Exciting news! Carolyn McManus, Herman & Wallace instructor of Mindfulness-Based Pain Treatment, will be a presenter in programming at the International Association for the Study of Pain (IASP) World Congress on Pain in to be held in Boston, September 11 - 16. This conference brings together experts from around the globe practicing in multiple disciplines to share new developments in pain research, treatment and education. Participants from over 130 countries are expected to attend. The last time it was held in the U.S. was 2002, so it presents an especially exciting opportunity for those interested in pain to have this international program taking place in the U.S. Carolyn will present a workshop on mindfulness in a Satellite Symposia, Pain, Mind and Movement: Applying Science to the Clinic.
 Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
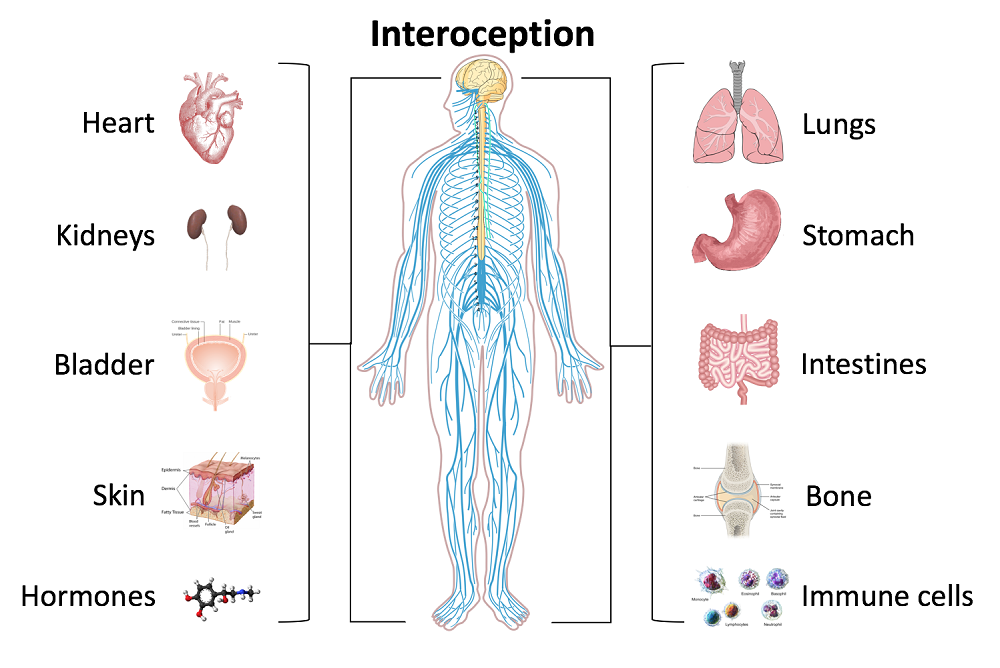
For many patients, pain is not linearly related to tissue damage and interventions based on structural impairment alone are inadequate to provide full symptom relief. Mindfulness training can offer a key ingredient necessary for a patient to make additional progress in treatment. By learning therapeutic strategies to build body awareness and calm an over-active sympathetic nervous system, patients can mitigate or prevent stress-induced symptom escalation. They can learn to move with trust and confidence rather than fear and hesitation.
A growing body of research in mindfulness-based therapies demonstrates multiples benefits for patients suffering with pain conditions. Research suggests that mindfulness training can be helpful to women preparing for childbirth and patients suffering from fibromyalgia, pelvic pain, IBS and low back pain. In addition, for patients with anxiety, mindfulness training may contribute to reductions in anxiety and in adrenocorticopropic hormone and proinflammatory cytokine release in response to stress. Authors of this study conclude that these large reductions in stress biomarkers provide evidence that mindfulness training may enhance resilience to stress in patients with anxiety disorders.
In addition to her presentation at the IASP World Congress Satellite Symposia, Carolyn will be sharing a more in-depth examination and practice of mindfulness in her upcoming course Mindfulness-Based Pain Treatment, August 4 and 5 at Virginia Hospital Center, Arlington VA, and again November 3 and 4 at Pacific Medical Center in Seattle, WA. Please join an internationally-recognized expert for 2 days of innovative training in mindfulness that will both improve your patient outcomes and enhance your own well-being!
Duncan LG, Cohn MA, Chao MT, et al. Benefits of preparing for childbirth with mindfulness training: A randomized controlled trial. BMC Pregnancy Childbirth 2017 May 12;17(1):140.
Fox SD, Flynn E, Allen RH. Mindfulness meditation for women with chronic pelvic pain: a pilot study. J Reprod Med.2011;56(3-4):158-62.
Garland EL, Gaylord SA, Paisson O. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing and affective processing of pain sensations. J Behav Med. 2012;35(6):591-602.
Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized Clinical Trial. JAMA. 2016;315(12):1240-9.
Hoge EA, Bui E, Palitz SA, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328-332.
