- Do you work with postpartum patients and wish you could help them recover more quickly in the postpartum time period?
Do you work with pelvic pain patients who have sacroiliac joint pain?
Do you work with patients that have a weak core?
Rehabilitative ultrasound imaging is a tool that is very helpful for the clinician to assess motor control and muscle morphology. It is also very helpful as a biofeedback tool for patients trying to improve their pelvic floor or core strength.
In an article published in 2021, researchers performed a systematic review of the efficacy of rehabilitative ultrasound imaging for improving motor control exercises compared to no feedback and other feedback methods. Studies included in the systematic review assessed the abdominal wall muscles, pelvic floor, serratus anterior, and/or lumbar multifidus. What they found was that rehabilitative ultrasound imaging was more effective than tactile and verbal biofeedback for motor control exercise performance. Patients using ultrasound imaging demonstrated increased muscle activity, muscle thickness, and target exercise success compared to tactile and verbal biofeedback. Additionally, longer retention was noted when ultrasound imaging was used. Having constant feedback by watching the monitor of the ultrasound while performing an exercise compared to feedback after performing an exercise showed superior motor learning long-term (Valera-Calero, 2021).
Using ultrasound is a marketing tool and something that will enhance your clinical offerings. Patients enjoy using this biofeedback method! When asked what they thought of the use of ultrasound, this is how a few patients responded:
- “Using the ultrasound has helped me to learn to use my deep core muscles. This has helped me to recover from back pain after having twins. I am a radiologist and Allison's use of ultrasound in therapy was very unique for me and made the difference between getting better and living with pain.” (RK, 39 years)
- "I loved using ultrasound to view my pelvic floor muscles to help with my incontinence. It was so easy and made therapy kind of fun. I highly recommend using ultrasound.” (AJ, 65 years)
- “My doctor told me to get on the waitlist for therapy using ultrasound instead of going elsewhere. He was right, it was totally worth it! I have tried therapy several times before but this time, I feel I am actually getting stronger and better!” (MK, 29 years)
 Learn to use rehabilitative ultrasound in your practice and take the course with Herman & Wallace. Rehabilitative Ultrasound Imaging: Pelvic Health and Orthopedic Topics is offered at multiple locations. If you have a US machine with a curvilinear transducer that images a frequency that ranges from 3 to 10 MHz and is capable of abdominal viewing then you can also register as a "Self-hosted" attendee. This course is offered in a two-day option (Orthopedic Topics) with external labs, and a three-day option (Pelvic Health & Orthopedic Topics) that includes transperineal labs.
Learn to use rehabilitative ultrasound in your practice and take the course with Herman & Wallace. Rehabilitative Ultrasound Imaging: Pelvic Health and Orthopedic Topics is offered at multiple locations. If you have a US machine with a curvilinear transducer that images a frequency that ranges from 3 to 10 MHz and is capable of abdominal viewing then you can also register as a "Self-hosted" attendee. This course is offered in a two-day option (Orthopedic Topics) with external labs, and a three-day option (Pelvic Health & Orthopedic Topics) that includes transperineal labs.
Join us to learn how to use this great clinical tool!
Rehabilitative Ultrasound Imaging: Orthopedic Topics - Satellite Lab Course - October 25-26, 2024
Rehabilitative Ultrasound Imaging: Pelvic Health & Orthopedic Topics - Satellite Lab Course - October 25-27, 2024
Reference:
Valera-Calero JA, Fernández-de-Las-Peñas C, Varol U, Ortega-Santiago R, Gallego-Sendarrubias GM, Arias-Buría JL.(2021). Ultrasound Imaging as a Visual Biofeedback Tool in Rehabilitation: An Updated Systematic Review. Int J Environ Res Public Health. 18(14):7554. doi: 10.3390/ijerph18147554. PMID: 34300002; PMCID: PMC8305734.
AUTHOR BIO:
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.
An Ancient Science with a Modern Evidence-Based Approach
A 15-year-old patient walked into the clinic with her mom presenting with symptoms of constipation, lower abdominal spasms, and pain with bowel movements. Over the course of the visit, I learned that she was on medication for depression and was also suffering from chronic anxiety. Anxiety pervaded every aspect of her life, from things happening during the day to her near and far future. Her symptoms were worse when her anxiety was high and she struggled to relax her body and mind.
So, in addition to teaching her a program with breathing exercises, self-abdominal massage, pelvic girdle stretching, and the use of a squatty potty, I also taught her perineal self-acupressure at the acupoint Central Vessel 1 (CV 1) for constipation and two self-regulation points Central Vessel 17 (CV 17) and Yintang (EX-HN 3) for alleviating her anxiety.
