This post was written by H&W instructor Ginger Garner, MPT, ATC, PYT. Ginger will be instructing the course that she wrote on "Yoga as Medicine for Labor and Delivery and Postpartum" in Washington this August.
Note: This post is for colleagues, patients, and friends whose greatest desire is to have a healthy baby via natural childbirth. In this article, natural childbirth refers to an unmedicated delivery of your baby, assisted with natural, non-pharmaceutical means. While not all women have the luxury of natural childbirth, and some choose other means, please know that Ginger’s course supports all women and their personal decisions about birth.

My first natural birth was December 27, 2005. After a long, hard labor that started on Christmas, my son Michael arrived safe and healthy into my arms.
But something was missing.
I could have better prepared for birth. Bradley technique had reinforced that yoga was a wonderful way to relax and give into the sensations of contractions. Prenatal Pilates and walking, along with yoga, had also provided me with the endurance to go the long 36-hour distance during labor.
What was missing was my active, deliberate, and planned participation during birth.
A birth plan helps to organize your thoughts, but a mother needs her own, personal birth plan too. After Michael’s birth, I began to create my own future personal birth plan, which also changed the way I saw, and helped, my own prenatal patients.
That personal birth plan carried me beautifully (and with less pain and more control) through my next two births, William and James. An n of 2 (subject size of 2, in research terms) was small, but very soon after science began investigating the actual effects of using yoga for childbirth preparation and actual labor and delivery. The results are very promising, as I’ll discuss below.
Expectant women should work directly with an experienced physical therapist to create their own personal birth plan based on their individual mind-body needs. Mind-body needs should consider the following variables:
- Physical Labor Needs: Adapt labor and birth positions based on the patient’s specific orthopaedic injuries or aches and pains that can prevent focus or certain positioning during birth. This could include but is not limited to problems like hip impingment, shoulder impingement, sacroiliac joint pain, back pain, limitations in ROM, or existing pelvic pain.
- Psychoemotional/Physical Labor Needs: Consider previous birth trauma or history such as prior C-section, episiotomy, or difficulty with pain management or dilation that may affect labor progression.
- Psychoemotional/Energetic/Spiritual Labor Needs: Establish adequate birth support during labor. A 2012 Cochrane review of RCT’s found that women with continuous support were more likely to have a spontaneous vaginal birth, less likely to have pain medications, epidurals, negative feelings about childbirth, vacuum or forceps-assisted birth, and C-sections. Women with support also had shorter labors by 40 minutes, higher APGAR scores, and the best overall outcomes. Constant support means a mother has someone continuously at her side during the entirety of labor. That person must also be an active, knowledgeable participant in the labor process, not just a warm body taking up space.
- Intellectual Labor Needs: Educate the mother and her birth partner about how to execute the personal birth plan, which can include yogic breathing, a bevy of yoga posture options for individualized labor and birth positions, guided imagery and/or motor imagery techniques, and hands-on manual therapy techniques.
- Psychoemotional/Energetic Labor Needs: Address any previous birth or sexual trauma which could create anxiety and fear. Anxiety and fear of childbirth can prolong labor more than 90 minutes (Adams et al 2012).
Yoga is an amazing, proven method to directly diminish perceived pain during labor, immediate postpartum pain, and shorten labor duration, as well as improve maternal comfort and birth outcome scores, as found in a 2008 randomized trial of 78 pregnant Thai women.
Ginger’s course, Yoga as Medicine for Labor, Delivery, and Postpartum prepares the physical therapist to meet the needs of the laboring mother with an evidence-based mind-body holistic perspective, which includes designing individualized birth plans for labor and delivery. Future posts will also address the postpartum curriculum included in the course. To learn more about Ginger’s course, visit Yoga as Medicine for Labor, Delivery, and Postpartum.
Last week in our blog, you learned about Susannah Britnell, a physiotherapist who works in a multidisciplinary pelvic pain treatment setting. I learned of her clinic when I came across this journal article) about developing an interdisciplinary clinic for patients with endometriosis and pelvic pain. Below is Part 2 of the questions that she was kind enough to answer for us so that we can hear more from her perspective!