Last year, I was teaching our Pelvic Floor Series Capstone course. It was the end of day three of the course. Most, students were thanking us for a course that filled in so many gaps in their practice and taught them a whole new way to use their hands. They were feeling energized and excited to bring all the new information back to their patients who had plateaued, so this was a surprising and atypical comment. To those of you who are unfamiliar with Capstone, it is a course for experienced pelvic therapist who have already taken three of the series courses, and it was written to address truly challenging patients, to learn to problem solve with manual therapies, to address all the things that my co-authors and I wished we had known five years into our field. It teaches complex problem solving and more receptive and dynamic use of their hands. So, usually, by this course, therapists are fully committed to this field and geeked-out to get so many more pearls. They are usually on board and looking for more sophisticated tools.
 As one student, Soniya (name changed) was walking out, she said, “I took this course to figure out if I want to treat pelvic patients, and I definitely don’t. It confirmed what I already knew about pelvic rehab being wrong for me.” I was so confused at that point. All I could say in that moment was, “Can you please tell me more about that? I’m interested.”
As one student, Soniya (name changed) was walking out, she said, “I took this course to figure out if I want to treat pelvic patients, and I definitely don’t. It confirmed what I already knew about pelvic rehab being wrong for me.” I was so confused at that point. All I could say in that moment was, “Can you please tell me more about that? I’m interested.”
Soniya went on to explain that she used to be a pelvic therapist. She said she loved it at first. But, she got so enmeshed with her patients and found she stopped having energy for the rest of her life: her kids, her health, her own enjoyment. She said she would go into her “dark cave” treatment room with her patients, isolated with them one at a time, and come out spent and depleted at the end of the day. She clarified that it was rewarding helping people so profoundly, but there came a point when she had to choose between helping others and saving herself. She changed back to outpatient ortho, choosing to treat in the gym, dynamically interacting with other PT’s all day and not being one-on-one in a room with patients and her problems. She also changed to part time, stating she just couldn’t be around patients five days a week anymore.
I understood. I totally got it. I hear this all the time at courses from other pelvic PT’s: that they love what they are doing, and they feel called to this line of help, but ultimately, they are depleted. I have been there. Pelvic rehab can get to be a little confusing with all the blurred lines. There are so many boundaries that are different. We ask our patients questions normal PT’s don’t. We do treatments in areas that other therapists don’t normally touch or see. We are one on one in a private room with our clients. We know more private details about our patients than most of their friends and family. And…we care deeply and listen intently….sometimes many hours a day to stories of other people’s pain, fears, and stress. Often, we are a lone pelvic practitioner in a practice with other kinds of PT’s. Let’s face it, our colleagues who don’t do pelvic rehab think we are a little weird! With HIPPAA, we can’t talk to our coworkers about our heart wrenching stories. We are also not trained psychologists, and our training in PT school really didn’t address how to deal with all we face in a day, especially the psychological aspects.
A recent study found nursing students show compassion fatigue before they even graduate and that “Therefore, knowledge of compassion fatigue and burnout and the coping strategies should be part of nursing training”. Yet, as pelvic therapists we are taught to recognize signs of trauma in our patients, but we are not yet taught how to stop ourselves from being traumatized.
I asked “Soniya” if it had worked for her: changing back to outpatient ortho and going part time. She said it had for the most part. She felt she had her life and energy back for the most part.
So, I asked “Soniya” how she landed at Capstone? What brought her here? It turns out her boss had asked her to come to Capstone and consider going back to pelvic rehab. So, she came and heard about all kinds of problem solving and new research with very complex patients at Capstone: cancer, multiple surgeries, systemic inflammation, endometriosis, and even gender affirming/change surgeries. She learned about complex hormonal issues, pharmacology and anatomy she hadn’t ever considered as an experienced pelvic therapist. She spent around 10 hours that weekend in lab, learning new ways to use her hands to make change. At the end, she said the thought of going “back in the cave” with such complex patients and having her hands on them all day long was draining to her. She just couldn’t go back.
There is a point where caring so much and wanting to help becomes counter-productive to us, until we burn out. We can develop true compassion fatigue. Compassion fatigue makes us feel apathetic, spent, and sometimes even jaded or cranky. But, how do we turn that caring off in time? Our compassion is what led us to this field in the first place.
This post is a two-part series on practitioner burnout and compassion fatigue from faculty member Nari Clemons, PT, PRPC. Nari helped to create the advanced Pelvic Floor Series Capstone course, which is available several times each year. Nari is also the author and instructor for Boundaries, Self-Care, and Meditation, Lumbar Nerve Manual Assessment and Treatment, and Sacral Nerve Manual Assessment and Treatment. Stay tuned for part two in an upcoming post on The Pelvic Rehab Report!
