Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician who wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process. To learn more join Christine in her upcoming course scheduled for February 10-11, 2024.
Conversations about menopause are becoming more mainstream. What used to be a taboo subject has thundered into the media in triumphant fashion. Drew Barrymore, Oprah Winfrey, and Maria Shriver are just a few of the celebrities spreading the word about this transition that will affect all menstruating people at some point in their lives. Despite the headlines and increased coverage, most women feel uneducated and underprepared for how this transition will manifest itself in their bodies concerning symptoms and long-term health (Tariq et al., 2023). Pelvic health providers are the perfect people to educate their patients on these changes.
Menopause is defined as twelve months with no menstrual cycle. Once this has occurred, a patient has then entered a post-menopausal state. However, the process of reaching this twelve-month milestone will begin long before menopause is achieved (Lewis 2021). Symptoms are often experienced in the transitional process leading up to menopause, years before it finally occurs. Perimenopause is the precursor to menopause and represents a time when the ovary begins to change. Hormone levels begin to fluctuate which can affect cycle regularity and intensity. Cycles can now occur every three weeks, ovulation can become irregular, and periods can become heavier. When hormones and cycles change, symptoms can begin. Sleeplessness and night sweats before the onset of menstruation can be an early indicator of perimenopause as well as increased anxiety, brain fog, and irritability (Aninye et al., 2021). These changes can begin in patients as early as their late teens but most commonly will occur in the late 30’s and early 40’s. Knowing how to recognize symptoms that can occur during the perimenopause transition can help to educate patients on what is occurring and what they can anticipate as the ovary continues to age.
Genitourinary Syndrome of Menopause is just one of the many conditions that can occur during this time. It is a cluster of symptoms that can be experienced by patients during this transition. Vaginal dryness, dyspareunia, urinary frequency, and urinary incontinence are included in this disorder (NAMS 2022). To better treat these diagnoses, healthcare providers need to ask questions about menstrual regularity and cycle changes in addition to a patient’s bowel and bladder habits. Often, hormones play a role in their urinary and vulvar symptoms. Without understanding this connection, providers are often missing an important piece that could assist in the treatment of genitourinary complaints.
Changes in hormone levels will also impact other systems in the body. As these fluctuations begin, patients can begin to have effects on their cardiovascular system, brain function, and bone health (Aninye et al., 2021). As health care providers, understanding this impact can help to guide patients down a better path of wellness through lifestyle modifications and referrals to physicians specializing in menopause. Basic recommendations on sleep, exercise, and eating habits during this transition can set up a trajectory of better aging and holistic health.
While the prescription of medications is beyond a therapist’s scope of practice, having a thorough understanding of the risks and benefits of these treatments can help educate our patients on their options for symptom management. Understanding their applications in the treatment of symptoms helps to remove societal and medical biases that have existed for over twenty years. It allows for giving patients more informed choices when it comes to their bodies. Women going through menopause are made to think that bearing their symptoms is a rite of passage, yet proper care and consultation can ease these often life-altering effects. Education on options of treatment and appropriate referral is key to empowering patients.
It is never too early or too late to begin a conversation about menopause. Habits and lifestyle in younger people, such as exercise, sleep hygiene, and self-care can have an impact on the changes they will experience later in life. In our post-menopausal patients, these same habits and lifestyle choices can be implemented to assist with improving health outcomes and the aging process. Understanding this transition is key to any healthcare provider treating current or past menstruating people.
As clinicians, we are often the first line of support when it comes to these patients. There is a lack of education for treating this population (Macpherson and Quinton 2022). Knowing the questions to ask can allow for better treatments, healthcare outcomes, and longevity. Patients are hungry for this information but sometimes need encouragement in pursuing treatments and finding solutions with their healthcare team. As pelvic health specialists, this gap can be bridged by providing patients with information regarding their changing cycles and how this can affect their long-term health. This education can change their lives. Let us keep making menopause mainstream.
References:
- The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause, 2020. 27(9): p. 976-992.
- Aninye, I.O., et al., Menopause preparedness: perspectives for patient, provider, and policymaker consideration. Menopause, 2021. 28(10): p. 1186-1191.
- Lewis, R., Why is menopause a priority in primary care?, in Confidence in the Menopause, N.H. Research, Editor. 2021, Fourteen Fish: United Kingdom.
- Macpherson, B.E. and N.D. Quinton, Menopause and healthcare professional education: A scoping review. Maturitas, 2022. 166: p. 89-95.
- Tariq, B., et al., Women's knowledge and attitudes to the menopause: a comparison of women over 40 who were in the perimenopause, post menopause and those not in the peri or post-menopause. BMC Women’s Health, 2023. 23(1): p. 460.

It's been four years since my pelvic floor bestie (fellow Lead TA Carly Gossard) convinced my introverted self to try my hand at teaching assistant. I was hesitant, to say the least. I had taught small lab groups at Stockton University and mentored many of my colleagues in different areas, including pelvic health, but a class of 50 people relying on me to guide them through their first pelvic exam experience…I was terrified. It was the weekend before the world shut down for COVID, so there was this underlying current of “What does the future hold” and “Should we steal the gloves and hand sanitizer?”
Flash forward to the present day. I consider myself so lucky to wear many hats for Herman & Wallace. That first TA experience sparked this love of being with the Level 1 students as they embark on their pelvic health provider journeys. When HW needed to shift to the satellite model, I was one of the first TAs to jump into that role. When Megan Chamberlain (herder of the TAs) asked for help building a Lead TA program, I gave her my list of suggestions (I may consider Leslie Knope from Parks & Rec a role model). One of my favorite things about HW is that they take feedback seriously. At one point, they realized they needed someone to track the patterns of that feedback and guess who got that job….ME!
In 2023, the HW team decided it was time to take that feedback and update the main series to be more…more inclusive, more advanced, more hands-on, more to take home immediately to clinical practice. I was quick to chime in as I had a lot of subjective data from years of review synthesis. We have been organizing, researching, considering, consulting, and revamping the main series, and the first two classes of the series launched in January 2024! As the series rolled out, I decided I needed to TA each class to feel and experience the changes.
