Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
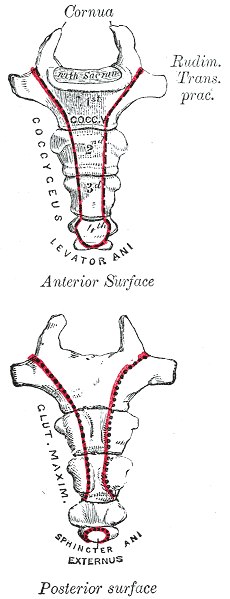
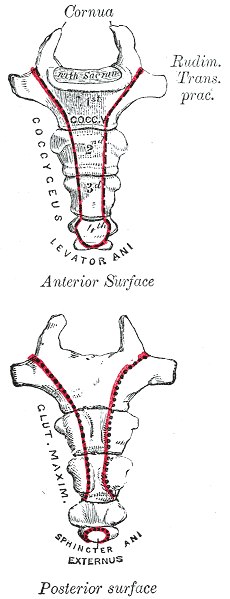
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sitting to standing. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: (1)
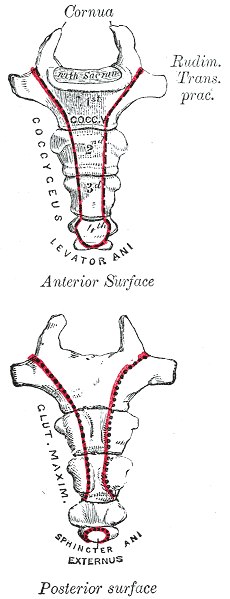
- Anterior Tip: Iliococcygeus and pubococcygeus, Sacrococcygeal ligament
- Lateral: Coccygeal muscles that run parallel with the sacrospinous ligament
- Posteriorly: Fibers of gluteus maximus and sacrotuberous ligament
Along with serving as a major attachment site for the above structures it provides support for weight bearing in the seated position and provides structural support for the anus. However, the coccyx is only 10% weight-bearing, so what seems to go wrong that this bone is taking the brunt of the weight-bearing? Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall or an internal trauma like a difficult childbirth (1,2).
In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulted in coccyx pain were from the use of instruments such as forceps delivery or vacuum-assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth (3). Other causes of coccyx pain can be non-traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction (1).
When assessing a patient with coccyx pain, it is also of the utmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retro rectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign and if excision is necessary. Quite often, these masses can be felt as a bulge on rectal examination (4, 5).
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain (1). Special wedge-shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain.
Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx (1). Unique taping methods demonstrated in video by Dr. Abbate can be used as a follow-up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroiliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered. Luckily, conservative treatment is successful in about 90% of cases (1).
Join Lila Abbate in her upcoming Coccydynia and Painful Sitting remote course on December 14th. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
References:
- Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
AUTHOR BIO
Lila Abbate, PT, DPT, OCS, WCS, PRPC

Lila Abbate (she/her) is the Director/Owner of New Dimensions Physical Therapy with locations in Roslyn, Long Island, and the Noho Section of New York City. Dr. Abbate graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release.
She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series and the Pregnancy and Postpartum Rehabilitation courses. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
She is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, and the International Pelvic Pain Society. Dr. Abbate is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.

Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sitting to standing. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: (1)
- Anterior Tip: Iliococcygeus and pubococcygeus, Sacrococcygeal ligament
- Lateral: Coccygeal muscles that run parallel with the sacrospinous ligament
- Posteriorly: Fibers of gluteus maximus and sacrotuberous ligament
Along with serving as a major attachment site for the above structures it provides support for weight bearing in the seated position and provides structural support for the anus. However, the coccyx is only 10% weight-bearing, so what seems to go wrong that this bone is taking the brunt of the weight-bearing? Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall or an internal trauma like a difficult childbirth (1,2).
In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulted in coccyx pain were from the use of instruments such as forceps delivery or vacuum-assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth (3). Other causes of coccyx pain can be non-traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction (1).
When assessing a patient with coccyx pain, it is also of the utmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retro rectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign and if excision is necessary. Quite often, these masses can be felt as a bulge on rectal examination (4, 5).
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain (1). Special wedge-shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain.
Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx (1). Unique taping methods demonstrated in video by Dr. Abbate can be used as a follow-up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroiliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered. Luckily, conservative treatment is successful in about 90% of cases (1).
Join Lila Abbate in her upcoming Coccydynia and Painful Sitting remote course on December 14th. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
References:
- Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
AUTHOR BIO
Lila Abbate, PT, DPT, OCS, WCS, PRPC

Lila Abbate (she/her) is the Director/Owner of New Dimensions Physical Therapy with locations in Roslyn, Long Island, and the Noho Section of New York City. Dr. Abbate graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release.
She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series and the Pregnancy and Postpartum Rehabilitation courses. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
She is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, and the International Pelvic Pain Society. Dr. Abbate is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.
So often as “pelvic floor therapists”, our name and scope of manual treatment can seem to center around stretching or strengthening pelvic floor muscles. But, if you have been practicing for a while, maybe you want to go deeper.
We talk in the Pelvic Function Series about “zooming out” (considering postural, musculoskeletal, breathing, autonomics, and pressure systems). We also have noticed in our field an increased emphasis on the nervous system for regulating the system.
We also talk about “zooming in”, bringing our focus inside the pelvis. That could be pelvic floor muscles, but if we want to zoom in even deeper, we may start to look at peripheral nerves, supportive ligaments, and the interplay between bones, ligaments, fascia, and muscles that could be keeping pain, dysfunction, over-activity, or tension syndromes alive.
The sacrospinous and sacrotuberous ligaments are incredible structures we often don’t give enough attention to. Both the SS and ST ligaments have coccyx attachments and can affect coccyx pain, position, and create tension in the coccygeal nerves.
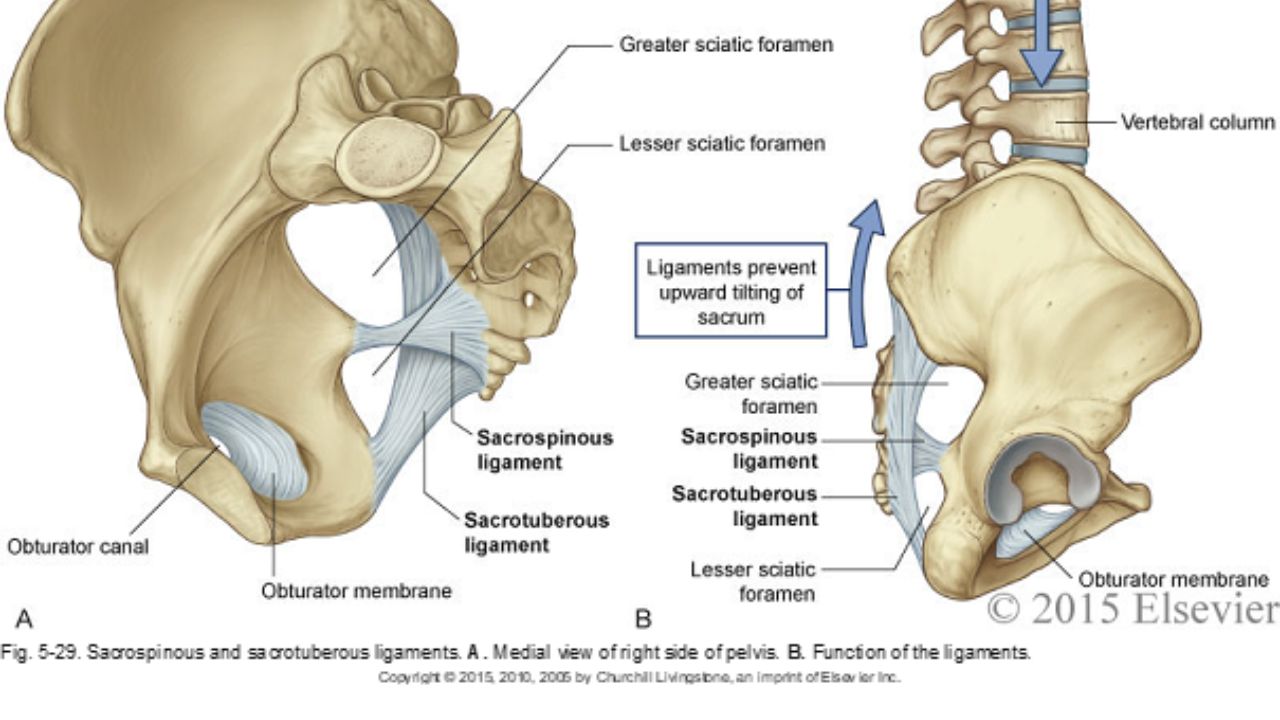
The entire support and structure of the posterior-lateral pelvic bowl is constructed from these two ligaments (with the posterior longitudinal SI ligament). They can become tight and rigid from bearing the burden of stabilizing. The SS ligament may even hold the support for the vaginal canal after hysterectomy. These two ligaments create the greater and lesser sciatic foramen and the nerves of the sacral plexus (pudendal, sciatic, gluteal nerves, and posterior femoral cutaneous nerves) all have intimate relationships and are affected by the tension in these ligaments.
