This week The Pelvic Rehab Report sat down with Kate Bailey, PT, DPT, MS, E-RYT 500, YACEP, Y4C, CPI to discuss her career as a physical therapist and upcoming course, Restorative Yoga for Physical Therapists, scheduled for September 11-12, 2021. Kate’s course combines live discussions and labs with pre-recorded lectures and practices that will be the basis for experiencing and integrating restorative yoga into physical therapy practice. Kate brings over 15 years of teaching movement experience to her physical therapy practice with specialties in Pilates and yoga with a focus on alignment and embodiment.
Who are you? Describe your clinical practice.
My name is Kate Bailey. I own a private practice in Seattle that focuses on pelvic health for all genders and ages. I work under a trauma-informed model where patient self-advocacy and embodiment are a priority. My dog, Elly, assists in my practice by providing a cute face and some calming doggy energy. My patients often joke that they come to see her just as much as to see me, which I think is great. In addition to being a physical therapist, I’ve been teaching Pilates for nearly 20 years and yoga for over 10. They are both big parts of my practice philosophy and my own personal movement practice
What books or articles have impacted you as a clinician?
I have a diverse library of Buddhist philosophy, emotional intelligence, trauma psychology, human behavior, breathwork/yoga, and sociology and, of course, a bunch of physical therapy pelvic floor books. I also love a children’s book on emotional regulation or inclusion, even for adults. One of my favorite finds is the Spot series that gives kiddos different ways to use their hands to help deal with different emotions. I’ve used it for adults who need physical self-soothing options. There are so many, and I find that it's the amalgamation of information that really impacts my practice the most.
How did you get involved in the pelvic rehabilitation field?
I have a deep interest in the human experience and how culture and dissociation create mass-disembodiment and how hands-on work can be profound in how we experience our body. Pelvic rehab allowed me the opportunity to work more closely with people on areas that bring up the most shame, disembodiment, and trauma, and therefore have some pretty amazing possibilities to make an impact not only in their lives but how they act in culture. In many ways, I see my work in pelvic rehab as a point of personal activism in creating a more embodied, empowered, and powerful culture.
What has your educational journey as a pelvic rehab therapist looked like?
I knew I wanted to go into pelvic health from my second year in PT school. I’ve always been at bit…well, let’s call it driven. I did an internship with great therapists in Austin and then only considered full-time pelvic floor positions once licensed. I took as many courses as I could handle in my first couple years of practice, which worked well for me, but understandably is not the right path for all those entering this field for a number of reasons. I went through the foundational series, and then into visceral work as well as continued my yoga and Pilates studies. I continued my education in trauma and emotional intelligence which is both a personal and professional practice. I found that a blend of online coursework and in-person kept me satisfied with my educational appetite.
What made you want to create your course, Restorative Yoga for Physical Therapists?
I was a yoga teacher long before I became a PT. When I found my way into the specialty of pelvic floor physical therapy, this particular part of my yoga teaching became incredibly useful for patients who had high anxiety, high stress, and difficulty with relaxation and/or meditation. This course was a way for me to share some of my knowledge of restorative yoga with the community of health care providers, where it could not only be used as a means of helping patients, but also as a means to start valuing rest as a primary component of wellbeing.
What need does your course fill in the field of pelvic rehabilitation?
Learning about yoga as a full practice and understanding that it has many components is very useful in deciding which component would be a good match for a pelvic health patient. Is it strengthening from an active practice? Is it meditation or pranayama (breath manipulation)? Or is it supported rest? This particular course focuses on the lesser-known aspects of the yoga platform: breath, restorative practice, and a bit of meditation. I have clients all the time struggle with meditation because their nervous systems aren’t ready for it. So we look at breathing and restorative yoga both as independent alternatives, but also as a way to get closer to meditation. Learning how to help people rest, the different postures, how to prop, and how to dose is an important component of this class. As a bonus, giving the clinicians another skill for their own rest practice can be useful when feeling tired, overwhelmed, or burned out. All this under a trauma-informed, neuro-regulation-focused model is a lovely way to deepen one’s physical therapy practice.
What demographic, would benefit from your course?
People who are stressed out or who work with people who are stressed out. In particular, clinicians who work with people who have pelvic pain or overactivity in their pelvic floors.
What patient population do you find most rewarding in treating and why?
I love working with female-identifying patients that struggle with sexual health or those who are hypermobile and trying to figure out movement that feels good. I love working with all genders generally and do so regularly. There’s nothing quite like helping a male-identifying patient find embodiment and understanding of their pelvis in a new way. I think for me, working to dismantle female normative structures for those identifying as female, particularly in the realm of sexual health feels inspiring to me because it combines physical, emotional, spiritual health with going against the cultural standards of how those identifying as women fit into society, and being able to sit with the trauma of all types that so many people face.
