Recently my coworkers and I celebrated a male patient’s recovery from a long and difficult journey with persistent pelvic pain. “Ben’s” case had many elements of what we normally see in our patients: chronic muscle holding, restricted fascia, allodynia, hyperalgesia, castrophizing and kenisiophobia. Ben was also very upfront about how his pain impacted his emotional well-being and vice versa. His healing process taught us a lot about the biopsychosocial aspects of treating persistent pain. Along his journey we dreamed of the day we could write a blog together and help other people learn from the experience. Ben also decided to make a career change entering school to become a PTA so that he could help others in pain. Here is my interview with this brave patient.
 1. Tell us about how your pain started
1. Tell us about how your pain started
My pain started with urethral burning. Tests showed there was no infection. In retrospect, the cause of pain could have been the beginning of tension on pudendal nerve branches from extreme stress and a series of traumatic incidents that happened within weeks of each other. They included a very embarrassing and stressful summer of unemployment, a father who had heart failure and triple bypass in the fall, and a girlfriend who gave me an ultimatum when I was too stressed to get an erection.
2. What medical tests or treatments were done?
When the pain started, I first thought it was a basic urinary tract infection. I went to the med center and was prescribed an antibiotic. After 3 days without change, I went back in and although they still found no sign of infection, they prescribed an additional antibiotic. The urethral pain never stopped and seemed to get worse. Following a series of visits to numerous doctors and urologists, I repeated tests on the prostate fluid, blood tests, and more bacterial tests. No infection. My PCP also made a fairly large overture of testing me repeatedly for HIV. For five months I had a blood test every month, all came back negative. This was damaging to my psyche. For those months I was terrified my life was over. In retrospect, that doctor was out of line, I changed doctors.
3. What were your thoughts when your doctor suggested physical therapy?
When the doctor suggested pelvic floor physical therapy, I was a little skeptical because I was still convinced that something was wrong in a chemical or infectious way (as is typical for most men with pelvic floor dysfunction). However, desperate to take away the constant pain, I followed the advice.
Stay tuned for part two of our conversation with Ben, coming up in our next post on the Pelvic Rehab Report!
Speaking with a runner friend the other day, I mentioned I was writing a blog on yoga for pelvic pain. She had the same reaction many runners do, stating she has doesn’t care for yoga, she never feels like she is tight, and she would hate being in one position for so long. Ironically, neither of us has taken a yoga class, so any preconceived ideas about it are null and void. I told her yoga is being researched for beneficial health effects, and one day we just might find ourselves in a class together!
 Saxena et al.2017 published a study on the effects of yoga on pain and quality of life in women with chronic pelvic pain. The randomized case controlled study involved 60 female patients, ages 18-45, who presented with chronic pelvic pain. They were randomly divided into two groups of 30 women. Group I received 8 weeks of treatment only with nonsteroidal anti-inflammatory medication (NSAIDS). Group II received 1 hour, 5 days per week, for 8 weeks of yoga therapy (asanas, pranayama, and relaxation) in addition to NSAIDS (as needed). Table 1 in the article outlines the exact protocol of yoga in which Group II participated. The subjects were assessed pre- and post-treatment with pain scores via visual analog scale score and quality of life with the World Health Organization quality of life-BREF questionnaire. In the final analysis, Group II showed a statistically significant positive difference pre and post treatment as well as in comparison to Group I in both categories. The authors concluded yoga to be an effective adjunct therapy for patients with chronic pelvic pain and an effective option over NSAIDS for pain.
Saxena et al.2017 published a study on the effects of yoga on pain and quality of life in women with chronic pelvic pain. The randomized case controlled study involved 60 female patients, ages 18-45, who presented with chronic pelvic pain. They were randomly divided into two groups of 30 women. Group I received 8 weeks of treatment only with nonsteroidal anti-inflammatory medication (NSAIDS). Group II received 1 hour, 5 days per week, for 8 weeks of yoga therapy (asanas, pranayama, and relaxation) in addition to NSAIDS (as needed). Table 1 in the article outlines the exact protocol of yoga in which Group II participated. The subjects were assessed pre- and post-treatment with pain scores via visual analog scale score and quality of life with the World Health Organization quality of life-BREF questionnaire. In the final analysis, Group II showed a statistically significant positive difference pre and post treatment as well as in comparison to Group I in both categories. The authors concluded yoga to be an effective adjunct therapy for patients with chronic pelvic pain and an effective option over NSAIDS for pain.
