For the past 20 of my 49 years as a physical therapist, I have been focusing on osteoporosis management thanks to the intervention of Sara Meeks who began studying osteoporosis in the 1980s before it was even a “thing.” The WHO did not identify osteoporosis as a systemic disease until 1993! About 15 years ago, after attending all of Sara’s Osteoporosis seminars, she selected my current business partner, Frank Ciuba, and I to “carry the torch.” Since then, we have been teaching her course with updated evidence, additions, and new research as it becomes available.
According to the Bone Health and Osteoporosis Foundation, 50% of individuals over age 50 are diagnosed with low bone density (osteopenia or osteoporosis) and many assume the only therapy option is medication.
Not so fast!
While some individuals may need bisphosphonates or anabolic drugs to get control of their rapidly decreasing bone strength, everyone can benefit from exercise. And research is showing that exercise can slow bone density loss and even help increase it. But it must be the right exercise, performed correctly and consistently.
Even though strength training consisting of high-intensity resistance and impact training (HiRIT) has been shown to build bone, it is not traditionally recommended for individuals with osteoporosis because of the perceived high risk of fracture.
Today I want to talk about the LIFTMOR Trial. LIFTMOR stands for Lifting Intervention For Training Muscle and Osteoporosis Rehab. This program, from Australia, utilizes brief, bone-targeted HiRIT with impact loading for post-menopausal women with low bone mass. It found that there was an increase in bone density compared to the more traditional low-intensity exercise program, and no adverse effects other than one report of minor lower back spasm. Additionally, functional measures such as TUG, 5 Times Sit-to-Stand, and Functional Reach improved.
As rehab practitioners, and especially PTs and OTs treating people with fragile bones, when it comes to exercise prescription, the question is often, “How much is too much?” As the ancient Greek physician, Hippocrates said, “Primum non nocere.” First, do no harm! So often we default to being gentle with our elderly, frail population in order to not harm them. Don’t get me wrong. I’m not saying we should have them all doing Burpees! One of the standout aspects of the LIFTMOR trial was lifting weights at 85% of 1 Rep Max compared to the Control group who worked at 65% of their 1 Rep Max. The report, according to the American Society for Bone and Mineral Research in 2017 reads: Contrary to current opinion, HiRIT was efficacious and induced no adverse events under highly supervised conditions for our sample of otherwise healthy postmenopausal women with low to very low bone mass.
“Highly supervised conditions.” I think that’s the key. We must make sure that our patients are educated and can demonstrate proper alignment and body mechanics. And of course, we must provide the correct exercises. And then increase the weights methodically with continued supervision to load the bones once our patients have the proper technique. Many patients (and therapists) want to know, does exercise really build bone density? Not to be coy, but my answer is often, “It depends.”
It depends on whether it’s the right exercises, performed with proper technique, and good compliance by the patient. Then yes, exercise does build bone density. One of our challenges though, is in trying to follow the evidence, is that “Exercise” means many different things to different people. Even the professionals! Teaching the wrong exercises can be unsuccessful at best and possibly catastrophic (causing a fracture) at worst!
That’s why Frank and I, with Sara’s blessing, created this program that is exercise-specific, based on solid evidence, and one that can be shifted into gear first thing on Monday morning.
Osteoporosis Management is scheduled for this spring and fall. Consider joining us in the remote course on April 27th or September 14th. We hope to see you soon!
AUTHOR BIO:
Deb Gulbrandson, PT, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
She can be reached at This email address is being protected from spambots. You need JavaScript enabled to view it.
“Is anyone else feeling super burnt out from complex patients right now? I’ve been in pelvic health for 20 years and used to see a lot of easy urinary incontinence patients who all got better fairly quickly. Now all I have is pudendal neuralgia, pelvic pain, and bowel dysfunction. I can’t remember the last SUI patient I had!!”
This week I was tagged in a social media post, that started with the above inquiry…and quickly filled up with thirty-six replies from therapists all over the US, with comments like:
- “The burnout is real.”
- “Mental health issues of today are complicating our patients’ presentations.”
- “Some days I wish for a straightforward TKA.”
- “It’s mentally exhausting.”
- “The simple solutions are rare.”
- “There is so much going on in our world, toxin exposure, stress, work expectations, loneliness, less access to nature and healthy food, less access to being outside…our health is suffering.”
- “The better our skills, the more complex our patients become.”
The last is a favorite. You, dear therapist, INVEST and WORK HARD to EQUIP yourself to serve a population of patients that is ever-increasing in complexity.
You are taking clin ed, watching social media posts, reading books and articles to keep up.
BUT have you thought of equipping yourself to better serve…YOURSELF?
How many of us…
- Give so much, day in and day out, feeling like we are left with only crumbs for ourselves and our loved ones?
- Feel frustrated by patients who seem to have very little buy-in to their own health management?
- Are never able to complete paperwork within a patient session?
- Feel energetically dumped on and drained by some patients?
As rehab professionals, we were taught SO MANY SKILLS to take a good history, perform a thorough evaluation, and apply meaningful treatments. But most of us were never taught how to:
- Have healthy boundaries in patient care
- Protect our own physical and energetic bodies from becoming over-taxed
- Skillfully manage time to make sure we can complete tasks like paperwork
- Involve patients in a SHARED RESPONSIBILITY model of care
- Impact our patients' NERVOUS SYSTEMS in a meaningful way to enable the healing process to occur
If you can relate to this post, please consider joining us for Boundaries, Self-Care, and Meditation. A two-part course dedicated to supporting YOU in how you show up for your patients, your loved ones, and YOURSELF.
Born out of our combined experience of significant burnout, Nari and I are dedicated to equipping and empowering you to be the best, healthiest version of YOU as you work and as you live. Please join us and experience what others have said about this course:
- I loved the class; enlightening and freeing that I am not responsible for my patients' process - just a coach; also that I am actually robbing them of self-confidence when I do not give them responsibility for their own progress.
- This course is so needed for so many practitioners! Highly recommend to anyone and everyone!
Boundaries, Self-Care, and Meditation is being offered on these days:
- Boundaries, Self-Care, and Meditation - Part 1 April 20th and October 26th
- Boundaries, Self-Care, and Meditation - Part 2 May 19th and November 23rd
Hope to see you!
Jen and Nari
In 2022 The National Center for Transgender Equality (NCTE), a US trans rights organization, undertook an extensive survey of binary and non-binary transgender people in the USA and recently released preliminary results. This was an update to the 2015 U.S. Transgender Survey which had 28,000 participants from the transgender community. In 2022 the number of respondents tripled to over 90,000 people. It included people from every state and many US territories. Unlike the previous survey, which included only adults, the 2022 survey included 8,000 youth aged 16-17. Additionally, the number of available questions almost doubled to 624, allowing for more nuanced data collection.
The report details continued discrimination and mistreatment of people who are transgender. This includes experiencing poverty, unemployment, and job loss due to their gender identity and/or expression, mistreatment or bullying at school, and denial of restrooms that align with their gender identity.
