When it comes to discussing nutrition with our clients in pelvic rehab, it is normal to initially feel both uncertain and perhaps a bit overwhelmed at the prospect of delving into this topic. Yet we know that there must be links, some association between nutrition and the many chronic conditions we encounter. Gradually, over the last several years, a cornerstone of my practice with patients in pelvic rehabilitation has become providing nutritional guidance.
 I was both humbled and immensely grateful when many of my colleagues and peers attended Nutrition Perspectives for the Pelvic Rehab Therapist (NPPR) in Kansas City last March. In the following months, our clinics underwent a significant change in the types of discussions occurring with our patients. By embracing concepts presented in NPPR, a continuous stream of patient stories developed about lives having been touched by this shift. For many, “one small change” made a very big difference or served as the catalyst to many more positive lifestyle changes. Simply placing a high priority on re-thinking health situations through the lens of nourishment has been a very important shift, one that can occur across the spectrum of pelvic rehab practitioners if we choose to answer the call to “do what’s necessary”.
I was both humbled and immensely grateful when many of my colleagues and peers attended Nutrition Perspectives for the Pelvic Rehab Therapist (NPPR) in Kansas City last March. In the following months, our clinics underwent a significant change in the types of discussions occurring with our patients. By embracing concepts presented in NPPR, a continuous stream of patient stories developed about lives having been touched by this shift. For many, “one small change” made a very big difference or served as the catalyst to many more positive lifestyle changes. Simply placing a high priority on re-thinking health situations through the lens of nourishment has been a very important shift, one that can occur across the spectrum of pelvic rehab practitioners if we choose to answer the call to “do what’s necessary”.
Learning the essence of a topic outside our comfort zone is not easy, yet in present time is necessary for providers trying to grapple with how to wrap our professional minds around what we know in our hearts to be true: the effect of nourishment on health is profound. This brings to mind the resonating wisdom of Francis of Assisi:
“Start by doing what’s necessary, then do what’s possible;
and suddenly you are doing the impossible.”
At this crossroads in our health care system we know that nutrition matters. We must start by doing what’s necessary: acknowledging our role in helping patients along their path to a better life through less pain, ease of movement, normalization of function, and healing. With commitment to our patient’s well-being, we too must commit to investigating the realm of nutrition and rehabilitation. Next, we can strive to do what’s possible. NPPR can serve as a springboard for professionals ready to develop programs incorporating sound nourishment principles in relation to both specific conditions in pelvic rehab and general health and well-being. Finally, we may - in a few short years - realize that suddenly we are doing the impossible; integrating these vital principles as standard care in rehabilitation.
Please join us in White Plains, NY March 31-April 1, 2017 for Nutrition Perspectives for the Pelvic Rehab Therapist. Whether you are just beginning to integrate nutrition and its correlates to pelvic rehab or are already well on your way along this path, you will come away with both a strong understanding of how food affects function along with tools you can immediately begin sharing with the clients you serve.
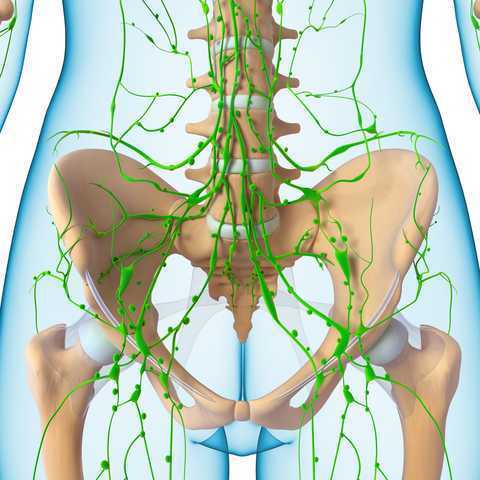
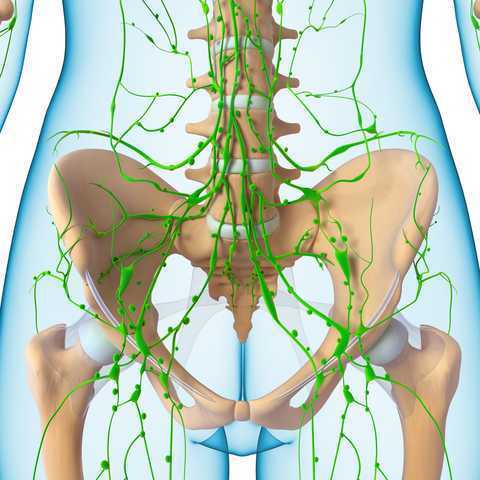 In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
Dr. Chassé became a certified lymphedema therapist in 2000 and a certified Lymphology Association of North America therapist in 2001. She continued training by moving into osteopathy taking her into the direction of lymphatic vessel manipulation. In 2006 she began taking courses in pelvic pain and obstetrics with a focus on pelvic floor dysfunction. It was at this point that Dr. Chasse realized nobody was applying lymphatic treatment to women’s health and pelvic floor dysfunction. In 2009 she became a Board Certified Women’s Health Clinical Specialist in Physical Therapy and began traveling around the United States offering workshops in the area of lymphatic treatment.