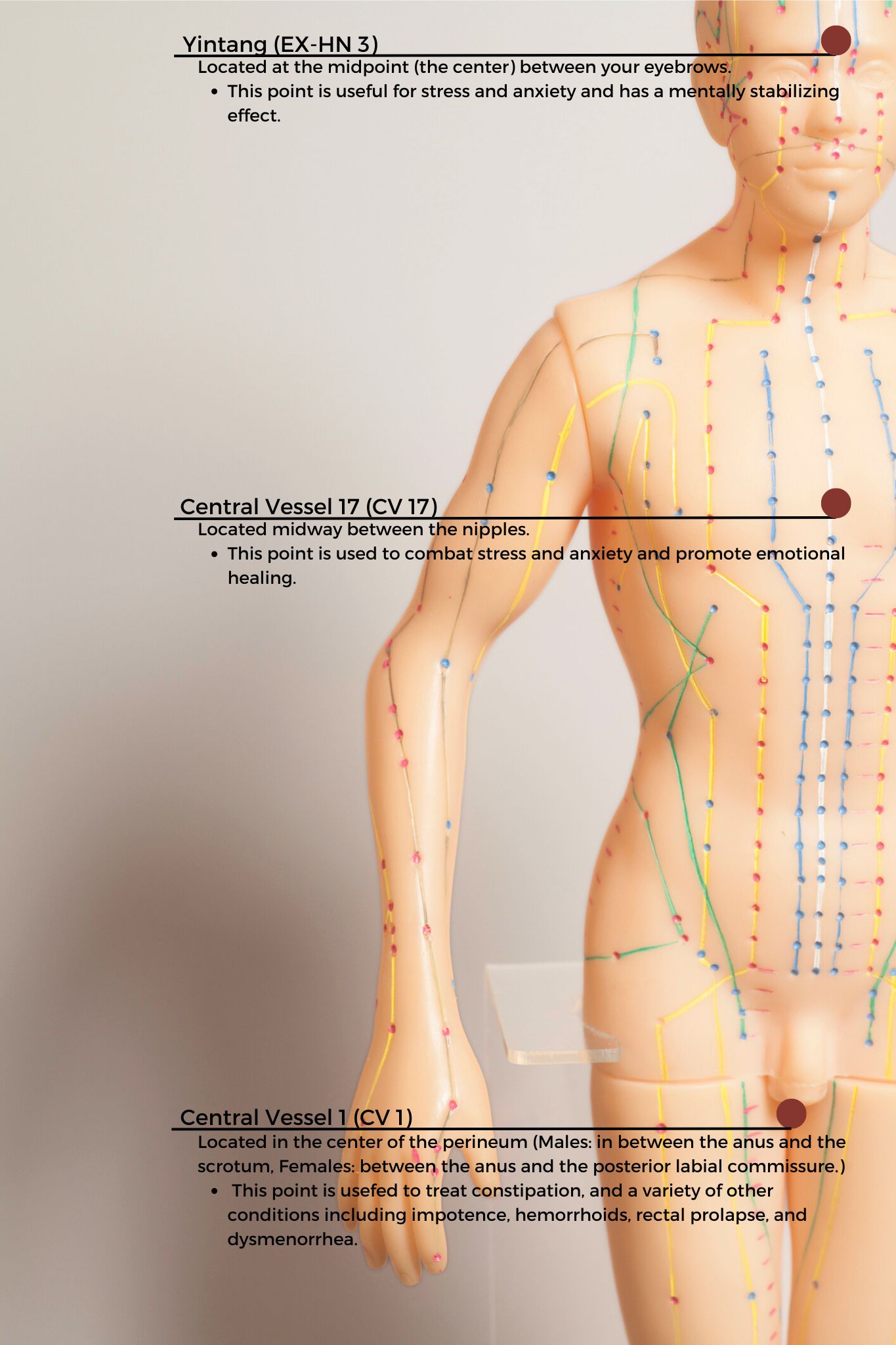 CV1 also known as Huiyin is located at the perineum. A study by Abbott et al. reported that the perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. CV17 is located at the center of the chest and is known to be a point for emotional healing while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM).
CV1 also known as Huiyin is located at the perineum. A study by Abbott et al. reported that the perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. CV17 is located at the center of the chest and is known to be a point for emotional healing while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM).
The patient returned the next visit and reported that her abdominal spasms were 50% better and she no longer had pain with bowel movements. She also reported that she felt calmer and was able to use the perineal self-acupressure technique to evacuate very quickly. Over the past several years, I have found that adding Acupressure to my clinical practice has added so much value as an Integrative holistic tool to complement traditional care.
Evidence-based Integrative health and medicine practices blend traditional physical therapy methods with holistic practices that address the whole person-physically, mentally, emotionally, and spiritually (Justice et al). Acupressure is considered an Integrative medicine practice and is based on traditional Chinese meridian theory in which acupuncture points are pressed to stimulate the flow of energy or Qi. Acupuncture meridians are believed to form a network throughout the body, connecting peripheral tissues to each other and to the central viscera. This tissue network is also continuous with more specialized connective tissues such as periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (Kaptchuk).
There is robust scientific evidence supporting acupressure as an effective non-pharmacological therapy for the management of a host of conditions such as anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions to name a few.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety (Monson et al).
To learn more about Acupressure, join the upcoming remote course Acupressure for Optimal Pelvic Health scheduled for October 12th-13th. This course introduces practitioners to the basics of traditional Chinese medicine (TCM), acupuncture & acupressure, and provides an introduction to Yin yoga. Of the 12 major Meridians or energy channels, the focus is on the majority of acupoints in the Bladder, Kidney, Stomach, and Spleen meridians. In addition, there are other important meridian points that stimulate the nervous system and can be used for self-regulation, improving the flow of Qi the life force energy to improve the physiological functioning of the organs. The course also explores Yin poses within each meridian to channelize energy through neurodynamic pathways with powerful integrative applications across multiple systems. If you are not able to attend the October course date, then check out the website for the options scheduled for 2025.
References
- Chen SR, Hou WH, Lai JN, Kwong JSW, Lin PC. Effects of Acupressure on Anxiety: A Systematic Review and Meta-Analysis. J Integr Complement Med. 2022;28(1):25-35. doi:10.1089/jicm.2020.0256
- Abbott R, Ayres I, Hui E, Hui KK. Effect of perineal self-acupressure on constipation: a randomized controlled trial. J Gen Intern Med. 2015;30(4):434-439.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.