In the Pain Medicine journal, Huang et al.2017 presented a single-arm trial attempting to study the effects of a group-based therapeutic yoga program for women with chronic pelvic pain (CPP), focusing on severity of pain, sexual function, and overall well-being. The comprehensive program was created by a group of women’s health researchers, gynecological and obstetrical medical practitioners, yoga consultants, and integrative medicine clinicians. Sixteen women with severe pelvic pain of at least 6 months’ duration were recruited. The group yoga classes focused on lyengar-based techniques, and the subjects participated in group classes twice a week and home practice 1 hour per week for 6 weeks. The Impact of Pelvic Pain (IPP) questionnaire assessed how the participants’ pain affected their daily life activities, emotional well-being, and sexual function. Sexual Health Outcomes in Women Questionairre (SHOW-Q) offered insight to sexual function. Daily logs recorded the women’s self-rated pelvic pain severity. The results showed the average pain severity improved 32% after the 6 weeks, and IPP scores improved for daily living (from 1.8 to 0.9), emotional well-being (from 1.7 to 0.9), and sexual function (from 1.9 to 1.0). The SHOW-Q "pelvic problem interference" scale also improved from 53 to 23. The multidisciplinary panel concluded they found preliminary evidence that teaching yoga to women with CPP is feasible for pain management and improvement of quality of life and sexual function.
Whatever treatment we provide for our patients, we need to consider the individual and their often biased opinions or perceptions. Providing research and educating each patient on the efficacy behind the proposed therapy will likely impact their outcome. The Yoga for Pelvic Pain course can enhance a clinician’s understanding and allow them to better implement a potentially life-changing therapy for their clients.
Saxena, R., Gupta, M., Shankar, N., Jain, S., & Saxena, A. (2017). Effects of yogic intervention on pain scores and quality of life in females with chronic pelvic pain. International Journal of Yoga, 10(1), 9–15. http://doi.org/10.4103/0973-6131.186155
Huang, AJ, Rowen, TS, Abercrombie, P, Subak, LL, Schembri, M, Plaut, T, & Chao, MT. (2017). Development and Feasibility of a Group-Based Therapeutic Yoga Program for Women with Chronic Pelvic Pain. Pain Medicine. http://doi.org/10.1093/pm/pnw306
Assuring patients with chronic pain they are not crazy by explaining the neurophysiology behind what is happening in their brain and body can be life changing. Increasing our patients’ knowledge about physical conditions can reduce anxiety and provide hope. As a healthcare provider, being confident in your differential diagnosis skills can help narrow down the physical source of pain, weed out the psychological components, and connect the dots to the neurological influence on the patient’s persistent symptoms.