Dr. Chassé’s approach is to incorporate all her varied skills in the clinic to produce the best patient outcomes. Debora explains that she is “…showing the similarities between pelvic pain and the lymphatic system. The treatment principles are the same, when you are treating both lymphedema or pelvic pain, you are working to reduce inflammation, pain and scarring.”
Another advantage of the lymphatic treatment approach is that it is more comfortable for the patient. “Most intravaginal techniques causes increased pain and inflammation. However, using lymphatic drainage intravaginally is well tolerated and decreases the intravaginal pain. The results are phenomenal!”
Dr. Chassé recollects her experience with a 21 year old female who suffered from chronic pelvic pain. By applying intravaginal lymphatic drainage techniques for 5 consecutive days, the patient experience a 4.83 reduction in pelvic girdle circumference and her intravaginal pain went from 8/10 to 2/10. The patient was amazed at how much better she felt. “My pants fit better, my energy level increased 25% and pain decreased more than 50%. I went from having 2-3 bad days per week to having 2-3 bad days per month, even when my work level increased. My feet no longer swell and I haven’t missed any classes since receiving this treatment.
In her course, “Lymphatics and Pelvic Pain: New Strategies”, Dr. Chassé seeks to train practitioners to utilize lymphatic drainage techniques when treating specifically pelvic pain. Participants will learn lymphatic drainage principles and techniques. They will learn how to clear pathways to transport lymph fluid and internal techniques which will have incredible impacts for patients.
One of my dear patients was recently diagnosed with Ehlers-Danlos sydrome (EDS). The diagnosis brought a sense of relief for sweet Katie who for years struggled with numerous health problems and was often misunderstood and under cared for by the medical community. Katie was referred to me 2 years ago at 28 for pelvic pain, endometriosis and IC. Upon exam we also discovered a significant elimination disorder and paradoxical elimination. Katie regularly timed her elimination and was spending at times up to 2 hours trying to empty her bowels. As we worked together we uncovered bilateral hip dysplasia, left hip labral tear, ilioinguinal and pudendal neruralgia and POTS (Postural Orthostatic Hypotension Syndrome). Katie already had a history of anxiety and depression but managed well with good family and friend support. When the diagnosis of EDS came, she finally felt like she had an explanation for why her body is like it is. This brought great relief as well as the knowledge that her condition was genetic and her conditions needed to be managed as best as possible to give her the most function, but would likely never be fully resolved.
 In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
It seems that EDS is becoming more widely recognized. As rehabilitation specialists we should be alert to problems stemming from joint hypermobility when we notice how our patients position themselves. Often legs are curled up or double crossed. Upon questioning we might find that the patient has a history of being "double jointed" or was able to do "party tricks" with their bodies. The Bighton scale is a test of joint hypermobility which we should all be familiar with. It is also important to note that a patient may have hypermobility without having EDS, and that EDS is usually associated with pain. A rheumatologist, or in Katie's case a geneticist, can help confirm a suspected EDS diagnosis.
If you have a patient with hypermobliiy or with EDS, know that their ability to know where their body is in space is limited as their joints have much more range of motion than normal. The proprioceptors do not fire well at mid range and the patient will have to be trained to become accustomed to neutral joint positions. This was really painful for Katie and it took a huge mental and physical effort. She is getting stronger now and it is becoming easier to achieve. Stretching and soft tissue massage can feel really good when your muscles have to work so hard to maintain your joints in healthy positions. Patients should be instructed to not stretch into end range and also not "hang out" on their ligaments. Some patients may have to begin just with isometrics. I used Sara Meeks' program for safe and effective floor exercise with Katie. The floor gave her support while she strengthened her core muscles. Then she was able to progress to seated and seated on a ball as well as standing exercises. She loves the body blade! Yoga, Pilates, exercise in water can be effective for strength, propriception and movement reeducation. Mirrors are helpful for increasing position sense.