Specific to healthcare, almost half of adult respondents reported at least one negative experience with a healthcare provider in the last year due to being transgender. This includes refusal of health care, using the wrong pronouns, and verbal and physical abuse during treatment. Nearly a quarter of people avoided seeking medical care when they needed it due to fear of mistreatment.
A key positive takeaway from the survey is that people have higher life satisfaction after gender transition. When combining those who were “a lot more satisfied” with those who were “a little more satisfied,” 94% reported increased life satisfaction when they lived at least some of the time with gender expression in line with their gender identity. Similarly, 98% of those getting hormone treatment and 97% of those who had at least one gender-affirming surgery reported increased life satisfaction.
The 2022 U.S. Transgender Survey highlights the need for further training for healthcare professionals and the significant positive impact gender-affirming healthcare has on the lives of people who are transgender. I’m proud of the rehab professionals I get to work with. In the seven-year interval of the survey a lot has changed in PT and OT involvement in transgender health. When I started working with people undergoing gender-affirming vaginoplasty (GAV). I could find nothing on pelvic therapy for GAV. There was not education aimed at rehab professionals and ways we could improve outcomes. Fast forward seven years, and now there are many rehab course offerings on many aspects of transgender health. Our original course included a broad overview of transgender care for the rehab professional. With all the offerings on care for people in the LGBTQIA2S community, the course is now focused deeply on gender-affirming genital surgeries, including of vulvo/vaginoplasty, metoidioplasty, and phalloplasty. Our gender affirming genital surgery course has more time devoted to multiple aspects of the recovery, rehabilitation, and improving outcomes of these surgeries. The full description is in this link: https://hermanwallace.com/continuing-education-courses/transgender-health-for-the-rehab-professional.
I enjoy teaching gender-affirming care and hope participants of our course, Transgender Health for the Rehab Professional, go on to help train their staff and team. Together we can help improve the health and lives of people who are transgender, join me in one of our upcoming courses scheduled for April 13th or August 17th.
If you enjoyed this article and are looking for other course recommendations I recommend the following:
- Intersex Patients: Rehab and Inclusive Care with instructor Molly O'Brien-Horn, PT, DPT, CLT scheduled for May 4th
- Inclusive Care for Gender and Sexual Minorities with instructor Brianna Durand, PT, DPT - scheduled for June 8th and December 7th
- Sexual Interviewing for Pelvic Health Therapists with instructor Mia Fine, PhD, LMFT-S, CST-S, CSE - dates to be announced
References:
James, S.E., Herman, J.L., Durso, L.E., & Heng-Lehtinen, R. (2024). Early Insights: A Report of the 2022 U.S. Transgender Survey. National Center for Transgender Equality, Washington, DC.
See publications from the course instructors:
Gallagher, S., Smigelski, C., Luikenaar, R., Dugi, D. (2022). Pelvic Physical Therapy for Gender-affirming Genital Vaginoplasty. In M. Van Trotsenburg, R. Luikenaar, R, & M. Meriggiola (Eds.), Context, Principles and Practice of TransGynecology: Managing Transgender Patients in ObGyn Practice. (pp 261-265). Cambridge: Cambridge University Press.
Jiang DD, Gallagher S, Burchill L, Berli J, Dugi D 3rd. Implementation of a Pelvic Floor Physical Therapy Program for Transgender Women Undergoing Gender-Affirming Vaginoplasty. Obstet Gynecol. 2019 May;133(5):1003-1011. doi: 10.1097/AOG.0000000000003236. PMID: 30969210.
Peters BR, Annen AA, Berli JU, Gallagher S, Smigelski C, Kahn LH, Skelton HE. Neurosensory Re-education following Gender-affirming Phalloplasty: A Novel Treatment Protocol. Plast Reconstr Surg Glob Open. 2022 Oct 24;10(10):e4616. doi: 10.1097/GOX.0000000000004616. PMID: 36299822; PMCID: PMC9592297.
Smigelski, C. (2023). [Review of the book Understanding Trans Health: Discourse, Power and Possibility, by R. Pearce]. Journal of Pelvic, Obstetric and Gynaecological Physiotherapy, Autumn 2023(133), 100-101.
Whitehead, D., Gallagher, S., & Condran, C (2023) Gender Affirmation Surgery. In West, A. M. (Ed.). The Transgender Athlete: A Guide for Sports Medicine Providers. (1st ed., p. 80). Elsevier. https://doi.org/eBook ISBN: 9780323916202
AUTHOR BIO:
Sandra Gallagher, PT, DPT, WCS
Sandi is a pelvic health physical therapist in Portland OR. Her practice includes providing evaluation and treatment of pelvic health conditions in adults and children of all gender identities. Dr. Gallagher received her primary physical therapy training in 1986 with a BS in Physical therapy from the University of Lowell in Massachusetts. She has pursued varied continuing education from manual therapy, Feldenkrais, biophysical agents, pelvic health, and pregnancy. She completed her Doctorate of Physical Therapy in June 2020.
Sandi has served on varied committees and boards at the state and national levels, most recently has the chair of the CAPP-OBC committee for the Academy of Pelvic Health of the APTA. She has presented on the role of PT in gender-affirming vaginoplasty at the UCSF Transgender Health Summit, the APTA Combined Sections Meeting, and at the 2018 international meeting of the World Professional Association for Transgender Health (WPATH). She is the recipient of the 2020 Elizabeth Noble Award from the Academy of Pelvic Health.
- You took Pelvic Function Level 1 and you left with more questions than answers when it comes to consent, vulnerability, chaperones, safety, and clinical decision-making about how to deal with tough client situations.
- Your state requires you to take an ethics class and you're looking for a new class that actually applies to your area of expertise. (The thought of taking another ethics class honestly makes you feel like you'll immediately fall asleep).
- You'd love to be in a conversation with a small group of like-minded professionals in pelvic health with varying levels of experience about common challenging ethical scenarios for pelvic health providers.
- You have a burning ethical concern that you would love help with and the ability to anonymously offer it up to a think tank of other pelvic health providers sounds like a dream. You feel icky about something and need to get it off your chest and find solutions.
- You're looking to learn about what ethics is, why it matters, and how to apply these concepts to your clinical practice, whether you're a newbie or veteran to the therapist life.
In all seriousness, Ethical Concerns for the Pelvic Health Professional is an ethics class created to fulfill your state requirements, answer your clinical practice questions on this topic, and help soothe any situations that may be causing you stress (maybe just a little, maybe a whole lot). Every time it runs, it's slightly different because although there is a structured curriculum, there is also a lot of dedicated time for applicable case study situations and group discussion of real concerns of the providers attending. Join Mora on April 20th in her next course!