I spent January 14th and 15th at Hunter College in NYC with 30+ students during the second run of Pelvic Function Level 1. It went just as amazing as I had hoped as I helped the content team build it. The precourse work laid the foundation for more inclusive providers, reviewed the basics, and set students up to be ready for more advanced and hands-on content in class. There was penile-scrotal anatomy in this course instead of participants having to dive deeper into the pelvic floor series to learn these structures exist. It took about 2 years of my pelvic health career for that to happen in a class for ME! Students came in with more comfort on what they were going to do in person. They also confirmed that the workbook was the thing that hands-on, visual learners dream of. They even noticed we used bigger fonts and included closed captioning.
If you’ve interacted with me at all, through TA experiences, classes, or watching me mic run at HWConnect 2023, you’ll see I’ve come a long way from being the shy wallflower in the back of a PF1. This January, in addition to being one of the teaching assistants for Pelvic Function Level 1 in NYC, I’m also one of the first “TA Takeover” guinea pigs. What does this mean? Probably more videos of me dancing with pelvic organs from iHeartGuts joining the internet! I do hope to show you a little glimpse into what it's like to take a class with HW. In all seriousness though, HW’s goal and mission to bring quality, accessible, and inclusive care to all individuals makes it easy for me to say yes and sign up for any adventure they propose.
Pamela A. Downey, PT, DPT, WCS, BCB-PMD, PRPC is Senior Faculty with Herman & Wallace and is instructing the upcoming Pudendal Neuralgia and Nerve Entrapment scheduled for January 27, 2024. She is the owner of Partnership in Therapy, a private practice in Coral Gables, Florida where she treats women and men with pelvic floor dysfunction, related urogynecological and colorectal issues, spine dysfunction, osteoporosis, and complaints associated with pregnancy and the postpartum period. Her mission is to educate and integrate healthy lifestyles for patients on the road to wellness. Pam sat down with the Pelvic Rehab to discuss her upcoming course.
What makes pudendal neuralgia such a difficult diagnosis to treat?
I think people often see the content in Pelvic Function Level 1 - Introduction to Pelvic Health and it's like a tidy little box. Then you get the patient and as the practitioner you're like I don't know what to do with this person. We need to show that pudendal skills are needed in differential diagnosis. Even though this course is called Pudendal Neuralgia and Nerve Entrapment, it is about differential diagnosis for a lot of pelvic pain. When you feel more secure in knowing what you're treating and have a systematic way of looking at it, then you can be more productive in your patient care.
I think some ortho therapists treat in a linear fashion, and they go from week one to week eight through a protocol and things generally go well because it's a predictable course when you're rehabbing a total knee replacement, or you have an elbow tendonitis, and you expect these structures to follow a path. But then when you come into the nerve side of things, nerves can be unpredictable. They're influenced by lots of factors. It could be your mood. It could be the range of motion around a joint. It could be a previous history of another neurologic problem feeding it, such as disc pathology. It can be something around a postural habit, and it could be a straight up other dysfunction that then affects the pudendal distribution. And if you don't treat the cause of the initial, you will never improve the latter, which is the neurological presentation in pudendal.
I love that it's more about figuring out the differential diagnosis for pelvic pain and going from that angle into pudendal dysfunction, entrapment, neuralgia, and everything that goes with that. For example, you're going to get a patient with an order for pudendal neuralgia, or even worse entrapment. When they get an order for pudendal neuralgia, then they'll kind of forget that the person may not have pudendal neuralgia. They have problems in the pudendal distribution, but that's basically everything we treat. So as a pelvic rehab practitioner they have to tease it out.
When I look at a script I always say, “that's nice.” The referring doctor may have written it as pudendal neuralgia so that the patient could get reimbursement for the therapy with the diagnosis code. But then we get to add our diagnosis codes on top of that and drive a treatment plan.
So, I think that is a big hangup. Practitioners run when they usually see this diagnosis. You don't want a pudendal patient. Especially if you do not have a lot of skills, because you are going to be like, well, what can I do for this patient? If they sit, they have pain. If they exercise, they have pain. They don't have like a whole repertoire. In the pudendal neuralgia course, we talk about how to figure out if the driver is the spine, the hip, the nerve itself, if it's the pelvic floor musculature, or if it's biomechanical. There are so many facets.
How often do these scripts come in for patients that have pudendal neuralgia?
In pelvic pain they're probably coming in a high percentage, like I would say three-quarters. In practice, depending on who's referring into the person's practice, it's going to be a significant amount of walk-in traffic and referred traffic. Because every levator syndrome patient could have a pudendal issue driving the levators, and long-standing levator pain can end up being pudendal.
It's kind of like are you treating the chicken or the egg? I think giving the person skills to do test and retest and having a way to keep falling back on to this and then to also be able to transmit the idea that this isn't a fix -it problem. You know, we just don't put a band aid on it and you're done. Other folks who are more newish, who expect this linear event, they're going to struggle because there's going to be setbacks and sometimes doing more is the exact opposite of what needs to be done. Less is more.
When you look at the H&W course catalog, where would you recommend that practitioners take the Pudendal Neuralgia course?
The sweet spot for taking the pudendal neuralgia course would be practitioners who have taken PF1 and Pelvic Function Level 2A - Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain, because they learn the rectal canal and PF2A. Practitioners who focus specifically on treating the male pelvic patient would benefit from this course because it is a good thinking course for how to treat men. It could pair well with Pelvic Function Level 2C - Men’s Pelvic Health and Rehabilitation (formerly Male Pelvic Floor). In my practice I get a lot of men coming in because they look on the internet and decide that they got pudenda neuralgia.
If you understand differential diagnosis you can touch on is this a sciatic nerve problem? Is this a genitofemoral problem? We look at the lumbo-sacral plexus in a decision tree, and then we then focus on pudendal and then how people manage them from a medical standpoint and from a therapy standpoint. I talk about using a rule-out method - this could be genital femoral, this could be pudendal nerve. And then you prove what the problem is by doing test and retest.