- Justice C, Sullivan MB, Van Demark CB, Davis CM, Erb M. Guiding Principles for the Practice of Integrative Physical Therapy. Phys Ther. 2023;103(12):pzad138. doi:10.1093/ptj/pzad138
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Abaraogu UO, Igwe SE, Tabansi-Ochiogu CS. Effectiveness of SP6 (Sanyinjiao) acupressure for relief of primary dysmenorrhea symptoms: A systematic review with meta- and sensitivity analyses. Complement Ther Clin Pract. 2016;25:92-105
- He Y, Guo X, May BH, et al. Clinical Evidence for Association of Acupuncture and Acupressure With Improved Cancer Pain: A Systematic Review and Meta-Analysis. JAMA Oncol. 2020;6(2):271-278. doi:10.1001/jamaoncol.2019.5233
AUTHOR BIO
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
 Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna currently practices in an outpatient setting. The majority of her clinical orthopedic practice has focused on treating musculoskeletal, neurological, pre- and post-operative surgical conditions to name a few. She specializes in working with pelvic health patients who have bowel & bladder issues with high pelvic pain which sparked her interest in Eastern holistic healing traditions and complementary medicine. She has spent many hours training in holistic healing workshops with teachers based worldwide. She is a member of the American Physical Therapy Association and a member of APTA’s Academy of Orthopaedic Physical Therapy and Academy of Pelvic Health Physical Therapy.
Rachna also owns TeachPhysio, a PT education and management consulting company. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
If you’ve spent any time on social media as a healthcare practitioner, you’ve probably encountered a flood of ads promoting shockwave therapy as a miracle solution for everything from orthopedic pain to urological and gynecological conditions. The marketing push for these devices has skyrocketed over the past five years, driven by claims of its ability to treat a wide range of diagnoses. Recent research, including a comprehensive review published in The Journal of Clinical Medicine, confirms that shockwave therapy is making significant waves in modern medicine. But with all the buzz surrounding this technology, the real question remains: is it truly a game changer for patients and clinics alike?
As a medical professional, my approach to any new treatment, procedure, or modality begins with skepticism. I believe it is my responsibility to ensure that the interventions I offer in my clinic are grounded in solid research, and proven efficacy. When I first encountered shockwave therapy in early 2020, I was highly skeptical. The companies I spoke with made sweeping claims, portraying shockwave therapy as a universal solution for virtually every condition. Despite their promises, I remained cautious. However, after hearing positive feedback from a few trusted colleagues and witnessing a session that yielded seemingly impressive results, I decided to delve deeper into the research.
I found that while there is a substantial amount of literature available, much of it is confusing and, it lacks clarity — especially in the area of pelvic health. The majority of the research outside of orthopedics focuses on conditions such as erectile dysfunction, with little attention given to men’s pelvic health concerns and even less given to women’s pelvic health issues.
Recent advances in shockwave therapy have highlighted its growing potential in the field of men's and women’s sexual and pelvic health. The latest research trends are clear. As a non-invasive treatment, shockwave is no longer considered solely beneficial for orthopedics and sports medicine. Its applications are expanding rapidly in gynecology, urology, and pelvic floor disorders. This shift is driven by the therapy’s ability to enhance blood flow immediately and provide significant pain relief faster than traditional methods, making it an innovative option for conditions such as chronic pelvic pain, dyspareunia, and vaginal atrophy.
However beneficial, the fact remains that confusion abounds when, as a clinician, you are deciding which device would be best for your patients. At the forefront of the confusion when you delve into the research are:
- protocols vary substantially between devices
- energy levels and units of measure aren’t consistent among devices,
- There are popular devices in the research labeled shockwave, when in fact, they do not produce shockwaves and create different outcomes.
If you would like to learn more about incorporating shockwave therapy into your daily practice, register for my one-day remote course Shockwave Treatment: Therapeutic Interventions in Pelvic Health & Demystifying the Research scheduled for October 22, 2024. This course provides an introduction to using this cutting-edge technology in the clinic for improved patient outcomes and an understanding of how shockwave can enhance manual therapy treatment skills. Course lectures cover what is shockwave, how it decreases pain and potentially accelerates healing, the research behind it, the different types of shockwave devices, and the best indications of use for each of them as well as case studies discussing patient protocols and outcomes.
AUTHOR BIO
Stacey Roberts, PT, RN, MSN

Stacey Roberts, PT, RN, MSN (she/her), has been a physical therapist specializing in outpatient orthopedics and sports medicine, since 1990. After completing a sports medicine fellowship and working at several hospitals and outpatient clinics, in 2000 Stacey had an opportunity to move overseas, where she became adept with complementary medicine approaches, becoming a master in herbalism in 2003. From 2004 to 2017, Ms. Roberts owned and operated a cash-based health and wellness clinic on the Gold Coast of Australia specializing in women’s health and hormones and couples' fertility, where she began seeing patients via Telehealth in 2006.
Combining her knowledge of functional medicine, conventional medicine, and complementary medicine, Stacey emphasizes lifestyle changes, and her treatment programs are based on cutting-edge evidence-based research. Currently, she is a co-principle investigator for an IRB-approved study related to shockwave and Dyspareunia.