In the Sacral Nerve Manual Assessment and Treatment Class, we learn techniques to deeply release these ligaments (without stressing our hands), external fascial techniques for the coccyx fascia and ligaments, releases for the deep hip muscles that these nerves run through, and how to individually do neuro-lymphatic work to decrease perineural thickening and swelling within the nerve that prevents pain-free gliding. We use differential diagnosis, manual technique, home program, and intricate anatomy study to learn how to get closer to the root of dysfunction in the pelvic floor and posterior gluteals, saddle region, and leg. Come join us on May 11&12 to add depth to your toolbox and understanding of the anatomy of the pelvic nerves.
*Images used with permission from Elsevier 2015.
AUTHOR BIO:
Nari Clemons, PT, PRPC

Nari Clemons was born and raised in the Midwest before moving to Portland, Oregon. At Herman & Wallace, Nari teaches the Pelvic Function Series (PF1, 2A, 2B, and PF Capstone). She was one of three co-authors. Her passion is taking difficult concepts and techniques and simplifying them so that participants can leave courses with confidence, enthusiasm, and feeling empowered in their clinical practice.
Nari graduated from the Medical College of Ohio in consortium with the University of Toledo, with a degree in physical therapy. She owns a private practice, Portland Pelvic Therapy, where she focuses on pelvic, abdominal, and neural issues. Nari has studied visceral and neural manipulation extensively, traveling as far as France to take courses from Jean Pierre Barral. She is also a registered yoga teacher, having trained at the Yoga Center of Seattle and It’s Yoga. Additionally, she has accumulated months of time at intensive meditation retreats. Nari’s approach to the body is holistic and eclectic while being well-rooted in research.
Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She has obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012. Dr. Abbate is Senior Faculty with Herman & Wallace and can be found instructing the Pelvic Floor Series as well as her own courses Coccydynia and Painful Sitting and Bowel Pathology and Function.
Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sitting to standing. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence:¹
- Anterior Tip: Iliococcygeus and pubococcygeus, Sacrococcygeal ligament
- Lateral: Coccygeal muscles which runs parallel with the sacrospinous ligament
- Posteriorly: Fibers of gluteus maximus and sacrotuberous ligament
Along with serving as a major attachment site for the above structures it provides support for weight bearing in the seated position and provides structural support for the anus. However, the coccyx is only 10% weightbearing, so what seems to go wrong that this bone is taking the brunt of the weightbearing? Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall or an internal trauma like a difficult childbirth.1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulted in coccyx pain were from the use of instruments such as forceps delivery or vacuum-assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non-traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction.¹ When assessing a patient with coccyx pain, it is also of the utmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retro rectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign and if excision is necessary. Quite often, these masses can be felt as a bulge on rectal examination.4,5
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain.1 Special wedge-shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain. Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx.1 Unique taping methods demonstrated in video by Dr. Abbate, can be used as a follow-up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroiliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered.