PARTICIPANT TESTIMONIALS:
-
“Dr. Pluchino was an excellent teacher. She used a lot of practical examples and anecdotes from her own professional experience. She created very engaging environment and made us think about presented topics” - Klara Melli
- "This is the best ethics course I've ever taken! It was relevant to pelvic floor PTs and she kept us all engaged, offering many breaks. This material is typically quite dry, but Mora made it enjoyable and applicable." - Anonymous
- "I very much enjoyed this course. It was much more beneficial then when I took it in PT school as it was nice to apply life-case scenarios." - Anonymous
- "I really appreciated how responsive the instructor was to our questions and how willing she was to engage with our thoughts and questions. It felt very accepting and validating. The instructor was affirming and pleasant and she gave us good feedback. She also shared some of her personal experiences which allowed me to feel like I am not the only one who struggles with certain things and she offered helpful solutions." - Anonymous
AUTHOR BIO:

Mora Pluchino, PT, DPT, PRPC
I am a graduate from Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman & Wallace since 2020 and have over 150 hours of lab instruction experience.
B K S Iyengar describes pranayama as an “extension of breath and its control”1. Pranayama, or breathwork, includes inhalation, exhalation, and breath retention. As clinicians treating pelvic health, there are several clinical applications for breathwork.
Mechanical relationship to the pelvic floor
Physical therapists Paul Hodges (et al) and Julie Wiebe describe a piston-like relationship between the diaphragm and pelvic floor2,3. Applying mindfulness to breathing can enhance this relationship, especially if muscular holding patterns in the pelvis are secondary to pain.
On inhalation, the diaphragm moves caudally and the pelvic floor muscles respond to this change in pressure, also lengthening caudally. On exhalation, the diaphragm and pelvic floor muscles reverse direction and ascend cranially4. As clinicians, we can offer patients the tool of using the breath in coordination with the pelvic floor muscles.
We can tailor breath awareness to our clinical goals of downtraining or facilitating the pelvic floor muscles. Cuing to downtrain gripping patterns in the pelvic floor can be supportive for people experiencing pelvic pain. Facilitating the pelvic floor in coordination with the breath can help obtain optimal stability and continence.
Pelvic organ prolapse, stress urinary incontinence, and fecal incontinence are often associated with a lack of tonic support/muscular strength and coordination of the pelvic floor, core, and surrounding pelvic girdle musculature5. Optimizing pelvic floor support with adequate strength, core stability, and neuromuscular control can help improve continence and pelvic organ support.
The local core stabilizers (pelvic floor muscles, transverse abdominals, multifidi, and diaphragm) coordinate to provide optimal core stability6. Mary Massery conceptualized the “Soda Pop Can Model of Postural Control”. This illustrates how the pressure system of an aluminum soda will maintain the stability of the structure7. Non-optimal control of pressure can happen at the top of the canister (i.e. tracheotomy), front (i.e. diastasis recti abdominus), back (i.e. disc herniation), or bottom (i.e. pelvic organ prolapse or incontinence). A “leak” in the structural integrity could affect postural control, core stability, and continence. This concept underlines the importance of breath retraining as one aspect of our treatment plan.
Nervous system relationship to pelvic pain
Breathwork offers your patient an instant strategy to offset a rise in sympathetic nervous system activity, which happens when someone experiences pain. Creating a mindful pause can encourage a shift in the autonomic nervous system by invoking a parasympathetic response.
Diane Lee highlights some common areas of holding patterns in the body, including lateral and posterior-lateral expansion of the rib cage during inhalation8. By paying attention to our breathing we can increase range of motion in the thorax, especially for folks who wear sports bras or bind. We can practice exploring diaphragmatic breathing without gripping the chest and abdominal wall.
Example of pranayama
Dirgha
Dirgha is also called the Three-Part Breath.
- Inhale and allow the belly to fill. If this feels this challenging, you could place a book on your belly laying supine or try breathing in quadruped.
- Continue the breath up into the ribcage and feel the lateral and posterior lateral aspect of the ribs opening.
- Third aspect is allowing the collarbones to float up, unless you are trying to retrain dominant apical breathing
- After trying this for 10 breath cycles, stop and notice sensations in the body. It can be helpful to set an alarm during the day as a reminder to pause, move, and breathe.
Integrating into the clinic
Breathwork can be performed supine, sitting with hands for feedback on the abdomen and chest, or integrating with movement. These examples are only the beginning of possibilities!
To learn more, join Dustienne in her remote course Yoga for Pelvic Pain this year! Courses are scheduled for March 16-17, May 4-5, and September 14-15.
References:
1) Iyengar BKS. Light on Yoga: Yoga Dipika. Schocken; 1995.
2) Sapsford RR, Richardson CA, Maher CF, Hodges PW. Pelvic floor muscle activity in different sitting postures in continent and incontinent women. Arch Phys Med Rehabil. 2008;89(9):1741-1747.15.
3) Julie Wiebe, Physical Therapist | Educator, Advocate, Clinician. 2015; http://www.juliewiebept.com/.
4) Talasz H, Kremser C, Kofler M, Kalchschmid E, Lechleitner M, Rudisch A. Phase-locked parallel movement of diaphragm and pelvic floor during breathing and coughing-a dynamic MRI investigation in healthy females. Int Urogynecol J. 2011;22(1):61-68.
5) Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther. 2004;9(1):3-12.
6) Lee DG. The Pelvic Girdle: An integration of clinical expertise and research, 4e. Churchill Livingstone; 2010.
7) Massery M. THE LINDA CRANE MEMORIAL LECTURE: The Patient Puzzle: Piecing it Together. Cardiopulm Phys Ther J. 2009;20(2):19-27.
8) Lee DG. The Pelvic Girdle: An integration of clinical expertise and research, 4e. Churchill Livingstone; 2010.
AUTHOR BIO:
Dustienne Miller, MSPT, WCS, CYTDustienne Miller is the creator of the two-day course Yoga for Pelvic Pain and an instructor for PF1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga videos series called Your Pace Yoga in 2011. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Continence Society, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
She started her clinical practice, Flourish Physical Therapy, in Santa Rosa CA, and moved to downtown Boston. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga postures and breathing into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health.
Dustienne's love of movement is apparent not only in her physical therapy and yoga practice but also in her career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for Radio City Christmas Spectacular. She is currently an assistant professor of jazz dance for the musical theatre department at Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life. Find her on SM @yourpaceyoga and on her website, www.yourpaceyoga.com, where you will find her blog, guided meditations, videos, and additional resources.

Erica Vitek, MOT, OTR, BCB-PMD, PRPC has attended extensive post-graduate rehabilitation education in the area of Parkinson disease and exercise. She is certified in LSVT (Lee Silverman Voice Treatment) BIG and is a trained PWR! (Parkinson Wellness Recovery) provider, both focusing on intensive, amplitude, and neuroplasticity-based exercise programs for people with Parkinson disease. You can learn more about this topic in Erica's remote course, Parkinson Disease and Pelvic Rehabilitation scheduled for April 19-20, 2024.
Parkinson disease (PD) is the second most common neurodegenerative disorder. It is typically characterized by its cardinal motor symptoms of resting tremor, bradykinesia, and rigidity. A myriad of non-motor symptoms accompanies the motor symptoms with constipation being one of the most frequent, affecting nearly 80% of people with PD. Constipation has been labeled a prodromal symptom appearing, in some, up to 20 years pre-diagnosis. It is theorized that there are two neuropathological subtypes of PD, “brain first" and “body first." The "brain first" subtype is characterized by central nervous system degeneration in the area of the brain that produces dopamine which results in characteristic cardinal motor system dysfunction. In the “body first” subtype, the peripheral autonomic nervous system and enteric nervous system are said to be affected by the neurodegeneration which then spreads to the brain via the vagus nerve.