What do you find is the most useful resource for your practice?
A pelvic floor model is great. The most important part of my practice is a conversation about consent, not only for internal work but for everything I offer during visits and also for patients to understand that they can give or retract consent with any medical provider for just about any service. Emergency procedures are a smidge different, but I hope my patients walk away with the understanding that the medical community is here to serve their embodied experience. My newest favorite resource is a series of metal prints that depict the emotional intelligence grid used in the RULER syllabus. I have a magnet that patients can use to identify how they are feeling and help develop their language for emotional and then somatic or interoceptive knowledge.
What has been your favorite Herman & Wallace Course and why?
There was nothing quite like PF1. I don’t think I’ll ever forget it. The instructors were Stacey Futterman Tauriello and Susannah Haarmann. I was still in grad school prepping for my internship and ended up being the model for labs which falls squarely in line with my upbringing as a dancer who wanted to understand everything from the inside out. It was a challenging weekend on pretty much every level. I went through phases of dissociation and total connection. It made me realize that my decision to enter health care after having a career in movement was the right one.
What lesson have you learned from a course, instructor, colleague, or mentor that has stayed with you?
Meet the patient where they are at first and validate that they live in an incredibly intelligent body. I think sometimes it’s so exciting to see the potential that patients have because, as clinicians, we’ve seen the progress of others. In yoga, there is a practice of the beginner’s mind. It asks the student to sit with an empty cup of knowledge and experience each practice with the curiosity of someone just being introduced to yoga. I have knowledge that may be helpful to patients. Patients have so much knowledge of their own body from their life experiences, some of which are conscious and so much of which is subconscious. The fun part is seeing how my experience and their experience match (or don’t sometimes) to then assess how to craft the care plan.
If you could get a message out to other clinicians about pelvic rehab what would it be?
That it's so much more than pelvic rehab. We get to talk to people about things that aren’t talked about and normalize the human experience. Pelvic rehab gives safety to patients to experience their bodies in all the sensations that come from having a nervous system: from sadness to joy to relief to fear. It's all in there and when we learn about those sensations from pelvic rehab, my hope is that it can flood into other areas of life.
What is in store for you in the future as a clinician?
Refining, learning, and seeing what else comes. Hoping to publish a book of cartoon organs shortly. But most importantly to create a safe space for patients to feel cared for and supported in my corner of Seattle.
Kate Bailey (She/Her)
Pelvic Floor Physical Therapy
Yoga & Pilates
This email address is being protected from spambots. You need JavaScript enabled to view it.
 Last week- on May 6 amid a pandemic- the Department of Education released changes to Title IX. Title IX is a 1972 Civil Rights Act that bans sexual discrimination within the educational system. Sadly, the new provisions within the 2,033 page document include the following changes:
Last week- on May 6 amid a pandemic- the Department of Education released changes to Title IX. Title IX is a 1972 Civil Rights Act that bans sexual discrimination within the educational system. Sadly, the new provisions within the 2,033 page document include the following changes:
- Narrows the definition of sexual harassment
- Reduces options to survivors of sexual assault, dating violence and stalking
- Reduces liability of colleges and universities
- Reduces mandated reporting of sexual violence
- Deregulates federal guidelines to protect sexual violence survivors
- Changes the ‘standard of proof’ from ‘preponderance’ to ‘clear and convincing’
- Bolsters protections for perpetrators
- Allows for live hearings and cross examinations of the assault survivor
- Only investigates if assault reported to ‘certain people’
23% of undergraduates and 11% of graduate students report having experienced sexual violence, AND we know survivors under-report assaults. We talk extensively about medical and legal considerations for sexual violence survivors in my "Empowering the Sexual Assault Survivor" course. Participants who took my course will need to know those protections we discussed just a few days ago are slated to be rolled back. Today, in my remote course "Trauma Informed Care", we lay the physiological and neurobiological framework for empowering the sexual assault survivor. Following that, in addition to how to continue empowering for survivors, we elaborated on the legal changes listed above.
Outrageously, these Title IX deregulating provisions are to go into effect August 14, 2020 while schools are struggling to keep students safe amid coronavirus pandemic. Again, let us look at these percentages (23% of undergraduates, and 11% of graduate students) and think about who needs safety and protection.
