Aparna Rajagopal, PT, MHS, WCS, PRPC, Capp-OB Certified is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interest in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction.
Leeann Taptich DPT, SCS, MTC, CSCS leads the Sports Physical Therapy team at Henry Ford Macomb Hospital where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
Aparna and Leeann co-authored the course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Abdominal bloating and distension are two very commonly reported GI symptoms in the pelvic practice setting. However, these symptoms are not commonly recognized in other physical therapy settings. While many people experience occasional bloating/discomfort it does not necessitate medical intervention, but repeated and long-standing bloating/distention can impact the quality of life.
One diagnosis which is associated with these symptoms is Abdomino-Phrenic dyssynergia where patients develop a paradoxical abdomino-phrenic response. Normally, as a response to an increase in intraluminal gas, the diaphragm relaxes, and the abdominal musculature contracts. When dyssynergia is present, the opposite happens and the diaphragm contracts, and the abdominals relax. Abnormal pelvic floor function is also associated with this diagnosis. Treatments typically used are biofeedback therapy and breathing techniques.
Where Leeann and I work, we are seeing patients increasingly referred with this diagnosis. Recently we treated a 72-year-old female patient with a long-standing history of troublesome bloating and distention, with the diagnosis of Abdomino phrenic dyssynergia.
- The patient had complaints of bloating and abdominal distension all day long, worsening toward evening
- She reported limiting her food intake in the evenings on account of the discomfort and "tightness" in the abdomen
- She rated the discomfort as 3-5/10 in the morning time with an increase to 8/10 by late evening
- She also reported poor sleep because of how "hard and tight" the abdomen felt by bedtime
Upon examination, amongst other findings, the patient demonstrated:
- Significant tightness in her posterior chain and her erector spinae in both thoracic and lumbar regions
- Decreased thoracic rotation/mobility
- Increased connective tissue restrictions in both upper abdominal quadrants, especially in the epigastric area and inferior to the rib cage
- Decreased lower rib cage mobility
- Poor ability to prolong exhale or to exhale strongly
- Decreased ability to relax the pelvic floor musculature after a contraction
In addition to biofeedback and visceral mobilizations, treatment techniques included joint mobility techniques inclusive of simple rib and thoracic spine mobilizations, soft tissue mobility techniques including gentle diaphragm releases, breath training, and breathing techniques to aid in pelvic floor relaxation.
The patient received 9 treatment sessions and a home maintenance program which she followed with good compliance. She reported a 70% overall improvement and was now able to sleep through the night and eat in the evenings without discomfort.
In our course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, you will learn:
- Explain normal diaphragmatic breathing and the role of the internal and external oblique musculature.
- Assess and treat dysfunctional breathing patterns including but not limited to chest, abdominal, and paradoxical breathing patterns.
- Understand the concept of Intra-Abdominal Pressure (IAP) and the control and use of IAP with the diaphragm in a lowered position as a stabilizing mechanism for the spine.
- Understand the concept of regional interdependence and its application in the treatment of back or pelvic pain patients.
- Recognize the effects of postural patterns and the linkage to the diaphragm and pelvic floor.
- Understand the muscles and myofascial components involved in dysfunctional breathing and techniques to effectively treat the same.
- Understand and demonstrate mobilizations of the rib and thoracic spine and develop a comprehensive treatment program.
- Develop an exercise progression for dysfunctional breathing for use in the clinic and in-home programs.
- Integrate diaphragmatic breathing and mobility in the athletic clientele

Course Dates: April 22-23
Price: $450
Experience Level: Beginner
Contact Hours: 14
Description: This remote course is an integrated approach where participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes while looking at structures from the glottis and the cervical region to the pelvic floor.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. Instructed techniques are applicable to patients who present with Diastasis Rectus Abdominis, pelvic pain, incontinence, and prolapse, as well as cervical, thoracic, scapular, and lumbar pain.
Aparna Rajagopal, PT, Mhs, PRPC, and Leeann Taptich, PT, DPT are the authors and instructors of the Breathing and the Diaphragm remote course. Aparna and Leeann bring a wealth of experience to this course.
Aparna: About 10-plus years ago I had a patient who had a large para esophageal hernia which had been surgically repaired. She had been referred to therapy because of general debility and weakness and she couldn't do endurance-based things like gardening or walking for long periods of time. She was in her mid-sixties. She had seen 2 or 3 therapists and they couldn’t figure things out. She had the same complaint that she couldn’t breathe and every time she said she couldn’t breathe the therapist would obviously refer her back to the doctor who would run cardiac tests, and all kinds of other tests and say she was cleared from a medical standpoint and then send her back to therapy. So in this process, the patient came to me and one of the first things she said was that she had difficulty taking in a breath of air -that she felt like she couldn’t expand - not that she couldn’t breathe.