It is also helpful to note that even patients with EDS may be hypermobile in some joints and hypomobile in others. Isobel reports that her SI joints were extremely unstable while her thoracic spine was very rigid to the point that her lung capacity was affected. Having her therapist work on the hypomobility and doing breath work was life changing.
As pelvic health therapists and rehabilitation providers we may be the first professional to suspect EDS in a patient. There is a great deal that we and the greater medical and holistic community can do to help patients with EDS lead lives with less pain and dysfunction.
Faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC has written in to encourage us all to practice kindness and patience. A positive attitude can affect more than just your friends and family; your patients will benefit in so many ways as well!
 First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
Now back to the clinical. Just about two years ago I had the privilege of teaching with Nari Clemons. We taught PF2B together. Nari said something during one of her lectures that revolutionized my PT practice. She challenged us in lab to find three positive things about our lab partner and share those things before recognizing any deficits. How many times do we get finished with an evaluation and sit down with a patient and list all the things we found that need correction or help, perhaps drawing on our Netter images to fully illustrate the parts of their body that are broken or need fixing.
So I changed things up a bit and started remarking about the positive things I found on exam. "Wow, your hips are really strong and stable." "You've got a really coordinated breathing pattern, that is going to work in your favor." "You're pelvic muscles are really strong." and then later drawing on those positives outline how we could use the patient's strengths to help them overcome their challenges. "Because you have a great breathing strategy we are going to use that to help your whole nervous system to relax which with help your pelvic floor relax," for example.
The results were shocking. Person after person told me how much it meant to them to leave feeling positive and hopeful. One delightful woman who I saw for a diastasis had amazing leg muscles and I told her so. When she returned she said, "I've felt so self conscious about my flabby belly, but this week all I could think about were my strong leg muscles. Thanks for telling me that."
We do know is that our attitudes and beliefs as providers influence not only our clinical management but patient outcomes as well. Darlow et. al. performed a comprehensive literature review looking at how attitudes and beliefs among health care providers affected outcomes in patients with low back pain and discovered, "There is strong evidence that health care provider beliefs about back pain are associated with the beliefs of their patients."
Why not use that truth to our advantage and be positive? Would love to hear about your experiences!
Join Jennafer at one of her upcoming courses, Pelvic Floor Level 2B - Trenton, NJ - February 24-26, 2017, Pelvic Floor Series Capstone - Arlington, VA - May 5-7, 2017, Pelvic Floor Series Capstone - Columbus, OH - August 18-20, 2017, and Pelvic Floor Series Capstone - Tampa, FL - December 2-4, 2016.
Herman & Wallace are pleased to announce a new course! Pudendal Neuralgia and Nerve Entrapment will be presented by Michelle Lyons in Freehold, NJ on June 17/18, 2017. We chatted with Michelle about this new course to hear her thoughts and get an overview of the contents
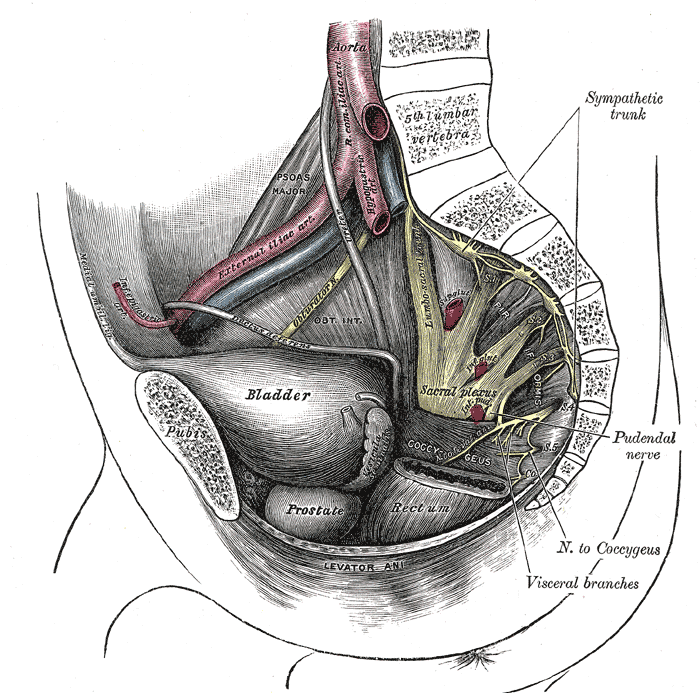 There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
When I was approached about developing this course for the Institute, I jumped at the opportunity. For those who don’t know me, I really like to bring an integrative approach to my work, both clinically and educationally. I have experience and training in nutrition, coaching, yoga, Pilates and mindfulness as a therapeutic intervention and I think these fit really well alongside traditional pelvic rehab approaches. Manual therapy and bespoke exercise prescription will always be the bedrock of my approach, but sometimes our patients, especially those with chronic pain, need some extra support. I’m also a bit of an anatomy nerd, so the chance to delve deep into pelvic neuroanatomy and neurodynamics was too much to resist!