She has written 3 hard-copy books and 7 ebooks on women’s health and couples' fertility. Her new book, The Pain-Free Formula: A Holistic Approach to Finally Getting Rid of Pain Without Surgery, Drugs, Or Injections, is coming out in 2025. Ms. Roberts has mentored over 100 medical professionals in her women’s health and couples fertility training program. After returning to the United States, Stacey was hired by a national physical therapy company, Aegis Therapies, from 2018 to 2020 to assist in the growth and development of their orthopedic outpatient practice in Wisconsin. She set records for the company related to bringing clinics to profitability faster than any of their other outpatient clinics in the country at that time.
From 2016- to 2020 Stacey was an associate clinical professor at the University of Wisconsin Milwaukee’s Physical Therapy doctoral program until opening New You Health and Wellness, a cash-based clinic, where she brings her knowledge of wellness, hormone health, fat loss, and musculoskeletal health to treating patients with issues related to musculoskeletal injuries, sexual health, and pelvic health. Since 2020 she has been analyzing Shockwave research extensively to develop clear and concise therapeutic applications and protocols for pelvic health, sexual health, and muscular-skeletal patients. She is finding extraordinary results with her patients using this modality in her cash-based practice.
Stacey completed her MBA in 2021, her RN license, and her master’s in nursing (MSN) in 2020. She will eventually complete a nurse practitioner certificate. Stacey has also appeared on World News Now in New York, was featured on Oprah, locally on TMJ4’s Morning Blend, and on several news shows and radio stations in the United States and Australia.

September is Ovarian Cancer Awareness Month. Ovarian cancer is the seventh most common type of malignant neoplasm in women and the eighth cause of mortality for women (Gaona-Luviano et al, 2020). In women who have died from gynecological cancers, ovarian cancer is the leading cause of death (Arora et al., 2021). This type of cancer can originate from any of the ovary's three main components, including the epithelium, stroma, and germinal cells. Per Gaona-Luviano et al., 2020, “epidemiology of this cancer shows differences between races and countries due to several factors including genetic and economic.” Detection of ovarian cancer is problematic because there is no standardized screening process and most cases of ovarian cancer are found in the advanced stages (Gaona-Luviano et al, 2020).
How is ovarian cancer diagnosed?
Sadly, the existing screening tests have a low predictive value. A gynecological evaluation, transvaginal ultrasound, and tumor marker testing (cancer antigen-125/CA-125 assay) can help with early detection strategies but this has not shown a significant effect on the morbidity or mortality of this cancer (Arora et al., 2021).
How is ovarian cancer treated medically?
Research shows that the standard line of care treatment includes surgery and platinum-based chemotherapy. Additional options including anti-angiogenic bevacizumab and Poly(ADP-ribose) polymerase (PARP) inhibitors have also been used more recently. (Arora et al., 2021)
What are the outcomes of an ovarian cancer diagnosis?
There is a high rate of recurrence after the initial detection treatment. Many of the cases re-occurred and these secondary cases were less curable with increased incidence of treatment failures (Arora et al., 2021).
What are ovarian cancer risk factors?
Some risk factors include advanced age, early menarche, late menopause, family history, nulliparity, obesity, perineal talc use, smoking, endometriosis, and hormone replacement therapy (Arora et al., 2021). Some protective factors include oral contraceptives, bilateral tubal ligation or salpingectomy, breastfeeding, and multiparity (Arora et al., 2021).
Some research shows there may be some health disparities in the diagnoses between Non-Hispanic Black women compared to Non-Hispanic White women. In a study by Washington et al. in 2023 53,367 women were included in the analysis with the profile being 82% Non-Hispanic White, 8.7% Non-Hispanic Black, 5.7% Hispanic, and 2.7% Non-Hispanic Asian/Pacific Islander. They found that the Non-Hispanic Black race was associated with a higher risk of death than Non-Hispanic White race and Non-Hispanic Black women versus Non-Hispanic White women had an increased risk of mortality among those with low and mid socioeconomic status groups.
In response to this potential inequity, the National Cancer Institute has launched 3 studies to look at these patterns to “better understand the causes of racial and ethnic disparities among women with ovarian cancer.” These studies will examine whether the treatments with these patient populations were consistent with standard clinical guidelines and ensure all patients received quality care. Additional studies will look at a “cells-to-society approach” to assess the biology behind these trends. In both cases, the researchers will assess a range of potential factors that can affect disparities, from the molecular makeup of tumors to environmental factors, and comorbidities (NCI, 2024).
What can pelvic health providers do to help?
As pelvic health providers, we can educate ourselves on how best to screen and refer our patients to ensure early diagnosis and medical treatment if we hear anything suspicious. It is difficult to self-advocate in this current medical climate and having a skilled provider guiding the questions to ask and the support to seek is invaluable. If a patient is already into their treatment journey, we can provide the needed rehabilitation support including things like coordination and strengthening of the core and pelvic floor, stretching and positioning to lengthen tight areas, scar mobilization, patient education, and symptom management with the patient for any symptoms that may pop up throughout their course of care.
If you’re unsure that you have these skills in your skill set, please check out the Oncology of the Pelvic Floor Series to gain more knowledge and experience in these areas to better help patients with these diagnoses. Certified Lymphatic Therapists may skip this course and move on to the level Oncology of the Pelvic Floor Level 2A and Level 2B courses.
- Oncology of the Pelvic Floor Level 1, next scheduled for November 2-3, 2024, is the first course in the series and focuses on topics that prepare practitioners to be part of the interdisciplinary oncology team. Topics will include the basics of cancer: terminology, staging, medical treatment, and the sequelae of these medical treatments. These topics include the lymphatic system as well as issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis.