Schools do have choice in whether they roll back their protections to survivors of sexual violence. If you're looking for ways to help, you may want to reach out to your alma mater and ask what changes they are planning to make in the context of this new deregulation and disempowerment of Title IX protections. Maybe contact your local sexual assault coalition and see how you can become involved. You could also contact your legislature and/or leave comment on www.regulations.gov (search title IX and education).Empower yourself so that you can empower others! As a physical therapist specialized in pelvic rehabilitation, empowering survivors of sexual violence happens every day in my practice. I hope you feel empowered, supported and successful in doing this challenging work too!
A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Tory Pines State Park provided much needed rejuvination. Ahh sea air.
2. Self-care is mandatory:
We spent Friday relaxing at a beautiful resort in Del Mar. We are learning we don’t need to justify or feel bad about caring for ourselves. It’s necessary and important. We are responsible for meeting our own needs and for refueling ourselves when we provide care for others.
3. Get out of your comfort zone:
The robes we got from the resort were super cozy and it was chilly on the beach, so why not walk the beach in a robe? We laughed at ourselves and others laughed at us and with us. But we were comfy and warm.
4. Do the work when it is time to do the work:
Instead of thinking and talking about the course all day we committed ourselves to being in the moment. When it came time to discuss the details of the next three days, a plan came together with relative ease. This is us working at the resort.
5. Challenges can change your perspective. And a change in perspective can help you with challenges:
This is a (terrible, sorry) picture of us interrupting our morning run to climb a tree. It was a fun challenge and gave us an interesting perspective on our day.
A little more about the course. Woah. The people who showed up came with open minds and hearts, ready and ripe for change. We had powerful times of sharing, listening, learning, and supporting. Meditation and yoga and a healing, honest and real atmosphere brought about transformation in the most beautiful awe-inspiring way. We were profoundly moved. The changes Nari suggested were PERFECT and I was grateful for her innovations. We were all pretty much out of our comfort zones, but that is where change happens.
In the words of one student, “This course couldn’t have come at a more appropriate time because I was in major burnout. I was becoming an unhappy person both professionally and personally. I needed to make a change. Now I am leaving this course empowered to care for myself so I can help patients in a healthy way and enjoy my job again. I am walking away from this course with so many valuable strategies and also feel so much more relaxed and hopeful”
6. Be silly sometimes:
Laugh a lot. Especially at work. Play jokes, have fun. You know what they say about all work and no play. Play.
7. At the end of the day Shake it off (and use pain science as needed):
Our last day we took a run to the beach. When crossing a rail line I tripped and bashed the HECK out of my lower leg. Since I could still run I repeated the mantra “Hurt not harm!!” (which we discuss in class) with great vigor until the throbbing subsided, and we enjoyed a beautiful sunset and the conclusion of our time in San Diego.
Last words of Wisdom:
Gratitude can change us in powerful ways.
A huge and heart felt thank you to Herman & Wallace, our host site, and for each and every participant. We couldn’t do what we do without you and for this we are eternally grateful.
Thank you. Thank you. Thank you.

Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has just joined the Herman & Wallace faculty and co-authored the new course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Aparna was kind enough to introduce herself to us here on The Pelvic Rehab Report.
 Thank you for your time Aparna! To start, tell us a little bit about yourself.
Thank you for your time Aparna! To start, tell us a little bit about yourself.
My name is Aparna. I’ve been a physical therapist for 22 years. About 16 years ago I switched focus from orthopedics to treating pregnancy and postpartum patients and that’s where my initial interest in pelvic care started. In 2006 following my pregnancy and birth of my daughter, my interest in pelvic care grew with my special interest becoming pelvic pain.
I teach and mentor the pelvic health therapists within the fairly large hospital system that I work at and collaborate with our spine center team and our sports team.
What can you tell us about this new breathing course that is not mentioned in the “course description” and “objectives” that are posted online?
Physical therapy has evolved and continues to evolve as we speak. Regional inter dependence, wherein the different systems interplay, and one structure influences another, is fascinating. No longer is the body considered and treated as independent fragmented pieces. The ‘core’ with the contribution of the Diaphragm and the pelvic floor is so much more than just the Transverse Abdominis and the Multifidus working together. Fascial restrictions of the lower abdomen and the pelvis can influence how the low back feels, thoracic stiffness can influence the interplay between the various abdominal muscles by way on their insertion into the lower ribs, musculo- skeletal pain and postural deviations can stem from incorrect breathing patterns etc.
Normal breathing rate is about 10 times every minute. Breathing incorrectly reinforces wrong movement patterns tens of thousand times a day with negative consequences on the musculoskeletal system.
This course offers an in depth look at the diaphragm from the perspective of both orthopedic and pelvic therapists and attempts to tie in the diaphragm to the thoracic spine, the ribs, the pelvic floor, the core, posture and finally the athlete.
What essential skills does the breath course add to a practitioner’s toolkit?