There's also a lot of pain neuroscience, so practitioners who have taken Pain Science for the Chronic Pelvic Pain Population would benefit from this course. The pudendal neuralgia course goes really well with this course because the practitioners who have taken the pain science course already know that there's going to be ups and downs. Also Nari Clemon’s nerve courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are definitely lab -oriented courses and this could be a backgrounder even going into her series, because she's going to talk about a lot of nerve techniques that can be then applied to the pudendal. Nari's courses give solid hands-on skills to deal with nerves, palpation, and finding them. Then this course shows you how to treat them. Not necessarily Pudendal, but all the nerve things. These courses enhance each other. It's like a decision tree where pudendal is on there and you can pass through it and go into Nari’s stuff where you can get a good idea and then use your myofascial, your orthopedic, your neuro skills.

Emily McElrath, PT, DPT, MTC, CIDN is instructing her upcoming course Pregnancy & Postpartum Considerations For High Intensity Athletics scheduled on March 9, 2024. Emily is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance and is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and CrossFitter and has personal experience modifying these activities during pregnancy and postpartum.
It’s no secret that high intensity exercise during pregnancy and early postpartum has been debated for years. For many decades, pregnant female athletes have been told things like “you shouldn’t be doing that,” or “that’s not safe.” Are these claims rooted in truth or misunderstanding? I personally think more of the latter, and as it turns out the research supports that as well. In fact, the entire narrative around high intensity exercise in pregnancy seems to be shifting.
In truth, I believe some of the disconnect comes from a lack of understanding of high intensity exercise by clinicians. While many clinicians themselves participate in high intensity exercise, many others do not and also do not understand high intensity exercises like powerlifting, orange theory, crossfit, triathlon training, etc. The other part of the disconnect comes from a general lack of research on the subject. Thankfully, this is also changing and more research is being done on the impact of high intensity exercise on fetal and maternal health, as well as the pelvic floor and core. But up until recent years, we had mostly anecdotal evidence. Finally, we are seeing more and more clinicians being athletes themselves, which has led to a personalized understanding of high intensity exercise during pregnancy and postpartum. Interestingly enough, many of these athlete clinicians are on the frontlines of the current research.
Some of the most recent research that we should highlight includes:
“Clinical and exercise professional opinion of return-to-running readiness after childbirth: an international Delphi study and consensus statement.” This international Delphi survey was published in the British Journal of Medicine and surveyed over 100 clinicians and exercise professionals on readiness to return to running postpartum. They asked these professionals to define “runner” and “postpartum,” what biopsychosocial milestones they felt runners needed to meet, various methods of screening they recommended, supportive items they may recommend, a timeline for when and how to return to running, factors that may contribute to them advising a patient against running, and other educational points they felt were important. At least 75 % of the participants or more felt that, following a minimum 3-week period of rest and recovery, and as long as the patient has met all screening criteria, an individualized return to running progression can be considered.
“Impact of Pelvic Rest Recommendations on Follow-Up and Resolution of Placenta Previa and Low-Lying Placenta.” This retrospective study was published in the Journal of Ultrasound in Medicine in March of 2023 and reviewed 410 pregnancies of women who had placenta previa (144) or low-lying placenta (266). 45% of placenta previa patients and 12% of low-lying placenta patients were placed on pelvic rest. All of the study participants were given an ultrasound at 28 weeks gestation. Resolution occurred in 51% of the placenta previa patients and 75% of the patients with low-lying placenta regardless of whether they were placed on pelvic rest or not. This is exciting because it may indicate that women with placenta previa and/or low-lying placenta previa may not need to be placed on pelvic rest and/or limited from activity.
Another study done by Eichelberger, et al. in the American Journal of Perinatology in 2011 found that 84% of complete placenta previas and 98% of marginal placenta previas resolved naturally by roughly 28 weeks. This study is promising because it shows that while some pregnant athletes may be temporarily limited from exercise, they may be able to return after resolution of the previa.
A study published in 2020 by Chen et al looked at the role of exercise in treating low back pain in pregnancy and found that the transverse abdominis, multifidus, pelvic floor, and diagonal trunk musculature play a significant role in load transfer in the lumbopelvic region. This is important to consider when working with pregnant athletes as we can use these concepts via accessory work to support their tissues for more strenuous activity.
While many of these studies were small, and survey only in nature, it is promising to see more research being done. In the meantime, we have lots of anecdotal evidence that women who were high intensity athletes prior to pregnancy can in fact continue their desired level of exercise confidently and safely. Additionally, when we as clinicians have a thorough understanding of the musculoskeletal system, and how those tissues handle various loads, we can help patients modify as needed to continue loading those structures appropriately and without risk of injury. The goal of my course Pregnancy and Postpartum Considerations For high intensity Athletics is to help give clinicians the confidence they need to work with this patient population. I blend research, clinical experience, and personal experience as a pregnant athlete to help clinicians understand how to meet these athletes where they are to help them continue doing what they love. My mission is to empower women to feel strong, capable, and healthy (mentally, emotionally, and physically) throughout their pregnancy and as they recover postpartum and to change the narrative surrounding high intensity exercise during pregnancy from one of fear and misunderstanding to one of empowerment and encouragement.
Dawn Sandalcidi PT, RCMT, BCB-PMD is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. Dawn is a national and international speaker in the field. In addition to lecturing internationally on pediatric bowel and bladder disorders, You can join Dawn Sandalcidi with HW in her courses, Pediatrics Level 1 - Treatment of Bowel and Bladder and Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders. Her next HW course, Pediatrics Level 1, is scheduled for February 3-4 and still has seats available for registration.
In the realm of pediatric pelvic health, the issue of urinary and fecal leakage is a subject that demands a nuanced understanding. Too often, these incidents are dismissed as mere "accidents," inadvertently subjecting children to shame and stigma. It's crucial to recognize that in many cases, children are grappling with conditions such as enuresis and encopresis, which are not behavioral issues or mistakes but rather manifestations of underlying health issues. In this blog, we'll explore the issue of the most common pediatric bowel and bladder disorders, the challenges faced by both parents and healthcare professionals and the need for a holistic approach to treatment.
Understanding the Scope of Pediatric Incontinence
Enuresis and encopresis are clinical terms used to describe involuntary urine and fecal leakage, respectively, in children beyond the age when such control is typically expected. Contrary to common misconceptions, these occurrences are not the result of a child's intentional mistake. Instead, they often signal underlying physiologic disturbances as well as pelvic floor and core dysfunction, which can have wide-ranging effects on a child's physical and psychological well-being.