Luckily conservative treatment is successful in about 90% of cases.¹ Join Lila Abbate in her upcoming Coccydynia and Painful Sitting remote course on March 31st. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
References:
1. Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
2. Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
Coccydynia and Painful Sitting
Course Dates: March 31, June 17, September 22, and December 10
Price: $175
Experience Level: Intermediate
Contact Hours: 5.5
Description: Coccyx pain is a common, frustrating condition for the patient who often has difficulty sitting, one of the most important tasks necessary for daily activity. Patients who find help from a pelvic rehabilitation provider have often experienced pain near the tailbone for long periods of time, leading to chronic pain in addition to neuromusculoskeletal dysfunctions. This one-day, remote continuing education course allows the therapist to focus on this vital, sensitive area to learn and refine skills in assessment and treatment. Anatomy, pathology, and palpation skills of the coccyx region are instructed.
This course includes a video lab on both internal and external neuromuscular taping techniques which can immediately be applied in the clinic. This course also includes a review of seating options to reduce pain.
Fun fact: Did you know that the pelvis fans and folds just like the hand and foot?
Ischial tuberosities change position and move medial to lateral and back based on the functional task. Pelvic floor muscles length and fascial integrity and its ability to conform to demands become an important factor in treating painful sitting.
The one-day course gives you a basic anatomy review and discusses the biomechanics of sitting and the difference of quadruped and its assessment. External coccyx treatments are explained and reviewed through video format along with a discussion to assist patients in making good decisions using sitting relief pillows. You will learn 5 basic tips to know if your patient has true coccydynia or if the pain is being driven from elsewhere up or down the chain. A review of the literature and how the medical community views basic coccydynia and which medical interventions can assist patients with long-standing sitting pain.
Most people spend their days alternating between sitting and standing, changing positions constantly. How many of us take the time to think about the position of our coccyx, ilia, or sacrum? The coccyx typically is minimally weight-bearing in sitting, about 10%, just like the fibula. However, it can become a major pain generator if the biomechanics of the ilia, sacrum, and femoral head positions are not quite right.
Coccydynia and Painful Sitting is a course that can be related to all populations that physical therapists treat. A lot of patients will state “my pain is worse with sitting” which can mean thoracic pain, low back/sacral pain, and even lower extremity radicular pain.
Coccyx pain patients often have more long-standing pain conditions than other patient types. For the most part, the medical community does not know what to do with this tiny bone that causes all types of havoc with patient pain levels. Lila shares that "Sometimes treating a traumatic coccydynia patient seems so simple and I am bewildered as to why patients are suffering so long - and other times, their story is so complex that I wonder if I can truly help."
Lila Abbate discussed this in her past blog, Case Studies in Coccyx Pain. She wrote that "The longer I am a physical therapist, the more important the initial evaluation has become. Our first visit with the patient is time together that really helps me to create a treatment hypothesis. This examination helps me to put together an algorithm for treatment.
I hear their story and repeat back their sequence of events in paraphrase. Then I ask if there is any other relevant information, no matter how small or simple, that they need to tell me? Some will say, I know it sounds weird, but it all started after I twisted my ankle or hurt my shoulder (or something like that). I assure them that we have the whole rest of the visit together and they can chime in with any relevant details."
Determining the onset of coccyx pain will help you gauge the level of improvement you can expect to achieve. Coccyx literature states that patients who have had coccyx pain for 6 months or greater will have less chance for resolution of their symptoms. However, none of the literature includes true osteopathic physical therapy treatment, so I am very biased and feel that this statement is untrue."
The remote course Coccydynia and Painful Sitting is very orthopedically-based which takes Lila Abbate's love of manual, osteopathic treatment and combines it with the women’s health internal treatment aspects so that practitioners are able to move more quickly to get patients back on the path to improved function and recovery. The course looks at patients from a holistic approach from the top of their heads down to their feet. In taking on this topic, the course hones basic observation skills, using some of Lila's favorite tools: the Hesch Method, the Integrated Systems Model, and traditional osteopathic and mobilization approaches.
This course is designed to spark your orthopedic mindset, encouraging the clinician to evaluate the coccyx more holistically.
- What are the joints doing?
- How does it change from sitting to standing? Standing to sitting?
- What is the difference from sitting upright to slump activities?
Working through the basics and the obvious with failed results takes practitioners to the next step of critical thinking about how the patient presents, what seems to be lacking, and how to correct them biomechanically to achieve pain-free sitting?