What do you find rewarding as a therapist in working in this setting?
Working with people in pain can be challenging but also extremely rewarding. I really value being able to help women realize what they can do, how they can shape their current life experience and their future. We provide tools and strategies that they can put into practice successfully. I love being able to be a part of moments when there is a shift in thinking, an opening of opportunity, when women who have seen nothing but barriers and hopelessness realize that there could be the possibility of positive change. I really find satisfaction in helping women perform daily activities, manage bladder, bowel and sexual pain concerns and increase overall activity and participation in life.
What would you say is powerful for the patients in terms of having the team available?
Patients have a great sense of support being a part of this team. Gynecological, musculoskeletal and psychosocial components are addressed with a synergistic approach. Patients are searching for answers and once they receive a diagnosis, whether its endometriosis, pelvic girdle pain, sensitization or a combination, this does help them to move forward. More often than not, the diagnosis will be a combination of gynecological, musculoskeletal, and psychosocial components, with central sensitization. When they are aware that appropriate full medical management has taken place, a readiness for change and acceptance of the active role self- management can be fostered. Our patients learn self management tools in our workshop and then we support them as they practice these and integrate them into their lives.
Our team ensures that our language and message is consistent, supportive and empowering. We work hard to avoid any language that perpetuates confusion, fear or loss of hope and we clarify any misinformation or myths patients have encountered in the past. So many women have had negative past medical experiences and feel they have not been heard, or they have been told their pain is not real. This is obviously distressing for them, so to have a team that listens, supports and then helps to give strategies for change can be a big relief.
If a concern or question comes up during a session, we can usually address this with the appropriate team member before the patient leaves the clinic. This is important as it saves time for the patient and practitioner, but also helps to resolve those unanswered questions or worries that can lead to rumination and anxiety.
Our team has weekly meetings to communicate about treatment plans, discharge planning and for problem solving particular concerns. This is invaluable for communication and helps to give our team cohesion.
What do you sense are some barriers to others creating this type of environment?
Funding would be a big barrier. The reality is that these programs cost money to run. Many of these women have experienced pain and disability for years, which of course affects all facets of life, including being able to work. They often are unable to pay for private treatment and so without a publically funded program they go without. It is challenging to decide how best to use our limited resources so that we can try to meet the needs of so many patients.
Another barrier is that there are not enough physiotherapists and counsellors that have the experience or even the interest in working with women with chronic pelvic pain, so ongoing community support and follow-up in the patient’s communities can be difficult. We have a yearly Fellowship program for gynecologists who have an interest in this area. Part of our outreach plan is to help provide educational opportunities for physicians, physiotherapists and counsellors in BC.
A common perception from the medical side is that there is no hope for these patients and that nothing can be done for them. Isolated practitioners have a high burn out rate working in the area of chronic pelvic pain. However, with a supportive team, working in this area can be rewarding and exciting.
In an ideal world, are there some disciplines that you would love to see added to this group?
It would be fabulous to have a yoga Instructor and a dietician trained in biopsychosocial approach to chronic pain.
Are there any particular patient populations or conditions you love to work with or learn about?
I love working with women with chronic pelvic pain, in particular chronic pelvic girdle pain, dyspareunia, and bladder and bowel pain.
Thank you to Susannah for sharing her knowledge and experiences in our blog! If you would like to contact Susannah she can be reached via email at This email address is being protected from spambots. You need JavaScript enabled to view it., and her clinic website is www.womenspelvicpainendo.com. To discover more information about working with chronic female pelvic pain, you can attend one of our series courses such as Pelvic Floor Level 2B or our advanced course, Pelvic Floor Level 3. These courses always sell out, so sign up soon!