Causes of enuresis and encopresis can vary, encompassing a range of physical and psychological factors. In many cases, these conditions are linked to pelvic floor dysfunction and bowel issues such as constipation. However, other contributing factors may include genetic predispositions, neurological issues, hormonal imbalances, and emotional stressors. Traditional approaches, such as the outdated notion of letting a child "grow out of it," fail to recognize the multifaceted nature of these conditions. Such passive strategies not only prolong the child's suffering but also perpetuate societal misconceptions around pediatric incontinence — ” What’s ‘wrong’ with these kids?”. Truly, nothing is “wrong”, except that children aren’t granted the access they need to professionals equipped to help. It is imperative to replace such antiquated views with informed, proactive approaches that address the root causes of enuresis and encopresis, providing children with the support and interventions they need to thrive.
Enuresis and Encopresis: Current Challenges
Only about 15% of children per year will organically “outgrow” bedwetting. This statistic underscores the prevalence of the issue and highlights the need for a compassionate and informed approach. Many children experiencing urinary and fecal leakage endure shame, embarrassment, and self-esteem issues, leading to internalizing and sometimes externalizing psychological behaviors.
Parents and healthcare workers encounter formidable challenges when confronted with pediatric incontinence. Beyond the inherent complexities of addressing the physical and emotional well-being of affected children, navigating the healthcare landscape presents additional hurdles. The prevailing societal perception that dismisses these incidents as mere "accidents" contributes to the challenges parents and healthcare professionals face. One of the primary obstacles is the scarcity of trained healthcare providers specializing in pediatric pelvic health. Locating professionals with the expertise to address the nuanced complexities of enuresis and encopresis can be a daunting task, often resulting in delayed or inadequate care.
Moreover, time constraints faced by healthcare providers pose another significant challenge. Parents seeking assistance often find themselves struggling to locate professionals who not only possess the necessary expertise but also have the time to listen attentively to their concerns. In a system where healthcare practitioners are stretched thin, the need for personalized attention and understanding of the intricate nature of pediatric incontinence can be overlooked.
Navigating the intricate web of insurance and referral systems exacerbates the situation. Healthcare workers often grapple with bureaucratic hurdles that can impede the timely access of patients to necessary interventions. Delays in appointments due to administrative complexities not only prolong the child's suffering but also add to the stress experienced by both parents and healthcare providers.
Furthermore, the societal misconception surrounding pediatric incontinence compounds the emotional burden on families. The prevailing notion that these incidents are either behavioral or somehow otherwise the fault of the child contributes to a culture of silence, making it challenging for parents to seek support and understanding from their social circles. The stigma associated with pediatric incontinence can lead to feelings of isolation and shame, inhibiting open discussions about the challenges faced by affected children and their families.
In light of these challenges, it becomes evident that addressing pediatric incontinence requires a multi-faceted approach. Dawn Sandalcidi, a trailblazer and seasoned practitioner in pediatric pelvic health, emphasizes that these issues go beyond the pelvic floor. Children with pelvic floor dysfunction often present with ribcage and core dysfunction, necessitating a broader perspective in treatment. Without a “how-to” manual, Dawn tackled these issues head-on. She incorporated her decades of clinical experience and developed coursework such that other practitioners in the United States (and around the world!) can more easily access effective training on how to treat the pediatric pelvic floor.
Efforts should be directed not only toward enhancing the availability of trained healthcare professionals but also toward dismantling societal misconceptions and streamlining administrative processes. By fostering a more supportive and informed environment, we can empower parents, healthcare workers, and, most importantly, the children affected by enuresis and encopresis to navigate the intricate landscape of pediatric pelvic health with resilience and understanding.
A Holistic Approach to Pediatric Pelvic Health
Dawn Sandalcidi's courses offer a comprehensive understanding of pediatric pelvic health. Pediatrics Level 1 - Treatment of Bowel and Bladder Disorders covers the basics of pediatric pelvic floor anatomy, physiology, and voiding reflexes. Biofeedback and ultrasound techniques provide less invasive alternatives for children. Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders expands the focus beyond the pelvic floor, examining the entire musculoskeletal system in more complex cases, offering evaluation and treatment techniques that “zoom out” to look at the whole child.
Acknowledging that children don't comprehend pain in the same way as adults, a biopsychosocial approach is essential. The incorporation of enjoyable elements makes the treatment process more accessible for young patients.
It's time to shift the narrative around pediatric incontinence. Labeling these incidents as accidents not only oversimplifies the complex challenges children face, but lends to an environment where children aren’t able to truly heal - not just physically, but mentally and emotionally as well. Dawn Sandalcidi's expertise underscores the need for practitioners to view pediatric pelvic health holistically, and to move toward a trauma-informed approach. By understanding the interconnectedness of pelvic and full-body musculoskeletal health and adopting innovative treatment approaches, we can empower both children and their families to navigate the complexities of pediatric incontinence with compassion and understanding. Let's move beyond the 'accident' label and foster an environment where children feel supported, not ashamed, in their journey to health and well-being.

Ramona Horton, MPT, DPT developed and instructs the visceral and fascial mobilization courses for HW and presents frequently at local, national, and international venues – including International Pelvic Pain Society, CSM and HWConnect - on topics relating to women’s health, pelvic floor dysfunction, and manual therapy. Join Ramona in her upcoming course, Mobilization of the Myofascial Layer: Pelvis and Lower Extremity this February 2-4, 2024.
1. Learn from Ramona Horton!
Ramona C. Horton MPT, DPT serves as the lead therapist for her clinic’s pelvic dysfunction program in Medford, OR. Her practice focuses on treating adults and children with urological, gynecological, and colorectal issues. Her PT career began in the US Army, and she has taken the military “mission first” mentality into her approach to patient care. Simply said, “Diagnosis is just a label, perform a comprehensive musculoskeletal evaluation and treat what you find”. For her many contributions to the field of pelvic health, Ramona was awarded the prestigious Academy of Pelvic Health Elizabeth Noble Award in 2020.
2. The myofascial course is a concepts course.
The whole idea of the myofascial course is to help clinicians learn to problem-solve. To learn some basic concepts of physiology and mobility testing to stop chasing the boo-boo, and instead find and treat the cause. Just because it hurts at the right SI joint, doesn’t mean that you should treat the right SI joint. Joint hypermobility is profoundly nociceptive, especially in a one-bone/two-joint scenario as the sacrum and SI joints. Consider the idea that pain may be generated on the right from hypermobility that is a result of hypo-mobility on the left. Which side should then be treated, the painful side or the stiff side? Let’s treat where the brain is protecting and guarding the tissue.
