muscle evaluation through digital exam offers strength but does not appropriately address electrical activity such as resting tone, ability to recruit or release tone in the muscle. The use of biofeedback addresses the specificity of muscle contraction and release offering an additional view of muscle function.
In a 2020 research study by Pilkar et al, clinicians reported sEMG barriers of use which included limited time and resources, clinically inapplicable sEMG system features, and the majority of clinicians' lack of training and/or confidence in utilization of sEMG technology. This research also noted technical challenges including the limited transfer of ever-evolving sEMG research into the off-the-shelf EMG systems, nonuser-friendly intuitive interfaces, and the need for a multidisciplinary approach for accurate handling and interpretation of data. (1)
To break this down into layman terms, one contraindication may be the price of a biofeedback unit. Tiffany Lee recommends using a 2-channel sEMG biofeedback hand-held unit with the software on a laptop or computer. In fact, to become board certified in pelvic floor biofeedback, the Biofeedback Certification International Alliance (BCIA) requires that you have a 2 channel EMG system with software. If you are using a hand-held one channel unit, the patient will have a difficult time seeing the muscle activity and the coordination between the abdominals and pelvic floor. This prevents meaningful treatment with this treatment tool as the patient cannot understand or interpret the LED bars on the machine (and often the therapist cannot understand either). In truth, the benefits outweigh the cost of the equipment and within a few treatments, you can cover the cost of the unit with the appropriate software to offer the proper visualization of muscle function.
Training is another issue, to start utilizing biofeedback in your clinical setting you need to have proper training in the modality. Most therapists have never been properly trained and if they take a course where the instructor doesn’t believe in the benefits of biofeedback, they feel negatively toward a tool they have never personally explored. Biofeedback relies on a skilled clinician to interact with the patient, give verbal cues, ensure that the proper muscles are contracting and relaxing, and must be used in conjunction with their other skills and knowledge.
Think of sEMG biofeedback as a tool in your toolbox. Tiffany shares, "in a study by Aysun Ozlu MD, et al., the authors conclude that biofeedback-assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone." She continues, "Biofeedback is a powerful tool that can benefit your patient population and add to your skill-set."(2)
Essentially, the acceptance of sEMG biofeedback in rehabilitation requires a unit (with software and sensors), training, and a multidisciplinary approach. Used correctly, it can positively impact patient performance and care in the clinic. Keep in mind sEMG is a non-invasive technique. It has already shown great promise in the field of neuro-rehabilitation and has been a widely-utilized tool to assess neuromuscular outcomes in research. Jane Kaufman concludes that "In short, biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors." This gives the patient the opportunity to recognize that ‘yes, they are in charge of this muscle and that they can achieve success in overpowering the symptoms.’ Biofeedback routinely allows the patient to understand that they are empowered to heal themselves with the tools you offer. They are in charge of their bodies and the outcome of treatment.

There is a long history of scientific evidence to support the use of sEMG biofeedback in the management of incontinence symptoms or pain symptoms. As a non-invasive, cost-effective, and powerful treatment modality, healthcare providers should consider this treatment tool when managing patients with pelvic floor dysfunction. Providers should be educated in the proper use of this valuable modality to gain the most out of the skills and knowledge that can be achieved through this intervention. For more information regarding courses and certification please visit www.BCIA.org.
Tiffany asked several PTs and OTs that have been to the board certification courses what they love about biofeedback. Here are a few answers:
- “Biofeedback empowers my patients and gives them the confidence that they are actually doing their exercises and/or relaxing correctly! I’ve had nothing but positive feedback from patients and it’s such a great tool to have as a pelvic floor therapist.”
- “My patients really love it, and they ask for it. I especially see the value for dyssynergia work on bearing down and learning eccentric abdominals and relaxed pelvic floor muscles. For men, I work on relaxing in standing and postures if they can’t empty their bladder. Ultimately the treatment needs to be meaningful to the patient. Biofeedback can complement other treatments. Their needs come before ours.”
- “After ONE session with a 5-year-old with constipation, mom called me in sheer excitement, screaming over the phone that he pooped on the potty!!! Something he has NEVER done before. Biofeedback helped him find and coordinate the potty muscles and tummy muscles and this made a huge difference for him!”
- “Becoming certified in biofeedback has only been positive for me. My patients feel that the initial sEMG evaluation sets the stage for my plan of care, and my reassessment at discharge is a tangible reflection of their progress. Not to mention its strength as a marketing tool.”
The Satellite Lab Course, Biofeedback for Pelvic Floor Muscle Dysfunction, scheduled for December 4-5, 2021 provides a safe space for clinicians to learn and practice this valuable tool. Registrants will gain knowledge about the benefits of using this modality in their clinical practice. Participants will learn how to administer biofeedback assessments, analyze and interpret sEMG signals, conduct treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences.
Special Issue article in the Biofeedback Journal for the Association for Applied Psychophysiology and Biofeedback
- * Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Jane Kaufman, PT, MEd BDB-PMD; Kathryn Stanton, PT, DPT; Tiffany Ellsworth Lee, MA, OTR BCB-PMD, PRPC. Biofeedback (2021) 49 (3): 71–76. https://doi.org/10.5298/1081-5937-49.3.01.