Based on that complaint, I started my assessment. I started looking at the thoracic spine and found that she actually couldn’t expand from the rib cage at all because of her surgery to fix her large para esophageal hernia. One of the things we know about para esophageal hernias is also that it can be associated with increased intraabdominal pressure - related to things like chronic severe constipation, chronic cough, etc. She got better. She healed, and I realized that this was something that patients needed. In the process of treating her, my interest in breathing and the diaphragm developed.
Leeann: I started at Henry Ford Health Systems, where Aparna and I currently work together, about 7 years ago. Around that time, Aparna did a one-hour lecture on dysfunctional breathing and breathing to help us understand the mechanics of the pelvic floor and the abdominals, and the diaphragm. I’ve always looked for my missing link in my treatment, specifically in my lumbar/low back pain patients. The lecture was a lightbulb moment for me, and it made sense to me. What I used to focus on at that time was Transverse Abdominis engagement and it didn't always work for all patients.
I call Aparna my missing link. So, it started off with the one-hour lecture that she delivered. Then we collaborated and worked on developing a four-hour course on the same topic that ended up with eight hours worth of content because of how much great research there was available about the topic. Gradually the four-hour class transitioned into what we have now - a full weekend course. It’s a great mash-up of ortho and pelvic floor approaches for both of us and has really helped both of us treat our patients better from both a pelvic standpoint and an orthopedic standpoint.
Aparna: We work together. We are able to treat patients jointly, bringing in the diaphragm/breathing aspect, incorporating the sports and manual training that Leeann has and the pelvic knowledge that I have. We are able to tie everything together and treat our patients in a very holistic way.
Leeann: My big thing is that we try to incorporate more of the regional interdependence model. When patients come in with symptoms in an area, we look above, below, and beyond to see how the whole system is functioning together. We like to see how the body moves as a whole instead of focusing on just one part of it. That’s where most of our treatment is derived from and how we work together.
Breathing and the Diaphragm - Remote Course
Course Dates:
November 19-20
January 21-22, 2023
Price: $450
Experience Level: Beginner
Contact Hours: 14
Description: This remote course is designed to expand the participant's knowledge of the diaphragm and breathing mechanics. Through multiple lectures and detailed labs, participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi-component system that works together. Optimal function of the diaphragm and breathing patterns are key to a healthy pelvic floor, a normal functioning core, and postural stability. Evidence-based methods to assess the diaphragm and breathing mechanics are presented along with easy-to-apply practical intervention strategies.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. The assessment concepts and treatment techniques can easily be integrated into a therapist's current evaluation and intervention strategies.
Proper breathing is discussed and taught in many ways and forms. All of this is a step in the right direction, but what if the person physically can not lengthen tissues to expand certain key structures that are essential to the breathing mechanism? In the remote course, Breathing and the Diaphragm, Aparna Rajagopal and Leeann Taptich teach different methods to identify breathing patterns, dysfunctional breathers, and how to determine motor control issues from mobility or strength issues.
Breath is utilized widely in the exercise world. Pilates uses breath for core stability. Yoga utilizes breath to help connect the body. Strength and conditioning coaches and personal trainers emphasize breath to provide power to lift. Breathing mechanics, aka proper breathing, is also core to any type of abdominal exercise.
Respiratory muscles are directly involved in these core abdominal strengthening, stability, and stretching exercises (1). Research led by DePalo, way back in 1985, concluded that the diaphragm is actively recruited during resistance exercises such as sit-ups (2). Inefficient breathing can lead to muscular imbalances, and motor control changes that can affect motor quality. Therapists are taught at length about tissue and joint mobility versus motor control or strength issues. These same principles can be applied to assess and treat the diaphragm, breathing, and abdominals.
In regards to working with patients, Aparna shares, "Different cues work with different patients. While verbal and tactile cues to correct patterns can work with some of our patients, they do not necessarily work in all of our patients. We need different ways to correct patterns in patients that have a tissue or joint mobility issue. Such issues can cause restriction and force the patient to breathe in a specific way."
Aparna and Leeann deep dive into mobility and learn to assess and treat joint restrictions of the ribs and the thoracic spine during their remote course Breathing and the Diaphragm scheduled for October 23-24, 2021. These mobility techniques combined with specific motor control and strengthening exercises can improve myofascial restrictions that restrict breathing.
Breathing and the Diaphragm will help build a foundation to improve your patients' functional activities. No matter if it is coughing, having a bowel movement, performing wall ball in CrossFit, or hitting a tennis ball!