- Oncology of the Pelvic Floor Level 2A, (not yet scheduled for 2025), builds on information presented in Oncology of the Pelvic Floor Level 1 and focuses on male pelvic cancers (prostate cancer, penile cancer, and testicular cancer), colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. Topics discussed include sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life, rehabilitation, and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy. Participants MUST register with a partner, or plan to have a volunteer available to work on during course labs.
- Oncology of the Pelvic Floor Level 2B, next scheduled for December 7-8, 2024, builds on information presented in Oncology of the Pelvic Floor Level 1 and focuses on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. Topics discussed include sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life, rehabilitation, and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy. Participants MUST register with a partner, or plan to have a volunteer available to work on during course labs.
References:
- Arora, T., Mullangi, S., & Lekkala, M. R. (2021). Ovarian cancer.
- Gaona-Luviano, P., Medina-Gaona, L. A., & Magaña-Pérez, K. (2020). Epidemiology of ovarian cancer. Chinese Clinical Oncology, 9(4), 47-47.
- NCI. Ovarian cancer studies aim to reduce racial disparities. Ovarian Cancer Studies Aim to Reduce Racial Disparities - NCI. (2024, June). https://www.cancer.gov/news-events/cancer-currents-blog/2020/ovarian-cancer-racial-disparities-studies#:~:text=Credit:%20iStock,impeded%20research%20in%20this%20area.
- Washington, C. J., Karanth, S. D., Wheeler, M., Aduse-Poku, L., Braithwaite, D., & Akinyemiju, T. F. (2024). Racial and socioeconomic disparities in survival among women with advanced-stage ovarian cancer who received systemic therapy. Cancer Causes & Control, 35(3), 487-496.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much she has not treated since beginning this journey and she is always happy to further her education to better help her patients meet their goals.
She strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, She opened her own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.

If you saw Ethical Considerations for Pediatric Pelvic Health and thought “Why are they making ANOTHER ethics class?” please let me take a moment to explain its origin and purpose in the Herman and Wallace course offerings. I wrote my Pediatric Pelvic Floor Play Skills course when I had colleagues asking for ways to play with their patients. When I started teaching this class, some of the most common questions that came up seemed like ETHICAL questions. How do we handle pediatric care in different settings? How do we get consent from minors? If a child says no but their legal guardian wants the assessment done, what does the provider do?
Pediatric Pelvic Floor Play Skills is a class written to help providers take the pelvic health knowledge they have, and learn activities they can perform with different ages of children to help work on their pelvic floor function. One of the tricky parts of working with children is including the child in their care plan and coordinating with caregivers. In this course, talk about specific concerns and considerations by age, as well as strategies to bring to a provider's practice. This class is for the provider who does not have a lot of experience treating pediatric patients and wants to learn how to make sessions enjoyable and effective. While in Ethical Considerations for Pediatric Pelvic Health, we review the different overall milestones, as well as what age-appropriate expressions of sexuality may look like as children develop toward adulthood.
Let's talk about Pediatric Care
When we say “pediatric” this can span from infants to teenage age groups. Dealing with a crying baby will be different decision-making versus a toddler in a tantrum or a defiant teen. The pediatric population is a vulnerable group because they can’t advocate for themselves, their own interests, and their health to protect themselves from harm. When we consider decision-making with a child, a therapist should consider things like their development, family structure, competence, and education levels. Children develop in a variety of areas including their fine and gross motor skills, language, cognitive, social, emotional, and behavior.
In pediatric care, obtaining informed consent has two parts because it requires therapists to secure consent from caregivers and to seek assent from the child. Once they have obtained the parent’s permission, therapists should explain the procedures, potential benefits, and risks in an age-appropriate manner to the child. Therapists have to make sure the child feels comfortable and involved in their care at each step.
Pelvic health providers should establish clear guidelines about what information will be shared with caregivers and what will remain confidential when working with children, especially tweens and teens. This helps the therapist to build trust with the patient and encourages open communication with the patient. We must also consider what the caregivers are entitled to hear about their child’s life and medical care. For example, if a tween wants to talk to you about sex, do you feel equipped with the ethical implications for yourself in your practice? What about if a child discloses a sexual assault at school? What about if a teenager tells you they are pregnant but hasn’t told their parents? This class will give some guidelines to make these decisions and provide a peer “think tank” to further discuss.
One of the easiest ways to be an effective pediatric provider includes communication with the patient and their support system. Make sure to review topics like the condition, treatment options, and expected outcomes to empower them to make informed decisions. Keep your communication clear and provide educational materials that are accessible and understandable. Make sure to check with caregivers about what words and pictures they are comfortable with the child seeing and hearing. Some children or caregivers may have personal, religious, or cultural implications that may limit what education they want the child to be exposed to.
Every child is unique, and their treatment should reflect their individual needs, preferences, and circumstances. Therapists should listen to the child and their support network, and incorporate their feedback into the plan of care. Consider their life and routine to make sure their care and homework fit into their daily schedule. Advocating for the needs and rights of pediatric patients is a critical aspect of ethical care. Therapists may need to recommend resources, treatments, and accommodations, and promote awareness and education about pediatric pelvic health issues within the broader community. This may include coordinating with a child’s daycare, school, or other medical providers.
What course is right for you?
- Ethical Considerations for Pediatric Pelvic Health on October 13th - Learn more about the ethical challenges pediatric pelvic health practitioners may experience including consent, managing situations of trauma and abuse, and managing autonomy for minors. If you work with pediatric patients on a regular basis, this class can be an additional step in your practice. It will review topics like consent, abuse, education, communication, and diagnoses that tend to have more ethical considerations with pediatric patients. Join us to review background information and then discuss, as a group, different cases and ethical situations to help further your pediatric clinical practice.