References:
- Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations. Rakesh Pilkar, Kamyar Momeni, Arvind Ramanujam, Manikandan Ravi, Erica Garbarini, Gail F. Forrest. Front Neurol. 2020; 11: 578559. Published online 2020 Dec 18. doi: 10.3389/fneur.2020.578559 PMCID: PMC7780850
- Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD. Neurourol Urodyn. 2017 Nov;36(8):2132-2141. Epub 2017 Mar 27. doi: 10.1002/nau.23257 PMID: 28345778.
- The basics of surface electromyography. R. Cram, G. S. Kasman. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7.) Jones and Bartlett. 2011
This week The Pelvic Rehab Report sat down with some of our favorite Occupational Therapists to discuss the role of OTs in the field of pelvic rehabilitation. The following blog is provided by Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, Lindsey Vestal, MS, OT, and Laura Rowan OT/L.
Most people associate pelvic health with PTs- so many are surprised to see OTs in this specialty. Herman and Wallace faculty and instructor Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, LPF-CT has been an OT for 28 years and has spent the last 20 years specializing in pelvic health. She recalls, “My first Herman and Wallace course was PF1 11 years ago. I was the only OT in a class of 50. I was so appreciative of H&W’s foresight to include OTs in the course offerings. A PT sat down next to me and said, “Why are you here? I didn’t know OTs could treat pelvic health!” Yes, we can! It is within our scope of practice and the majority of therapist specialized learning comes post-graduation.
Lindsey Vestal, OTR/L has been an OT for 11 years and her private practice focuses on pre and postnatal people. She is a moderator of the Facebook group “OTs for Pelvic Health” with over 3,100 members. She is bringing awareness to the PH specialty by educating OTs on the best way to treat and collaborate with PTs and other providers in the field. She says, “ Just as OTs and PTs work side-by-side in other fields of rehab, there's a huge need for us to work collaborating in pelvic health. In grad school, OTs study motivational interviewing, nonverbal communication, we have mental health classes and a strong background in sensory approaches, energy conservation, self-regulation strategies, the involvement of the nervous system, time management, working with trauma, habits, routines, ADLs, the musculoskeletal system, functional movement, and activity grading. Pelvic floor function is a crucial part of a much broader functional task of toileting and intimacy, both of which have broader connections within a person’s emotional, cognitive, and social abilities. It's also important to consider the social implications for people with pelvic floor issues such as withdrawal from social and recreational activities, social isolation, disempowerment, lack of self-esteem, anxiety, depression, and the impact on close relationships such as with our spouse, our friends, and our children. This OT-specific background has given me a great foundation to serve my PF population.”
Another seasoned PHOT is Laura Rowan, OT/L who has been an OT for 21 years and the last 14 years has dedicated her practice to pelvic health. She works with all gender diversities across the lifespan with a focus on complex pain patients and athletes. Laura provides manual therapy courses and mentorship for OTs starting in this specialty. She says, “OTs are great at analyzing how the client is executing functional tasks and offering new strategies, adaptations, and compensation techniques for a less provoking and safer way to accomplish the task at hand. OT’s will often see progress using a whole person approach where a client may have plateaued with a less holistic treatment plan”

Laura shares about her start in the PH journey - “My success did not come without challenges. The vast majority of PTs did not share the same acceptance of OTs as Herman and Wallace. Due to a lack of understanding that continues to exist today, OTs struggle to begin their career in pelvic health. It took me 8 years after PF1 to officially break into the field. I felt like a lone OT in a PT world due to the lack of OT presence and support. I didn’t understand the roadblocks I was facing as pelvic health seemed a natural fit for OTs. OT practitioners have long been lending our expertise in the areas of functional restoration, psychosocial considerations, behavioral modifications, time management, stress management, coping strategies, and task analysis. These are major components of a comprehensive plan of care for individuals with pelvic health dysfunction in relation to their Activities of Daily Living (ADL’s) and Instrumental Activities of Daily Living (IADL’s). I am thankful for the many PTs that mentored me along the way. I was hired by a PT clinic with mentorship and continuing education opportunities. This provided strong foundations for me to later branch out and start a successful private practice. I have further developed into an educator and mentor role to provide the emerging OT practitioners the support I received starting out but through the unique lens of an OT.”
Tiffany adds, “OTs and PTs working collaboratively is a winning combination. We can share patients and focus on treating the whole person. For example, a patient with constipation, dyspareunia, SI dysfunction, and urinary incontinence can work with both OT and PT. I may address their constipation and UI using behavioral therapy, biofeedback, and lifestyle modifications while my PT co-worker addresses the spine, hip, and back dysfunction. If you work in an outpatient setting, you are able to bill separately and treat the same patient. We are taking the same courses side-by-side and learning the same skills. Our backgrounds are diverse and we can serve our patients with a multidisciplinary approach. Instead of being divisive and noninclusive, we should be supporting each other and collaborating. There is plenty of business to go around and PH therapists are some of the most compassionate and empathetic people I have ever met!”