The practitioner will walk away with the ability to view the patient as a “whole”. It offers a different perspective on neck and back pain, posture/ alignment along with the ability to assess for and connect breathing and the diaphragm to stability/ the core, continence issues and the Autonomic Nervous System.
As therapists we already do a great job of addressing strength issues, assessing and correcting posture, mobilizing etc. You can add to your treatment options by learning how the diaphragm works in concert with other muscles (especially the abdominals) and systems, identifying breathing pattern dysfunctions and postures, and movement patterns which may be linked to breathing pattern dysfunctions. This understanding is beneficial for both orthopedic and pelvic patients.
What inspired you to create this course? What void does this new offering fill?
I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now. As the mentor for the pelvic program at my hospital, and as a part of the spine team and sports team, I work with pelvic therapists, orthopedic therapists, manual certified therapists, and sports certified therapists. Through my interactions I have come to realize that although many of the therapists are aware that the Diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions. I initially started conducting classes within the hospital system. At the same time Leeann who is a sports certified therapist and holds a manual therapy certificate and I started collaborating on our patients. Using a combination of her knowledge and effective manual techniques with my pelvic care and breathing techniques we realized that along with my pelvic patients; our back and neck patients, and her sports patients were all benefitting from this combined approach. We realized along the way that we had information worth sharing with our colleagues that would benefit them in treating their patients, and started classes within the hospital system and that is how this class was born!
What was your process like creating this course?
As a trained pelvic therapist, I have incorporated and used breath and the diaphragm in my treatment for over a decade. Leeann and I have created this course using a combination of our clinical experiences, our education in our respective chosen paths of patient care, and most importantly using recent and relevant research articles from journals to guide us extensively in creating this course.
Breathing and the Diaphragm: Pelvic and Orthopedic Therapists is a new course being offered next March 27-29, 2020 in Sterling Heights, MI, and again on December 11-13, 2020 in Princeton, NJ. It is created and taught by Aparna Rajagopal, PT, MHS and Leeann Taptich, PT, DPT. Come learn how the diaphragm and breathing can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi component system that works together.
Herman & Wallace is excited to announce an upcoming course on pelvic rehab for the gender diverse patient, written and instructed by Dr. Laura Meihofer, DPT, ATC. As Dr. Meihofer indicated in a recent blog, "[t]he number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016)... With the rise of individuals who identify as transgender, gender non-binary and intersex, healthcare professionals have equally seen an influx of patients who require care throughout their discovery and transition."
The new course from Dr. Meihofer is called "Gender Diversity and Pelvic Health: Comprehensive Care for Transgender Men and Women", and it will be debuting on May 29-31, 2020 in Livingston, NJ.
Dr. Meihofer was kind enough to share some thoughts about the new course, her practice, and herself with The Pelvic Rehab Report. Thank you, Laura!
Tell us about yourself, Laura!
My name is Laura Meihofer and I’ve been a physical therapist for 7 years. I work at Mayo Clinic and I see patients throughout the gender spectrum who most commonly struggle with pelvic floor dysfunctions relating to overactive muscles such as: chronic and acute pelvic pain, urinary frequency/urgency/incontinence/hesitancy, constipation, pain with intercourse, low back and hip pain.
 What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
Currently there are roughly 1.25 million transgender identified individuals in the United States and this number is growing. This course will help to dispel the idea of “other” when treating this demographic and demonstrate how much sameness there is when treating pelvic floor dysfunction.
These skills will greatly benefit any practice as this population is so underserved, they are looking for allies that are not just nice but competent. When you are able to successfully treat gender diverse patients, they spread the word about the great care they received and you now have a strong referral base. Taking this course opens up a whole new referral base of amazing people.
This course will not only feature videos from thought leaders in the field but will also highlight testimonials from patients and caregivers who have undergone their own gender transitions.
What essential skills does your course add to a practitioner’s toolkit?
I think the most important technique that attendees will learn will be how to assess a trans women and trans man after they have undergoing genital reconstruction surgery. Attendees will gain competence in the care of the gender diverse patient at any stage during their gender transition.
What was your inspiration to create this course for trans-identified patients?
Working at a major medical institution, I found that it was difficult finding providers in a patient’s area that were competent in care of a transgender patient. As I talked more and more with various physical therapists I realized they were thirsty for knowledge on how to serve these individuals. So I created the course!
What prepared you to create this course?
The most important thing I have done for this course is treat hundreds of patients who are trans identified throughout their gender journey. This allowed me to not only see all the medical interventions they went through but also to hear their personal journey of transition. These experiences expanded my empathy for what they go through and inspired me to search within myself on how I can be better for them. This desire to improve opened a creative well inside of me from which this course grew.