- Pediatric Pelvic Floor Play Skills on October 20th - This is a beginner-level course and is a good fit for providers who do not have a lot of experience treating pediatric patients and want to learn how to make sessions enjoyable and effective. In this course, we discuss specific concerns and considerations by age, strategies to bring to a provider's practice, sample home programs, equipment purchase lists (with a budget in mind), tips for helping get families on board with the implementation of care, and resources such as outcomes measures, developmental milestone checklists, and recommendations things parents ask for like how to talk about periods and sex.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC
 I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.
Dawn Sandalcidi will be a keynote speaker at HWConnect 2025 on March 28-30, 2025. You can also join her in upcoming courses: Pediatric Pelvic Floor, Diaphragm, and Postural Development: Intro to Core Function and Continence in Children on September 29th, Pediatrics Level 1 -Treatment of Bowel and Bladder Disorders on October 26-27, or Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders on November 2-3.
As physical and occupational therapists, we aim to provide the best possible care for our young patients by understanding and addressing the underlying mechanisms affecting their health. The diaphragm is one of the most important yet often overlooked structures. This muscle plays critical roles in both respiratory and postural functions and has far-reaching implications for the stability and health of children.
In this blog, we’ll explore the anatomy, function, and clinical relevance of the diaphragm, its connections to the pelvic floor muscles, and the broader implications for pediatric therapy.
Anatomy Of The Diaphragm

In order to appreciate the functions that the diaphragm plays in breathing and movement, you must first understand the anatomy. The diaphragm is the thin, dome-shaped muscle that separates the thoracic and abdominal cavities. Its structure is divided into two primary components:
- The Crural (Vertebral) Portion: The crural portion, or muscular “legs” of the diaphragm, originates from vertebrae of the lumbar spine, providing stability and anchoring the diaphragm in place.
- The Costal Portion: The costal portion originates from the xiphoid process of the sternum and the upper margins of the lower rib pairs.
At the center of the diaphragm lies the “central tendon”, the non-muscular aponeurosis at which the muscular fibers converge. This tendon acts as a pivotal point during the contraction of the diaphragm.
When the diaphragm contracts during inspiration, the dome of the diaphragm descends, shortening the muscle fibers and increasing the volume of the thoracic cavity. This action decreases intrapleural pressure, allowing the lungs to expand and fill with air. At the same time, abdominal pressure increases as the diaphragm displaces the rib cage and moves downward.
The relationship between the diaphragm and the rib cage is vital for effective breathing and functional movement. Keep this in mind when working with kids who have low tone or poor strength. Breathing mechanics and diaphragm optimization are essential to assess. Proper contraction of the diaphragm not only facilitates lung expansion but also ensures that the core and extremities are stabilized, leading to efficient and stable movement patterns.
Let’s take a closer look at these functional connections.
The Diaphragm’s Connections To Posture And Pelvic Floor

A critical concept in understanding the diaphragm’s function is the Zone of Apposition (ZOA). The ZOA is the vertical area of the diaphragm that extends from the inside of the lower ribs to the top of the diaphragm. This zone maintains the diaphragm's dome shape, which is important for effective breathing.
When the ZOA is well-maintained, the diaphragm can contract efficiently without the need for accessory muscle recruitment. This efficiency prevents compensatory breathing patterns that can lead to respiratory and postural issues.
Conversely, a decreased ZOA can result in poor diaphragm contraction, leading to inefficient breathing and overuse of accessory muscles. Musculoskeletal effects on posture can include issues such as:
- Anterior rib flare
- Lung hyperinflation
- Hyperlordosis
- Protruding abdomen
- Weakness of the anterior core muscles with poor pressure system management
The diaphragm works in close coordination with the pelvic floor muscles (PFM) and the abdominal muscles. This interaction is vital for managing intra-abdominal pressure (IAP) and maintaining stability in both the thoracic and abdominal cavities when breathing.
- During inspiration, the diaphragm descends, causing an eccentric lengthening of the abdominals and the PFM, which stabilizes the core.
- During exhalation, the diaphragm relaxes and ascends, while the abdominals and PFM contract concentrically.
This basic overview of the diaphragm's connections is expanded upon in my live online course, Pediatric Pelvic Floor Diaphragm and Postural Development, where I delve deeper into how these relationships impact children with pelvic floor issues like constipation, diastasis rectus, and even cystic fibrosis.
The diaphragm, in coordination with the abdominal muscles and the PFM, helps to stabilize the spine and pelvis during movement. This stabilization is essential for maintaining balance and posture when learning developmental motor skills.
This coordination also ensures that pressure within the thoracic and abdominal cavities is managed effectively, influencing respiratory capacity and lymphatic drainage.
Furthermore, the fascial connections from the diaphragm establish healthy function of many organ systems. Let’s take a look at this in more detail, so you can understand how this directly affects your practice as a pediatric therapist.
The Diaphragm’s Fascial Connections To Organ Systems
 Beyond its muscular and respiratory functions, the diaphragm is also deeply interconnected with the body’s fascial system. Fascia surrounds every structure in the body, providing support and facilitating movement. Fascia has contractile properties, so a problem with the diaphragm or its related structures can cause dysfunction along the entire fascial chain.