Laura agrees and says, “Pelvic Health is too large of a specialty to be a generalist and have all the answers. It’s always beneficial to have a second set of eyes and even better to have a diverse background for a comprehensive whole-person approach to client-centered care. It’s not about the therapist and their discipline, rather taking a multisystem approach to meet the needs of our clients and how we can better serve them with an interdisciplinary team. We often run out of time to address all of the underlying impairments contributing to the client’s symptoms. OTs and PTs working together allow for all of the contributing factors to be addressed with the appropriate amount of attention required for successful outcomes.”

Lindsey chimes in, “It can take a village to care for pelvic health clients, so why not lean on our colleagues for their areas of strength? I mean isn’t that why we are rehab professionals? To ultimately serve our clients the best way possible? Pelvic health is a very underserved population and in my opinion, there's space for us all.”
Tiffany, Lindsey, and Laura have thriving private practices serving the PH population and each has PH continuing education companies that offer courses and mentoring. They are passionate about spreading awareness of the OT's role in pelvic health and the many benefits of working alongside PTs to meet the needs of this underserved population. By bridging the gap in understanding the valuable role of the PHOT, we can start to decrease extensive waitlists, and open up jobs to qualified passionate OT’s eager to begin their pelvic health careers. You can reach them through email -
This email address is being protected from spambots. You need JavaScript enabled to view it. or www.pelvicfloorbiofeedback.com
This email address is being protected from spambots. You need JavaScript enabled to view it. or www.essentialpelvichealth.com
This email address is being protected from spambots. You need JavaScript enabled to view it. or www.functionalpelvis.com
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 is Board certified in Orthopedics, a Certified Integrated Manual Therapist, and a Herman & Wallace certified Pelvic Rehab Practitioner. Rachna has a personal interest in various eastern holistic healing traditions and she noticed that many of her chronic pain patients were using complementary health care approaches including acupuncture and yoga. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
A patient walks into the clinic 30 minutes late for their appointment with me, brimming with anxiety and apologizing profusely. “I’m so sorry,” they say, “I kept driving around in circles and could not find a single parking spot.” Another patient, a teacher, reports that her anxiety and pelvic pain progressively worsens as her day progresses and peaks when she gets home with her own two young children at the end of a long day. A third patient with a 15-year history of pelvic pain with unexplained infertility who has failed every conventional ART treatment suddenly conceives her miracle child naturally with acupuncture. She shares, “My anxiety was always so high, I could never relax. They stimulated acupuncture points all over my body, and it worked. My anxiety was so much under control this time.”
Here are the things running through my mind as I work with these patients:
- What could be the most effective hands-on clinical intervention I could use to calm them down?
- Could I teach them daily acupressure self-care and wellness regimens to alleviate anxiety?
- Could I foster a feeling of self-control in them to manage anxiety in stressful situations?
- How does acupuncture really work for infertility, and why does it use points all over the body?
- Can acupressure be used to stimulate key potent acupoints for anxiety?
- Is there a physical practice of yoga that is calm and meditative and is complementary to acupressure?
These questions led to researching the currently available evidence, and I found that there has been a rising clinical interest in complementary holistic practices over the last several decades for anxiety & chronic stress management. Current research supports both acupressure and yin yoga as powerful tools in the realm of energy medicine.
Acupressure is based on 3000 years of Traditional Chinese Medicine (TCM) that believes in Meridian Theory and energy channels which are connected to the function of the visceral organs. There is emerging scientific evidence of acupoints transmitting Qi energy through the vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera with potentially powerful integrative applications across multiple systems. This network is also continuous with more specialized connective tissues such as the periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (1). Fascia and connective tissue literally pervade every anatomic dimension in the body.
Helene Langevin (2) and colleagues proposed an anatomical/ physiological parallel to explain some of the key concepts of TCM.
- Qi: Sum of all body energetic phenomena (e.g. metabolism, movement, signaling, information exchange)
- Meridian Qi: Connective tissue biochemical/bioelectrical signaling
- Blockage of Qi: Changed connective tissue matrix composition leading to a change in signal transduction
- Restoration of the flow of Qi: Cellular activation/gene expression leading to restored connective tissue matrix composition and signal transduction
Modern acupressure charts map the principal 12 meridians connected to the physiological functions of key organs. The key meridians to focus on in pelvic health patients would be the bladder, kidney, spleen, and stomach meridians. Acupressure is systemically effective for a host of conditions including anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions. Each acupressure point has many internal connections to the visceral organs. Stimulating these points by using acupressure assists the body’s self-regulating mechanisms and facilitate healing and neurophysiological quieting.
A recent study by Elizabeth Monson (3) and colleagues retrospectively analyzed 519 acupressure treatments on hospitalized patients, nurses, and the general public across six US states. They followed a specific acupressure protocol and looked at pre- and post-treatment in conjunction with self-rated pain and anxiety scores, where 0 represented no pain or anxiety, and 10 represented the worst pain and anxiety. They found that:
- Hospitalized patients demonstrated a 4 point ↓ in pain scores and 5 point ↓ in anxiety scores
- Nurses demonstrated a 3 point ↓ in pain scores and 4 point ↓ in anxiety scores
This study concluded that acupressure is a highly satisfactory complementary therapy that can demonstrate a clinically significant decrease in self-rated pain and anxiety scores (2).