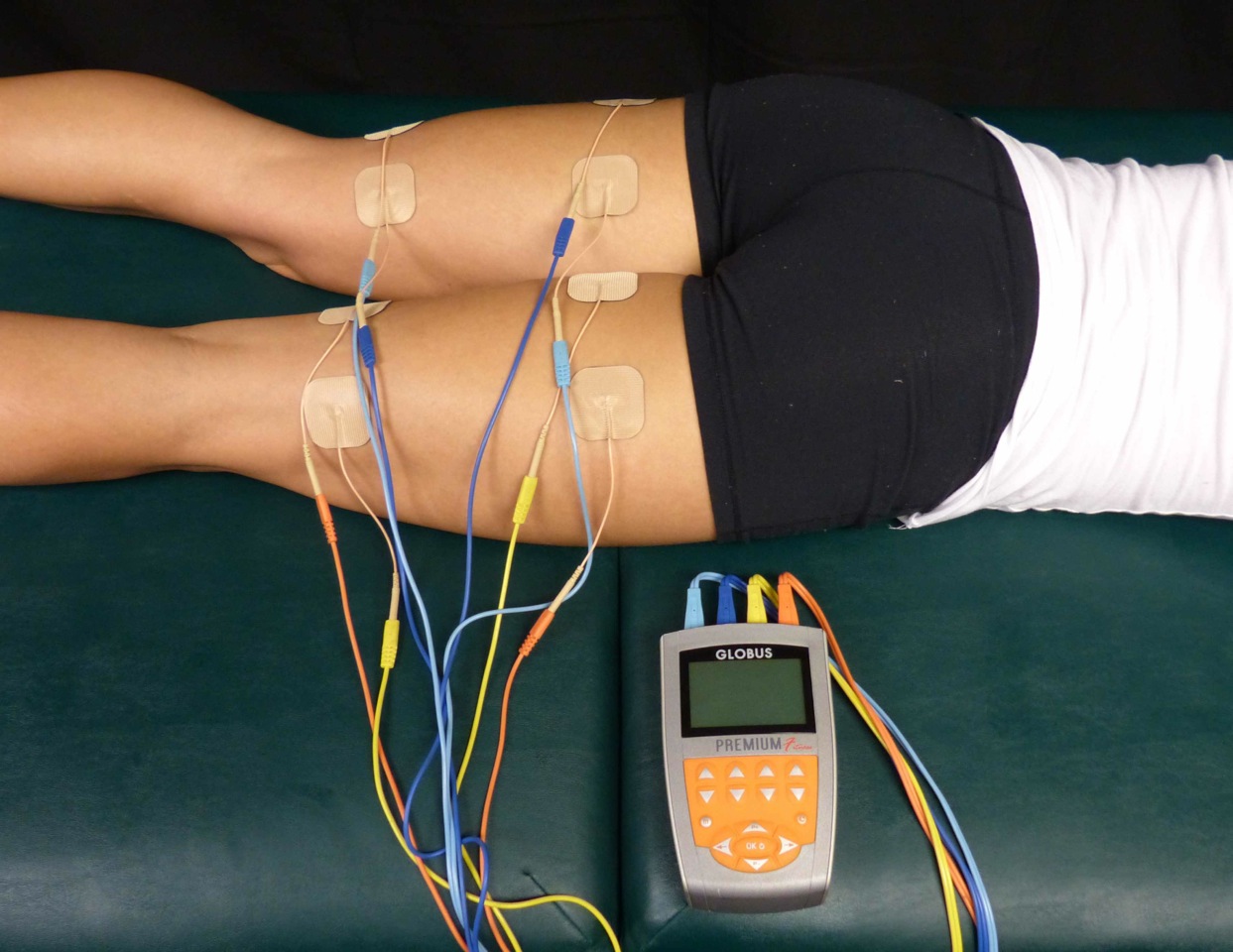 A 2015 article in Pain Medicine (Gurian et al) found a direct association between pain sensitivity and treatment of chronic pelvic pain. The study involved 58 women with at least 6 months of pelvic pain, and they were evaluated on pain threshold using transcutaneous electrical nerve stimulation before treatment and 6 months after a multidisciplinary approach to treatment of the pelvic pain. Pain intensity was also evaluated using the visual analog scale and the McGill questionnaire. Depending on the specific condition, treatment included manual therapy, physical therapy, pain medications, laparoscopy, oral contraceptives, nutrition intervention, or psychological support. After receiving treatment for 6 months, the pain threshold mean improved from 14.2 to 17.4. The effect sizes of 0.86 in the group with pain reduction and 0.53 in the group not achieving pain reduction were both within the 95% confidence interval. The authors concluded in this study that central sensitization does occur in patients with chronic pelvic pain, and treatment can reduce the general pain sensitivity of the patient.
A 2015 article in Pain Medicine (Gurian et al) found a direct association between pain sensitivity and treatment of chronic pelvic pain. The study involved 58 women with at least 6 months of pelvic pain, and they were evaluated on pain threshold using transcutaneous electrical nerve stimulation before treatment and 6 months after a multidisciplinary approach to treatment of the pelvic pain. Pain intensity was also evaluated using the visual analog scale and the McGill questionnaire. Depending on the specific condition, treatment included manual therapy, physical therapy, pain medications, laparoscopy, oral contraceptives, nutrition intervention, or psychological support. After receiving treatment for 6 months, the pain threshold mean improved from 14.2 to 17.4. The effect sizes of 0.86 in the group with pain reduction and 0.53 in the group not achieving pain reduction were both within the 95% confidence interval. The authors concluded in this study that central sensitization does occur in patients with chronic pelvic pain, and treatment can reduce the general pain sensitivity of the patient.
Kutch et al., (2015) performed a study regarding the change in men’s resting state of neuromotor connectivity as affected by chronic prostatitis or chronic pelvic pain syndrome (CP/CPPS), showing men are also subject to central sensitization. Fifty-five men (28 males with pelvic pain for at least 3 months and 27 healthy males) completed the study, with resting state functional magnetic resonance imaging detecting the functional connectivity of the pelvis with the motor cortex (pelvic-motor). The right posterior insula and pelvic-motor functional connectivity was found to be significantly different in men with chronic pelvic pain and prostatitis versus the healthy control group. Contraction of the pelvic floor corresponded with activation of the medial aspect of the motor cortex, while the left motor cortex was more associated with contraction of the right hand. The authors concluded this relationship may explain the viscerosensory and motor processing changes that occur in men with CP/CPPS and could be the most important marker of brain function alteration in this group of patients.