3. Understand the true function and mechanisms of manual therapy.
Manual therapy is presented as a concept and technique that does NOT “release” tight or bound fascia based on the skill or magic hands of the practitioner. The issue is not in the tissue, if the tissue is tight, it’s tight because the brain is keeping it that way. Muscles are marionettes, and the brain is the puppet master. Manual therapy utilizes the fascial system to access the nervous system. In other words, having a conversation with the brain over the tissue that it appears to be protecting while trusting that the homeostatic mechanism is functioning in the body. If this is done in a non-threatening manner, the brain will normalize the tissue it is holding and guarding.
4. Add a whole host of new tools to your practitioner toolbelt.
The myofascial course teaches basic screening techniques that will point you in the right direction toward finding where the body is protecting, not where symptoms are being expressed. You will learn a variety of techniques to approach different fascial layers including direct and indirect fascial stacking for superficial nerves within the panniculus, muscular, and articular restrictions, as well as indirect technique of positional inhibition for trigger points. In addition, the science behind basic neural mobilization, instrument-assisted fascial mobilization and fascial decompression (cupping) are presented.
5. Learn more about fascia, its origins, and its functions.
Fascia is EVERYWHERE throughout the body; it is the ubiquitous connective tissue that holds every cell together much like the mortar in a brick wall, in addition to cells, it connects every system in the body. Fascia contains a vast neurological network including nociceptors, mechanoreceptors, and proprioceptors just to name a few. The fascial system has multiple layers within the body: starting at the panniculus which blends with the skin, the investing fascia surrounding muscles and forming septae, the visceral fascia which is by far the most complex and the deepest layer of fascia, the dura surrounding the central nervous system extending to the peripheral nerves. All fascial structures, regardless of layer or location have their origin in the mesoderm of early embryologic development. The myofascial course presents evaluation and treatment techniques for three of the four fascial layers while the three visceral courses address the complex visceral fascial layer.
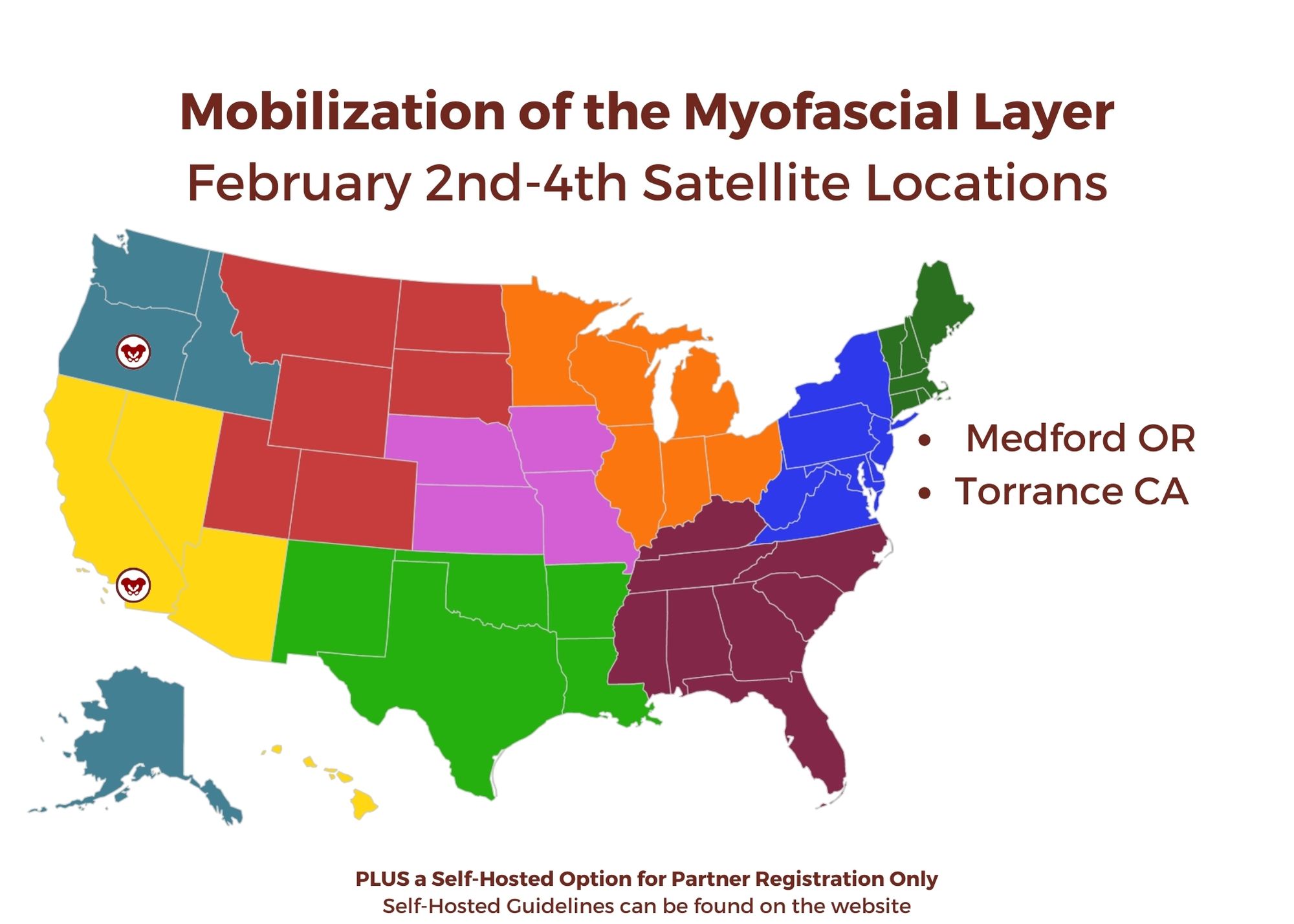
Mobilization of the Myofascial Layer: Pelvis and Lower Extremity
February 2-4, 2024
Price: $675
Experience Level: Intermediate
Contact Hours: 22.5
Medford, OR Satellite
Torrance, CA Satellite
Self-Hosted
HW Looks forward to seeing you in a future course!