Mathias CT, Wentzel DL. Descriptive study of burnout, compassion fatigue and compassionsatisfaction in undergraduate nursing students at a tertiary education institution in KwaZulu-Natal. Curationis. 2017 Sep 22;40(1):e1-e6. doi: 10.4102/curationis.v40i1.1784. PMID: 2904178
I’m Elizabeth Hampton PT, DPT, WCS, BCB-PMD and I teach “Finding the Driver in Pelvic Pain”, which offers practitioners a systematic screening approach to rule in or rule out contributing factors to pelvic pain. This course helps clinicians to understand and screen for the common co-morbidities associated with pelvic floor dysfunction, like labral tears, discogenic low back pain, nerve entrapments, coccygeal dysfunction, and more. Importantly, it also coaches clinicians to organize information in a way that enables them to prioritize interventions in complex cases. I've noticed that there are some questions that course participants frequently have as they talk through common themes in their care challenges and wrote this blog to share some clinical pearls you may find to be helpful for your own practice or as an explanation to your clients.
Here are some of the most common questions that I get when teaching Finding the Driver in Pelvic Pain:
1) Question: How do I even start to organize information when a client has a complex history and I am feeling overwhelmed?
I write down a road map with key categories: Bowel and bladder; Spine; Sacroiliac Joint/Pubic Symphysis; Hip; Pelvic floor muscles; biomechanics; respiration; neural upregulation; whatever details can be fit into ‘big buckets’ of information. I use it to both organize my thoughts for my notes, as well as educate the client as to what my findings are and the design of their treatment program.
2) Question: How do you get your clients to do a bowel and bladder diary?
I am proud to say that I can talk anyone into a 7 day bowel and bladder diary because I tell them how incredibly helpful it is to understand the way their body responds to what they eat, drink, and daily habits. It’s my secret weapon to snag clients to start connecting with their body and listening to their details, educate about defecation ergonomics and what happens in multiple systems when there is pelvic floor overactivity. It’s a great teaching tool that facilitates self-reflection and how their self-care choices impact their body’s behavior.
3) Question: How do you educate clients about pelvic floor function so they don’t focus so much on Kegels?
Pelvic floor muscles do three things:
-
They contract gently, or powerfully, with no discomfort, and totally normal breathing; PFMs should have the same kind of nuanced control like your voice does: they should be able to do a gentle contraction, like a “whisper” or a powerful contraction, like a “shout”, depending on the task position and intent.
-
They relax fully and completely when the body is resting in support, or they should be able to relax to a supportive level when they are needed posturally. Relaxation should be its own celebrated event!
-
They should be able to relax and gently lengthen.
Faculty member Elizabeth Hampton PT, DPT, WCS, BCB-PMD is the author and instructor of Finding the Driver in Pelvic Pain, a course designed to help practitioners utilize differential diagnosis in evaluating pain. Join Dr. Hampton in Portland, OR on July 27-29, 2018 or November 2-4, 2018 in Phoenix, AZ.
Tiffany Ellsworth Lee MA, OTR, BCB-PMD joined the Herman & Wallace faculty to teach a course on biofeedback along with Jane Kaufman, PT, M.Ed, BCB-PMD. The month of April is Occupational Therapy month, and we are celebrating by highlighting the role that Occupational Therapists play in pelvic floor rehabilitation. Tiffany founded a biofeedback program at Central Texas Medical Center in San Marcos in 2004, and currently runs her a pelvic rehab private practice .
 Working in this area of biofeedback is extremely rewarding and fulfilling to help change peoples’ lives. I have a private practice now exclusively dedicated to treating patients with pelvic floor dysfunction. I became involved in working with patients with incontinence and pelvic floor disorders because of many opportunities along my career path. I have been an Occupational Therapist since 1994. Both of my parents are also OTs, so I think I was born to do this!
Working in this area of biofeedback is extremely rewarding and fulfilling to help change peoples’ lives. I have a private practice now exclusively dedicated to treating patients with pelvic floor dysfunction. I became involved in working with patients with incontinence and pelvic floor disorders because of many opportunities along my career path. I have been an Occupational Therapist since 1994. Both of my parents are also OTs, so I think I was born to do this!
Erica Vitek, MOT, OTR, BCB-PMD, PRPC wrote a blog recently about the role of OTs in pelvic health. She writes:
“As we look closer at the framework and the definition of OT (Occupational Therapy Practice Framework: Domain and Process, 3rd edition 2014), there is clear evidence that the occupational therapist (OT) has a role in the treatment of pelvic health conditions. Importantly, occupations are defined by this document as ‘…various kinds of life activities in which individuals, groups, or populations engage, including activities of daily living (ADL), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation.”
The clearest examples of the OT’s role in pelvic health occupations within this section include:
- ADL section: toileting and hygiene (continence needs, intentional control of bowel movements and urination) and sexual activity.
- IADLs section: sleep participation (sustaining sleep without disruption, performing nighttime care of toileting needs).
- Achieving full participation in work, play, leisure, and social activities, requires one to be able to maintain continence in a socially acceptable manner in which they can feel confident and comfortable to fulfill their roles and duties.