This remote course provides 5.5 contact hours and the registration fee is $175. The 2022 scheduled course dates are:
Practitioners who have taken Sacroiliac Joint Current Concepts, Bowel Pathology, Sacral Nerve Manual Assessment and Treatment, Yoga for Pelvic Pain, or Ramona Horton's Mobilization of the Myofascial System courses may be interested in attending this course.
Lila Abbate PT, DPT, OCS, WCS, PRPC is the creator and instructor of Bowel Pathology, Function, & Dysfunction and Coccydynia and Painful Sitting. She also co-wrote the course Pudendal Neuralgia and Nerve Entrapment with fellow H&W faculty member Pamela Downey.
Often pelvic health physical therapists are nervous about treating patients with bowel dysfunction and constipation. Lila Abbate's mentor, Elise Stettner, is proud to be a PT who treats bowel conditions. “Any PT can treat urinary symptoms. The patients who are really suffering are those with bowel dysfunctions.” She passed this passion on to Lila, who is the creator and instructor of the Bowel Pathology, Function, & Dysfunction scheduled next on November 13-14, 2021.
Bowel dysfunctions and constipation are often embarrassing for those who suffer from them and thus are often under-reported, which may lead to statistical underrepresentation. The statistics that we do have show that the average prevalence of constipation worldwide in adults is 16%, and for adults over the age of 60 is over 33.5%. (1) Everyone has a different normal for bowel habits which makes it hard to define a normal frequency. Constipation can generally be defined as less than three bowel movements per week and can present as infrequent bowel movements or difficult passage of stools that lasts for several weeks.
There are many potential facets to pelvic floor muscle problems concerning constipation. Lila shares that she recommends that therapists provide a muscle activity assessment in a sitting position, and can even utilize computerized-biofeedback, with the patient's hip and knees at different heights can help determine the best position for muscle relaxation during defecation. At times, it can also be useful to incorporate abdominal massage in resolving a patient's constipation. Abdominal massage for bowel function is useful in motivating peristalsis in the gut, plus there are no known side effects. This is a safe and non-invasive way to manage constipation and can be taught to the patient for them to perform on their own as needed.
In the Bowel Pathology, Function, & Dysfunction Remote Course Lila focuses on teaching registrants about the details of normal gut motility, bowel function, medical tests, and medications relating to diagnosing and treating the medical side of bowel dysfunction. Some of the highlighted lectures are about fecal incontinence, chronic constipation, and abdominal pain and how they relate to pelvic floor muscle dysfunction and physical therapy interventions.
Also commonly encountered in pelvic rehabilitation practices are patients with coccyx pain. You may not think of constipation when treating coccydynia. However, defecation is one of the functional complaints that can be present. The coccyx can interfere with defecation as documented in a case study by Salar et al. They reported that the patient presented with an anteverted coccyx, and complained of "worsening rectal pain developing an hour before defecation and lasting for several hours afterward.” (2)
Lila Abbate also instructs the Coccydynia and Painful Sitting Remote Course. This course is a 1-day deep dive into treating patients who complain of coccyx pain with sitting and defecation. Lila shares that "The coccyx course is orthopedically-based and. I take my love of manual, osteopathic treatment, and combine it with the women’s health internal treatment aspects so that we can move more quickly to get patients back on the path to improved function and recovery."
When asked about the approach she took in creating the course, Lila explains, "this course looks at patients from a holistic approach from the top of their heads down to their feet. In taking on the topic of coccydynia, I focused on honing basic observation skills and using some of my favorite tools in my toolbox. These include the Hesch Method, integrated systems model, traditional osteopathic, and mobilization approaches mixed with internal vaginal and rectal muscle treatment skill sets."
Join faculty member Lila Abbate this November at her upcoming course Bowel Pathology, Function, & Dysfunction scheduled for November 13-14, 2021, or plan ahead and register for the Coccydynia and Painful Sitting Remote Course scheduled for February 4, 2022.