Senior faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC sat down with the Pelvic Rehab Report to talk about the role pelvic therapists play on the oncology team that will work with the patient throughout treatment and into survivorship and the impact pelvic health has on quality of life for people with cancer.
Alison is part of the HW faculty team that wrote and instructs the Oncology course series, the next course is Oncology and the Pelvic Floor Level 1 on January 27-28, 2024.
Did you know that there are over 15 million cancer survivors in the United States? As advancements in care and early diagnosis improve, this is expected to increase to over 20 million survivors in the next 10 years. The continuum of care for patients with cancer ideally begins at diagnosis and the rehabilitation professional is an integral part of the oncology team that will work with the patient throughout treatment and into survivorship.
Pelvic cancers can include bladder cancer, cervical cancer, colorectal cancer, ovarian cancer, prostate cancer, and uterine cancer, among others. These patients can experience changes in how their body functions during or after cancer and its treatment. Changes caused by the treatment of cancer can lead to pain, discomfort, and problems with bowel, bladder, and sexual function
Why did you become a pelvic therapist?
I was attracted to pelvic therapy because I enjoy helping people who aren’t getting the help they need from other sources. When I first started working in pelvic floor therapy, there were not as many therapists working in the field. I absolutely loved it! I really enjoyed seeing the improvements patients made and the excitement that they had when they could come in and share with me that they saw improvements. They would share with me news about bowel, bladder, or sexual function that they would not even share with their partner. To see the happiness that people had with improvements in this intimate part of their lives really brought me joy. I enjoy helping people have hope in their lives and working with these patients is very rewarding to me.
What role does a rehab practitioner play on the oncology team?
Rehab professionals are key members of the oncology team. While the other members of the oncology team are focused on curing the cancer and helping the patient live longer, rehabilitation professionals focus on getting the patient to be able to do things in their lives that they enjoy. We are trained in working with the body and identifying dysfunction within the body that is limiting the patient and keeping them from functioning to their full potential. We have skills to address the musculoskeletal, visceral, nervous, and integumentary systems that can help improve the way a patient’s body is working and therefore improve function. Sometimes we address the little things with patients that then make the biggest impact in them living their lives. One patient of mine said that “her doctors saved her life, but her therapist helped her put her life back together so she could live it.” This quote really demonstrates the role a rehabilitation professional can have on an oncology patient.
What are some of the most important things you (and pelvic therapists) do for people with cancer in your role?
One of the most important things we therapists can do for our oncology patients is to listen. We spend a lot of time with our patients and develop a rapport with our patients. They then often share things with us they may not other providers. We have the skills to treat and help our patients with very personal symptoms in intimate areas. Pelvic floor therapists can help oncology patients return to a life that is more similar to their life before their cancer diagnosis. This is important. Their lives have been changed forever with their cancer diagnosis. If we can listen to the patient, and improve some of the symptoms they are experiencing; it can make a bigger difference than we think in helping them return to living their lives.
What are some common concerns oncology patients have, and how do you help address them?
One of the biggest issues oncology patients experience is restricted movement within the body. Surgery, and radiation both cause changes to the body that lead to scarring, fibrosis, and adhesions. This leads to a tightness that limits the normal movement of a body part, or decreased glide of the tissues. We address this a lot in the oncology series. We learn how to work with this restricted movement and help improve it. If the rehabilitation clinician can improve the ability of the body to move (whether it is a joint, a muscle, or the glide within the tissues), then this can ease pain, improve the function of that body part, and improve overall mobility and function for the patient.
What is the number one thing that practitioners should be aware of when it comes to pelvic therapy and cancer?
Radiated tissue is never the same as before it was radiated. Even if it has been years. Radiation changes the tissues. It can lead to inflammation, fibrosis, scarring, adhesions, texture change, and elasticity changes, among other effects. The effects of radiation can continue for years, and the tissues should be treated differently even if it has been many years since the patient underwent radiation. The therapist should learn to “listen” with their hand to see what state the tissues are in, and how to treat these tissues in a gentle and non-aggressive manner.
How can people with cancer better communicate with their pelvic therapists, and how can the practitioner facilitate these conversations?
I would encourage any cancer survivor to tell their therapist what is keeping them from doing what they love. When someone is diagnosed with cancer and goes through treatment, they often become limited in some of their activities. Unfortunately, many people don’t return to the activities that brought them joy. I would encourage patients to tell their therapist things that they wish they could do but cannot. Even if it is something little like making the bed, cooking a meal, or walking to the bathroom without leaking. Or if it is something bigger, like jumping on the trampoline with their kids, or returning to their exercise routine.
The therapist needs to know what it is that the patient would like to do but cannot do at this time. That way we can analyze the situation and figure out what can be done to help the patient reach their goal. I encourage therapists to ask their patients “What do you wish you could do but can’t now?”, or “What activities bring you joy?” If they are not able to do these activities after cancer treatment, work with the patient to see if you can help them return to that activity. It may be in baby steps, but that still can bring the patient joy!
What are some of the most rewarding parts of your job?
What I enjoy most about my job and working with oncology patients is the hope that I get to experience alongside these patients. I have the privilege of being able to work with these fighters and help them to gain function. The happiness they have when they can return to a loved activity, have an orgasm again, or be able to go to a movie without having fecal urgency is so very rewarding. I work with patients and try to instill an optimism that they can return to a better state. However, they also give me hope in life. Seeing their perseverance, their will to live, and their fight is inspirational! Working with oncology patients provides a positive light in my life; knowing that I am helping people that really need it, and the inspiration I get from working with these patients is amazing!
Join Oncology and the Pelvic Floor Level 1 on January 27-28, 2024 to learn more about working with oncology patients as part of an interdisciplinary oncology team to improve patient outcomes and quality of life.
Kristina Koch, PT, DPT, WCS, CLT is a board-certified clinical specialist in women’s health physical therapy and a certified lymphedema therapist. Kristina has been treating pelvic health conditions in individuals of all ages and genders since 2001 and works in private practice in Colorado Springs, CO. Kristina is a member of the HW faculty with her own course, Pharmacologic Considerations for the Pelvic Health Provider, scheduled next on February 4, 2024.