As more research is being done on the neurophysiological level of pain, more truth can support the “it’s all in your head” accusation. However, it is a positive light to shed for a patient. The brain is powerful and controls how pain is perceived globally. Proper treatment of a chronic pelvic floor condition, for women and men, can help reduce stress on the brain and lessen pain sensitivity and perception in our patients. Never let a patient pursue the self-perception that they are crazy. Explain central sensitization and how sometimes the brain wins in the war of “mind over matter”; however, give them hope, explaining how the proper treatment can lessen the intensity of the battle wounds.
Maria Beatriz Ferreira Gurian, Omero Benedicto Poli Neto, Julio Cesar Rosa e Silva, Antonio Alberto Nogueira, Francisco Jose Candido dos Reis. (2015). Reduction of Pain Sensitivity is Associated with the Response to Treatment in Women with Chronic Pelvic Pain. Pain Medicine. 16 (5) 849-854; DOI: 10.1111/pme.12625
Kutch, J. J., Yani, M. S., Asavasopon, S., Kirages, D. J., Rana, M., Cosand, L., … Mayer, E. A. (2015). Altered resting state neuromotor connectivity in men with chronic prostatitis/chronic pelvic pain syndrome: A MAPP: Research Network Neuroimaging Study. NeuroImage : Clinical, 8, 493–502. http://doi.org/10.1016/j.nicl.2015.05.013
A recent article titled "Pain, Catastrophizing, and Depression in Chronic Prostatitis/Chronic Pelvic Pain Syndrome" describes the variations in patient symptom report and perception of the condition. The article describes the evidence-based links between chronic pelvic pain and anxiety, depression, and stress, and highlights the important role that coping mechanisms have in reported pain and quality of life levels. One of the ways in which a provider can assist in patient perception of health or lack thereof is to provide current information about the condition, instruct the patient in pathways for healing, and provide specific care that aims to alleviate concurrent neuromusculoskeletal dysfunction.
Most pelvic rehabilitation providers will have graduated from training without being informed about chronic pelvic pain syndromes. And as most pelvic rehabilitation providers receive their pelvic health knowledge from continuing education courses, unless a therapist has attended coursework specifically about male patients, the awareness of male pelvic dysfunctions remains low. If you are interested in learning about male pelvic health issues, the Institute introduces participants to male pelvic health in the Level 2A series course. The practitioner who would like more information about male patients can attend the Male Pelvic Floor Function, Dysfunction, and Treatment course that is offered in Torrance, CA at the end of this month.
The authors in this study point out that chronic pelvic pain is not a disease, but rather is a symptom complex. Despite the persistent attempts to identify a specific pathogen as the cause of prostatitis-like pain, this article states that "…no postulated molecular mechanism explains the symptoms…" As with any other chronic pain condition, research in pain sciences tells us that behavioral tendencies such as catastrophizing is not associated with improved health. The authors utilized a psychotherapy model in developing a cognitive-behavioral symptom management approach and found significant reductions in CPP symptoms. The relevance of this information for our patient population includes having the ability to screen our patients for depression, to recognize tendencies to catastrophize, and to implement useful strategies for our patient.
What does your facility currently use as a depression screening tool? Having this information at hand when communicating with a referring provider is very helpful. Explaining the biology of the vicious cycle of emotional stress and pain responses can help a patient understand why following up on a referral to a psychologist or counselor may be helpful towards his health. Identifying catastrophizing as the patient who is hypervigilent about symptoms, ruminates about his condition, expresses an attitude of helplessness, or magnifies the threat of the perceived pain can aid in identification of the patient who needs more than a few stretches, a TENS unit, or manual therapy.
A new course offered this year by the Institute will provide excellent foundational background information as well as practical patient care techniques about emotional and psychological principles that influence chronic pain. This course, Integrating Meditation and Neuropsych Principles to Maximize Physical Therapy Interventions, is instructed by Nari Clemons, a physical therapist who excels in pelvic rehabilitation, and Shawn Sidhu, a psychiatrist with a special interest in mind body medicine. The course is offered only one time this year, in September in Illinois, so sign up early!











