Beyond its muscular and respiratory functions, the diaphragm is also deeply interconnected with the body’s fascial system. Fascia surrounds every structure in the body, providing support and facilitating movement. Fascia has contractile properties, so a problem with the diaphragm or its related structures can cause dysfunction along the entire fascial chain.
The diaphragm has direct fascial connections to several key organs, including:
- Heart
- Lungs
- Liver and Colon
- Esophagus
These fascial connections highlight the diaphragm’s role in managing information between the chest and abdomen, as well as its influence on organ function. When kids have dysfunction in their diaphragm or its associated fascial structures, this can lead to a range of issues, such as digestive, breathing, and swallowing problems.
The diaphragm also influences postural stability through its relationship with the glottis, which controls airflow through the vocal cords. Engagement of the glottis during upright perturbations or stability tasks enhances thoracic stability. The proper function of the glottis needs to be considered when working with kids on breathing mechanics, trunk stability, or pelvic floor engagement.
You must also look at neurological connections to the diaphragm, such as those involving the phrenic, vagus, trigeminal, and hypoglossal nerves. What many therapists often see as classic mechanical issues or classic digestive issues, can actually have distal neurological origins. This includes mechanical conditions such as headaches and thoracic outlet syndrome, and autonomic digestive conditions such as gastroesophageal reflux, aerophagia, and functional gastrointestinal disorders.
Get good at connecting the pieces and understanding the root causes of dysfunction, rather than simply treating the kids’ symptoms.
Clinical Implications For Pediatric Therapy
 For pediatric therapists, understanding the diaphragm’s role in respiration, postural stability, and its broader connections within the body is essential for effective treatment. Children with conditions such as cerebral palsy (CP), respiratory issues, constipation, and musculoskeletal pain can benefit significantly from interventions that target the diaphragm and its associated structures.
For pediatric therapists, understanding the diaphragm’s role in respiration, postural stability, and its broader connections within the body is essential for effective treatment. Children with conditions such as cerebral palsy (CP), respiratory issues, constipation, and musculoskeletal pain can benefit significantly from interventions that target the diaphragm and its associated structures.
For example, in children with CP, research has shown that kids with better diaphragmatic function exhibit greater ambulatory mobility, abdominal expansion, and respiratory function compared to kids with impaired diaphragmatic function. You should prioritize treatment of the diaphragm for children with CP, especially those who are non-ambulatory. [1]
Similarly, addressing diaphragmatic function can play a critical role in managing pediatric patients with respiratory conditions, such as asthma. Ensuring that the diaphragm maintains its dome shape and ZOA can improve the child’s breathing efficiency, reduce the reliance on accessory muscles, and enhance overall respiratory function.
Lastly, the diaphragm’s role in maintaining intra-abdominal pressure and coordinating with the pelvic floor muscles is crucial for managing conditions like constipation and urinary incontinence. By optimizing diaphragmatic function, you can support children’s pelvic floor function and help improve their bowel motility and urinary continence.
There are many widespread health implications that you have the power to influence as a pediatric therapist! If you are looking to deepen your understanding of the diaphragm and its role in pediatric health, join me virtually for my live Pediatric Pelvic Floor Diaphragm and Postural Development course on September 29, 2024.
This course will provide you with the knowledge and tools you need to enhance your practice and improve outcomes for your young patients. Don't miss this opportunity to expand your skill set and make a meaningful difference in the lives of the children you treat.
Reference:
- Bennett S, Siritaratiwat W, Tanrangka N, Bennett MJ, Kanpittaya J. Diaphragmatic mobility in children with spastic cerebral palsy and differing motor performance levels. Respir Physiol Neurobiol. 2019 Aug;266:163-170. doi: 10.1016/j.resp.2019.05.010. Epub 2019 May 21. PMID: 31125702.
AUTHOR BIO
Dawn Sandalcidi PT, RCMT, BCB-PMD
 Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn is a national and international speaker in the field, and she has gained so much from sharing experiences with her colleagues around the globe. In addition to lecturing internationally on pediatric bowel and bladder disorders, Dawn is also a faculty instructor at the Herman & Wallace Pelvic Rehab Institute. Additionally, she runs an online teaching and mentoring platform for parents and professionals.
In 2017, Dawn was invited to speak at the World Physical Therapy Conference in South Africa about pediatric pelvic floor dysfunction and incontinence. Dawn is also Board-Certified Biofeedback in Pelvic Muscle Dysfunction (BCB-PMD). She has also been published in the Journals of Urologic Nursing and Section of Women’s Health.
In 2018, Dawn was awarded the Elizabeth Noble Award by the American Physical Therapy Association Section on Women's Health for providing Extraordinary and Exemplary Service to the Field of Physical Therapy for Children.

Movement competence (or Movement Literacy) is defined as the development of sufficient skills to ensure successful performance in different physical activities. Often used in the world of sports and youth, it also applies to our everyday activities. For example, standing up from a chair or toilet, getting in/out of a car, moving our body from Point A to Point B (and the difference between the ground being even and dry vs uneven and icy).
In our course, Osteoporosis Management: An Introductory Course for Healthcare Professionals, Dr Frank Ciuba and I approach the starting point for individuals with low bone mass (osteopenia or osteoporosis), from an “optimal alignment position.” Patients start supine with hips and knees flexed and are educated on what optimal alignment feels like. Many need to be propped using pillows, towels, or blocks behind their heads, forearms, or between their knees to achieve “their optimal alignment.” Breathing and awareness play a huge role in activating core musculature to sustain this alignment when moving to a vertical position such as sitting or standing. In vertical, our weight-bearing forces and gravity should pass down through the skeleton to take advantage of bone-building benefits. We use dowel rods, broom handles, and walls to give feedback. Optimal alignment can and should be taught in a variety of positions: side-lying, prone, hands and knees, ½ kneeling as we move up the developmental chain.