Why it is Important to Know Pharmacology
All rehab providers need to have a foundational understanding of pharmacology for numerous reasons, all of which contribute to providing safe, effective, and comprehensive care to their patients. In pelvic health, therapists often encounter patients who are taking numerous medications, and it is important for us to understand how these drugs may impact a patient's physical function, exercise tolerance, current complaints, and overall well-being.
Basic pharmacology knowledge includes:
- Understanding drug classes
- Pharmacokinetics and pharmacodynamics: how drugs exert their effect on the body and how the body impacts the drug
- Drug interactions: recognizing potential interactions between medications and how they may affect a patient's response to therapy interventions.
- Adverse Effects: awareness of possible side effects of medications that could impact a patient's ability to participate in therapy or contribute to their symptoms.
A more comprehensive understanding of pharmacology has clinical relevance on many fronts. The following bullet points highlight how understanding pharmacology has implications for clinical practice.
Assessment:
Pharmacological knowledge allows clinicians to conduct a more comprehensive assessment of their patients. Considering a patient's medication history as part of the overall health profile helps clinicians tailor treatment plans to individual needs and potential limitations.
Safe and Effective Patient Care:
Rehab providers often work with patients who are taking medications for various health conditions. Understanding pharmacology enables therapists to assess potential interactions between drugs and design safe and effective treatment plans.
Optimizing Rehabilitation Strategies:
Medications can impact a patient's response to exercise and rehabilitation. Understanding pharmacology enables rehab providers and therapists to modify treatment plans based on a patient's medication profile, potentially optimizing rehabilitation outcomes.
Pain Management:
Pain is a common reason our patients are seeking physical therapy. Knowledge of medications used for pain management enables therapists to collaborate with healthcare providers to create comprehensive pain management strategies for their patients.
Collaborative Care:
Clinicians often collaborate with physicians, nurses, and other healthcare providers. Knowledge of pharmacology facilitates effective communication, allowing therapists to discuss patient cases, contribute to treatment decisions, and foster a collaborative approach to patient care.
Educating and Empowering Patients:
Pelvic health practitioners and rehab providers play a vital role in educating patients about their health, including medications. Understanding pharmacology allows therapists to explain the purpose of medications, potential side effects, and the importance of compliance, encouraging patient engagement and adherence to treatment plans.
Recognition of Red Flags:
Knowledge of pharmacology enables pelvic health rehab providers to recognize signs and symptoms of adverse drug reactions, identify potential issues early, consult with healthcare providers, and modify treatment plans accordingly.
Informed Decision-Making:
In certain situations, therapists and rehab providers may need to make decisions regarding treatment plans and goals, treatment frequency, or modalities based on a patient's medication profile. A solid understanding of pharmacology contributes to informed decision-making.
Legal and Ethical Considerations:
Pelvic health practitioners need to work within their scope of practice. An understanding of pharmacology helps therapists recognize when it is appropriate to refer patients to other healthcare professionals for medication management.
Monitoring and Reporting:
Monitoring patients for signs of adverse reactions and knowing when to report concerns to other healthcare professionals or federal organizations.
Special Populations:
Pediatrics and geriatrics may require special consideration due to differences in pharmacokinetics and pharmacodynamics. Understanding how medications affect different age groups helps pelvic health therapists and rehab providers adapt our interventions accordingly.
As rehabilitation providers, we invest a substantial amount of time in direct interaction with our patients during their treatment sessions, surpassing the duration they spend with their primary care providers. This prolonged and more frequent engagement, spanning weeks or months, affords our patients an increased opportunity to communicate not only their physical concerns but also their apprehensions regarding medications and potential side effects. This dialogue exceeds what may occur with their physicians or primary care providers. Understanding the impact of medications on a patient is vital for effectively educating them about potential side effects and how these medications may contribute to their complaints, thereby augmenting the overall value of the treatment regimen.
With a solid grasp of pharmacology and insight into medications prescribed for pelvic health, therapists can engage in informed discussions with patients and collaborate effectively with other healthcare providers involved in their care. The capability to explore recent medications, supplements, or alternative approaches that may minimize side effects, mitigate impacts on quality of life, and enhance function. Remaining current on advancements in pharmacology is indispensable for delivering physical therapy interventions that are both effective and grounded in evidence-based practices.
In summary, a strong understanding of pharmacology enhances the overall quality of physical therapy practice. It ensures that physical therapists and rehab providers can provide patient-centered, evidence-based care while collaborating effectively within the broader healthcare team.
Join Kristina in Pharmacologic Considerations for the Pelvic Health Provider on February 4, 2024, to learn about the medications frequently used in pelvic health, their side effects, the clinical impact they may have on your patients, and possible alternatives to consider to improve patient outcomes and quality of life.

Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response.
She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
Indulgences over the holiday season lead many to experience symptoms of indigestion, part of the discomfort that fuels our renewed January focus on exercise and “eating right”.
With this in mind, let’s discuss how we as a nation handle GI distress or GERD (gastroesophageal reflux disease) symptoms. Typically here in the US, there are 2 methods we typically use:
- The quick way - by popping a Tums or Rolaids or
- The prolonged way - by taking PPI’s (proton pump inhibitors) or H-2 blockers on a regular basis (eg. Pepcid AC).
Both are reliable ways to efficiently feel a little less GI distress.
The quick relief strategy neutralizes the acid that is already in the stomach whereas the longer-acting PPI’s and H-2 blockers actually block or suppress acid production in the stomach. And even though these “longer term” drugs are designed for short-term use, the more I inquire about their use with my patients, the more a troublesome pattern emerges. Many of my patients struggling with complex symptom constellations (eg. a non-relaxing pelvic floor, constipation, perineal skin issues, gut issues, anxiety, depressive symptoms, etc.) describe that they have taken these “digestive aides” continually for years. YEARS.
So, this approach is fine, yes? We know acid reflux can lead to esophageal irritation, not to mention pain and nagging discomfort. It can lead to disordered sleep and its associated sequelae. In extreme cases, esophageal irritation could even progress to esophageal cancer. Therein lies the justification for using drugs that suppress or block acid production in the stomach over the long term. Even though long-term safe use of these drugs has never been established.
