Recent data suggests that there are about 4 million American women diagnosed with endometriosis, but that 6/10 are not diagnosed. Currently, using the gold standard for diagnosis there are potentially 6 million American woman that may experience the sequelae of endometriosis without having appropriate management or understanding the cause of their symptoms.
The gold standard for endometriosis is laparoscopy either with or without histologic verification of endometrial tissue outside of the uterus. However, there is a poor correlation between disease severity and symptoms. The Agarwal et al study suggests a shift to focus on the patient rather than the lesion and that endometriosis may better be defined as “menstrual cycle dependent, chronic, inflammatory, systemic disease that commonly presents as pelvic pain”. There is often a long delay in symptom appreciation and diagnosis that can range from 4-11 years. The side effects of this delay are to the detriment of the patient; persistent symptoms and effect of quality of life, development of central sensitization, negative effects on patient-physician relationship. If this disease continues to go untreated it may affect fertility and contribute to persistent pelvic pain.
 The authors suggest a clinical diagnosis with transvaginal ultrasound for patients presenting with persistent or cyclic pelvic pain, patient history, have symptoms consistent with endometriosis, or other findings suggestive of endometriosis. The intention of using transvaginal ultrasound is to make diagnosis more accessible and limit under diagnosis. It is not intended to minimize laparoscopy as a diagnostic tool or treatment option.
The authors suggest a clinical diagnosis with transvaginal ultrasound for patients presenting with persistent or cyclic pelvic pain, patient history, have symptoms consistent with endometriosis, or other findings suggestive of endometriosis. The intention of using transvaginal ultrasound is to make diagnosis more accessible and limit under diagnosis. It is not intended to minimize laparoscopy as a diagnostic tool or treatment option.
The algorithm for a clinical diagnosis evaluates patient presentation of the following:
- Symptoms including persistent or cyclic pelvic pain, dysmenorrhea or painful menstruation cramps, deep dyspareunia or pain with deep vaginal penetration, cyclic dyschezia or straining for soft stools, cyclic dysuria or pain with urination, cyclic catamenial symptoms located in other systems such as acne or vomiting.
- Assessment of patient history including infertility, current chronic pelvic pain, or painful periods as an adolescent, previous laparoscopy with diagnosis, painful periods that are not responsive to NSAIDS, and a family history.
- Physical exam physicians assess for nodules in cul de sac, retroverted uterus, mass consistent with endometriosis, visible or obvious external endometrioma. Imaging should be ordered or performed.
- Clinical signs would consist of endometrioma with US, presence of soft markers (sliding sign) this is where the fundus of the uterus is compared to its neighboring structures and can indicate the immobility of those structures, and nodules or masses.
Of course, there are differential diagnosis for endometriosis, and those are symptoms of non-cyclical patterns of pain and bladder/bowel dysfunction that would indicate IBS, UTI, IC/PBS. A history of post-operative nerve entrapment of adhesions. Examination positive for pelvic floor spasm, severe allodynia in vulva and pelvic floor, masses such as fibroids. It is important to note that these other diagnoses can coexist with endometriosis and do not rule out possible endometriosis diagnosis.
Hopefully, diagnosing individuals earlier and possibly at a younger age would limit the disease severity and symptoms. This would allow this population to limit the possibility of central sensitization and pain persistence that can affect so much of daily life. Earlier diagnosis may affect infertility and allow this population to make informed decisions about family and career from a place of empowerment.
Agarwal SK, Chapron C, Giudice LC, Laufer MR, Leyland N, Missmer SA,Singh SS, Taylor HS, "Clinical diagnosis of endometriosis: a call to action", American Journal of Obstetrics and Gynecology (2019), doi: https://doi.org/10.1016/j.ajog.2018.12.039.
September is Gynae Cancer Awareness Month – but how aware are we as clinicians of the signs and symptoms, the epidemiology and the sequalae of treatment afterwards? As pelvic rehab specialists, we have the privilege of helping women live well after cancer treatment ends, both on a ‘local’ pelvic area (bladder, bowel, sexual and pelvic pain management strategies) but also on a more ‘global’ level – dealing with issues such as cancer related fatigue, bone health and cardiovascular concerns.