Many studies have linked greater non-motor symptom severity with the presence of constipation and irritable bowel syndrome (Tai, Y.C., et al., 2023; Yu Q.J., et al. 2018). The authors report that people with PD and Irritable bowel syndrome (IBS) have greater non-motor symptom severity than those without IBS; the severity of IBS positively correlated with non-motor symptom severity especially mood disorders and the severity of constipation correlated with the severity of motor dysfunction. In another recent study by Al-Wardat et al. 2024, the authors explored a link between constipation and pain experienced in people with PD. The prevalence of people with PD experiencing pain is 40-88%. The neuropathological mechanism is complex and multifactorial however altered pain processing due to abnormalities in neurotransmitters related to PD may impair endogenous pain modulation. Additionally, people with PD, during dopamine replacement therapy off-times, have been shown to have increased spinal nociceptive activity and decreased ascending inhibition lowering their pain thresholds. This demonstrates how neurodegeneration in the brain and enteric nervous system, which may be enhanced by constipation, contributes to non-motor symptom severity.
There appears to be a cascade of potential contributors to the relationship between constipation and pain in people with PD. First, physical inactivity, commonly seen as PD progresses, can lead to exacerbated constipation, increased muscular rigidity, and increased musculoskeletal pain sensitivity. Second, when constipated, the person with PD will have reduced dopamine replacement medication absorption which occurs in the small intestine leading to worse motor function and pain sensations. Third, opioid analgesics can contribute to slow colonic motility when they bind to receptors in the enteric nervous system consequently causing inhibition of the motor and secretory neurons. Fourth, gut microbiome dysbiosis, resulting from constipation, is hypothesized to cause maladaptive pain processing and alter the brain’s endogenous pain modulatory abilities.
Looking at the gut microbial dysbiosis further, there are three potential drivers that these alternations may be affecting the neuroplasticity of the pain processing pathways. Dysbiosis induces an immune repose, releasing proinflammatory factors which then heighten the sensory neurons of the dorsal root ganglion and dorsal horn. The gut microbiome's proper function is necessary for the gut’s serotonin production, which is one of our neurotransmitters involved in pain modulation (as well as mood and cognition). Finally, serotonin is involved in the local regulation of the movements in the gut therefore depletion will further alter motility.
Clinically, during our assessments, asking our patients with PD about any pain experiences they might have should be included. Because of this identified link between constipation, higher risk of pain, and other non-motor symptom probability, we can develop a treatment plan that will help to improve or restore motility, improve absorption of dopamine replacement medication, gut microbiome functionality, and potential reduction in pain medications with reduced sensitivity of pain. Our knowledge of behavioral and lifestyle modifications related to fiber, fluid, routine increases in physical activity, and strategies for the management of anxiety and depression can be great first steps to improving the daily lives of people with PD.
We have the tools as pelvic health clinicians to play a role in helping people with PD improve their quality of life. Knowing that improving constipation could positively affect non-motor symptom likelihood and severity and potentially slow the neurogenerative process is hope that we can offer. Let’s get together in April and explore the unique issues people with PD experience from the esophagus to the pelvic floor which will help shape your strategies for these patients in the clinic.
References:
- Al-Wardat, M., Grillo, P., Schirinzi, T., Pavese, C., Salimei, C., Pisani, A., & Natoli, S. (2024). Constipation and pain in Parkinson’s disease: a clinical analysis. Journal of Neural Transmission, 131(2), 165-172.
- Tai, Y. C., Liao, P. H., Leta, V., Lin, C. H., & Chaudhuri, K. R. (2023). Irritable bowel syndrome based on Rome IV diagnostic criteria associates with non-motor symptoms of Parkinson's disease. Parkinsonism & Related Disorders, 105496.
- Yu, Q. J., Yu, S. Y., Zuo, L. J., Lian, T. H., Hu, Y., Wang, R. D., ... & Zhang, W. (2018). Parkinson disease with constipation: clinical features and relevant factors. Scientific reports, 8(1), 567.

Note: If you missed my last post, read about the three diaphragm (voice-to-pelvic floor) approach here: https://hermanwallace.com/blog/the-voice-of-pelvic-healthbuilding-a-3d-treatment-toolbox
How well can you speak when you are nervous? How well can a person sing if they are crying? What happens to the pelvic floor if someone is nervous or crying, or both? It doesn’t take too much investigation to realize that the health of our voice and pelvic floor are intimately intertwined – and tied to – our stress response.
We know the way we respond to stress impacts our performance. So, when we ask what makes someone a pelvic floor athlete – the answer is – anything that person does that impacts their stress response. If the voice is intimately tied to the stress response as well, then the sport of voicing, or singing, qualifies as an athletic event for the pelvic floor. Thankfully, we have a long string of evidence-base to support the impact of breathing on the pelvic floor, but what about voicing?
The concept of using a three-diaphragm model in rehabilitation was introduced in Medical Therapeutic Yoga (2016) based on the original five-diaphragm theory suggested by Bordoni and Zanier in 2015.1 Since that time, the science of how the voice and the use of music impact rehabilitation outcomes, has continued to evolve.
How music and sound enable learning and impact the mind-body complex is a long-pursued scientific question for every season of the human lifespan, from early childhood development to the golden years of senior living. With regards to motor rehabilitation, the last 25 years of research has supported the notion that musical rhythm entrains movement in patients with neurological disorders.2 In people with acute and persistent pain, results from a meta-analysis of 97 trials suggest that “music interventions overall have beneficial effects on pain intensity, emotional distress from pain, use of anesthetic, opioid and non-opioid agents, heart rate, systolic and diastolic blood pressure, and respiration rate.”3
Across healthy populations, music has been shown to impact several biomarkers. In a systematic review of 44 studies, half measured the stress hormone cortisol and of those, 100% demonstrated a stress modulation effect of listening to music, chiefly through reduction of cortisol.4 Blood glucose levels also improved in response to music listening in the same analysis.
The human voice, however, is the original instrument, which means listening to the quality of it offers two tools: therapeutic and diagnostic. In other words, the phrase “Are you listening to your patients (and yourself)?” becomes more than just a superficial question about hearing someone. Listening to the voice becomes another way of evaluating the pelvic floor.
Are You Really Listening to Your Patient’s (and Your) Voice?
Listening to someone’s voice can offer you instant and intimate insight into the overall health of the person. The anatomical and neurophysiological connections of the voice-to-pelvic floor are well defined, while investigation into the detailed functioning between the voice and pelvic floor is emerging. In a small study of 11 participants, counting (inclusion of glottal function) improved balance in postpartum women versus not including the laryngeal diaphragm.5 In another small study of opera singers, transperineal ultrasound imaging was used to confirm that the professional vocalists did indeed recruit the pelvic floor during singing.6 And in a third small study, 10 untrained subjects (half men, half women) were asked to do various pelvic floor and vocal tasks with pelvic floor responsiveness noted via transabdominal ultrasound imaging, which showed variable results for lengthening and contraction of the pelvic floor during voicing.7 These early studies are a vital guide for future research and understanding of two variables: the role of pelvic floor therapy in vocal performance and the role of the voice in pelvic floor therapy.