A robust body of research also attests to yoga being a powerful integrative health practice for alleviating daily anxiety and stress. Yoga is an umbrella term for various physical, mental, and spiritual practices originating in ancient India. Hath Yoga is the most popular form of Yoga in western society. Yin Yoga, a derivative of Hath Yoga, is a much calmer meditative practice that uses seated and supine postures, held three to five minutes while maintaining deep breathing. Its focus on calmness and mindfulness makes Yin Yoga a tool for relaxation and stress coping, thereby improving psychological health (4).
Yin Yoga is also a wonderful complimentary practice that can be combined with Acupressure. Yin Yoga engages the physical, emotional, and energy body. Yin postures supportively align the body to stress connective tissues along specific meridian lines that activate potent acupressure points along those meridians. The Acupressure for Optimal Pelvic Health remote course explores Yin postures within key meridians and integrates acupressure and Yin Yoga with modifications into rehabilitation interventions. Anxiety and daily wellness self-care program is also a key part of the course.
As pelvic health therapists and medical providers, we can empower our patients to recognize the mind-body-energy interconnections and how they affect multiple systems, giving them the tools and self-care regimens to live healthier anxiety and pain-free lives. Combining our orthopedic skills with mindfulness-based holistic interventions also complements our best evidence-based practices.
The course Acupressure for Optimal Pelvic Health is an evidence-based journey of holistic healing and empowerment curated and taught by Rachna Mehta. To learn how to integrate acupressure and Yin Yoga into your practice, join the next scheduled remote course on October 23-24, 2021.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.2.
- Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec. 2002;269(6):257-265. doi:10.1002/ar.10185
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521. doi:10.1089/acm.2018.0422
- Daukantaitė D, Tellhed U, Maddux RE, Svensson T, Melander O. Five-week Yin Yoga-based interventions decreased plasma adrenomedullin and increased psychological health in stressed adults: A randomized controlled trial. PLoS One. 2018;13(7)
- Hmwe NTT, Browne G, Mollart L, Allanson V, Chan SW. An Integrative review of Acupressure interventions for older people: A focus on sleep quality, depression, anxiety, and agitation. Int J Geriatr Psychiatry. 2019;34(3):381-396. doi:10.1002/gps.5031
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of Acupressure on Anxiety: A Systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
Molly O'Brien-Horn, PT, DPT, CLT is a pelvic health physical therapist in California. She is a teaching assistant with Herman & Wallace and will be acting as a TA in the upcoming remote course, Inclusive Care for Gender and Sexual Minorities. Molly is a Certified Lymphedema Therapist (CLT), an LSVT BIG Parkinson’s Disease certified therapist, a trained childbirth doula, and a trained postpartum doula. She is a member of the American Physical Therapy Association Section of Pelvic Health. She has experience in a variety of physical therapy settings, including pediatric oncology, school-based pediatrics, outpatient orthopedics, and wound care. Her passion, however, is working in the field of pelvic floor physical therapy with children, teens, and adults of all gender identities, all sexualities, and all ability levels. In her spare time, Molly enjoys doing yoga, hiking, and relaxing at the beach.
October is LGBT History Month. This annual occurrence is a month-long observance of lesbian, gay, bisexual, and transgender history, and the history of the gay rights and related civil rights movements. H&W is proud to offer courses for treating the whole patient across the gender and age spectrum. The remote courses featured in this blog are Inclusive Care for Gender and Sexual Minorities with instructor Brianna Durand, and Transgender Patients: Pelvic Health and Orthopedic Considerations with co-instructors Sandra Gallagher and Caitlin Smigelski.
Many LGBTQ+ individuals, drag artists, and cisgender and heterosexual persons engage in binding, tucking, packing, and padding for several reasons. These techniques can be life-changing. Many people use these techniques for gender expression, but they can also be used for gender affirmation.
Gender dysphoria occurs when an individual feels distress due to a mismatch between their assigned gender at birth and their own gender identity. For many folx who are transgender, non-binary, queer, or intersex, these practices help reduce gender dysphoria. Instead, they provide feelings of gender euphoria by creating joy, enhancing mental well-being, and improving quality of life through affirming gender identity. Additionally, these methods can provide safety by helping to protect folx in unsafe and unfamiliar environments. Some of these devices, such as packers, can even be used for sexual function and urination
So how does it all work? Binding is when a person wears a device, called a binder, to flatten or minimize the appearance of their chest. Many folx who identify as transmasculine and non-binary engage in binding. However, not all people who bind identify as transmasculine or non-binary. For example, cis and queer women, and cisgender men with gynecomastia may use binders. Also of note, not all people who bind use the same binding methods. Compression shirts and tops, sports bras, and tape are a few examples of the many different binding methods available.
Conversely, padding can be used to enhance the shape and appearance of one’s body, often at the hips and gluteal regions. Padded bras can also be used to enhance breast size and shape. Many transfeminine, queer, intersex, non-binary, and cisgender women often use some form of padding or shapewear devices to help create a more effeminate silhouette. Drag artists often use some form of padding to modify their appearance for their performances to achieve the optimal look for their drag persona. Transmen and cismen can also use padding. Furthermore, wigs and prosthetics (e.g. silicone breast forms, breastplates, and prosthetic vaginas) can be used by these populations to achieve a desired appearance.