I think this is a Golden Age in pelvic health – there are so many great learning opportunities and resources available to us to help serve our patients better. Another area that I find fascinating to explore is the huge leap we have made in understanding neuroscience and the role of pain education when it comes to chronic pelvic pain. I’m a big fan of the work done by Moseley and Butler in Australia, and I love how authors like Hilton, Vandyken and Louw have transferred that to the world of pelvic pain in their book "Why Pelvic Pain Hurts". The language that we use is very important when discussing how the brain responds to chronic pain and the changes that occur with central sensitization. We never want our patients to feel as if we think their pain is ‘all in their heads’ but at the same time, we need to be able to incorporate strategies such as motor imagery and graded exposure and to demonstrate to our patients that"…it is important to acknowledge that chronic pain need not involve any structural pathology" (Aronoff 2016).
Those are some of the discussions we’ll be having in Freehold, NJ next June – I hope you’ll come and join the conversation!
"What Do We Know About the Pathophysiology of Chronic Pain? Implications for Treatment Considerations" Aronoff, GM Med Clin North Am. 2016 Jan;100(1):31-42
"Why Pelvic Pain Hurts: Neuroscience Education for Patients with Pelvic Pain" Hilton, Vandyken, Louw, International Spine and Pain Institute (May 28, 2014)
My job as a pelvic floor therapist is rewarding and challenging in so many ways. I have to say that one of my favorite "job duties" is differential diagnosis. Some days I feel like a detective, hunting down and piecing together important clues that join like the pieces of a puzzle and reveal the mystery of the root of a particular patient's problem. When I can accurately pinpoint the cause of someone's pain, then I can both offer hope and plan a road to healing.
 Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
My patient relayed that she was 6 months post partum with her first child. She was nursing. Her labor and delivery were unremarkable but she tore a bit during the delivery. She had tried to have intercourse with her husband a few times. It was painful and she thought she needed more time to heal but the pain was not changing. She was a 0 on the Marinoff scare. She was convinced that her scar was restricted. "Oh Goodie," I thought. "I love working with scars!" But I said to her, "Well, we will certainly check your scar mobility but we will also look at the nerves and muscles and skin in that area and test each as a potential pain source, while also completing a musculoskeletal assessment of the rest of you."
Her "external" exam was unremarkable except for adductor and abdominal muscle overactivity. Her internal exam actually revealed excellent scar healing and mobility. There was significant erythemia around the vestibule and a cotton swab test was positive for pain in several areas. There was also significant muscle overactivity in the bulbospongiosis, urethrovaginal sphincter and pubococcygeus muscles. Also her vaginal pH was a 7 (it should normally be a 4, this could indicate low vaginal estrogen). I gave her the diagnosis of provoked vestibulodynia with vaginismus. Her scar was not the problem after all.
Initially for homework she removed all vulvar irritants, talked to her doctor about trying a small amount of vaginal estrogen cream, and worked on awareness of her tendency to clench her abdominal, adductor, and pelvic floor muscles followed by focused relaxation and deep breathing. In the clinic I performed biofeedback for down training, manual therapy to the involved muscles, and instructed her in a dilator program for home. This particular patient did beautifully and her symptoms resolved quite quickly. She sent me a very satisfied email from a weekend holiday with her husband and daughter.
Although this case was fairly straightforward, it is a great example of how differential diagnosis is imperative to deciding and implementing an effective treatment plan for our patients. In Herman & Wallace courses you will gain confidence in your evaluation skills and learn evidence based treatment processes that will enable you to be more confident in your care of both straightforward and complex pelvic pain cases. Hope to see you in class!