What Can Be Learned from Listening to the Quality of the Voice?
First, let’s start with the top diaphragm – the laryngeal diaphragm. The proverbial apple does not fall from the tree, in that vocal habits are often a mirror of the health of nearby structures, such as the jaw and neck.
Clinicians should screen their patients, asking questions like - Does the person clinch the jaw or grind their teeth at night? Do they have existing jaw pain, clicking, headaches, and/or neck pain? Do they get frequent laryngitis or have a chronic throat clear or hoarseness? Do they have acid reflux or postnasal drip? Any of these variables can lead to a degradation of the voice and can easily cause vocal fatigue and/or injury.
Next, if the clinician determines these things exist – a sequela of issues can follow, typically starting with evaluating breath support. If any of the above issues are present, a person typically must drive their voice harder to create sound, which means the demands on the respiratory system increase. Secondary muscles of respiration, typically reserved only for forced expiration, now come into play. Muscles like the abdominal wall, specifically the internal obliques, but also the cervical paraspinals, sternocleidomastoid, scalenes, intercostals, and even the psoas and iliacus, can be recruited during speaking. To help in patient and public health education, I coined and use the phrases “Psoas Speaking, Oblique Speak, and/or Paraspinal Speaking” to make it easier for people without healthcare backgrounds to understand what is happening when they drive their voice too hard to create sound. Clinicians may also be surprised to know just how hard the body will work to create sound, even when it creates a downward pressure gradient in the pelvic floor, as happens in many cases where vocal dysfunction is present.
But let’s return to why the person is using forced expiration, which is the strategy most often employed when it becomes increasingly difficult to create sound.
What Do We Know about Forced Expiration?
We know that it’s employed typically during a sympathetic nervous system response. That is – forced expiration is a result of the stress response – where if we don’t choose “rest and digest” we are left with fight, flight, freeze, or fawn. Getting our needs met (as outlined in Maslow’s hierarchy of needs - see figure below) as human beings simply cannot happen if we are stuck in a sympathetic nervous system response. Whether or not the person is conscious of it, as Bessel Van der Kolk’s book of the same name tells us, the body keeps the score. Our body will perceive a stress or pain response if we are forcing the laryngeal diaphragm to create sound under chronically bad conditions. But the tricky part, beyond recognizing what vocalizing under bad conditions looks and sounds like is this – the stress response will happen even when the person doesn’t perceive stress or pain. So, it becomes the clinician’s job to help the individual recognize signs of vocal distress and to determine if they can help as a pelvic health practitioner, or whether or not a referral to an ENT, SLP, or another provider may be necessary.
To determine if we can help – we first must recognize the voice as an integral part of pelvic health assessment and intervention.
In a trauma-informed model, the three-diaphragm approach asks the therapist to attune to a person’s basic needs first. We cannot expect to solve their pelvic floor or pelvic girdle problems if we haven’t taken note of the stressors in their life – this means being aware of and screening for social determinants of health, such as whether or not they have a safe space at home, access to sunlight and green space, transportation to and from therapy, and/or whether or not they live in a food desert.
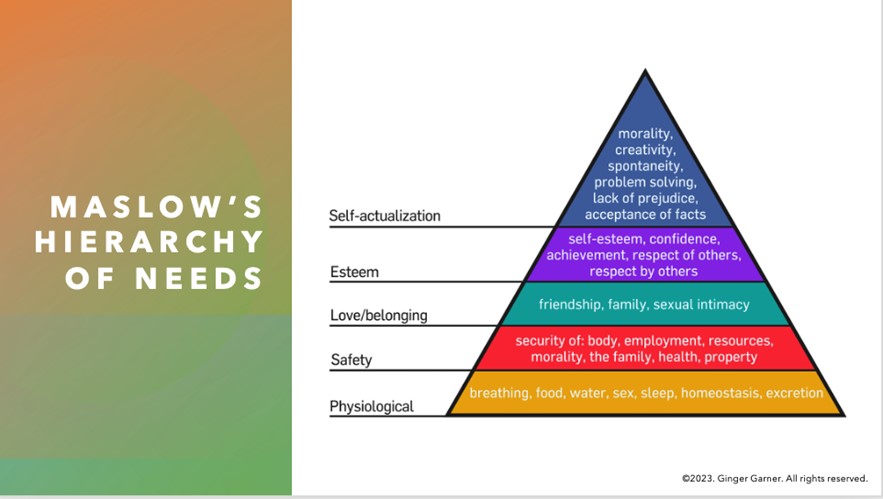
I often use the example of not attuning to the social determinants of health in our patients being akin to not addressing sensorimotor issues in someone with autism spectrum disorder. It’s hard to sit still and learn the math that your teacher wants you to learn if the tag in your sweater feels like a hot match on fire. Right? In the same way, it’s difficult for our patients to resolve their voice, breathing, and/or pelvic floor issues if we are not making sure they feel safe and sound in the therapy environment first. Once we have done that, we can then move to identifying whether or not they would benefit from voice-to-pelvic floor therapy.
The short answer is everyone can benefit from an enhanced model of pelvic floor evaluation that includes voice assessment, or the three-diaphragm model. However, if your patient has an anatomically narrow airway or any of the following issues, a referral could be necessary:
- Asthma
- COPD
- Allergies or Pollutants - environmental, food
- Sleep Apnea or poor sleep quality
- Breathing Anomalies - long COVID, or poor breathing in general that cannot be addressed in pelvic PT/OT
- Reactive airway to exercise - exercise-induced asthma
Our Voice is Our Life
Finally, our goal of Three Diaphragm Therapy is to have a person entrain their voice to their core and pelvic floor movements. Many clinics, mine included, use ultrasound imaging as a clinical go-to tool. However, I want to be clear that you do not need to have imaging to appreciate and evaluate or treat, the voice-to-pelvic floor connection. Red flags for vocal dysfunction to easily screen for in your practice include:
|
|
The voice should be considered as one of the vital biomarkers of pelvic health. Dis”ease” in any of the three diaphragms especially impedes health and well-being, especially since creation of sound and voicing requires two motor systems, the emotional and musculoskeletal or voluntary motor systems.8
As clinicians, we have typically spent all our time focusing on the latter motor system, instead of the former, and now it’s time to do a deep dive to understand just how to influence the emotional motor system in its influence on the three diaphragms and the stress response. Talking is one of the activities of daily living that we all use and need, and most therapists depend on their voice to make a living.
There are many methods to optimizing voice-to-pelvic-floor health in the individual, which is part of the “art” in pelvic health prescription. Learn how to assess and plan interventions using a voice-to-pelvic floor trauma-informed approach at Dr. Garner’s course – The Voice and the Pelvic Floor scheduled for April 6 and September 7, 2024.