 We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
This can present a clinical conundrum – often pelvic rehab therapists are nervous when working with a patient who has a current or previous gynecologic cancer diagnosis, but similarly oncology rehab specialists may have qualms about dealing with pelvic health issues, with the result that these women fall through the cracks and do not have their pelvic health issues managed properly (or at all). Theodore Roosevelt once said ‘No one cares how much you know, until they know how much you care’ and this is especially relevant for oncology pelvic rehab. Often you may be the first clinician to ask about bladder, bowel or sexual function or dysfunction. An understanding of the effects of cancer treatments on the pelvis is important but so too is the wealth of information you may already have about bladder, bowel and sexual health as well as neuroscience and pain education.
The most important thing is to ask these women about their pelvic health concerns – the National Coalition for Cancer Survivorship defined cancer survivorship as extending from ‘the time of diagnosis and for the balance of life’. An emphasis on quality of life has been emphasised – if we know that cancer survivors may not independently volunteer information about their pelvic floor dysfunction, it is our responsibility to ask the questions and comprehensively treat and advocate for these women, in order to help them live well after cancer treatment ends.
- Hazewinkel MH. Sprangers MA, Velden Jvd, Vaart CH, Stalpers LJ, Burger MP ‘Longterm cervical cancer survivors suffer from pelvic floor dysfunction symptoms: A cross-sectional matched cohort study’ Gynecol Oncol 2010;117(2):381-6
- Erekson EA, Sung VW, Disilvestro PA, Myers DL ‘Urinary symptoms and impact on quality of life in women after treatment for endometrial cancer’ Int Urogynecol J 2009;20(2):159-63
- Malone P, Danaher D, Galvin R, Cusack T ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’ Physiotherapy Practice and Research 38(2017)93-102
More than a year ago, after working on updating the pelvic floor series courses PF1, 2A and 2B, the Institute turned our attention to the final course in our popular series, PF3. To determine what content our participants wanted to learn about in the last continuing education course of the series, we asked that exact question. From a large survey of therapists who had taken all or most of the courses in the pelvic core series, we collected detailed data from therapists about what was needed to round out their comprehensive training. The results of that survey guided hundreds (and hundreds!) of hours of work completed by a team of instructors. This month, in the beautiful city of Denver, the three instructors who created the Capstone course will share their wisdom, clinical experiences, as well as their thoughtfully-designed lectures and labs. You will have an opportunity to learn in depth about topics covered in the prior courses in the series.
Such topics include lifespan issues and health issues common to different ages, conditions of polycystic ovarian syndrome, endometriosis, infertility, pelvic organ prolapse and surgeries, pelvic fascial anatomy, pharmacology and nutrition. Lab components are detailed and comprehensive for working with specific common implications from conditions in pelvic dysfunction or surgery. This course focuses on the female pelvis, including diving into the complexities of female pelvic health issues. The instructors have all worked in the field for many years, are experienced in working with complex patient presentations, and all excel at manual therapies. I asked each of them to briefly share thoughts about the Capstone course that they each dedicated the last year in developing; following you can read their thoughts.
 "I'm excited for every therapist who will take this course, as it is made to help you approach your practice at a whole new level. We are eager to help your hands work dynamically with more intelligence and how to tackle complex restrictions in the pelvis and abdomen that go far beyond releasing muscles. Additionally, the practitioners will raise their capacity of recognizing and helping the patient manage complex conditions, such as endometriosis, PCOS, fibroids, and IBS."
"I'm excited for every therapist who will take this course, as it is made to help you approach your practice at a whole new level. We are eager to help your hands work dynamically with more intelligence and how to tackle complex restrictions in the pelvis and abdomen that go far beyond releasing muscles. Additionally, the practitioners will raise their capacity of recognizing and helping the patient manage complex conditions, such as endometriosis, PCOS, fibroids, and IBS."