"We believe that the great patient need that exists can be better served by having trained OTs able to treat pelvic health conditions"
How to get started as an OT
Occupational therapists wishing to pursue pelvic floor have a few options. The first thing is to find a pelvic floor clinical setting or work with their respective settings to check to see if they can start a women's health program with a strong focus on pelvic floor. OTs quite often do not start out in pelvic health directly after school and since this is a newer area as compared to other certifications such as the NDT and PNF it takes a little bit of research, time and effort to find one’s exact niche. To get started, an OT should seek out courses that teach the basics of bladder and bowel management. It is important to understand the anatomy and physiology of the bladder, bowel, and sexual systems.
Incontinence and pelvic floor disorders have a profound impact on occupation, the daily activities that give life meaning! OTs should have a larger role in treating this patient population. Offering hope to our patients is imperative when he/she is dealing with pelvic floor dysfunction!
Keep an eye out for an upcoming post from Tiffany with some inspiring clinical case studies. You can join Tiffany and Jane Kaufman in Biofeedback for Pelvic Muscle Dysfunction to get lots of hands-on time with surface eletromyography, and to work toward BCIA certification!
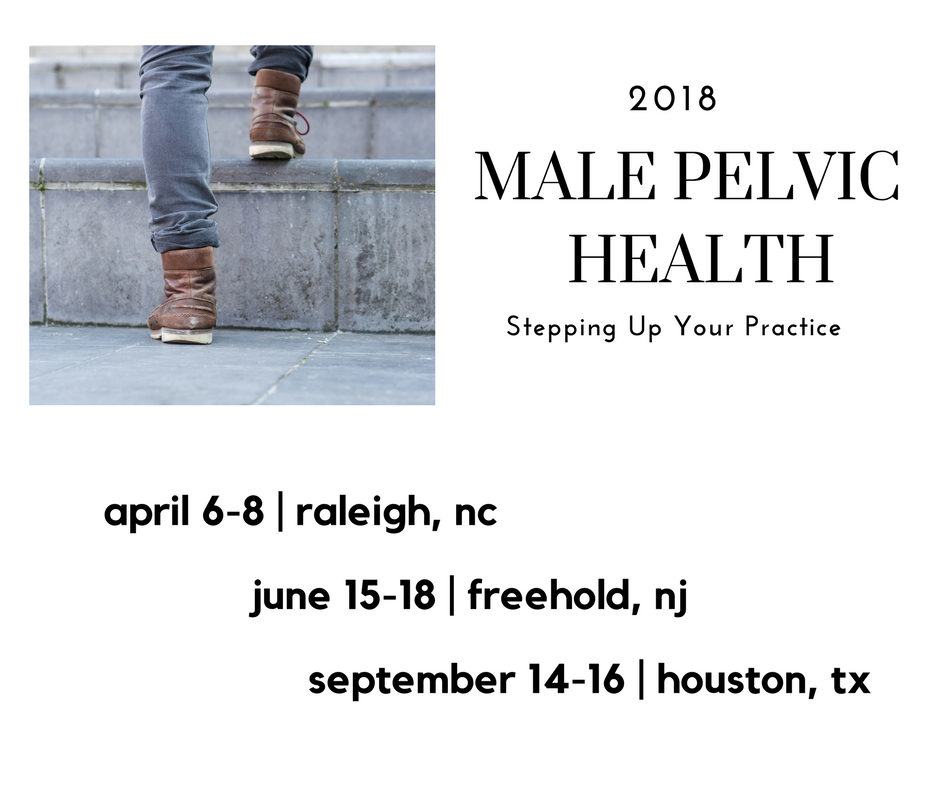
Sara Chan Reardon, DPT, WCS, BCB-PMD is a pelvic floor dysfunction specialist practicing in New Orleans, LA. Sara was named the 2008 Section on Women’s Health Research Scholar for her published research on pelvic floor dyssynergia related constipation. She was recognized as an Emerging Leader in 2013 by the American Physical Therapy Association. She served as Treasurer of the APTA’s Section on Women's Health and sat on their Executive Board of Directors from 2012-2015. Today she was kind enough to share a bit about her course Post-Prostatectomy Patient Rehabilitation, which is taking place twice in 2018.
 My name is Sara Reardon, and I teach the Post-Prostatectomy Patient Rehabilitation course, which I wrote and developed in the year 2015. At the time, I had been a pelvic health Physical Therapist for over 10 years. Earlier in my career, I had taken the Pelvic Floor 2A course by Herman and Wallace Institute, which was a fantastic and thorough introduction to treating a male patient.
My name is Sara Reardon, and I teach the Post-Prostatectomy Patient Rehabilitation course, which I wrote and developed in the year 2015. At the time, I had been a pelvic health Physical Therapist for over 10 years. Earlier in my career, I had taken the Pelvic Floor 2A course by Herman and Wallace Institute, which was a fantastic and thorough introduction to treating a male patient.
Over the years, I started seeing more and more men with post-prostatectomy urinary incontinence and erectile dysfunction in my clinic. Urinary incontinence is the most common and costly complication in men following prostate removal surgery, and their quality of life is directly related to their duration of experiencing those symptoms. Evidence supports that pelvic floor muscle training started as soon as possible after surgery can help decrease incontinence and improve quality of life. I enjoyed being able to help men decrease their incontinence and improve their other symptoms after all they had been through following a cancer diagnosis and treatment.