Resources:
- Bordoni, B., Zanier, E., 2015. The continuity of the body: hypothesis of treatment of the five diaphragms. J. Altern. Complement. Med. 21, 237–242. https://doi.org/10.1089/acm.2013.0211
- Braun Janzen, T., Koshimori, Y., Richard, N.M., Thaut, M.H., 2022. Rhythm and Music-Based Interventions in Motor Rehabilitation: Current Evidence and Future Perspectives. Front. Hum. Neurosci. 15, 789467. https://doi.org/10.3389/fnhum.2021.789467
- Lee, J.H., 2016. The Effects of Music on Pain: A Meta-Analysis. J Music Ther 53, 430–477. https://doi.org/10.1093/jmt/thw012
- Finn, S., Fancourt, D., 2018. The biological impact of listening to music in clinical and nonclinical settings: A systematic review. Prog Brain Res 237, 173–200. https://doi.org/10.1016/bs.pbr.2018.03.007
- Rudavsky, A., Hickox, L., Frame, M., Philtron, D., Massery, M., n.d. Certain Voicing Tasks Improve Balance in Postpartum Women Compared with Nulliparous Women. Journal of Women’s Health Physical Therapy 10.1097/JWH.0000000000000242. https://doi.org/10.1097/JWH.0000000000000242
- Volløyhaug, I., Semmingsen, T., Laukkanen, A.-M., Karoliussen, C., Bjørkøy, K., 2024. Pelvic floor status in opera singers. a pilot study using transperineal ultrasound. BMC Women’s Health 24, 67. https://doi.org/10.1186/s12905-024-02895-6
- Rudavsky, A., Turner, T., 2020. Novel insight into the coordination between pelvic floor muscles and the glottis through ultrasound imaging: a pilot study. Int Urogynecol J 31, 2645–2652. https://doi.org/10.1007/s00192-020-04461-8
- Holstege, G., Subramanian, H.H., 2016. Two different motor systems are needed to generate human speech. J. Comp. Neurol. 524, 1558–1577. https://doi.org/10.1002/cne.23898
AUTHOR BIO:
Dr. Ginger Garner PT, DPT, ATC-Ret

Dr. Ginger Garner PT, DPT, ATC-Ret is a clinician, author, educator, and longtime advocate for improving access to physical therapy services, especially pelvic health. She is the founder and CEO of Living Well Institute, where she has been certifying therapists and doctors in Medical Therapeutic Yoga & Integrative Lifestyle Medicine since 2000. She also owns and practices at Garner Pelvic Health, in Greensboro NC, where she offers telehealth and in-person wellness and therapy services. Ginger is the author of multiple textbooks and book chapters, published in multiple languages. She has also presented at over 20 conferences worldwide over 6 continents across a range of topics impacting the pelvic girdle, health promotion, and integrative practices.
Ginger is an active member of APTA, serving as the Legislative Chair for APTA North Carolina, as a Congressional Key Contact for APTA Private Practice, and in the Academy of Pelvic Health. Ginger lives in Greensboro, NC with her partner, 3 sons, and their rescue pup, Scout Finch. Visit Ginger at the websites above and on Instagram and YouTube.

Eating Disorders Awareness Week (EDAW), is February 26-March 3, 2024! It is an annual campaign to promote education about eating disorders. This week is also intended to provide hope and support for individuals and families affected by eating disorders. Awareness is key for both the public and the healthcare community.
We, as pelvic health providers, have the privilege to work with people of all genders with complex and often complicated medical histories. What are we really missing? What do we read (or not read) between the lines? What are cries for help that we are not hearing or noticing? As pelvic providers, we just need to keep our eyes, ears, and hearts open to our patients. The art of listening, observing and respectfully inquiring may be our greatest superpower. Imagine we are doing a puzzle without the puzzle box. Often it will take us time to gather the pieces and start to see the fuller picture. As health care providers, we carefully look at the whole puzzle - not just one piece… and sometimes this does take time.
Let’s take a look at a typical day in our busy clinical lives. Maybe you can relate. On our first visit with our patient, we are working hard (and sometimes fast) to try to get a thorough history, have appropriate functional outcome measures completed, ensure that all of the necessary “paperwork” is completed for our office or health care system, do our objective examination, pelvic muscle assessment, establish a prognosis, goals, a plan of care, etc. Does this sound familiar? How much can we fit into the time we are allotted at our workplace to get a picture of our patient? During this first visit do we get all of our answers? Or do we instead have a lot more questions?
We all see people struggling with eating disorders or people who have been recovering from an eating disorder - whether we are aware of this or not. The important thing to remember is that we do not treat eating disorders - we treat the individual who walks into our office with pelvic pain, constipation, abdominal pain, abdominal bloating, fecal incontinence, pelvic organ prolapse, urinary urgency, urinary incontinence, etc. We can ask some questions, do some observation, and have some conversations with our patients.
Many people have disordered eating patterns - perhaps eating too much or too little, following fad diets, having ideals of what they want their body should look like, etc. However, for some, their life may take a path that they did not expect from a multitude of biological, psychological, and social factors. Some of these factors include genetics/ family history, environment, societal / health care weight stigmas, trauma, sexual abuse, personality traits, brain chemistry, negative energy balance, hormonal levels, social support (or lack of), family dynamics and comorbid medical and/or mental health conditions (to name a few).
Eating disorders are mental illnesses with serious and sometimes fatal medical complications. Please understand - this illness is not about the food. Just eating “more” or “less” is not going to “cure” the illness. It is not that easy. What triggers an eating disorder may not be what keeps someone in the grips of it. Living with an eating disorder is distressing, consuming, life-sucking, isolating, secretive and painful. Having an eating disorder is NOT a choice. Treatment for eating disorders requires a team of support including mental health professionals, dieticians, primary care practitioners and specialists skilled with working with these individuals. We can be a part of this team. These disorders cause GI distress and nutritional rehabilitation for those who have to bring more nutrition into their body also causes GI distress. Recovering from an eating disorder is a complicated and often bumpy journey and we have the skills to help these people!
Here is a secret about eating disorders - they often ARE secrets. This is not something that someone may openly offer or even know for sure themselves. People with eating disorders are in all body sizes, genders, races and ages. We cannot make assumptions based on a person's weight or body size. Truthfully, people with atypical anorexia nervosa are often in bodies that would not trigger a clinical “alarm”, however, these individuals suffer from the same medical issues and complications as people with “typical” anorexia nervosa. Individuals in larger bodies may be utilizing purging behaviors such as vomiting, laxative use, may be binging and/or restricting food intake the same as someone in a smaller body. We cannot expect just a young, white, thin woman to have an eating disorder. They certainly may - but so may the person you just saw the hour before who is a thirty-year-old transgender woman, the 18-year-old male wrestler from the day before, the mother who is 2 months postpartum who is coming in this afternoon, or the 74-year-old woman you saw two hours ago.