 "One of the best things about the Capstone course is that it provides the participants tools to treat more complicated patients. Topics such as endocrinology, oncology, vulvar dermatology, and surgical procedures are addressed, which will complete the picture for some of those patients that are hard to treat due to the complexity of their case. This knowledge, along with more advanced manual treatment techniques, will add to the skill set of the participants to improve their treatment outcomes. I am excited for the participants to combine their current clinical skills along with some new knowledge and techniques to be able to treat the whole person when working with complex and challenging patients."
"One of the best things about the Capstone course is that it provides the participants tools to treat more complicated patients. Topics such as endocrinology, oncology, vulvar dermatology, and surgical procedures are addressed, which will complete the picture for some of those patients that are hard to treat due to the complexity of their case. This knowledge, along with more advanced manual treatment techniques, will add to the skill set of the participants to improve their treatment outcomes. I am excited for the participants to combine their current clinical skills along with some new knowledge and techniques to be able to treat the whole person when working with complex and challenging patients."
 "Designing and creating Capstone with Nari and Allison was an incredible experience. My own knowledge and clinical expertise grew profoundly while researching and writing this material. Capstone is designed to really take the experienced pelvic health therapist to the next level of understanding and treating more complex patients. I can't wait to see the impact this material has on participants and their patients."
"Designing and creating Capstone with Nari and Allison was an incredible experience. My own knowledge and clinical expertise grew profoundly while researching and writing this material. Capstone is designed to really take the experienced pelvic health therapist to the next level of understanding and treating more complex patients. I can't wait to see the impact this material has on participants and their patients."
There is still time to register for the few remaining seats in Denver this weekend!
This post was written by H&W instructor Michelle Lyons, PT, MISCP, who authored and instructs the course, Special Topics in Women’s Health: Endometriosis, Infertility & Hysterectomy. She will be presenting this course this February!

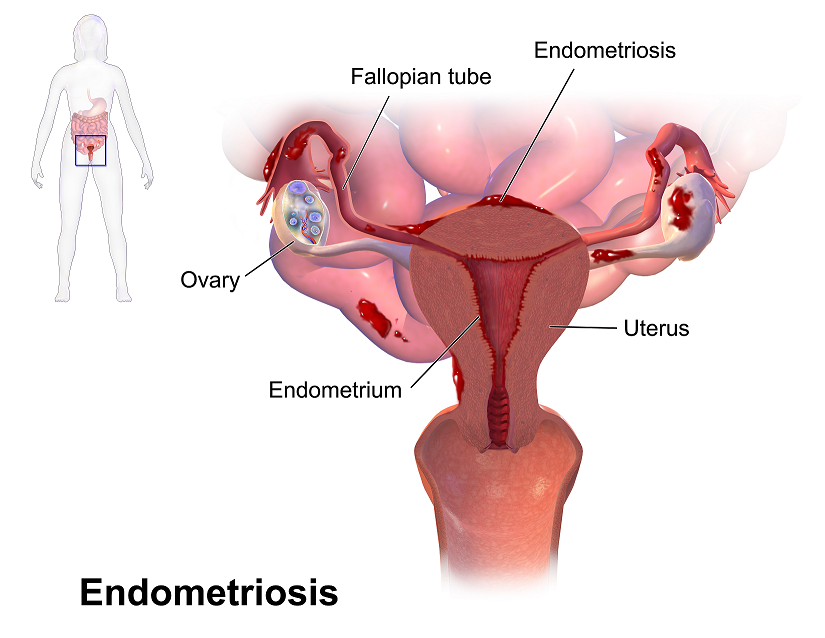
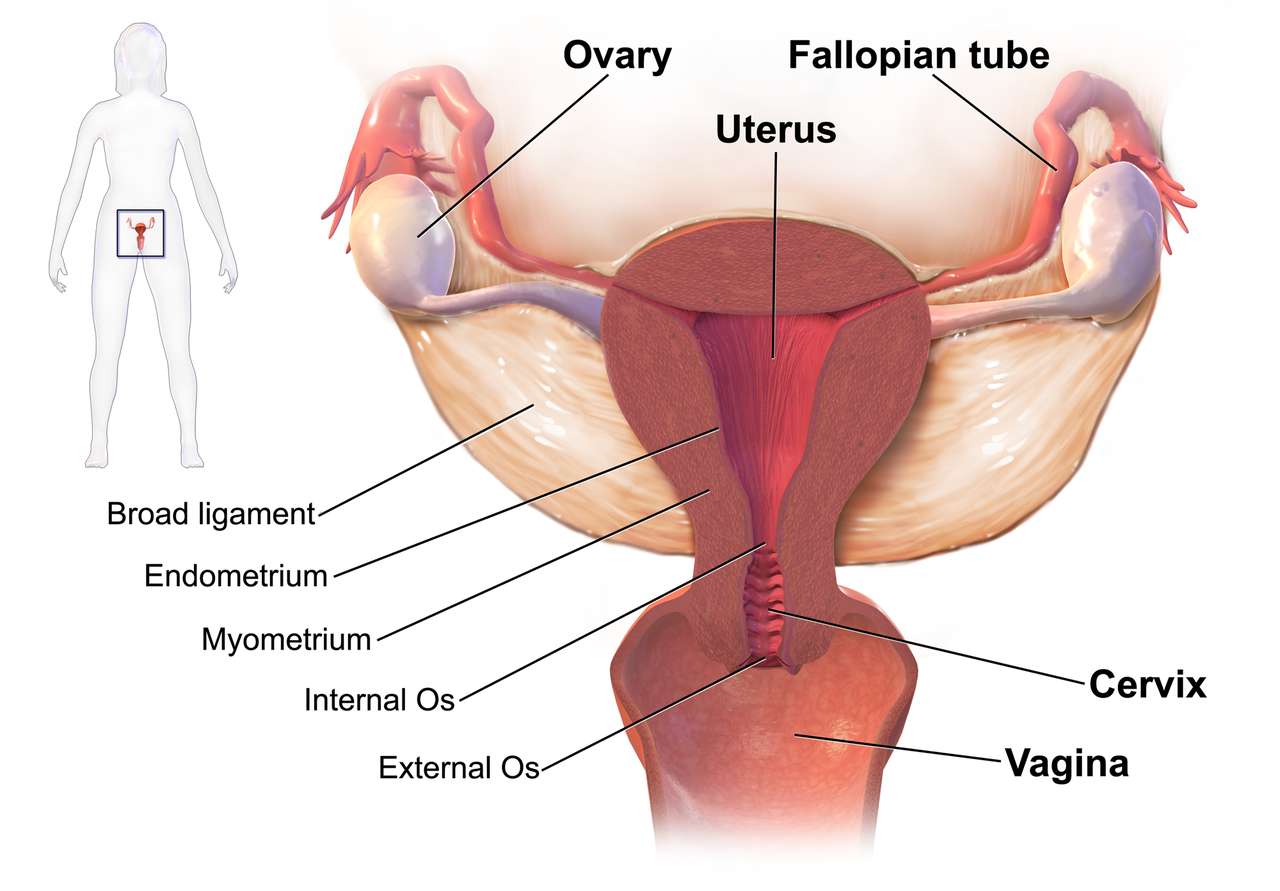
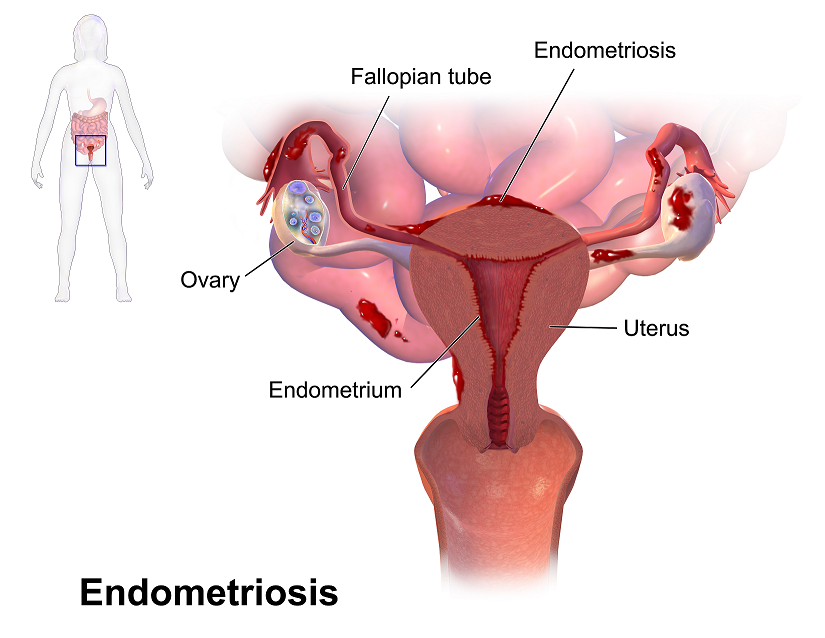
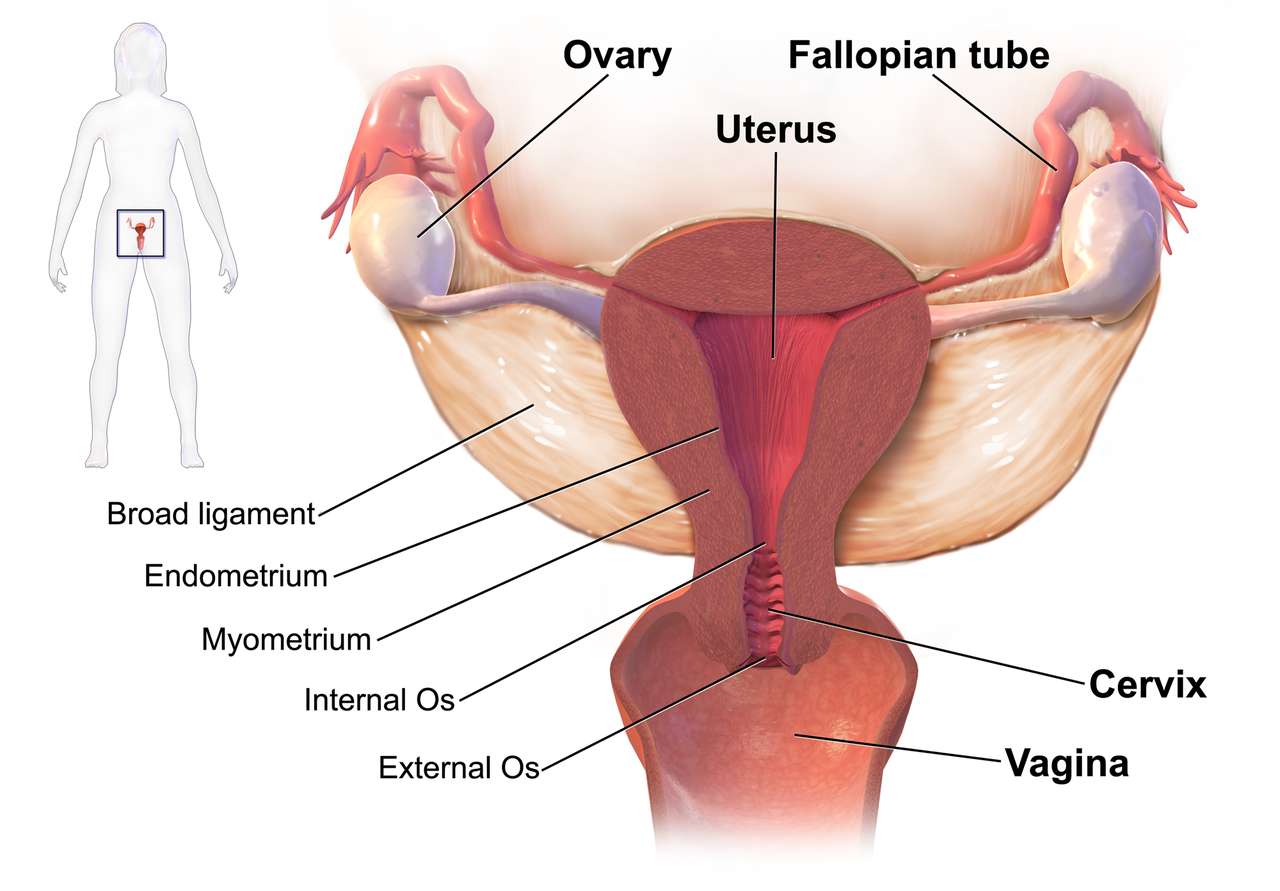
Endometriosis is a common gynaecological disorder, affecting up to 15% of women of reproductive age. Because endometriosis can only be diagnosed surgically, and also because some women with the disease experience relatively minor discomfort or symptoms, there is some controversy regarding the estimates of prevalence, with some authorities stating that as many as one and three women may have endometriosis (Eskenazi & Warner 1997)
There is a wide spectrum of symptoms of endometriosis, with little or no correlation between the acuteness of the disease and the severity of the symptoms (Oliver & Overton 2014). The most commonly reported symptoms are severe dysmenorrhoea and pelvic pain between periods. Dyspareunia, dyschezia and dysuria are also commonly seen. These pain symptoms can be severe and have been reported to lead to work absences by 