Our understanding of treating pelvic pain keeps growing as a profession. We have so many manual therapies such as visceral manipulation, strain counter strain, and positional release adding dimension to our treatment strategies for shortened and painful tissues. Pharmacologic interventions such as botox, valium, and antidepressants are becoming more popular and researched in the literature. We are beginning to work more collaboratively with vulvar dermatologists, urogynecologists, OB’s, family practitioners, urologists, and pain specialists.
 Pelvic rehab providers are in a unique position of being able to offer more time with each patient and to see our patients for several visits. Frequently we are the ones being told stories about how a particular condition is really affecting our patient’s life and the emotional struggles around that. We are often the one who gets a clear picture of our patient’s emotional and mental disposition. A rehab provider may realize that a patient seems to exhibit mental patterns in their treatment. It can be anxiety from how the condition is changing their life, difficulty relaxing into a treatment, poor or shallow breathing patterns, frequently telling themselves they will never get better, or being able to perceive their body only as a source of pain or suffering, losing the subtlety of the other sensations within the body. Yet, aside from contacting a physician, who may offer a medication with side effects, or referring to a counselor or psychologist, our options and training may be limited. Patients may be resistant to seeing a mental health counselor, and we have to be careful to stay in our scope.
Pelvic rehab providers are in a unique position of being able to offer more time with each patient and to see our patients for several visits. Frequently we are the ones being told stories about how a particular condition is really affecting our patient’s life and the emotional struggles around that. We are often the one who gets a clear picture of our patient’s emotional and mental disposition. A rehab provider may realize that a patient seems to exhibit mental patterns in their treatment. It can be anxiety from how the condition is changing their life, difficulty relaxing into a treatment, poor or shallow breathing patterns, frequently telling themselves they will never get better, or being able to perceive their body only as a source of pain or suffering, losing the subtlety of the other sensations within the body. Yet, aside from contacting a physician, who may offer a medication with side effects, or referring to a counselor or psychologist, our options and training may be limited. Patients may be resistant to seeing a mental health counselor, and we have to be careful to stay in our scope.
Research is showing us that meditation as an intervention can be very helpful in addressing these chronic pain issues.
In a study in the Journal of Reproductive Medicine, 22 women with chronic pelvic pain were enrolled in an 8 week mindfulness meditation course. Twelve out of 22 enrolled subjects completed the program and had significant improvement in daily maximum pain scores, physical function, mental health, and social function. The mindfulness scores improved significantly in all measures (p < 0.01).
The questions have arisen, if meditation alters opiod pathways, how can it be administered safely with prescription medications. However in a 2016 study in the journal of neuroscience, it was concluded that meditation-based pain relief does not require endogenous opioids.” Therefore, the treatment of chronic pain may be more effective with meditation due to a lack of cross-tolerance with opiate-based medications.” “The risks of chronic therapy are significant and may outweigh any potential benefits”, according the the journal of American Family Medicine. Meditation training can be a tool to help our patients manage their pain without risk of long term opiod use.
In the two day course, Meditation for Patients and Providers, participants will learn several different meditation and mindfulness techniques they can use for patients with different dispositions, and to tailor the most appropriate approach to specific patients. The aim of the course is to be able to work meditation into a treatment and a home program that is best suited for your patient. The course also covers self care, preventing provider burn out and ways to be more mentally quiet as a provider seeking to give optimal care with appropriate boundaries.
Fox, S. D., Flynn, E., & Allen, R. H. (2010). Mindfulness meditation for women with chronic pelvic pain: a pilot study. The Journal of reproductive medicine, 56(3-4), 158-162.
LEMBKE, A., HUMPHREYS, K., & NEWMARK, J. (2016). Weighing the Risks and Benefits of Chronic Opioid Therapy. American Family Physician,93(12).
Zeidan, F., Adler-Neal, A. L., Wells, R. E., Stagnaro, E., May, L. M., Eisenach, J. C., ... & Coghill, R. C. (2016). Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. The Journal of Neuroscience, 36(11), 3391-3397.
 Dr. Peter Philip, a faculty member with the Herman & Wallace Institute, has published a new book! "Pelvic Pain and Dysfunction: A Differential Diagnosis Manual" is available now through Thieme Medical Publishers. We caught up with Dr. Philip to learn a bit more about his project.