We may see a person who avoids a mirror or is constantly checking their appearance. We may notice a person who is always cold and wearing layers. We may have someone who when we ask them about their relationship with food, clearly avoids the topic or tells us that they eat “ultra clean” and have limited many types of food groups in their “diet”. We may hear someone tell us many times how they do not want to gain weight so they will not consider eating more frequently, despite their painful constipation, because they “fast” for 22 out of 24 hours a day. They may also be able to give us calculated accounts of how much or how little they ate. Or, maybe they will tell us that they are so ashamed that they eat so much when they are stressed and how they cannot help it. Possibly, we may hear our patients tell us that they exercise every day, despite the weather, and sometimes more than once a day. Maybe they tell us that they haven’t been hanging out with their friends anymore and that no one understands them.
If you do notice that there are concerns, talk to your patient, let them know why you are concerned, and offer to help them find resources to provide support for them. If you do suspect someone is struggling with an eating disorder, provide them resources if they are agreeable. National Eating Disorders Association (NEDA), National Association for Anorexia Nervosa and Associated Disorders (ANAD), Eating Disorder Hope, National Alliance on Mental Illness (NAMI), Eating Recovery Center (ERC) are just a few of the great places to start.
Try to build a network of dieticians, mental wellness providers, primary care providers, GI specialists, and other practitioners who have interest, knowledge and expertise with people with eating disorders. This will likely not be easy to find. We have the skills to help these individuals during distress with active disorders and during recovery.
Join us in Eating Disorders and Pelvic Health Rehabilitation on April 6 and 7 to discover more about eating disorders and ways that we, as pelvic health professionals, can provide assistance and relief to these individuals as they struggle and as they recover. Learn more about the dangerous medical complications with eating disorders, how to identify individuals who may need support, and treatment options to assist these individuals on their journey to improved health. Explore ways to grow your clinical practice with this patient population. Looking forward to seeing you there!

In my first year of PT school, in the jumble of summer anatomy class and lab, the pelvic floor was briefly mentioned. The gist of the lesson was that it was a very in-demand field, there were not enough people doing it, and the majority of people affected were female. I was immediately intrigued, but also a little confused by the quick overview that was barely ever mentioned again until our special topics course 2 years later. By then, I was certain I wanted to learn more.
In my third year of PT school, I took the Herman & Wallace Pelvic Floor Level 1 (now Pelvic Function Level 1) course and entered my last clinical internship at a fully dedicated pelvic floor practice. The experience gave me exposure to the wide variety of pelvic floor issues that physical therapy can address. In school, it was mainly presented as something that was primarily addressed post-partum. In the clinic, it actually showed up as that coupled with a bulk of nulliparous patients of all genders and lifestyles with pelvic pain, complex cases with multiple co-morbidities, and incontinence in all age groups. This larger view of the field solidified my belief that pelvic floor rehab was being underutilized.
Through the following years, I worked in many different settings including hospital-based outpatient and private practices. Exposure to multiple populations across three states again broadened my view of pelvic rehab to something that could benefit so many people throughout their lifespan. In the summer of 2020, I began working under the mentorship of Raquel Perlis in her clinic in Wellesley, MA. Being one of the first pelvic rehab practitioners in the PT world, Raquel is widely known for her treatment of the chronic pelvic pain population. Together we addressed many cases of vaginismus, vulvodynia, SI joint pain, coccydynia, endometriosis, rectal pain, etc. Working with the pelvic pain population was both challenging and rewarding, as working with many chronic conditions in PT can be.
The experience of working with so many people suffering not just from the initial physical condition, but also from neglect, medical gaslighting, and shame, led to my decision to sign up for the Pelvic Rehab Practitioner Certification exam towards the end of my time in the Boston area in 2023. I knew I wanted to try to go out on my own in my next location and I believed that having the PRPC would give both me and my patients confidence in my skills as a practitioner operating independently for the first time. I had done most of my pelvic floor education with Herman & Wallace and mentors and for this reason, this was the best choice for me.
For me, seeing patients with pelvic pain has become my main interest. In my years of experience, no matter where in the country I am working, I see that the dismissal of pain, especially in women, LQBTQIA+, and nonbinary individuals, is all too common and often compounds the distress of those already suffering from physical discomfort. There have been multiple times when I or a colleague would be the first to acknowledge that a patient’s pain was even real. Too many were initially told by healthcare providers that the pain was in their heads or stemmed from anxiety. Of course, anxiety is often seen in the chronic pain population, but as a result of the pain they are experiencing, not the cause of it.
Gaslighting individuals with symptoms that are not easily explained has been an ongoing theme in the history of medicine and it continues to be an issue despite the advances we have made. It is estimated that innovation in the area of women’s health is at least 20 years behind other fields. We should not be dismissing what we do not know. The current structure of our healthcare system often does not give healthcare providers enough time or bandwidth to address complex pain and acknowledge what they cannot explain. That is the gap rehab providers like me seek to fill.
For me, patient education is without a doubt the most important aspect of my interaction with patients. Education is key to reducing anxiety over the unknown and giving people back power over their bodies. It is also preventative medicine. When a patient is taught how and encouraged to care for themselves, we prevent the recurrence of a condition or disease. Unfortunately, working together with patients to teach them how to care for themselves and repair their bodies is the important work that is often the first thing to be thrown out in a system built for acquiring as many high-paying codes in as little time as possible. Luckily, PTs and other rehab professionals are given a little more time with patients to help them understand their physical bodies and conditions.
Currently, I own and operate my own mobile pelvic PT clinic in Burlington, Vermont where I go to meet people where they are. This concept evolved over years of seeing busy individuals with long work hours, non-existent childcare, transportation issues, or all of the above struggle to make their recurrent follow-up PT appointments that often are scheduled for the middle of the day. My caseload now includes individuals as young as 15 as well as those who are middle-aged, post-partum, just out of college, and older adults.
Recently, I have been pursuing continuing education and training in helping people overcome pain and recover function post-op gender-affirming surgery, cancer treatment, and oncological surgery. I also have begun filling in as a teaching assistant at Herman & Wallace courses when I can. Education is not only important for patients, but I think it is also key to being an evolving practitioner and keeping the work ever new, interesting, and exciting. I hope to continue growing as an educator and eventually move into more teaching roles in the future.
BIO:
Rachel Martone, PT, DPT, PRPC, CYT graduated with her Doctorate of Physical Therapy from Hunter College in 2016 and has been working as a physical therapist in pelvic rehab for the past 8 years. Dr. Martone is a Certified Pelvic Rehab Practitioner with Herman & Wallace and has received her yoga teacher certification from Down Under Yoga. Currently, Rachel owns and operates her own mobile pelvic rehab clinic in Burlington, VT.
Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES graduated from Central Washington University with a Bachelor of Science (BS) in exercise science and a minor in nutrition in 2004 and completed her Doctor of Physical Therapy (DPT) at the University of Washington in 2007. Rachel practices in Seattle at Flow Rehab in the Freemont Neighborhood with Holly Tanner and focuses her patient care on orthopedics, female athletes, and women’s health conditions for bladder & bowel dysfunctions, pelvic, pain, pregnancy, and post-partum issues.