- Forootan, M; Bagheri, N; Darvishi, M. Chronic Constipation: A review of the literature. Medicine (Baltimore) 2018: May. PMID: 29768326 PMCID: PMC5976340 doi:10.1097/MD.0000000000010631
- Salar et al.: Defecation pain and coccydynia due to an anteverted coccyx: a case report. Journal of Medical Case Reports 2012 6:175. doi:10.1186/1752-1947-6-175
In my mid 20’s I had a sudden onset of severe, persistent pain at the bottom of my spine. I had fallen while running on trails and thought maybe I had fractured my coccyx. It hurt terribly to sit, especially on hard surfaces. When I finally succumbed to seeing a doctor, he diagnosed me with a pilonidal cyst and performed a simple excision of the infection right there in the office. I recall passing out on the table and waking up with an open wound stuffed with gauze. What I thought was “just” coccydynia turned out to be something completely different, requiring a specific and immediately effective treatment.
 Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
In a more recent case study by Gavriilidid & Kyriakou 2013, a 73 year old male presented with 6 months of tailbone pain, worse with sitting and rising from sitting. The physician initially referred him to a surgeon for a pilonidal cyst he diagnosed upon palpation. The surgeon found an unusual mass and performed a biopsy, which turned out to be a sacrococcygeal chordoma. The tumor was excised surgically along with the gluteal musculature, coccyx, and the fifth sacral vertebra, as well as a 2cm border of healthy tissue to minimize risk of recurrence of the chordoma. These authors reported coccygodynia is most often caused by pilonidal disease, clinically confirmed by abscess/sinus, fluid drainage, and midline skin pits. They concluded from this case study if one or more of those characteristic findings are absent, differential diagnoses of chordoma, perineural cyst, giant cell tumour, intra-osseous lipoma, or intradural Schwannoma should be investigated.
Honestly, if I were not a physical therapy tech when my coccyx started killing me 20 years ago, I am not sure I would have gone to the doctor right away. My boss called me out when I winced every time I sat down, and he sent me off to get an exam. The majority of patients are not blurting out specific details about buttock pain when they come for evaluation. Modesty prevails but does not always benefit a patient with persistent coccydynia. Thankfully I did not have a chordoma, but the pain was intense enough to bring me to tears, and it could have required surgery if I had not been diagnosed early enough. Providing a comfortable environment for our patients during their initial encounter can help them feel less vulnerable and discuss the root of their pain. If we can decipher between chordoma and other causes of coccydynia, we may strike a chord that saves a patient from a poor outcome.
The Herman & Wallace course "Coccyx Pain Evaluation & Treatment" is an excellent opportunity to learn new differential diagnosis techniques for coccyx pain patients. The next opportunity to attend this course is March 25-26 in Tampa, Florida.
Blocker, O., Hill, S., & Woodacre, T. (2011). Persistent coccydynia – the importance of a differential diagnosis. BMJ Case Reports, 2011, bcr0620114408. http://doi.org/10.1136/bcr.06.2011.4408
Gavriilidis, P., & Kyriakou, D. (2013). Sacrococcygeal chordoma, a rare cause of coccygodynia. The American Journal of Case Reports, 14, 548–550. http://doi.org/10.12659/AJCR.889688
Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sit to stand. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: ¹
- Anterior: Levator ani muscles, Sacrococcygeal ligament
- Lateral: Coccygeal muscles, Sacrospinous ligament, Sacrotuberous ligament, Glute maximus muscle fibers
- Inferiorly: Iliococcygeus
 Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain. 1 Special wedge shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain. Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx. 1 Taping methods can be used as a follow up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroilliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered.
Luckily conservative treatment is successful in about 90% of cases. ¹ All of the above conservative tools will be taught in the upcoming Coccyx Pain Evaluation and Treatment course on April 23-24th, 2016 in Columbia, MO taught by Lila Abbate PT, DPT, OCS, WCS, PRPC. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
1. Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
2. Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
How many of us have heard a subjective report from a patient that clearly implicates the coccyx as the problem but quickly think, “I’m sure as heck not going there!”? We cross our fingers, hoping the patient will get better anyway by treating around the issue. That is like trying to get a splinter out of a finger by massaging the hand. As nice as the treatment may feel, the tip of the finger still has a sharp, throbbing pain at the end of the day, because the splinter, the source of the pain, has not been touched directly. For most therapists, the coccyx is an overlooked (and even ignored) splinter in the buttocks.