Discuss the effect conditions covered in your course have on a patient’s quality of life, your experience treating patients with this condition, and how their quality of life has increase after successful treatment.
Individuals who identify as transgender suffer from pelvic floor dysfunction just like our cis gender folks. There is no current data to capture the prevalence of pelvic floor issues in this specific population to date, however there is research to support the overall lack of care these individuals receive. Based on the results from the U.S. Transgender Survey which surveyed 28,000 respondents, the numbers in the health care field were staggering.
33% of respondents had at LEAST one negative experience with a health care provider in the last year due to being transgender. Negative experiences were qualified as verbal harassment, refusal of treatment or having to teach the health care provider about transgender people to receive appropriate care. 23% of respondents did not see a doctor when they needed to due to fear of being mistreated as a transgender person.
This course aims has two primary aims:
1) Educate providers on the unique concerns that transgender individuals experience related to hormone replacement and surgical techniques.
2) Equip attendees to provide competent care for this demographic
Join Dr. Meihofer for Gender Diversity and Pelvic Health this May 29-31, 2020 in Livingston, NJ!
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.

What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
New pain theory also supports that much of pain perception is the body perceiving danger or injury to a nerve. By clearing up the path of the nerve and mobilizing it, we can decrease the body's perception of nerve entrapment and thus create change in pain levels.
What do you hope practitioners will get out of this series that they can't find anywhere else?
I hope they will leave the course able to treat the nerves of the region, which is essentially the transmission pathway for most pelvic pain. I don't know of other courses that have this emphasis.
You've recently split your nerve course in two. Why the split?
I didn't want this class to be a bunch of nerve theory without the manual intervention to make change. After running the labs in local study groups, we found it took more time for people's hands to learn the language, art, and techniques of nerve work. To truly do the work justice and for participants to have a firm grasp of the manual techniques without being rushed, we found it takes time, and I wanted to honor that, as well as treating enough of the related factors and anatomy to make real and lasting change for patients.
How did you decide to divide up content?
Basically, we divided them up by anatomical origin:
The lumbar course covers the nerves of the lumbar plexus, the abdominal wall when treating diastasis, and treatment of the inguinal canal (obturator nerve, femoral nerve, iliohypogastric, ilioinguinal, genitofemoral nerves). Also, the lumbar nerves have more effect in the anterior hip, anterior pelvis, and abdominal wall.
The sacral nerve course covers all the nerves of the sacral plexus (pudendal, sciatic, gluteal/cluneal, posterior femoral cutaneous, sciatic, and coccygeal nerves), as well as subtle issues in the sacral base and subtle coccyx derangement work as well as the relationship with the uterus and sacrum, to take pressure off the sacral plexus. The sacral nerves have more effect in the posterior and inferior pelvis and into the posterior leg and gluteals.
What are the main stories that either course tells?
Both courses tell the story of getting closer to the root of the pain to make more change in less time. Muscles generally just respond to the message the nerve is sending. Yet, by treating the nerve compression directly, we are getting much closer to the root of the issue and have more lasting results by changing the source of abnormal muscle tone. Rather than an intellectual exercise of discourse on nerves, we devote ourselves to the art of manual therapy to change the restrictions on the pathway of the nerve and in the nerve itself.
If someone went to the old nerve course, what's the next best step for them?
The first course was initially all the lumbar nerves with a dip into the pudendal nerve. They would want to take the sacral nerve course, as those nerves were not covered in the first round.
Anything else you would like to share about these courses?
Sure. Essentially, we will take each nerve and do the following:
- Thoroughly learn the path of the nerve
- Fascially clear the path of the nerve
- Manually lengthen supportive structures and tunnels that surround the nerve.
- Directly mobilize the nerve
- Glide the nerve
- Learn manual local regional integration techniques for the nerve after treatment
- Receive handouts for and practice home program for strengthening and increasing mobility in the path of the nerve
Join Nari at one of the following events to learn valuable evaluation and treatment techniques for sacral and lumbar nerves
Upcoming sacral nerve courses:
Sacral Nerve Manual Assessment and Treatment - Winfield, IL
Oct 11, 2019 - Oct 13, 2019
Sacral Nerve Manual Assessment and Treatment - Tampa, FL
Dec 6, 2019 - Dec 8, 2019
Upcoming lumbar nerve courses:
Lumbar Nerve Manual Assessment and Treatment - Phoenix, AZ
Jan 11, 2019 - Jan 13, 2019
Lumbar Nerve Manual Assessment and Treatment - San Diego, CA
May 3, 2019 - May 5, 2019
 In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
If you’ve attended Pelvic Floor Level 1 with Herman & Wallace, you’ll remember we quote a study from Van der Welde about the effects of perceived danger on muscle activity in the upper trapezius and pelvic floor muscles. We also discuss the work of Levine, of ‘Waking the Tiger’ fame, who explores the somatic effects of trauma in our bodies – and how trauma, much like pain, is whatever we say it is.