In patients with lumbar disc herniation, how many patients have sacroiliac joint dysfunction? Answering this question was the aim of a study published in the Journal of Back and Musculoskeletal Rehabilitation in 2013. From an outpatient clinic at a university hospital, 202 patients with lumbar disc herniation (paracentral or intraforaminal) on imaging and clinical findings suggesting lumbosacral nerve root irritation were included. Excluded were patients who pregnant, had prior lumbar surgery, osteoporosis, fractures, diabetes, severe hip DJD, and neurological deficits. Clinical examination tests for SIJ dysfunction included seated forward flexion test with palpation of the PSIS, Patrick-Faber test, long-sitting test, Gillet test, Sphinx test, and palpation tests for sacral base asymmetry. Pressure provocation tests were applied to the sacrum and the pelvic innominates, palpation to long dorsal sacral ligament and lumbosacral junction. "Positive" sacroiliac dysfunction diagnosis meant that the patient had a cluster of at least 4 anatomical and 2 provocative tests. Patients ranged in age from 19-70 years with a mean age of 42.
Greater than 72% of the patient sample with known lumbar disc herniation also presented with sacroiliac joint dysfunction. Females, patients with recurrent pain, those who performed heavy work, and patients with a positive straight leg raise test were more likely to have sacroiliac joint dysfunction. Of the 72% of patients who were diagnosed with SIJ dysfunction, nearly 60% were female. No correlation was found between the presence of sacroiliac joint disease, working hours, duration of low back pain, or body mass index and the rate of SIJ dysfunction. The authors conclude that sacroiliac joint dysfunction has a "…high possibility of occurrence in low back pain" and should be included in the clinical examination and decision-making process. They also point out that while the differential diagnosis of back versus SIJ pain is well-defined in manual medicine texts, the medical books do not highlight screening of the SIJ when presented with a patient who has back pain.
If you would like to learn skills to perform differential diagnosis of the sacroiliac joint, sign up for the Sacroiliac Joint Treatment continuing education course taking place this July in Baltimore with Peter Philip.
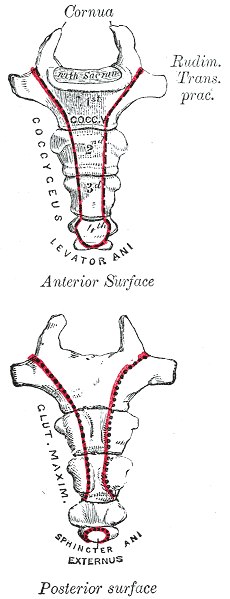
A recent publication of a case series proposes that clinicians use intranasal calcitonin, a medication prescribed for acute vertebral fractures in osteoporotic patients, for acute coccyx pain. This medication is administered as a nasal spray, has been demonstrated to have analgesic properties, and is theorized to have effects of beta-endorphin production, and inhibition of prostaglandin and cytokine production. Nasal calcitonin, a synthetic drug, is reported to have fewer and mild side effects when compared with the injectable form of the medication.
Of the 8 subjects treated and described in the case series, all had a fall on the tailbone, either landing hard into a chair on onto the stairs or floor. Some were seen within 3 months of injury date, and others were treated after 3 months from injury. The authors report that in the subjects who were treated acutely, 3 of 5 had at least 50% improvement in pain, without injections or surgery. The subjects treated in a chronic pain condition had similar levels of improvement but with the addition of coccyx injections for treatment.
Based on the lack of a control group, the small number of subjects treated, and because the mechanism of nasal calcitonin is unknown as far as effects on fracture healing in the coccyx, we would not, as rehab professionals, look to our referring providers to add nasal calcitonin routinely in the management of acute coccyx fracture. This article may, however, lead to interesting conversations with referring providers who are in a position to consider the addition of calcitonin for the proposed analgesic effect and potential bone healing augmentation. (The authors do suggest using the smallest effective dose for the shortest duration required.)
Clinically, is the difference in recovery for acute versus chronic coccyx pain of interest? Ideally, we would get to work with patients very soon after an injury, so that education is in place about self-care, self-treatment, optimal movement and thought patterns. The earlier that we can help a patient alleviate muscle tension and pain, and increase movement within tolerance, the better the outcomes usually are for the patient, as patterns of inactivity, fear, and muscle guarding are less likely to have set in. To learn much more about treatment of the coccyx, join faculty member Lila Abate in New Hampshire this September for the Coccyx Pain: Evaluation and Treatment continuing education course.