![By Sanba38 (Own work) [GFDL (http://www.gnu.org/copyleft/fdl.html), CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/) or FAL], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/thumb/f/f6/Splinter.jpg/256px-Splinter.jpg) A colleague of mine had a patient with relentless coccyx pain for 7 years and was about to lose a relationship, as well as his mind, if someone did not help him. He had therapy for his lumbar spine with “core stabilization,” and he had pain medicine, anti-inflammatory drugs, and inflatable donuts to sit upon to relieve pressure, but his underlying pain remained unchanged. Luckily for this man, his “last resort” was trained in manual therapy and assessed the need for internal coccyx mobilization to resolve his symptoms. The patient’s desperation for relief overrode any embarrassment or hesitation to receive the treatment. After a few treatments, the man’s life was changed because someone literally dug into the source of pain and skillfully remedied the dysfunction.
A colleague of mine had a patient with relentless coccyx pain for 7 years and was about to lose a relationship, as well as his mind, if someone did not help him. He had therapy for his lumbar spine with “core stabilization,” and he had pain medicine, anti-inflammatory drugs, and inflatable donuts to sit upon to relieve pressure, but his underlying pain remained unchanged. Luckily for this man, his “last resort” was trained in manual therapy and assessed the need for internal coccyx mobilization to resolve his symptoms. The patient’s desperation for relief overrode any embarrassment or hesitation to receive the treatment. After a few treatments, the man’s life was changed because someone literally dug into the source of pain and skillfully remedied the dysfunction.
Marinko and Pecci (2014) presented 2 case reports of patients with coccydynia and discussed clinical decision making for the evaluation and management of the patients. The patient with a traumatic onset of pain had almost complete relief of pain and symptoms after 3 treatment sessions of manual therapy to the sacrococcygeal joint. The patient who experienced pain from too much sitting did not respond with any long term relief from the manual therapy and had to undergo surgical excision. The first patient was treated in the acute stage of injury, but the second patient had a cortisone injection initially and then the manual treatment in this study 1 year after onset of pain. Both patients experienced positive outcomes in the end, but at least 1 patient was spared the removal of her coccyx secondary to manual work performed in what some therapists consider “uncharted territory.”
A systematic literature review was published in 2013 by Howard et al. on the efficacy of conservative treatment on coccydinia. The search spanned 10 years and produced 7 articles, which clearly makes this a not-so-popular area of research. No conclusions could be made on how effective the various treatments of manual therapy, injections, or radiofrequency interventions were because of the insufficient amount of research performed on the topic.
In an evidence-based era for physical therapy intervention, sometimes we limit ourselves in our treatment approaches. What if the best interventions just have yet to be oozing with clinical trials and published outcomes? The first person to pull a splinter out of a finger did not have a peer-reviewed guide instructing one to use 2 fingers to wrap around the splinter and pull it out of the skin. Coccyx mobilization internally and externally is a legitimate treatment without a lot of notoriety. The Coccyx Pain, Evaluation, and Treatment course uses the most current evidence to expand your knowledge of anatomy and pathology and hone your palpation skills to evaluate and treat an area where you never thought you’d go.
References: Howard, P. D., Dolan, A. N., Falco, A. N., Holland, B. M., Wilkinson, C. F., & Zink, A. M. (2013). A comparison of conservative interventions and their effectiveness for coccydynia: a systematic review. The Journal of Manual & Manipulative Therapy, 21(4), 213–219. http://doi.org/10.1179/2042618613Y.0000000040
Marinko LN, Pecci M. (2014). Clinical decision making for the evaluation and management of coccydynia: 2 case reports. J Orthop Sports Phys Ther, 44(8):615-21. doi: 10.2519/jospt.2014.4850
Coccyx pain is a frequently encountered condition in pelvic rehabilitation practices. Although sitting is one of the primary limitations for patients who present with coccyx pain, or coccygodynia, defecation can be included in the list of functional complaints. This brings to mind the question: what does the coccyx do during defecation?