No courses focused specifically on treating post-prostatectomy pelvic floor dysfunction were offered at the time, so I scoured the research, shadowed with physicians, observed surgeries, and attended urology conferences to understand how to effectively treat these individuals. Treating this population of men is fun, fulfilling, and rewarding, and I was inspired to help other pelvic health physical therapists dive deeper as I witnessed the impact pelvic health physical therapy can have on the quality of life of these patients. I love teaching this course, and I am excited to help other pelvic health professionals learn evidence based and effective treatment strategies to help these men navigate their recovery after prostatectomy.
Join Dr. Reardon in Philadelphia, PA on June 2-3, 2018 or in Houston, TX on November 10-11, 2018 to learn evaluation and treatment techniques for men recovering from prostatectomy surgery.
In an effort to provide the best possible educational experience for clinical rehabilitation application of neuroanatomy, I was on a mission. Having a core, base knowledge review of the nervous system is essential when leading into talking about dysfunction and disease of that system. I went on a search for anatomical depictions that could clearly identify the structures and processes I was trying to portray. New books from the library and books I own from when I was in college serve as great resources when trying to get back into studying the specifics, but do not offer the opportunity to easily get these images into a powerpoint. Online resources are also challenging. I am learning how time consuming the process can be to determine who owns the online image, if it is free to copy, save and utilize for my own teaching purposes, or if I need to go through the process of requesting permissions for use.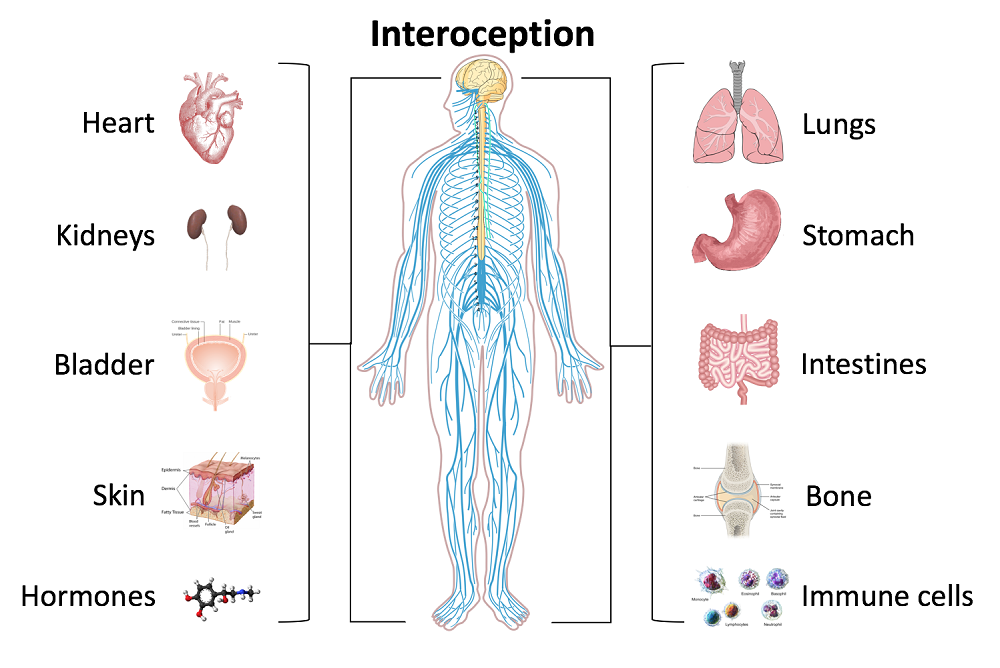
Through my employer, where I treat patients in the clinic, I have access to a program called Primal Pictures. I had used this in the past for clinic related marketing presentations and educational materials for patients and other clinicians I have mentored. Looking into the product further, I came to find out that there is a newer version of the program which offered so many more options. A truly unlimited amount of images which can be manipulated into an optimal position depicting the most clear neuroanatomical views I have ever been able to find. Not only does it provide me with the images I need in order to depict the treacherous pathways of the nerves in our body, but it also provides some amazing depictions of the physiological processes that occur within our nervous system to allow for healthy day to day functioning and protection of our bodies.
I also came across the title of a journal article that I was sure would provide some excellent depictions of neuroanatomy. The article titled, Sectional Neuroanatomy of the Pelvic Floor, provides cross sectional views of both the male and female pelvises. I obtained the article which has an excellent color-coded system, each nerve colored the same as the muscles and skin surface it innervates, going from superior to inferior cross sections. This makes for a clear understanding of each structures anatomical position. It is a great reference when looking at the anatomical relationships to adjacent structures and can help guide palpation skills. The article was more specifically written for physicians to best direct needle procedures/injections in the most accurate location possible when targeting nerves and structures. Neuroanatomy and physiology can be essential to understanding certain patient populations we encounter as we practice pelvic floor rehabilitation. Having clear depictions to refer to can help you provide the best possible base knowledge to your patients as you help them understand the challenges they face and how to overcome them.