Dr. Peter Philip, a faculty member with the Herman & Wallace Institute, has published a new book! "Pelvic Pain and Dysfunction: A Differential Diagnosis Manual" is available now through Thieme Medical Publishers. We caught up with Dr. Philip to learn a bit more about his project.
Peter is also the author and instructor of two courses offered through Herman & Wallace. Sacroiliac Joint Evaluation and Treatment is an opportunity to learn an exercise and stabilization approach to pelvic girdle, sacroiliac joint, and pelvic ring dysfunction. This course is available twice in 2016; May 21-22 in Austin, TX and later on November 6-7 in Bayshore, NY. Peter's other course, Differential Diagnostics of Chronic Pelvic Pain: Interconnections of the Spine, Neurology and the Hips, expands the practitioner's diagnostic toolkit for complicated chronic pelvic pain patients. This course is available on August 19-21 in Nashville, TN. Don't miss out!
H&W: Thanks for doing this interview, Peter! What's new?
Dr. Philip: After years of research, and writing, my textbook has been published and is ready for the public.
H&W: That's great! What can you tell us about the book?
Dr. Philip: It's called Pelvic Pain and Dysfunction; a Differential Diagnosis Manual, and it has been published by Thieme. Thieme is based out of Stuttgart Germany and is the world’s largest distributor of medical textbooks and journals! The purpose of the book is to answer the questions that so many clinicians have as it relates to their patient’s pain, such as:
- Why are there muscle spasms?
- How can the pain seemingly spread from one organ to the next? Or even from one system to another?
- How can I effectively and efficiently evaluate my patients who suffer with pelvic, bladder, bowel, or visceral pain and dysfunction?
- And so much more
The textbook also outlines a revolutionary strategy that immediately provides the patient with a reduction in their pain, and often immediate resolution of tight “spasms” or “trigger points”. The mysteries of how and why our patients' pain changes and progresses are outlined in a clear, linear fashion that integrates into a practitioner's current practice. The purpose of the textbook is to provide a means of understanding where pain originates and how to isolate it to a specific region. Once isolated, the book instructs how to treat that region effectively.
H&W: you mean to tell me that you’ve created a method which allows a suffering patient to experience “immediate relief”?
Dr. Philip: Yes! And it's actually quite simple once you understand the anatomy, and the integration of the central nervous system, the peripheral nervous system, psychology, viscera, muscles, tendons, ligaments, and nerves.
H&W: Who is this textbook written for?
Dr. Philip: the textbook is written for all my colleagues who treat patients with pelvic pain. Medical Doctors and Doctors of Science in both the United States and Germany have reviewed the material and found the information, concepts and strategies to be useful.
H&W: how did you put this all together?
Dr. Philip: I realized years ago that the field of pelvic health did not take into consideration the multiple facets that may be involved in a patient’s pain. Many strategies employed simply address restrictions in tissue mobility by “stretching” or “massaging” without taking into consideration the reason these structures are limited in mobility, or have spasms. Knowing why a structure is limited in its mobility or is spastic will allow the clinician to immediately address the suffering patient's needs and promote healing, even if the patient has been suffering for decades.
H&W: but how did you come up with this process?
Dr. Philip: my background is in non-surgical orthopedic medicine. Having three degrees in orthopedic physical therapy, and a certification by the International Academy of Orthopedic Medicine, I applied the differential diagnostic concepts of orthopedic medicine to the pelvic pain population with great success! Using the principles found within this textbook the clinician will have the opportunity to address the exact tissue at fault, provide a near immediate resolution of their pain, and provide a means for the patient to completely regain their wellness and move forward in their life.
H&W: I can see why you are so excited. Is this textbook available yet?
Dr. Philip: yes it is. It can be found at http://www.thieme.com/books-main/obstetrics-and-gynecology/product/3517-pelvic-pain-and-dysfunction. I put in a lot of effort to keep the book comfortably priced at $99.00! I know how tight cash can be for students and the working professional, so keeping it affordable was paramount to me.
H&W: What a fantastic project. Thank you so very much for taking the time to share it with us!
Dr. Philip: It's been a pleasure. Thank you to the Herman and Wallace Institute for allowing me to introduce my textbook and to teach these concepts and strategies.
Faculty member Carolyn McManus, PT, MS, MA is the instructor of Mindfulness Based Pain Treatment, a course which enables practitioners to learn about the impacts of cognitive and emotional state on pain. Herman & Wallace was very lucky to have her join the faculty in 2014, and she has written in to share more about her reasons for doing so. Join her in the Bay Area this May 14-15!