82% of women, with an estimated cost in Europe of €30 billion per year (EST 2005). Secondary musculoskeletal impairments caused by may include: lumbar, sacroiliac, abdominal and pelvic floor pain, muscle spasms/ myofascial trigger points, connective tissue dysfunction, urinary urgency, scar tissue adhesion and sexual dysfunction (Troyer 2007) – all of which may be responsive to skilled pelvic rehab intervention.
Endometriosis can lead to inflammation, scar tissue and adhesion formation and myofascial dysfunction throughout the abdominal and pelvic regions. This can set up a painful cycle in the pelvic floor muscles secondary to the decrease in pelvic and abdominal organ/muscle/fascia mobility which can subsequently lead to decreased circulation, tight muscles, myofascial trigger points, connective tissue dysfunction and pain and possible neural irritation.
Abdominal trigger points and pain can be commonly seen after laparascopic surgery for diagnosis or treatment. We know that fascially, the abdominal muscles are closely connected with the pelvic floor muscles and dysfunction in one group may trigger dysfunction in the other, as well as causing associated stability, postural and dynamic stability issues.
The pain created by muscle tension and dysfunction, may lead to further pain and increasing central sensitisation and further disability. Unfortunately for the endometriosis patient, as well as dealing with the problems already associated with endometriosis, she may also develop a spectrum of secondary musculo-skeletal problems, including pelvic floor dysfunction – and for some patients this may actually be responsible for the majority of their pain (Troyer 2007).