I became intrigued with the topic, so I was delighted to hear that Lauren Mansell has created a course to deal exactly with this topic. I was even more delighted when she sat down for a chat with me to explore the nuances of trauma awareness, boundary setting and self-care for therapists, especially pelvic therapists, who work with those who have experienced trauma of any kind.
I hope you find this conversation as interesting as I did! Here is our conversation:
1. ‘Vaginismus, a Component of a General Defensive Reaction. An Investigation of Pelvic Floor Muscle Activity during Exposure to Emotion-Inducing Film Excerpts in Women with and without Vaginismus’ van der Velde, J & Laan, Ellen & Everaerd, W. (2001)
2. ‘Waking The Tiger’ by Peter A. Levine (1997)
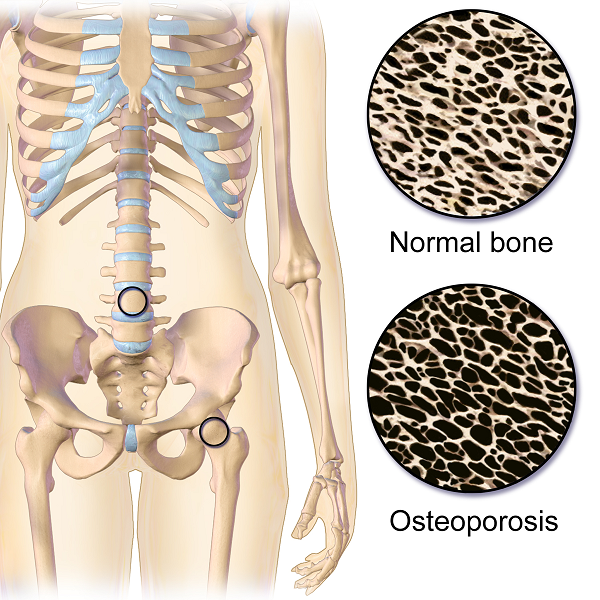
The following case study comes from faculty member Deb Gulbrandson, PT, DPT, a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method. Join Dr. Gulbrandson in The Meeks Method for Osteoporosis on September 22-23, 2018 in Detroit, MI!
The first sight I had of my new patient was watching her being wheeled across the parking lot by her husband. A petite 72-year-old, I could see her slouched posture in the wheelchair. With the double diagnosis of osteoporosis and Multiple Sclerosis (MS) it didn’t look good. However, “Maryanne“ greeted me with a wide grin and a friendly, “I’m so excited to be here. I’ve heard good things about this program and can’t wait to get started.“
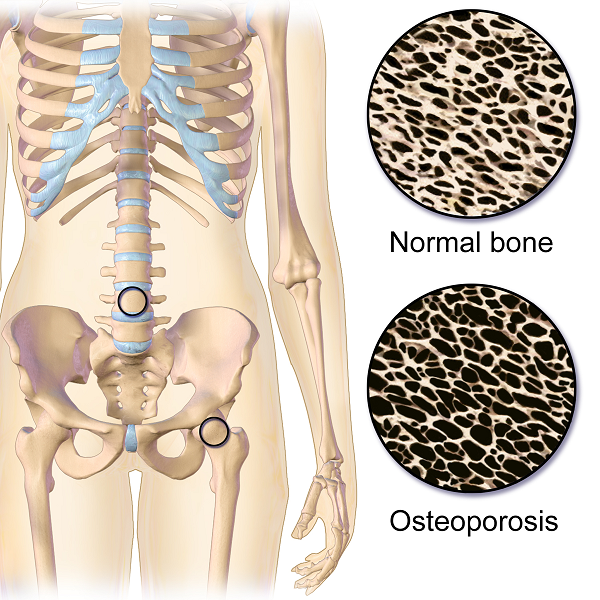 That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
Even though she had been exercising on a regular basis, she was unfortunately doing many of the wrong exercises. Her workout consisted of sit-ups and crunches. She used the Pec Deck bringing her into scapular protraction and facilitating forward flexion. She was also stretching her hamstrings by long sitting reaching to touch her toes.
Spinal flexion is contraindicated in patients with osteoporosis. A landmark study done in 19841 divided a group of women with osteoporosis into 4 groups. One group performed extension based exercises, a second group did flexion. A third group used a combination of flexion and extension and the fourth was the control and did no exercises. Below are the results 1-6 years later.