- Luca Cavaggioni, Lucio Ongaro, Emanuela Zannin, F. Marcello Iaia, Giampietro Alberti.Effects of different core exercises on respiratory parameters and abdominal strength. J Phys Ther Sci. 2015 Oct; 27(10): 3249–3253. Published online 2015 Oct 30. doi: 10.1589/jpts.27.3249.
- DePalo VA, Parker AL, Al-Bilbeisi F, et al.: Respiratory muscle strength training with nonrespiratory maneuvers.J Appl Physiol 1985 2004, 96: 731–734.
Leeann Taptich DPT, SCS, MTC, CSCS is Co-Author of the new Herman & Wallace offering, Breathing and Diaphragm: Pelvic and Orthopedic Therapist. Leeann leads the Sports Physical Therapy team at Henry Ford Macomb Hospital in Michigan where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
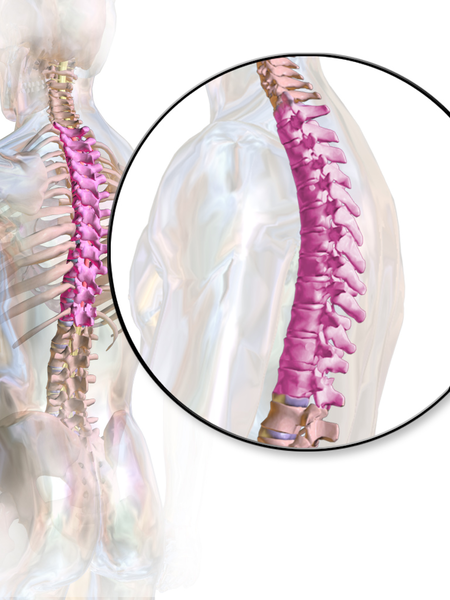
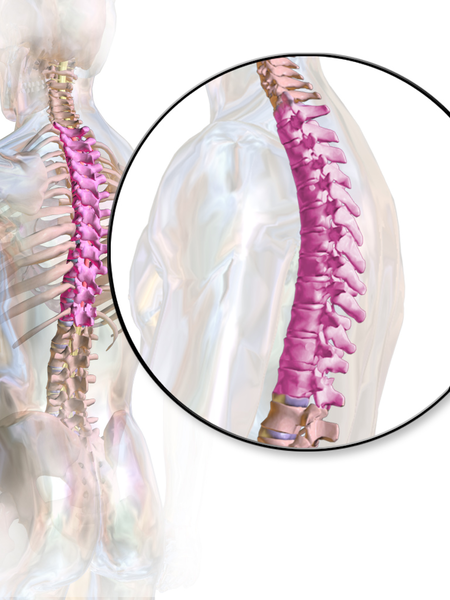 According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
Anatomically, the thoracic spine along with the ribs and sternum provide a frame that supports and protects the lungs and heart. Despite the rigidity that is required to fulfill that function, the thoracic spine contributes significantly to a person’s ability to rotate.2
One of the biggest roles the thoracic spine plays is in the regulation of the Sympathetic Nervous System, which is a part of the Autonomic Nervous System. The sympathetic nervous system, also known as the “Fight or Flight” system is in overdrive in our patients who present with pain. One of the many complications that arise from an upregulated sympathetic system is increased respiratory rate and/or dysfunctional breathing.3 Carefully applied manual therapy techniques to the thoracic region can help regulate the Autonomic Nervous System by affecting the diaphragm, the intercostals, and other respiratory musculature.4 Specific thoracic mobilizations/manipulations can improve respiratory function.4
In the Breathing and Diaphragm course, Aparna Rajagopal and I discuss the importance of the thoracic spine from both a regional and global perspective. Thoracic spine assessment is taught along with multiple mobilization techniques and manipulations all of which will help the clinician link the thoracic spine to the treatment of pelvic pain, low back pain, and breathing pattern disorders. Join Aparna and I in either Sterling Heights, MI this March or Princeton, NJ in December for Breathing and the Diaphragm: Pelvic and Orthopedic Therapists: From Assessment to Clinical Applications for Pelvic and Orthopedic Therapists!
1. Heneghan NR, Rushton A. Understanding why the thoracic region is the ‘Cinderella’ region of the spine. Man Ther. 2016; 21: 274-276.
2. Narimani M, Arjamand N. Three-dimensional primary and coupled range of motions and movement coordination of the pelvis, lumbar, and thoracic spine in standing posture using inertial tracking device. Journal of Biomechanics. 2018; 69: 169-174.
3. Bernston GG. Stress effects on the body: Nervous system. American Psychological Association. https://www.apa.org/helpcenter/stress/effects-nervous. January 18, 2020.
4. Shin DC, Lee YW. The immediate effects of spinal thoracic manipulation on respiratory functions. Journal of Physical Therapy Science. 2016; 28: 2547-2549.