Regarding prosthetics, many transmasculine folx, cisgender men, intersex folx, and queer individuals use prosthetics for packing. When someone packs, they use a phallic-shaped device to enhance the prominence of their genitals, often to create the appearance of a bulge in their pants. Some packers can extend the length of a phallus for sexual play, as well. This can be helpful for transmasculine folx post metoidioplasty, intersex folx who may have anatomical differences in sexual or reproductive anatomy, as well as cisgender men who suffer from erectile dysfunction. Packers are often made of silicone and can also include or not include certain features like pubic hair, moveable foreskin, and testes. However, packers don’t have to be made of silicone and can instead be made from other items, such as a pair of socks. They can have multiple functions and be used for things other than packing, such as standing for urination, sexual pleasure for oneself, and sexual pleasure for partners.
While packing increases the prominence of one’s genitals, tucking, conversely, is used to minimize the prominence of external genitalia by creating a flatter appearance between the legs. This act gets its name from the tucking of one's testicles into the inguinal canals, after which the penis and scrotum are then tucked between the legs back towards the anus. Frequently gaffs, tape, or tucking underwear are used to maintain the genitalia in these positions. Tucking is commonly used by transfeminine, non-binary, and intersex persons. However, tucking is not just limited to these groups, as cismen, drag artists, and other populations can tuck also.
While binding, packing, tucking, and padding have many positives, there can be some inherent drawbacks. For example, tucking can increase the risk of Urinary Tract Infections due to the position of the urethra close to the anus. Binding can alter posture and impact breathing by reducing diaphragmatic and rib mobility. Pads can be uncomfortable and hot, while packing devices, Stand-to-Pee devices, in particular, require regular cleaning to prevent unwanted smells and/or infections. All of these practices carry the risk of skin breakdown or irritation if performed too frequently or with improper technique. However, it is important to remember that even with these and other various drawbacks, these acts can be so lifesaving, gender-affirming, and life-protecting for many folx, that at times, the benefits of performing these practices greatly outweigh the risks.
The ins and outs of binding, packing, tucking, and padding can be quite complex, and there is so much to learn about proper usage and technique.
Want to learn more about these and other things related to LGBTQ+ health? Check out these remote course options:
- Inclusive Care for Gender and Sexual Minorities, Brianna Durand and her TA Molly O'Brien-Horn will dive deeper into these and other topics surrounding LGBTQ+ healthcare to educate pelvic health practitioners on how to provide better, safer, and more skilled care for the LGBTQ+ populations.
- Transgender Patients: Pelvic Health and Orthopedic Considerations, co-instructors Sandra Gallagher and Caitlin Smigelski will expand your skills for working with people of all gender identities. This course includes particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
What are you waiting for? Sign up and join us today!

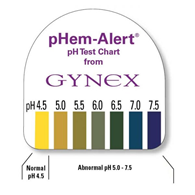
Many years ago a urology doctor shared the skill of testing vaginal pH as part of my pelvic floor exam. I’ve since used it to gather objective data around estrogen status, often finding elevated levels in post-partum, breastfeeding, and peri and post-menopausal women. When correlated with symptoms and visual skin changes this can be a helpful tool to both direct treatment and monitor treatment effectiveness.
To perform pH testing, place a pH strip into the distal vagina. Let it sit there for a few seconds to absorb vaginal moisture. Remove and record results. Any concerning changes in vaginal pH can be documented and reported back to your patient’s medical provider.
Here’s a quick tour through the research on vaginal pH. I hope you enjoy learning and consider adding vaginal pH testing to your clinical practice.
-Normal vaginal pH is considered to range between 4.0 and 5.0 in menstruating women (Garcia-Closas)
-Intervaginal pH does not vary between vaginal location (proximal, mid, distal)
-Clinician test vs self-test results vary slightly but not significantly (Ferris)
-Low serum estradiol levels are associated with high vaginal pH values
-Vaginal pH of 4.5 is indicative of premenopausal estradiol levels and the absence of bacterial overgrowth
-Vaginal pH of 5.0 to 6.5 may indicate either estrogen changes or bacterial overgrowth, a culture may be warranted
-Vaginal pH of 6.0 to 7.5 is strongly suggestive of menopause
-Vaginal pH measurements can be helpful in determining the efficacy of treatment with vaginal estrogen (Caillouette)
-Vaginal pH levels (high) were as sensitive as blood serum FSH levels in the detection of menopause status (Roy) and (Panda)
-Understanding of the vaginal microbiome and its effect on vaginal pH continues to evolve
-“Although lactic acid (produced by Lactobacillus) is the primary acid in normal vaginal secretions, other organic acids such as acetic, mydriatic, and linoleic acid are also normally found in vaginal fluid. Some healthy women actually lack vaginal Lactobacilli, but their vaginal pH is in the normal (moderately acidic) range, and other lactic acid-producing bacteria, such as Atopobium, Megasphaera, and/or Leptotrichia species, are present.”