- Extension Group: 16% incidence of fracture or wedging of vertebral bodies
- Flexion Group: 89% rate.
- Combination Extension/Flexion: 53% rate
- No Exercise Group: 67%
The results were astounding. Granted, it was a small study- 59 participants and it was done a long time ago. But this is a one study that no one wants to repeat, or volunteer for!
Several take home messages followed this study.
- Flexion is contra-indicated for individuals with osteoporosis.
- It’s better to do no exercise than the wrong exercise. The No Exercise group faired better than the Flexion group although at 67% it’s clear that many of our everyday activities- making beds, placing items on low shelves, and now computing and texting put us at risk.
Sadly, many individuals with osteoporosis are told by their physicians to start exercising.......but without any guidance they do what Maryanne did. Just start exercising. And putting themselves at greater risk.
Maryanne was also doing nothing to strengthen her back extensors and scapular area. After giving an overview of the vertebral bodies, pelvis, and hip joint with my trusty spine, I showed both my patient and her husband how forward flexion puts increased compression on the anterior aspect of the spine, particularly in the thoracic curve at T 7, 8, 9, the most common site of compression fractures. We started with Decompression, which is the beginning position for the Meeks method. Many therapists know this as hooklying. This position allows the spinous processes to press against the hard surface of the floor, opening up the anterior portion of the spine and providing tensile forces throughout the length of the spine. With the help of her husband, Maryanne could get down on the floor but I often advise patients who are unable to safely transfer to the floor to lay across the end of their bed. This is less cushy than lying longways where they sleep. Adding a yoga mat or a quilt on top to give more firmness improves the effect.
Supine is the least compressive of all positions; sitting is the most compressive. While Decompression may not seem like much of an exercise it is vital to reduce the effects of gravity and compression on the spine.
We addressed sitting posture by firming up the base of her wheelchair as well as recommending transferring into other chairs and positions frequently throughout the day. Spending time sitting towards the edge of a firm chair in what we call Perch Posture and practicing Foot Presses into the floor created improved alignment in her spine as well as isometrically activating glutes, abs, quads. Using the Foot Press is an example of Newtons 3rd Law, “For every action there’s an equal and opposite reaction” so by pressing her feet down she actually lengthened her torso and head. We also discussed discontinuing the contraindicated exercises in her workout routine and I assured her that the Meeks method would progressively challenge her core (the reason everyone thinks they should do sit-ups) and target the right muscles to help strengthen her bones. We use site specific exercises to target certain muscles that pull on the bone and increase bone strength.2
With instructions to Decompress several times daily to reduce compression on the spine along with the other adjustments made, I felt Maryanne was on her way to reducing her risk of fracture and increasing the quality of her life. She thanked me profusely for the education and the exercise of that session. We both look forward to the next one.
1. Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984 Oct;65(10):593-6.
2. Frost HM1. Wolff's Law and bone's structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64(3):175-88.
My name is Tina Allen. I teach a course called Manual Therapy Techniques for the Pelvic Rehab Therapist. I developed this course in 2016 out of desire to help clinicians feel comfortable in their palpation and hands on skills.
 My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
When I started out there just were not many classes. I spent time learning from physicians, reading anything I could find and applying ‘general ‘orthopedic principles to the pelvis. I traveled to clinics and learned from other clinicians. I soaked up anything I could and brought it back to my clinical practice. When Holly Herman and Kathe Wallace asked me to teach with them I was humbled, honored and terribly nervous. Holly and Kathe where two of my greatest resources and to be able to teach along side them to help others along was humbling. As I prepared to teach I realized the breadth of what we do as pelvic rehab clinicians has grown exponentially since I started out.
Over the past 10 years of teaching the pelvic series with H&W; I noticed that for some of the participants there was a gap in confidence in palpation skills and in treatment techniques applied to the pelvic floor region. For most, it’s confidence in what they are feeling and where they are. This course came out of wanting to fill that gap. I wanted to allow a space that clinicians could come and spend two days learning, affirming and building confidence in their hands. They could then take those skills and confidence back to their clinics and help more patients.
The thought of writing this course was daunting. First off, written words are not my thing. Don’t get me wrong I love to read but me coming up with what to put on paper, much less a power point slide, frightened me. With much encouragement and support from colleagues and H&W, I got to work. The first thing was to think about what techniques to include. At some point after 20 years in the field, your hands just do the work and you don’t think about how you do something. My colleague and dear friend Katy Rice allowed me to sit down with her, practice a technique and then write down each specific step to do the skill. She would read them over and then attempt to do the technique by following only the written instructions. I also had patients who were instrumental in helping me choose what techniques to include. They would say to me “that is what made all the difference for me; it has to be included in what you teach others. “
I would think about who taught me each technique, whether it was a course, another clinician or a patient. I know that I did not make any of these up myself; while I may have modified a technique to work with my hands I did not originate them. Holly Tanner was so kind to brain storm with me and lead me to references for some of the techniques that we as clinicians use every day and that I was planning to include.