I am inspired to teach for Herman and Wallace because I need more colleagues to help meet the continual demand for my skills and treatment approach. I teach patients mindfulness, body awareness and strategies to self-regulate the nervous system. Patients need to learn how to pay attention to the body in a therapeutic manner, release muscle tension, reduce the stress reaction and adopt an attitude that promotes healing and well-being. With the ability to rest the mind in the present moment, listen to the body with mindful awareness and take control of reactions to stress and pain, patients can reduce pain, make greater progress with exercise programs and improve activity levels. There is a huge demand for this treatment approach. I always have a full schedule and an insanely long wait list. More therapists who can offer mindfulness-based pain treatment are needed.
I also want to get the word out that there is a lot we can do to prevent chronic pain. Research suggests that a reduction in pain inhibitory mechanisms contribute to persistent pain. These mechanisms can be influenced by stress and cognitive and emotional modulation. Working with patients in pain for over 30 years, I have developed a clear and simple way to explain the role of cognitive and emotional factors in pain perception. I find that once patients truly understand how their reactions can amplify or inhibit nociceptive pathways, they are empowered to take an active role in a holistic treatment approach. We can improve the chances of recovery for patients at risk of chronic pain by identifying them early early on and providing them with education and mindfulness-based strategies to self-regulate the nervous system. Patients can be offered specific skills to reduce the stress reaction, fear, catastrophic thinking and the negative attitudes that amplify and prolong pain.
I want to teach other therapists to successfully help patients in pain in the way I have for many years. One recent course participant made my day when she said to me, “I now have so much more to offer my patients.”
If you are interested in offering a new course with Herman & Wallace, don't hesitate to reach out! Fill out the form at https://www.hermanwallace.com/teach-with-us and let us know about your course idea and why you would be a good fit for the team.
In our weekly feature section, Pelvic Rehab Report is proud to present this interview with Herman & Wallace instructor Holly Tanner PT, DPT, MA, OCS, WCS, PRPC, LMP, BCB-PMB, CCI

How did you get started in pelvic rehab?
I joined Apple Physical Therapy as an orthopedic outpatient clinic manager back in 2000. The previous manager had begun treating women who had urinary incontinence and we had this (huge) old biofeedback unit. I told the company owners that I would be willing to take a course in treating urinary incontinence, which I quickly did. I also quickly learned that to do a great job in pelvic rehab, and to serve the patients well, you need to keep taking classes to learn about all the other issues that make pelvic rehab so potentially complex and engaging.
What have you found most rewarding in treating this patient population?
The fact that patients are so trusting and share their most intimate issues that may be difficult to discuss. Patients with pelvic dysfunction are so profoundly grateful for the help they receive, and that in turn inspires me to want to be helpful.
What do you find most rewarding about teaching?
I love providing a groundwork upon which the therapists can build through their own practices and through other coursework and knowledge they bring to the table. There is never one approach or one course that can provide an answer for each patient, and as an instructor for Herman & Wallace, I have the privilege of standing on the platform that Holly Herman and Kathe Wallace established when they founded the Institute. I feel that I get to fast-track the therapists by sharing what I have learned through experience and all the training that I have received, and then they can keep expanding the knowledge and skills within our field. I also learn a lot myself through the generosity of the therapists who bring their knowledge and experience to the courses.
If you could get a message to all therapists about pelvic rehab, what would it be?
Shadow a pelvic rehab therapist for half a day. That's all it will take to see the world that opens up in front of you, to feel inspired by the amount of issues that go "missing" and how to address them, and also how to notice how simple and meaningful it is to offer some guidance or hope to a patient who has pelvic dysfunction.
If you could make a significant change to the field of pelvic rehab or the field of PT, what would it be?
Now that more therapists are joining the ranks of pelvic rehab, I hope that we see more of them move into treating men and children. As Dawn Sandalcidi (who teaches about pediatrics for the Institute) shares with us, many of the pelvic dysfunctions start in childhood, and we must get to the kids as soon as possible.
What is your favorite topic about which you teach?
My favorite condition to treat and lecture about is definitely scrotal pain. There is such a paucity of awareness about the potential causes of scrotal or testicular pain, and men have been suffering way too long when they have this issue. In my experience, men can respond very quickly and completely with intervention.