I have always been very particular about the precision of words. I have been known to ruminate about the origin, evolution, and application of words. As my husband always kindly says, I am an overthinker. This leads me to our nomenclature analysis for today, Diastasis.
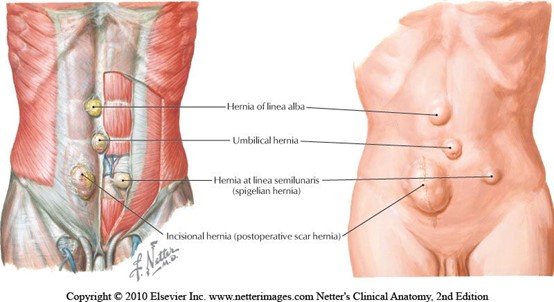 When teaching pregnancy and post-partum courses we always have healthy discussions about Diastasis Rectus Abdominus (DRA) as this is an important topic in the peripartum world. One question that always comes up is what is the difference between a hernia and DRA? If DRA is not a condition you deal with often in the clinic, it can be a bit confusing. According to the Merriam-Webster Dictionary diastasis means “an abnormal separation of parts normally joined together,” so DRA is often defined as a separation of the Rectus Abdominus muscles. I think the word separation is what causes the confusion. This word may lead some people to think there is an actual disruption of the abdominal tissue which is not the case. The rectus abdominus halves remain joined together by the linea alba. The linea alba is the tendinous raphe formed by interdigitating fascia of external/internal obliques and Transversus Abdominis. A DRA is an increase in the distance between the right and left Rectus Abdominus halves. If you stretch connective tissues (increase the distance between two ends), they may become thinner, lengthened, or weakened. A DRA is an increased distance between the right and left Rectus Abdominus halves that may result in lengthened, thinner, weaker tissue. In contrast, a hernia is an actual defect in the connective tissue. DRA and hernias are not the same thing; however, they can exist together.
When teaching pregnancy and post-partum courses we always have healthy discussions about Diastasis Rectus Abdominus (DRA) as this is an important topic in the peripartum world. One question that always comes up is what is the difference between a hernia and DRA? If DRA is not a condition you deal with often in the clinic, it can be a bit confusing. According to the Merriam-Webster Dictionary diastasis means “an abnormal separation of parts normally joined together,” so DRA is often defined as a separation of the Rectus Abdominus muscles. I think the word separation is what causes the confusion. This word may lead some people to think there is an actual disruption of the abdominal tissue which is not the case. The rectus abdominus halves remain joined together by the linea alba. The linea alba is the tendinous raphe formed by interdigitating fascia of external/internal obliques and Transversus Abdominis. A DRA is an increase in the distance between the right and left Rectus Abdominus halves. If you stretch connective tissues (increase the distance between two ends), they may become thinner, lengthened, or weakened. A DRA is an increased distance between the right and left Rectus Abdominus halves that may result in lengthened, thinner, weaker tissue. In contrast, a hernia is an actual defect in the connective tissue. DRA and hernias are not the same thing; however, they can exist together.
Let’s contrast these two conditions. Hernias can occur anywhere in the abdominal wall, whereas DRA is only at the midline. Hernia can strangulate intestines, but DRA does not as there is no hole or defect in the connective tissues. The only way to truly diagnose a hernia is by ultrasound. The only definitive treatment of a hernia involves surgery with closure of the hole, sometimes supported by mesh. Patients may elect to not have surgery if the hernia is small, is not painful, or if other conditions make surgery too risky. For diastasis, treatment rarely involves surgery. Hernias are disrupted fascia. Diastasis is lengthened, thinning, or weakened fascia.
 Diastasis Rectus Abdominus occurs commonly towards the end of pregnancy, with 66-100% of women having DRA by the end of the third trimester (Boissonnault & Blaschak, 1988; Mota et al, 2015). Mota et al. 2018 measured the distance between the two rectus halves in 84 primiparous women in the third trimester 2 cm below the umbilicus and found the average to be 49-79 mm. In contrast, a study of 150 nulliparous women (Beer et al.) showed the inter recti distance at that same point (2 cm below umbilicus) to be 16mm. However, DRA is not exclusive to the pregnant or postpartum person, they can exist in children and men as well.
Diastasis Rectus Abdominus occurs commonly towards the end of pregnancy, with 66-100% of women having DRA by the end of the third trimester (Boissonnault & Blaschak, 1988; Mota et al, 2015). Mota et al. 2018 measured the distance between the two rectus halves in 84 primiparous women in the third trimester 2 cm below the umbilicus and found the average to be 49-79 mm. In contrast, a study of 150 nulliparous women (Beer et al.) showed the inter recti distance at that same point (2 cm below umbilicus) to be 16mm. However, DRA is not exclusive to the pregnant or postpartum person, they can exist in children and men as well.
Another example of the word diastasis, where separation does not mean disruption, is with pubic symphysis diastasis. The words may be confusing. When a patient hears the word diastasis and is told it means separation, they may conclude they have a disrupted pubic joint. I think the definition of it from Stolarczyk et al. is much more descriptive and less likely to cause angst in a patient. “A pubic symphysis diastasis (PSD, diastasis symphysis pubis) is defined as excessive widening of the system of anatomical structures that make up the pubic symphysis (above the physiological norm of 10 mm), occurring during pregnancy or postpartum.”
This is another instance where the word separation may imply disruption when it just means increased distance.
Let’s return our thoughts to the title of this blog. I hope we are thinking about how the words we choose make our patients feel. Many of our patients receive a diagnosis and turn to the internet, where they may find confusing and even scary descriptions of their condition. If you were told that your abdominals had separated, doesn’t that sound scary? Would you feel nervous that your organs may fall out from your separated abdominals? I would have so many questions and fears! How will they get back together, what activities should I refrain from, can I even move? Wouldn’t the term separated make you feel scared to do anything? Think about the term separated shoulder, we hear it all the time in sports, we know it is a torn AC joint. There is an actual disruption of tissue, but DRA is not. As health care providers it is important that we use safe and encouraging words with our patients. Our role should be to educate them on their condition and make sure they understand the anatomy, physiology, and functional implications. We need to empower. The more a patient knows about their condition, the better choices they make regarding activity and lifestyle. Words are powerful.
References:
- Boissonnault, J. S., & Blaschak, M. J. (1988). Incidence of diastasis recti abdominis during the childbearing year. Physical Therapy, 68(7), 1082-1086.
- Mota, P., Pascoal, A. G., Carita, A. I., & Bø, K. (2018). Normal width of the inter-recti distance in pregnant and postpartum primiparous women. Musculoskeletal Science and Practice, 35, 34-37.
- Beer, G. M., Schuster, A., Seifert, B., Manestar, M., Mihic‐Probst, D., & Weber, S. A. (2009). The normal width of the linea alba in nulliparous women. Clinical anatomy, 22(6), 706-711.
- Stolarczyk, A., Stępiński, P., Sasinowski, Ł., Czarnocki, T., Dębiński, M., & Maciąg, B. (2021). Peripartum Pubic Symphysis Diastasis—Practical Guidelines. Journal of clinical medicine, 10(11), 2443.