This post was written by H&W instructor Dawn Sandalcidi, PT, RCMT, BCB-PMD. Dawn's course that she wrote on "Pediatric Incontinence" will be presented in in South Caroline this August.

Years ago when my oldest daughter was 4 years old and in Pre-school I received an urgent call at the office that she had an accident. Immediately my head began to race, “What hospital is she in?” “What did she break?” Then the director informed me she wet her pants. I collapsed in my chair with a huge sense of relief and I began to ponder “Did she have an ‘accident’ or did her bladder leak?
Merriam-Webster defines an accident as:
- 1. An unforeseen and unplanned event or circumstance
- 2.An unexpected and medically important bodily event especially when injurious
- 3.Used euphemistically to refer to an involuntary act or instance of urination or defecation
Now lets think about that. How would you feel if someone approached you after noticing a smell or a wet spot and asked you “Did you have an accident?” My first thoughts are maybe shame, embarrassment, guilt or failure. “I” had an accident. Children feel without easily being able to express these emotions thus internalizing their feelings. This then can be expressed with inappropriate behaviors.
When I work with children, and adults for that matter, I frame the conversion with the physiology of the anatomical structure that is unable to do the job it is designed to do. I teach the children about their anatomy and bladder/bowel function and I am clear to let them know that their bladder and/or bowel had a leak, they did not. It takes ownership away from the person and places it on the body part that is currently dysfunctional. At that point we discuss we can re-train the body part to do the job they were designed to do. The kids become empowered that they will be able to become “The Bladder/Bowel Boss”.
To learn more about Dawn's course visit Pediatric Incontinence
Earlier this year, when I came across this journal article about developing an interdisciplinary clinic for patients with endometriosis and pelvic pain, I was pleased to see that rehabilitation is included in this team setting. Upon reaching out to Susannah Britnell, physiotherapist, she agreed to answer some questions about her clinic and about her passion for pelvic rehab. Below you can read her responses to my questions. Stay tuned for Part 2 that will be published next week!

How long have you been working in the interdisciplinary clinic?
I’ve been working at the BC Women’s Centre for Pelvic Pain and Endometriosis in Vancouver, BC, since October 2012. We are a provincially funded program for women with chronic pelvic pain from all over the province of BC, Canada.
How long have you practiced?
I have been practicing since 1997 and love it! It is amazing how our practice can grow and move into different areas. We are truly lucky we have these opportunities.
What other settings have you worked in?
I have worked in hospital and private practice settings. I found my grounding in musculoskeletal physiotherapy, obtained my manual and manipulative therapy diploma in 2001, and worked in obstetrics for 10 years at BC Women’s hospital. I then started incorporating pelvic floor physiotherapy into my practice and developed a strong interest in chronic pain and the biopsychosocial approach to pain management. In addition to clinical practice, I teach the obstetrics component at UBC School of Rehabilitation as an annual guest lecturer and am an instructor for physiotherapy Rost Therapy courses for pelvic girdle pain, which I often co-instruct with Cecile Röst, a Dutch Physiotherapist.
How did you get involved with the interdisciplinary group?
Were you involved in the development of the center?
Our gynecologists, Dr Allaire and Dr Williams have been working at the Women’s Hospital and Health Centre for many years and identified the need for an interdisciplinary program for women with pelvic pain. After getting the funding in place, they hired a counsellor, physiotherapist, and nurse to be a part of the team. We now also have another gynaecologist, Dr Yong, as well as a Fellow. The gynecologists, counsellor, nurse, and myself along with administrative program manager worked together to develop the program. We have also had input from a Pain Specialist/anesthesiologist. I am so grateful and thankful to be a part of such a supportive and skilled team. As a physiotherapist, it truly is wonderful to have such support from the physicians
Our program consists of a full day workshop which includes pain education, life style changes, mindfulness based stress reduction and meditation techniques. We address fear of movement and give strategies for pacing and grading activity and we also include stretches, posture, and positioning advice. Women then book individual physiotherapy and counselling appointments so we can work on more specific concerns. Physiotherapy treatment may include some passive treatment techniques, but only as a bridge to more active self management. Patients will always have an active plan from the first visit. It is important that we don’t reinforce a sense that the woman needs someone to “fix” her concern and that she has no ability or power to make changes with her pain.