Coccygeal mobility was examined using MRI in this study by Grassi and colleagues. The authors included 112 subjects for the dynamic MRI research in positions of maximal contraction as well as straining for evacuation. Included in the study were subjects who complained of constipation, sense of incomplete evacuation of bowels, pain (not coccyx pain), organ prolapse, and minor trauma. Although the MRI was completed with the patient in supine (a non-functional defecation position), the authors reported that during a straining maneuver, the coccyx moves into extension, or backwards.
What if the coccyx does not move into extension during a straining maneuver? Is it possible for the coccyx to interfere with defecation? This appears to be true for a patient who appeared as the subject in the Journal of Medical Case Reports. The patient presented with an anteverted coccyx, and complained of “…worsening rectal pain developing an hour before defecation and lasting for several hours afterwards.” Pain was also reported during sitting on a hard surface. (See the linked article for an interesting image of the coccyx position and what is described as “rectal impingement.”) The patient was treated with coccygectomy which appeared to significantly reduce the symptoms (there are no outcomes tools reported in the case study, so progress reported is vague.) Although removal of the coccyx was the treatment in this particular case, the authors state that first-line treatment for coccyx pain includes conservative measures such as seat cushioning, coccygeal massage, stretching and manipulation, and injections, and that the majority of patients will respond favorably to these interventions.
There is more to learn about the coccyx and its role in defecation, sitting, and other daily functions. Faculty member Lila Abbate teaches a great course called Coccyx Pain, Evaluation & Treatment and it is a great opportunity to learn some new evaluation and treatment techniques. Join her this October 25-26 in Bay Shore, NY.
Herman & Wallace faculty member Lila Abbate instructs several courses in pelvic rehabilitation, including "Coccyx Pain, Evaluation and Treatment". Join Lila this October in Bay Shore, NY in order to learn evaluation and treatment skills for patients with coccyx conditions.
Case studies are relevant reading for physical therapists. Reviewing case studies puts you into the writer’s brain allowing you to synthesize your current knowledge of a particular diagnosis taking you through some atypical twists and turns in treating this particular patient type. In JOSPT, August 2014, Marinko & Pecci presented a very well-written case study of two patients with coccyx pain. By then, I had already written my Coccyx course and couldn’t wait to see what the authors had written. I eagerly downloaded the article to see another’s perspective of coccyx pain and their treatment algorithms, if any, were presented in the article. How were the author’s patients different than mine? What exciting relevant information can I add to my Coccyx course?
I believe that coccyx pain patients have more long-standing pain conditions than other patient types. For the most part, the medical community does not know what to do with this tiny bone that causes all types of havoc in patients’ pain levels. Sometimes treating a traumatic coccydynia patient seems so simple and I am bewildered as to why patients are suffering so long - and other times, their story is so complex that I wonder if I can truly help.
The longer I am a physical therapist, the more important has the initial evaluation become. Our first visit with the patient is time together that really helps me to create a treatment hypothesis. This examination helps me to put together an algorithm for treatment. I now hear their story, repeat back their sequence of events in paraphrase and then I ask: do you think there is any other relevant information, no matter how small or simple, that you think you need to tell me? Some will say, I know it sounds weird, but it all started after I twisted my ankle or hurt my shoulder or something like that. I assure them that we have the whole rest of the visit together and they can chime in with any relevant details. Determining the onset of coccyx pain will help you gauge the level of improvement you can expect to achieve. Coccyx literature states that patients who have coccyx pain for 6 months or greater will have less chance for resolution of their symptoms. However, none of the literature includes true osteopathic physical therapy treatment, so I am very bias and feel that this statement is untrue.
The coccyx course is a very orthopedically-based which takes my love of manual, osteopathic treatment and combines it with the women’s health internal treatment aspects so that we are able to move more quickly to get patient’s back on the path to improved function and recovery. The course looks at patients from a holistic approach from the top of their head down to their feet. In taking on this topic, I couldn’t do it without honing into our basic observation skills, using some of my favorite tools in my toolbox: Hesch Method, Integrated Systems Model, and traditional osteopathic and mobilization approaches mixing it with our internal vaginal and rectal muscle treatment skill set.
Marinko LN, Pecci M. Clinical decision making for the evaluation and management of coccydynia: 2 case reports. J Orthop Sports Phys Ther. 2014 Aug; 44(8): 615-21.