Kass, J. S., Chiou-Tan, F. Y., Harrell, J. S., Zhang, H., & Taber, K. H. (2010). Sectional neuroanatomy of the pelvic floor. Journal of computer assisted tomography, 34(3), 473-477.
In 2007, after only speaking on the phone and never meeting in person, my new friend and colleague Stacey Futterman and I presented at the APTA National Conference on the topic of male pelvic pain. It was a 3 hour lecture that Stacey had been asked to give, and she invited me to assist her upon recommendation of one of her dear friends who had heard me lecture. I still recall the frequent glances I made to match the person behind the voice I had heard for so many long phone calls.
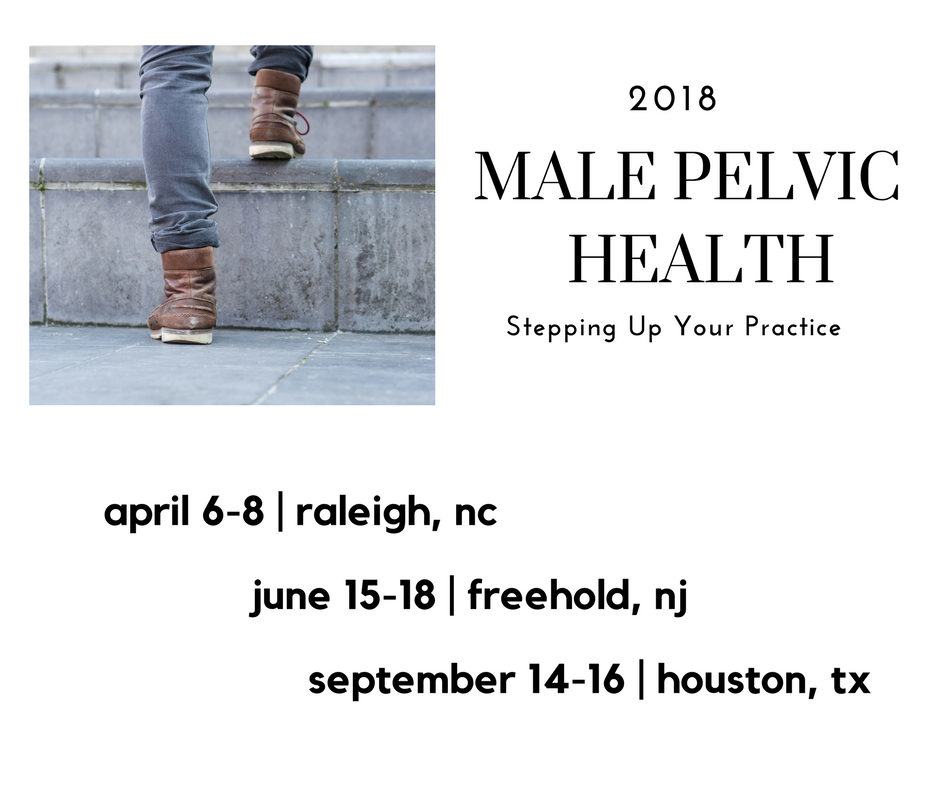 Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Make no mistake- women’s health topics were and are deserving of much attention in our typically male-centered world of medicine and research. Maternal health in the US is dreadful, and gone are the days when providers should allow urinary incontinence or painful sexual health to be “normal”, yet it is often described as such to women who are brave enough to ask for help. Times have changed for the better for us all.
The Male Pelvic Floor Course was first taught in 2008, and so far, 22 events have taken place in 18 different cities. 73 men have attended the course to date, with increasing numbers represented at each course. Rather than 20-25 attendees, the Institute is seeing more of the men’s health course filling up with 35-40 participants. In my observations, the men who attend the course are often very experienced, have excellent orthopedic and manual therapy skills, and have personalities that fit very well into the sensitive work that is pelvic rehabilitation.
The course was expanded to include 3 days of lectures and labs, and this expansion allowed more time for hands-on skills in examination and treatment. The schedule still covers bladder, prostate, sexual health and pelvic pain, and further discusses special topics like post-vasectomy syndrome, circumcision, and Peyronie’s disease. In my own clinical practice, learning to address penile injuries has allowed me to provide healing for conditions that are yet to appear in our journals and textbooks. As I often say in the course, we are creating male pelvic rehabilitation in real time.
Because the course often has providers in attendance who have not completed prior pelvic health training, instruction in basic techniques are included. For the experienced therapists, there are multiple lab “tracks” that offer intermediate to advanced skills that can be practiced in addition to the basic skills. Adaptations and models are used when needed to allow for draping, palpation, and education when working with partners in lab, and space is created for those therapists who want to learn genital palpation more thoroughly versus those who are deciding where their comfort zone is at the time. One of the more valuable conversations that we have in the course is how to create comfort and ease in when for most us, we were raised in a culture (and medical training) where palpation of the pelvis was not made comfortable. Hearing from the male participants about their bodies, how they are affected by cultural expectations, adds significant value as well.