What happened next was months of me sitting at the kitchen table combing through books, articles, course manuals and online videos looking for origins of the techniques I use every day in my clinical practice. I wanted to be sure to give credit to sources. It was tedious but also inspiring to realize that some of these techniques have been around and documented since 1956 (Dicke, E., & Bischof-Seeberger, I.) and also that the same techniques are sited by multiple different sources. After about 6 months of our kitchen table not being suitable for dinner it was time to see what I had gathered and how it would all fit together. The result was this 2 day course: Manual Therapy Techniques for the Pelvic Rehab Therapist which has seven labs including internal, external and combination techniques, home program/self care ideas and time for brainstorming treatment progressions. Join me in Philadelphia, PA this October 20 - 21 to learn these essential skills.
Nutrition Perspectives for the Pelvic Rehab Therapist
There are moments when I pause and realize how far we’ve come in a short period of time, and then others when I’m acutely reminded how far we have yet to go. Our destination is an integrative health care system which addresses nourishment first and early versus last, not at all, or only when all else fails. My mission is to support the concept of nourishment first and early though sharing of “Nutrition Perspectives for the Pelvic Rehab Therapist” through the Herman & Wallace Pelvic Rehab Institute.
 After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After the most recent live course event, a participant shared with me a letter she received from a patient in 2016 who mentions the lack of nutritional attention during her cancer treatment. I want to share with you the essence of this letter:
“In October 2015, I was diagnosed with cancer. The following December I started treatments of radiation and chemotherapy. I really appreciate all the fine employees who helped me through care and treatments. Every clinician I came across, whether a doctor, nurse, phlebotomist, radiation and chemo teams, and my PT, were all exceptional in showing care, concern and knowledge.
However, one area I felt was lacking in was nutrition. I was frequently offered a standard hospital-issue protein drink. When offered, I explained that I would not take it due to it containing high fructose corn syrup (HFCS). I asked if they knew that HFCS was like putting and accelerant on a fire? I received a smile and a nod of head as to say they understood.
I was also offered soda pop to wash down bad tasting medicines/ liquids I was to take. I opted to just down the medication without chasing it as I didn’t want to exacerbate my condition. While taking chemotherapy, I was offered snacks containing HFCS and other non-nutritive so-called foods.
I was also offered limited entree choices, but there were plenty of pies, cakes, jellies, and other non-nutritive foods to choose from. All Items I would not consider for a cancer diet or even a healthy diet. I finally took a picture of the menu selection sheet as I thought no one would believe such a thing could happen.
I received excellent care throughout your system with the exception of nutrition . I would ask that you take a look at making menus with truly healthy options as well as giving patients options that do not contain ingredients that feed the cancer.”
While this letter addresses an inpatient issue at one regional health system, it correspondingly brings into focus the irony present in the vast majority of health care settings across the nation from inpatient to outpatient settings: there is a profound lack of clarity about what it means to be nourished, especially when we are at our most vulnerable.
I cannot claim “Nutrition Perspectives” will solve our nation-wide problem, however, I am certainly encouraging a movement towards a collective understanding of the imperative fact that food is medicine - powerful medicine - and we must as front-line practitioners harness what this understanding can offer. Pelvic rehab practitioners are uniquely positioned to process this information and begin immediately sharing it in clinical practice.
Like many providers, this same participant shared with me that upon receipt of this letter two years ago, she struggled to make progress with what and how to offer nutritional information - mainly because of the overwhelming nature of the subject, and also because of the conflicting and oftentimes confusing information traditionally shared with the public. After attending Nutrition Perspectives, she said “I cannot even begin to describe how much your course has met ALL my hopes for helping clients!….I had struggled to put something together and here it all is - so unbelievably grateful.”
And that’s what this course is all about - empowering you as you broaden your scope of knowledge in a way that teaches you not facts, but deep understanding. Once that foundational understanding is laid, this grass-roots effort will progress like putting an accelerant on the integrative movement. Soon we’ll see the inclusion of nourishment information as first-line practice, and the lives impacted in a positive way will continue to grow.
Please join me at the next opportunity to share in this live experience with other like-minded clinicians. Nutrition Perspectives for the Pelvic Rehab Therapist will be coming to Denver, CO September 15 & 16, 2018!