Hmmm. I hope this is cause for pause. It’s true we don’t want GERD or indigestion, yet it remains ubiquitous. The prevalence of at least weekly GERD symptoms in the US is approximately 20% (El-Serag et al., 2014) with an overall prevalence estimated up to 30% in the US (Eusebi et al., 2017). This prevalence of GERD is deemed “exceedingly common”, ranking as the most frequent gastrointestinal diagnosis associated with outpatient clinic visits in the US (Richter, 2018). For as frequently as I see these drugs listed on patient intake forms - or forgotten to be listed since it is such a part of one’s routine - I feel strongly that we are dealing with an epidemic I call “indigestion nation”.
Instead of blaming our stomach acid, it’s time for us to look at the other side of the issue and ask why. Why are so many struggling with digestion? And is there a better way to get a handle on this under-appreciated situation?
Next question: how often is nutrition or food digestibility considered in scenarios involving GERD symptoms, GI upset, or indigestion?
When I ask my patients about this, the standard answer prevails: they try their best to avoid known triggers including fried and spicy foods. Beyond that, there is little forward thinking in terms of where our collective indigestion originates.
Further, how many healthcare providers or patients contemplate what long-term acid suppression might look like?
- Isn’t our stomach SUPPOSED to be acidic? (Answer: it is)
- What happens if it isn’t? (Answer: lots of undesirable things)
- From there, we begin connecting the dots to find points of clarity.
In order to digest proteins, our stomach has to be acidic. The acid in the stomach also kills or deactivates harmful viruses and bacteria that could otherwise gain access to the rest of our system via the intestinal barrier. And our standard American diet does not include foods that contain important bioactive compounds and enzymes that take some of the burden of digestion off our plate – or rather our stomach, intestines, and accessory digestive organs. These are not frequently discussed principles of digestion.
We are conditioned to seek the quick fixes to our digestive woes. Woes that have increased in prevalence in North America by approximately 50%, relative to the baseline prevalence in the early to middle 1990s (Richter, 2018). Our go-to quick (Tums and Rolaids) and long-term strategies (Pepcid AC) are not without consequences. And I’m not even referring to the recently elucidated serious issue of the H-2 blocker ranitidine (generic Zantac) containing N-nitrosodimethylamine (NDMA)….a probable human carcinogen (Mahase, 2019).
Facts like these will sometimes get us to take notice. However, the more pervasive problem is this: components of our diets have become so difficult to digest, so physiologically incompatible with us, that we forget to examine this issue through such a simple lens. If our diet consists of foods that are difficult to break down or contain substances that can be disruptive to our digestive processes, it’s no surprise our body may reject them or be unable to digest them fully.
However, if our diet consists of foods that are designed for nourishment, naturally pre-digested and ready to assimilate or use by the body for building blocks and fuel, our body will know how to break them down and utilize them fully…..miraculously reducing the digestive burden and improving symptoms of GI distress including GERD and indigestion.
It sounds simple enough.
But in this day and age, the savvy healthcare provider will do well to learn and appreciate the breadth and depth of this concept and what it means to you as both a consumer of food and one who cares for others who consume food - all of us. This understanding - especially for a pelvic rehab provider- is critical to harness.
From simple but nuanced concepts, one can help prompt remarkable changes. I’ve seen it firsthand innumerable times.
I invite each of you to learn more about this fascinating topic and how it interrelates with so many facets of our health. Take advantage of the multiple remote-course offerings of Nutrition Perspectives for the Pelvic Rehab Therapist in 2024 - February 24-25, April 27-28, June 8-9, and December 7-8.
References:
- Richter, J. E., & Rubenstein, J. H. (2018). Presentation and Epidemiology of Gastroesophageal Reflux Disease. Gastroenterology, 154(2), 267-276. doi:10.1053/j.gastro.2017.07.045
- Eusebi LH, Ratnakumaran R, Yuan Y, et al. Global prevalence of, and risk factors for, gastro- oesophageal reflux symptoms: a meta-analysis. Gut. 2017
- El-Serag HB, Sweet S, Winchester CC, et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014; 63(6):871– [PubMed: 23853213]
- Mahase, E. (2019). FDA recalls ranitidine medicines over potential cancer causing impurity. BMJ, 367, l5832. doi:10.1136/bmj.l5832

HW is excited to announce the addition of a brand-new course to our Pelvic Function (PF) Series!
Pelvic Function Level 2C (PF2C): the Male Pelvic Floor and Men’s Pelvic Health
Formerly the stand-alone course, Male Pelvic Floor Function Dysfunction and Treatment, this course is now being adapted and reformatted to be a part of the PF Series, reflecting the inclusive stance of H&W core series instructing in the care of all patients. This course is intended for the pelvic health clinician who treats patients with conditions including post-prostatectomy urinary incontinence, erectile dysfunction, and chronic pelvic pain (CPP).
This course will be offered as satellite, self-hosted, and in-person options in order to provide the most flexible pathway for participants.
It is a reality of our field that pelvic rehab evolved from a tradition of “women’s health physical therapy”, and that is reflected in the prior vulvovaginal emphasis of the existing coursework. As the scope of pelvic rehab has expanded to encompass men’s health and care for all genders, it is important that all pelvises be incorporated at every level of our series, and that men’s health be a foundational part of our curricula, rather than being siloed as a specialty offering.
It is now our expectation that providers who want to care for patients around topics provided in the men’s health course will now take our introductory course, Pelvic Function 1. This is a necessary change reflecting growth and progression of our field of pelvic healthcare. Over the years, it was helpful to offer a course focusing on post-prostatectomy dysfunction, pelvic and genital pain and sexual health and function that was open to all levels. However, while participants who took the former Male Pelvic Floor course developed competence in the instructed skills, by missing the rest of the series, foundational conversations including physiology of urinary function, discussion of trauma-aware care, and bowel health basics that often affect other pelvic functions were abbreviated. Including men’s health within the rest of the foundational series resolves the missed content from our foundational course. Attendees to our PF1 course will find that it has been elevated to be a more inclusive course that covers information about pelvic health which will allow a beginning pelvic health practitioner to immediately apply introductory principles of care to all genders.
More questions about changes to the PF series? Please see this FAQ page: https://hermanwallace.com/frequently-asked-questions#2024-PF-Series-Update