-Lactic acid is also a byproduct of anaerobic glucose metabolism within the cells of the vaginal mucosa
-The summation of vaginal pH is determined by both the vaginal mucosal metabolism (which is influenced by estrogen) and the vaginal microbiome, both of which are unique to each female
-Vaginal pH is around 5 in newborns, before colonization from microbes, rises to neutral range by 6 weeks of life, and falls when puberty ushers in an increase in estrogen
-Normal vaginal pH helps to keep optimal inflammatory responses and skin barrier functions in vaginal and vulvar skin. Elevated pH in menopause leads to susceptibility to vulvar contact dermatitis
-Topical application to the menopausal vagina restores surface pH and lowers infection risk
-Candida infections do not alter vaginal pH
-STI via chlamydia, gonorrhea, or trichomonas as well as bacterial vaginosis may cause elevations in vaginal pH (Linhares)
- “Detection of HPV was positively associated with vaginal pH, mainly in women < 35 years. Elevated vaginal pH was associated with 30% greater risk of infection with multiple HPV types and with LSIL (low-grade intraepithelial lesions), predominantly in women younger than 35 and 65+ years of age. Detection of C. trachomatis DNA was associated with increased vaginal pH in women < 25 years” (Clarke)
-pH self-testing during pregnancy and treatment of underlying infections positively impacted preterm birth rates (Holyoke and Saling)
-The microbiome in humans is generally >70% Lactobacilli, where other mammals have 1% or less
-Average pH of 21 non-human mammals is 5.4 to 7.8
-Authors propose that the high level of starch in human diets contributes to increased levels of vaginal glycogen which in turn proliferates lactobacilli…continued research will contribute to our collective knowledge base (Miller)
-Vaginal microbiome variability may have an effect on fertility (Xu)
-Douching with an over-the-counter lactic acid containing douche: did not significantly affect vaginal pH or microbiome composition and may promote candida infections (van der Veer)
|
Solution |
pH |
|
Gastric acid |
1.5-2.0 |
|
Vinegar |
2.9 |
|
Orange juice |
3.5 |
|
Beer |
4.5 |
|
4.5 |
|
|
Skin surface moisture |
4.0-5.5 |
|
Milk |
6.5 |
|
Pure water |
7.0 |
|
Saliva |
6.5-7.4 |
|
Semen |
7.2-8.0 |
|
Blood |
7.3-7.5 |
|
Seawater |
7.7-8.3 |
|
Sodium bicarbonate |
8.4 |
|
Hand soap solution |
9.0-10.0 |
|
Bleach |
12.5 |
Linhares. Vaginal pH and Lactobacilli. Am J Obstet Gynecol 2011.
References:
Caillouette, J. C., Sharp Jr, C. F., Zimmerman, G. J., & Roy, S. (1997). Vaginal pH as a marker for bacterial pathogens and menopausal status. American journal of obstetrics and gynecology, 176(6), 1270-1277.
Clarke, M. A., Rodriguez, A. C., Gage, J. C., Herrero, R., Hildesheim, A., Wacholder, S., ... & Schiffman, M. (2012). A large, population-based study of age-related associations between vaginal pH and human papillomavirus infection. BMC infectious diseases, 12(1), 1-9.
Ferris, D. G., Francis, S. L., Dickman, E. D., Miler-Miles, K., Waller, J. L., & McClendon, N. (2006). Variability of vaginal pH determination by patients and clinicians. The Journal of the American Board of Family Medicine, 19(4), 368-373.
García-Closas, M., Herrero, R., Bratti, C., Hildesheim, A., Sherman, M. E., Morera, L. A., & Schiffman, M. (1999). Epidemiologic determinants of vaginal pH. American journal of obstetrics and gynecology, 180(5), 1060-1066.
Hoyme, U. B., & Saling, E. (2004). Efficient prematurity prevention is possible by pH-self measurement and immediate therapy of threatening ascending infection.
Linhares, I. M., Summers, P. R., Larsen, B., Giraldo, P. C., & Witkin, S. S. (2011). Contemporary perspectives on vaginal pH and lactobacilli. American journal of obstetrics and gynecology, 204(2), 120-e1.
Miller, E. A., Beasley, D. E., Dunn, R. R., & Archie, E. A. (2016). Lactobacilli dominance and vaginal pH: Why is the human vaginal microbiome unique?. Frontiers in microbiology, 7, 1936.
Panda, S., Das, A., Santa Singh, A., & Pala, S. (2014). Vaginal pH: A marker for menopause. Journal of mid-life health, 5(1), 34.
Roy, S., Caillouette, J. C., Roy, T., & Faden, J. S. (2004). Vaginal pH is similar to follicle-stimulating hormone for menopause diagnosis. American journal of obstetrics and gynecology, 190(5), 1272-1277.
Xu, J., Bian, G., Zheng, M., Lu, G., Chan, W. Y., Li, W., ... & Du, Y. (2020). Fertility factors affect the vaginal microbiome in women of reproductive age. American Journal of Reproductive Immunology, 83(4), e13220.
Van Der Veer, C., Bruisten, S. M., Van Houdt, R., Matser, A. A., Tachedjian, G., van de Wijgert, J. H. H. M., ... & van der Helm, J. J. (2019). Effects of an over-the-counter lactic-acid containing intra-vaginal douching product on the vaginal microbiota. BMC microbiology, 19(1), 1-13.