The skilled pelvic rehab therapist has much to offer this under-served patient population in terms of reducing pain and dysfunction, educating regarding self-care and exercise and helping to restore quality of life. Interested in learning more? Join me for my new course: ‘Special Topics in Women’s Health: Endometriosis, Infertility & Hysterectomy’ in San Diego this February or Chicago in June.
This post was written by H&W instructor Michelle Lyons, PT, MISCP, who authored and instructs the course, Special Topics in Women’s Health: Endometriosis, Infertility & Hysterectomy. She will be presenting this course this February!

Endometriosis is a common gynaecological disorder, affecting up to 15% of women of reproductive age. Because endometriosis can only be diagnosed surgically, and also because some women with the disease experience relatively minor discomfort or symptoms, there is some controversy regarding the estimates of prevalence, with some authorities stating that as many as one and three women may have endometriosis (Eskenazi & Warner 1997)
There is a wide spectrum of symptoms of endometriosis, with little or no correlation between the acuteness of the disease and the severity of the symptoms (Oliver & Overton 2014). The most commonly reported symptoms are severe dysmenorrhoea and pelvic pain between periods. Dyspareunia, dyschezia and dysuria are also commonly seen. These pain symptoms can be severe and have been reported to lead to work absences by 82% of women, with an estimated cost in Europe of €30 billion per year (EST 2005). Secondary musculoskeletal impairments caused by may include: lumbar, sacroiliac, abdominal and pelvic floor pain, muscle spasms/ myofascial trigger points, connective tissue dysfunction, urinary urgency, scar tissue adhesion and sexual dysfunction (Troyer 2007) – all of which may be responsive to skilled pelvic rehab intervention.