We need to continue to create more coursework, more clinical training opportunities so that the representation of those treating male patients improves. If you feel ready to take your training to the next level in caring for male pelvic dysfunction, this year there are three opportunities to study. I hope you will join me in Male Pelvic Floor Function, Dysfunction and Treatment.
The following is the first in a series of posts by Erica Vitek, MOT, OTR, BCB-PMD, PRPC. Erica joined the Herman & Wallace faculty in 2018 and is the author of Neurologic Conditions and Pelvic Floor Rehab.

Looking back, being passionate about how to physically exercise a person with Parkinson disease to produce the best functional outcome actually became a passion of mine when I was offered my first job. I was thrown into treating people with Parkinson disease in an acute care setting. I had very limited knowledge about Parkinson disease at the time, but I learned quickly from the vast opportunity that was offered to me through my place of work, which was the regions sought after Parkinson disease center of excellence. At the same time, I was eager to further advance my skills as a pelvic floor therapist, which I developed a substantial interest in when I was in college.
As I learned more about what people with Parkinson disease had to manage in their daily lives, it became very clear to me that autonomic dysfunction was a very challenging, and sometimes disabling, aspect of the disease. Being knowledgeable about the neurological and musculoskeletal system along with the urinary, gastrointestinal, and sexual systems seemed to fit well together but there was no specific place to go to combine this knowledge. The research I began collecting on this topic was abundant and very intriguing. Bringing this information together could be practice changing for me to help people living with Parkinson disease.
As clinicians, we already know how to be understanding about the very personal details of the people we work with. People with Parkinson disease deal with an extra layer of challenge, such as, bradykinesia, freezing of gait, and tremor affecting their day to day self-care and relationships. Adding urinary incontinence, constipation or sexual dysfunction to the list makes for even more difficult management.
How does one clinician share their passion with other clinicians that also have the same desires to give the best care to their patients with Parkinson disease? Having a great deal of respect for Herman and Wallace and what they have to offer clinicians practicing pelvic rehabilitation, it seemed like it could be the perfect fit for a course like this. The work that would lie ahead if this idea took off was overwhelming but did not hinder me from my proposal. In fact, it has led to an even larger scope addressing the of treatment of the pelvic floor for a multitude of neurologic conditions many of us see daily in our clinics. Pulling it all together to share is a process that will reward not only people with Parkinson disease in my practice but hopefully yours as well.
As brain research in pain processing suggests, pain engages overlapping cortical networks responsible for nociception, cognition, emotion, stress and memory, a treatment model targeting nociceptive mechanisms alone can be inadequate to address the complexities of a patient’s pain experience.1 To help physical therapists understand and more effectively address multiple factors influencing a patient’s pain, the APTA, Orthopaedic Section and Pain Management Special Interest Group have brought together 10 physical therapists and a physician from around the country to present an informative and dynamic 2-day pre-conference course, Keep Calm and Treat Pain, Feb 21 and 22 at CSM 2018 in New Orleans. Presentation topics include the Science of Pain, Pain Education, Pain Psychology, Motivational Interviewing and Sleep and Pain. In addition, I will present An Introduction to Mindful Awareness Training and Its Role in Pain Treatment, and my colleague at Herman and Wallace, Megan Pribyl, PT, MSPT, will present Pain and Nutrition: Building Resilience Through Nourishment.
 As we are in the midst of the opioid crisis, this programming could not come at a better time. In this regard, I am especially excited to share information on how mindfulness training has been shown to help patients who are reducing opioid medications to increase positive affect, decrease pain interference and reduce opioid craving.2, 3 I will also describe how mindful awareness training helps address a patient’s fears and fear avoidant behavior and will guide mindfulness exercises.4, 5
As we are in the midst of the opioid crisis, this programming could not come at a better time. In this regard, I am especially excited to share information on how mindfulness training has been shown to help patients who are reducing opioid medications to increase positive affect, decrease pain interference and reduce opioid craving.2, 3 I will also describe how mindful awareness training helps address a patient’s fears and fear avoidant behavior and will guide mindfulness exercises.4, 5
I am honored to be a part of this pioneering program that combines didactic presentations with experiential exercises and lab practice to offer participants the latest science of pain and practical skills to more successfully treat pain. In addition, I am presenting an Educational Session sponsored by the Federal Section on the topic Mindful Awareness Training for Veterans with Comorbid Pain and PTSD based on my research experience at the Puget Sound VA in Seattle. I hope to see you at CSM!
While these presentations offer a taste of mindfulness training to improve patient outcomes, they provide just a glimpse into its potential. My joy and passion is my course, Mindfulness-Based Pain Treatment, where I can offer an in-depth exploration of the role mindful awareness training in pain treatment through a thorough review of mindfulness and pain research, the detailed exploration of the application of mindful awareness training to the biopsychosocial pain model and multiple experiential exercises and lab practices that provide participants with practical strategies to bring into the clinic Monday morning. I hope you can attend a Mindfulness-Based Pain Treatment course offered by Herman and Wallace in 2018 at Samuel Merritt University in Oakland, CA, June 9 and 10, Virginia Hospital Center in Arlington VA Aug 4 and 5, or Pacific Medical Center in Seattle, WA Nov 3 and 4. I look forward to helping you expand your toolbox of treatment techniques for patients with pain conditions.