*Citations are noted at the end of each article summary
This product was recommended by S. Roy for accurate testing:
It’s OK to be feeling (insert feeling) right now. (maybe: sad, fearful, angry, denial, numb, anxious, avoidant, bored?)
 It’s OK to acknowledge those feelings.
It’s OK to acknowledge those feelings.
It’s also OK to create a plan and direction about what we may do about our feelings, thoughts, and actions.
We can change how we think, what we do and ultimately how we feel.
Breathe. Place a hand on your chest and a hand on your abdomen. Practice inhaling long and deep as if you were pouring the air into your body- first filling the lower hand and then filling the top hand. Pause for a moment when you feel your canister is full and then exhale slowly (top to bottom or bottom to top- either works fine). I prefer breathing through my nose for inhale and exhale but know if you are congested, mouth breathing is fine or you can inhale through the nose and exhale through the mouth- find what works for you. Work on increasing the number counted (silently in your mind) while you inhale, pause briefly and then exhale- making that number count on exhale the same or even longer. Make it a game to see how long and deep your breath can become. Reduce intensity if feeling lightheaded.
Focus on your breath and feel calmness. Return to this breathing whenever you can.
Body Scan/Progressive Relaxation. Take a moment and scan your body for pain or tension. You can start at the top of your body or where your feet are grounded to floor. Notice your body and allow it to be, without judgement. Then starting from the top of your body or the bottom, contract your muscles systematically and then relax. Or focus on the muscle group and allow the muscles to relax and slacken. Maybe send your long, deep breath to each area? Maybe think of color washing each area? Make your scan personal and positive for you. Check-in to your body without judgement and send gratefulness for the work your amazing body does.
Stand Big. Find a wall and place your backside onto it. Pretend there is a string at the crown of your head and imagine your head being pulled up towards the ceiling. Lift your chest as you are standing tall and use your slow, steady, deep breathing to create bigness and calmness. Relax your shoulders. Maybe place the back of your hands onto wall and feel the opening of your chest. Once you have practiced this posture, you can refer to this posture during your day. Stand big, breathe big, be big.
Intentionally SCHEDULE into your life what you love. Schedule time listening to your favorite music. Maybe take up playing an instrument? Practice singing in the shower or car. Set a timer and dance fervently. Create time to draw or paint or write. Make a recipe. Get frozen berries and make smoothies. Maybe add frozen spinach to your smoothie?
Pick up a book. Play a game, cards or even solitaire. Practice Sudoku. Take a bath or shower. Go for a long walk while keeping your distance from others. Find a workout you can do at home that makes you feel powerful. Whatever you love, turn it into a scheduled ritual. Make one small goal and work towards it. Focus on what we can do instead of what we cannot. Find some activity and fulfill a passion just for you. Make sleep a priority and know if you have a bad night, that the next night you will likely sleep better. Perhaps create a sleeping ritual? Call others and ask what they are doing for themselves? Remember to forgive yourself and to feel or express the feelings that are within you. We are all going through this together. Make you a priority and schedule yourself some HAPPY.
Lastly- try to limit the news, your phone and the frig. All of these can create negative feelings that do not fulfill us.
Breathe. Find love in positive activities. Be brave. Be grateful. Forgive.
We are all in this together.
Lauren Mansell DPT, CLT, PRPC is the author and instructor of the Trauma Awareness for the Pelvic Therapist course. She is also offering several courses via Zoom video conference during the Covid-19 pandemic, which can be found on our Remote Learning Opportunities page. Prior to becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC) and Certified Yoga Therapist (CYT). She is a board member of Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Tory Pines State Park provided much needed rejuvination. Ahh sea air.
2. Self-care is mandatory:
We spent Friday relaxing at a beautiful resort in Del Mar. We are learning we don’t need to justify or feel bad about caring for ourselves. It’s necessary and important. We are responsible for meeting our own needs and for refueling ourselves when we provide care for others.
3. Get out of your comfort zone:
The robes we got from the resort were super cozy and it was chilly on the beach, so why not walk the beach in a robe? We laughed at ourselves and others laughed at us and with us. But we were comfy and warm.
4. Do the work when it is time to do the work:
Instead of thinking and talking about the course all day we committed ourselves to being in the moment. When it came time to discuss the details of the next three days, a plan came together with relative ease. This is us working at the resort.
5. Challenges can change your perspective. And a change in perspective can help you with challenges:
This is a (terrible, sorry) picture of us interrupting our morning run to climb a tree. It was a fun challenge and gave us an interesting perspective on our day.
A little more about the course. Woah. The people who showed up came with open minds and hearts, ready and ripe for change. We had powerful times of sharing, listening, learning, and supporting. Meditation and yoga and a healing, honest and real atmosphere brought about transformation in the most beautiful awe-inspiring way. We were profoundly moved. The changes Nari suggested were PERFECT and I was grateful for her innovations. We were all pretty much out of our comfort zones, but that is where change happens.