Endometriosis can lead to inflammation, scar tissue and adhesion formation and myofascial dysfunction throughout the abdominal and pelvic regions. This can set up a painful cycle in the pelvic floor muscles secondary to the decrease in pelvic and abdominal organ/muscle/fascia mobility which can subsequently lead to decreased circulation, tight muscles, myofascial trigger points, connective tissue dysfunction and pain and possible neural irritation.
Abdominal trigger points and pain can be commonly seen after laparascopic surgery for diagnosis or treatment. We know that fascially, the abdominal muscles are closely connected with the pelvic floor muscles and dysfunction in one group may trigger dysfunction in the other, as well as causing associated stability, postural and dynamic stability issues.
The pain created by muscle tension and dysfunction, may lead to further pain and increasing central sensitisation and further disability. Unfortunately for the endometriosis patient, as well as dealing with the problems already associated with endometriosis, she may also develop a spectrum of secondary musculo-skeletal problems, including pelvic floor dysfunction – and for some patients this may actually be responsible for the majority of their pain (Troyer 2007).
The skilled pelvic rehab therapist has much to offer this under-served patient population in terms of reducing pain and dysfunction, educating regarding self-care and exercise and helping to restore quality of life. Interested in learning more? Join me for my new course: ‘Special Topics in Women’s Health: Endometriosis, Infertility & Hysterectomy’ in San Diego this February or Chicago in June.
Recent research in The Journal of Pediatric and Adolescent Gynecology points to the alarming number of young women who present with pelvic pain who in fact also have endometriosis. Dr. Opoku-Anane and Dr. Laufer report that prevalence rates of endometriosis in an adolescent gynecology population have likely been underestimated (reported range of 25-47%) and that with advanced surgical methods the rates have been estimated to be as high as 73% in those who have pelvic pain. In their retrospective study, 117 subjects ages 12-21 completed laparoscopic examination for endometriosis. These subjects did not previously respond to non-steroidal anti-inflammatories or to oral contraceptives, and they were all referred for evaluation of chronic pelvic pain. In addition to collecting data about patient symptoms, the stage and descriptions of any endometrial lesions were documented.
A remarkable 115 of the 117 subjects (98%) presented with Stage I or II endometriosis as defined by the American Society for Reproductive Medicine guidelines. (Click here for the link to a detailed patient education document from the ASRM that describes endometriosis as well as staging.) The median age for onset of menarche in this population was 12 years old, and the median age of first symptoms reported occurred at age 13. Nearly 16% of the subjects also reported gastrointestinal complaints, menstrual irregularity in nearly 8%, and 76% of the participants reported a family history that included endometriosis, severe dysmenorrhea, and/or infertility. The authors of this research point out that advances made in surgical technique, both from a technological standpoint and a physician skill level, may be contributing factors in the increased rates of diagnosis of endometriosis.The authors also point out that it is yet unknown if early diagnosis and treatment will lead to improved outcomes in this population.
If you are interested in learning more about endometriosis in general, click here to follow the link to a free, full text article in PubMed Central. The article was first published in 2008, and even though advances in surgical diagnosis have been made, most of the information related to symptoms, medical treatment, and related risks remain significantly unchanged. In relation to etiology of endometriosis, one study that has set forth an environmental risk for endometriosis can be accessed here. Dr. C. Matthew Peterson, one of the researchers involved with the ENDO study, presented at the 2011 International Pelvic Pain Society meeting, and he encouraged all present to consider implementing strategies to minimize risks from chemicals in our daily lives. The Environmental Protection Agency offers advice towards protecting our health that can be accessed here. If environmental hazards are influencing the onset or progression of conditions such as endometriosis, it is in our best interest to reduce these risks. Consider not only the product exposure at home, but also at the workplace, and request less toxic products including cleaners when able.
In relation to pelvic rehabilitation, patients who present with pelvic pain or other pelvic health issues due to endometriosis often find relief when working with pelvic rehab providers. While surgery may be critical in reducing severe adhesions, maximizing tissue health and patient mobility and function is a job in which we can all actively participate. The evaluation and treatment of pelvic pain is instructed at various levels of depth in all of the main series courses as well as in many other courses offered at the Herman & Wallace Pelvic Rehabilitation Institute.