Our nurse is in contact with the patients from the beginning and is available if they have any questions as they go through the process. To learn more about the program, you can go to www.womenspelvicpainendo.com or contact Susannah at This email address is being protected from spambots. You need JavaScript enabled to view it..
To discover more information about working with chronic female pelvic pain, you can attend one of our series courses such as Pelvic Floor Level 2B, or our advanced course, Pelvic Floor Level 3
This blog was written by Carolyn McManus, PT, MS, MA, who will be presenting at the APTA's Virtual NEXT conference in North Carolina. Carolyn is instructing a new course with Mindfulness-Based Biopsychosocial Approach to Chronic Pain. This course will be offered November 15-16, 2014 in Seattle, WA.

We all know a highly stressed patient will have a more complicated and prolonged healing process than a non-stressed patient. Recent research is finally illuminating possible mechanisms causing the amplification of pain by stress. For example, stress has been shown to enhance muscle nociceptor activity in rats. (1) In this study, water avoidance stress produced mechanical hyperalgesia in skeletal muscle and a significant decrease in the mechanical threshold of muscle nocicpetors, a nearly two fold increase in the number of action potentials produced by a fixed intensity stimulus and an increase in conduction velocity from 1.25 m/s to 2.09 m/s! Researchers suggest these effects are due, at least in part, to catecholamines and glucocorticoids acting on adrenergic and glucocorticoid receptors on sensory neurons.
I always talk about this study with my patients who have persistent pain. It helps them understand that pain can escalate, not because of tissue damage, but because of the effects of stress hormones on their nerves. They understand that if they persist in escalating their stress reaction they will limit their healing potential. There is more research on this topic and strategies to help patients self-regulate their stress reaction that I look forward to discussing in my upcoming course in November.
Learn more about Carolyn's course Mindfulness-Based Biopsychosocial Approach to Chronic Pain
In Turkey, the rate of daytime urinary incontinence (DUI) was studied in primary school-aged children. A questionnaire was completed by parents of 2164 students. The Dysfunctional Voiding and Incontinence Symptoms Score Questionnaire was utilized and includes 14 questions about daytime and nighttime symptoms, voiding and bowel habits, and quality of life.
The population studied included approximately half boys and girls, with nearly half living in rural versus urban settings, and of a mean age of 10 years old. The overall prevalence of DUI was 8% (8.8% in girls, 7.3% in boys), and decreased with increasing age in this study population of children in 1st through 8th grades. 57.8% of those who did experience involuntary loss of urine were wetting less than 1x/day, 26.6% were wetting 1-2 times/day, and 15.6% were wetting greater than 2x/day. Urge incontinence was reported in nearly 59% of the children with DUI.
Independent risk factors for DUI included age, maternal educational level, family history of daytime wetting, urban versus rural setting, history of constipation or urinary tract infection (UTI), and urinary urgency. The authors conclude that "…educational programs and larger school-based screening should be carried out, especially in regions with low socioeconomic status." In this study, one of the strategies used to increase the survey response rate was to send medical and public health residents to the schools to speak about the study on 2 occasions.
Despite the numbers of therapists who have previously trained with educators such as faculty member Dawn Sandalcidi in her coursework for pediatric bowel and bladder function, the number of therapists focusing on pediatric pelvic health remains small while the need is great. Therapists who wish to expand community reach to pediatric urologists and pediatricians, and to serve the children who may unfortunately become adults who have bowel and bladder dysfunction, have the opportunity to attend the Pediatric Incontinence and Pelvic Floor Dysfunction continuing education course in Greenville, South Carolina this August.