In the words of one student, “This course couldn’t have come at a more appropriate time because I was in major burnout. I was becoming an unhappy person both professionally and personally. I needed to make a change. Now I am leaving this course empowered to care for myself so I can help patients in a healthy way and enjoy my job again. I am walking away from this course with so many valuable strategies and also feel so much more relaxed and hopeful”
6. Be silly sometimes:
Laugh a lot. Especially at work. Play jokes, have fun. You know what they say about all work and no play. Play.
7. At the end of the day Shake it off (and use pain science as needed):
Our last day we took a run to the beach. When crossing a rail line I tripped and bashed the HECK out of my lower leg. Since I could still run I repeated the mantra “Hurt not harm!!” (which we discuss in class) with great vigor until the throbbing subsided, and we enjoyed a beautiful sunset and the conclusion of our time in San Diego.
Last words of Wisdom:
Gratitude can change us in powerful ways.
A huge and heart felt thank you to Herman & Wallace, our host site, and for each and every participant. We couldn’t do what we do without you and for this we are eternally grateful.
Thank you. Thank you. Thank you.

In a previous post on The Pelvic Rehab Report, Sagira Vora, PT, MPT, WCS, PRPC explored the impact that pelvic floor exercises can have on arousal and orgasm in women. Today we hear part two of the conversation, and learn what factors can impact a woman's ability to achieve orgasm.
 “An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
“An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
Wow, that sounds like paradise! The question is--how to get there? Many of our cohorts and many our female patients have not experienced this or orgasm happens for them rarely. Findings from surveys and clinical reports suggest that orgasm problems are the second most frequently reported sexual problems in women. Some of the reasons cited for lack of orgasm are orgasm importance, sexual desire, sexual self-esteem, and openness of sexual communication with partner by Kontula el. al. in 2016. Rowland found that most commonly-endorsed reasons were stress/anxiety, insufficient arousal, and lack of time during sex, body image, pain, inadequate lubrication.
One factor that comes up consistently, is the ability of women to focus on sexual stimuli. This point has been brought up by various studies and presented in different ways. Chambless talks about mindfulness training and improvements in orgasm ability noted equally in women who practiced mindfulness vs. women who engaged in Kegels and mindfulness. Rosenbaum and Padua note in their book, The Overactive Pelvic Floor, “women who do not have a low-tone pelvic floor and who seek to enhance sexual arousal and more frequent orgasms have not much to gain from pelvic floor muscle training. Actually, a relaxed pelvic floor and mindful attention to sexual stimuli and bodily sensations seem a more effective means of enhancing sexual arousal and orgasm.” Various studies specifically studying the effect of mindfulness training have demonstrated both improved arousal and orgasm ability in women who practiced mindfulness. Brotto and Basson found their treatment group, which consisted of 68 otherwise healthy women, who underwent mindful meditation, cognitive behavioral training and education, improved in sexual desire, sexual arousal, lubrication, sexual satisfaction, and overall sexual functioning.
Cognitive-behavioral therapy appears to play a significant role in improving sexual function in women. Meston et. al. notes, “cognitive behavioral therapy for anorgasmia focuses on promoting changes in attitudes and sexually relevant thoughts, decreasing anxiety, and increasing orgasmic ability and satisfaction. To date there are no pharmacological agents proven to be beneficial beyond placebo in enhancing orgasmic function in women.”
Alas, there are no magic pills to create the above described “state of altered consciousness,” allowing women a sense of “well-being and contentment.” However, mindfulness training and cognitive behavioral therapy are both accessible and attainable for women who want to improve their ability to enjoy this much desired state. Many Pelvic floor therapist incorporate cognitive behavioral and mindfulness approaches in their practice.
The studies above mention pain as one of the factors for inability to experience arousal and orgasm. Hucker and Mccabe even noted that their mindfulness treatment group demonstrated significant improvements in all domains of female sexual response except for sexual pain. Dealing with sexual pain is a daily battle pelvic floor therapist face each day. So, how do women with sexual pain dysfunction differ from women who are experiencing sexual dysfunction but not pain? Let’s explore this in our next blog…
Chambless DL, Sultan FE, Stern TE, O’Neill C, Garrison S. Jackson A. Effect of pubococcygeal exercise on coital orgasm in women. J Consult CLin Psychol. 1984; 52:114-8
Bratto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women Behav Res Ther. 2014 Jun; 57:43-5
Hucker A. Mccabe MP. Incorporating Mindfulness and Chat Groups Into an Online Cognitive Behavioral Therapy for Mixed Female Sexual Problems. J Sex Res. 2015;52(6):627-33
Kontula O., Mettienen A. Determinants of female sexual orgasms. Socioaffect Neurosci Psychol. 2016 Oct 25;6:31624. doi: 10.3402/snp.v6.31624. eCollection 2016
Meston CM1, Levin RJ, Sipski ML, Hull EM, Heiman JR. Women’s orgasm. Annu Rev Sex Res. 2004;15:173-257. Review
Rosenbaum, Talli Y., Padoa, Anna. The overactive Pelvic floor. 1st ed. 2016
Roland DL, Cempel LM, Tempel AR. Women’s attributions on why they have difficulty reaching orgasm. J. Marital Therapy. 2018 Jan 3:0