1. Simons LE, Elman, I, Borsook D. Psychological processing in chronic pain: a neural systems approach. Neurosci Biobehav Rev. 2014;39:61-78.
2. Garland EL, Thomas E, Howard MO. Mindfulness-Oriented Recovery Enhancement ameliorates the impact of pain on self-reported psychological and physical function among opioid-using chronic pain patients. J Pain Symptom Manage. 2014;48(6):1091-9.
3. Garland EL, Froelinger B, Howard MO. Neurophysiological evidence for remediation of reward processing deficits in chronic pain and opioid misuse following treatment with Mindfulness-Oriented Recovery Enhancement: exploratory ERP findings from a pilot RTC. J Behav Med. 2015;38(2):327-36.
4. Schutze R, Rees C, Preece M, Schutze M. Low mindfulness predicts pain catastrophizing in fear avoidance model of chronic pain. Pain. 2010; 148(1):120-7.
5. Jay J, Brandt M, Jakobsen MD, et al. Ten weeks of physical-cognitive-mindfulness training reduces fear-avoidance beliefs about work-related activity. Medicine (Baltimore). 2016;95(34):e3945.
“Keep Calm and Treat Pain” is perhaps an affirmation for therapists when encountering patients suffering from pain, whether acute or chronic. The reality is this: treating pain is complicated. Treating pain has brought many a health care provider to his or her proverbial knees. It has also led us as a nation into the depths of the opioid epidemic which claimed over 165,000 lives between the years of 1999 and 2014 (Dowell & Haegerich, 2016). That number has swollen to over 200,000 in up-to-date calculations and according to the CDC, 42,000 human beings, not statistics, were killed by opioids in 2016 - a record.
 So why has treating pain eluded us as a nation? The answers are as complicated as treating pain itself. Which is why we as health care providers must seek out not simply alternatives, but the truth in the matter. Why are so many suffering? Why has chronic pain become the enormous beast that it has become? What might we do differently, collectively, and how might we examine this issue through a holistic mindset?
So why has treating pain eluded us as a nation? The answers are as complicated as treating pain itself. Which is why we as health care providers must seek out not simply alternatives, but the truth in the matter. Why are so many suffering? Why has chronic pain become the enormous beast that it has become? What might we do differently, collectively, and how might we examine this issue through a holistic mindset?
In just a few weeks, I have the privilege of teaching amongst 10 physical therapy professionals and one physician from around the nation who with coordinated efforts created a landmark pre-conference course at CSM in New Orleans through the Orthopaedic Section of the APTA. Included in the 11 are myself and another Herman & Wallace instructor Carolyn McManus, PT, MS, MA who teaches “Mindfulness Based Pain Treatment” through the Institute.
The CSM pre-conference course title is “Keep Calm and Treat Pain” representing a necessary effort to provide the clinician with ideas and inspiration for helping the profession as a whole treat pain with an integrative approach.
“Pain and Nutrition: Building Resilience Through Nourishment” is the section I look forward to sharing. It will introduce concepts we can leverage to allow us confidence in seeking alternate ways of taming this beast which is chronic pain - ways which can enhance health and well-being of our clients in pelvic rehabilitation. We must not be passive observers of the opioid epidemic. We must come to terms with the fact that our nations go-to tool for treating pain unfortunately causes side-effects which can and does include loss of life. We can do better. And we will.
While the CSM pre-conference course will give you a taste of the nutrition concepts available to you, it is a mere tip of the nourishment iceberg. I continue my passion and mission with the two-day course titled “Nutrition Perspectives for the Pelvic Rehab Therapist”, an experience that can elevate your conversations with clients. It will pave a path of understanding for the provider, allowing us to share options, understanding, and hope. “Nutrition Perspectives for the Pelvic Rehab Therapist is coming next to Maywood, IL March 3 & 4, 2018. I welcome you to join me.
APTA CSM: https://apta.expoplanner.com/index.cfm?do=expomap.sess&event_id=27&session_id=13763. Accessed January 8, 2018.
CDC: https://www.cdc.gov/drugoverdose/index.html. Accessed January 8, 2018.
Dowell, D., & Haegerich, T. M. (2016). Using the CDC Guideline and Tools for Opioid Prescribing in Patients with Chronic Pain. Am Fam Physician, 93(12), 970-972.
Lerner, A., Neidhofer, S., & Matthias, T. (2017). The Gut Microbiome Feelings of the Brain: A Perspective for Non-Microbiologists. Microorganisms, 5(4). doi:10.3390/microorganisms5040066
Murthy, V. H. (2016). Ending the Opioid Epidemic - A Call to Action. N Engl J Med, 375(25), 2413-2415. doi:10.1056/NEJMp1612578