In women with pelvic pain, is a pudendal nerve block effective, and how does the effectiveness correlate with findings of the history and clinical exam? These were the questions posed by a study published in 2012. Sixty-six patients were given a standardized pudendal nerve block, with Visual Analog Scores (VAS) and presence of numbness recorded prior to and up to 64 hours after the block. Inclusion criteria for the study involved having spontaneous or provoked pain in the distribution of the pudendal nerve, and patients were excluded if significant psychosocial issues, neurogenic or neuromuscular disorders, contraindication to sedation or allergy to utilized medication was present. A detailed history and physical examination was completed.
The pudendal nerve block was administered transvaginally and digitally, under sedation, in a lithotomy position. Following data collection, the researchers found that the presence of a positive Tinel's sign (palpation medial to the ischial spine for assessment of pain reproduction), a prior history of vulvovaginal candidiasis, or symptom worsening in the sitting position was associated with a return of the pain prior to the numbness wearing off. 92.4% of the subjects reported a "positive" response to the block, with varied lengths of time of symptom reduction. Nearly 87% of the subjects reported a reduction in one or more symptoms. This study only studied subjects for 64 hours, therefore it is not possible to discuss from this research the long-term implications of a pudendal nerve block in women with pudendal neuralgia. The authors did find a correlation between prior traumatic events including birth injuries, herniated discs, and fractures of the coccyx, pelvis or sacrum.
What does this research tell us about the role of pudendal blocks in the assessment and treatment of female pelvic pain? As already mentioned, the brevity of the data collection (only up to 64 hours) in addition to application of a non-guided block limit the ability to extrapolate this information to any long-term results. However, the correlations to clinical history and the return to pain prior to numbness ending may provide useful information as further clinical research is completed. The numbness was found to have inconsistent effects on a patient's symptoms such as bladder, bowel, sexual dysfunction, or sitting, and further research could measure the effects of a block on these functions. If you would like to discuss pudendal blocks with experts on pudendal dysfunction, sign up for the remaining spots in our August San Diego course!
Learn more about the Pudendal Neuralgia Assessment and Treatment course that we are holding at Comprehensive Therapy Services later this year.
This post was written by H&W instructor Dawn Sandalcidi, PT, RCMT, BCB-PMD. Dawn's course that she wrote on "Pediatric Incontinence" will be presented in in South Caroline this August.

I will never forget the morning I was called by one of my referring pediatricians to tell me an 11-year-old boy with fecal incontinence hung himself because his siblings ridiculed him. If you ever ask me why I do what I do, I will tell you so that nothing like that would ever happen again.
When we think of pediatric bowel and bladder issues we primarily focus on the physiologic issue itself and treating the underlying pathology. I think it is imperative to teach a child that she/he did not have a leak but their bladder or bowel had a leak. It makes the incident a physiological problem and not a problem of the child.
It is not always apparent how much the child is suffering from issues with self-esteem, embarrassment, internalizing behaviors, externalizing behaviors or oppositional defiant disorders. Dr. Hinman recognized theses issues years ago (1986) and commented that voiding dysfunctions might cause psychological disturbances rather than the reverse being true. Dr. Rushton in 1995 wrote that although a high number of children with enuresis are maladjusted and exhibit measurable behavioral symptoms, only a small percentage have significant underlying psychopathology. In more recent studies by Sureshkumar, 2009; Joinson 2007 it was noted that elevated psychological test scores returned to normal after the urologic problem was cured. Lettgen et al. 2002, Kuhn et al, 2008, van Gontard, 2012 all reported that children with urge incontinence are distressed by their symptoms but the family functioning is intact.
I frequently get testimonials from my patients. I would say the common denominator is the child and/or parental report that the child is “much better adjusted,” “happier”, “come out of his shell”, “more outgoing”, “making friends.” As a side note -- they’re happy they don’t leak anymore.
The International Children’s Continence Society (i-c-c-s.org) is filled with standardization documents that support the work we do to take care of kids with elimination issues. The work we do to take care of these kiddos in not only necessary but also mandatory to avoid these psychological disorders.
To learn more about Dawn's course visit Pediatric Incontinence
Read more about what Dawn does in PT in Motion
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./











