Hip Hinging, a well-known concept by therapists, must be practiced and mastered for patients with low bone mass to reduce the risk of vertebral fractures. Activities that involve bending at the waist such as brushing teeth, making a bed, and putting dishes in the dishwasher all place the anterior portion of the vertebral bodies under pressure and increase fracture risk.
Advancing from static optimal alignment postures to dynamic optimal alignment is a whole different ballgame; akin to advancing from sitting in a car to driving a car. There are many moving parts - pun intended.
Just as in athletics, mastery comes from repetition. It is not enough to teach patients a safe movement pattern one time, hand them a sheet of paper with pictures, and expect them to be able to comply and gain competence. Reinforcing proper technique and helping them become aware of compensation strategies (hunching shoulders when lifting objects, overarching the back when reaching overhead, etc.) are critical if Movement Competency is to “stick.”
I like to think of movement competency as building a house. First, you need a firm foundation before putting up the walls and roof. Our patients require that foundation to be able to layer on more complicated patterns of movement.
Please join us for this one-day course on September 14th or November 2nd to learn more Osteoporosis-safe exercises, balance and gait activities, and additional ways to help your patients build a strong foundation for movement competence!
AUTHOR BIO:
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
Did you know that September is prostate cancer awareness month? As of 2020, prostate cancer is the most common cancer in men worldwide. Prostate cancer accounts for one in every 14 cancer diagnoses globally, and 15% of all cancers in patients born with a prostate. It ranks second in terms of cancer mortality in this population, second only to lung cancer.(1) A recent Lancet Commission on prostate cancer is projecting a significant increase in the number of new cases of prostate cancer annually. They are projecting that the number of new cases will rise from 1.4 million annually worldwide in 2020 to 2.9 million by 2040. This is due to changing age structures within the population and improved life expectancy.(1) This projected rise in prostate cancer cannot be prevented by lifestyle changes or public health interventions. Due to this projected increase in new cases, screening is a must and will be critical to better prognosis and survival for these patients. Along with a rise in prostate cancer, it is expected that other conditions such as diabetes and heart disease will mirror the projected increase in prostate cancer. It is recommended that screening and early diagnosis programs should not only focus on prostate cancer but “men’s health more broadly.”(1)
The Commission also recommended outreach programs to educate the population about prostate cancer. Social media and traditional media were both recommended to be used to reach individuals who may not be accessing medical care as frequently. This is something that we as rehabilitation clinicians can help with! As a rehabilitation clinician, we are expert educators for our patients. So much of what we do with patients is educate them about their bodies and things that can be done to assist in healing. We can take it a step further and educate them to have general health checks that would include screening for prostate cancer, among other screens such as for heart disease, and diabetes. We may also be able to reach other individuals by educating our patients to encourage their family and friends about the importance of general health screens. Many of us are also very adept at using social media to reach the community. Can we post something about Prostate Cancer Awareness Month? How easy is it to post a quick word about the expected rise in prostate cancer diagnoses and encourage patients to see their doctor for their annual health exam? Let’s all try to reach a few additional individuals this month in honor of Prostate Cancer Awareness Month! If we each are able to get a few more individuals in for screening, what impact could we make? This is something we should continue to do over the next several decades to encourage our patients to health screens! Mark your calendars every September to honor this month and educate our patients and their families!
To learn more about prostate cancer and how to treat this population, take Oncology of the Pelvic Floor Level 2A. This is an online course where you can learn specific techniques to help patients who have been diagnosed with pelvic cancers and colorectal cancers. It is offered September 7-8. Register today!
Reference:
- James N, Tannock I, N’Dow J, et al. (2024). The Lancet Commission on prostate cancer: planning for the surge in cases. The Lancet Commissions. 403(10437): P1683-1722. DOI:https://doi.org/10.1016/
S0140-6736(24)00651-2
AUTHOR BIO:
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.
Outside of work, Allison enjoys spending time with her family, caring for her animals, reading, traveling, and most importantly of all, being a mom! She lives in the Denver metro area with her family.
The Herman & Wallace course catalog does not include a pessary-focused course at the time of posting. Pelvic Organ Prolapse is discussed in Pelvic Function Level 1 and more in-depth in Pelvic Function Level 2B.
A pessary is a device that is placed in the vaginal canal to support the pelvic organs. They have been used by humans for millennia to treat pelvic organ prolapse (POP), being crafted of various materials from pomegranate to cork1. Most modern-day pessaries are made of silicone, although some medical pessaries are even engineered to release estrogen. Recent research suggests that combining pessary use with pelvic floor muscle training for treating POP may be even more effective than pelvic floor muscle training alone2.
A pessary can be worn only during an activity that typically provokes symptoms, such as running, or used almost continuously with periodic cleaning. People looking to avoid or delay pelvic organ prolapse surgery, such as those planning to give birth, may especially benefit from pessary use. Many transgender and nonbinary people with a front canal also find pessary use helpful for reducing POP symptoms.
Pessaries have additional benefits beyond improving prolapse symptoms. For example, some pessaries are designed to mitigate urinary incontinence by applying pressure to the urethra1. A 2024 study even indicated that they may improve sexual wellness in people with pelvic organ prolapse2. One case study series suggests that intersex people who have undergone vaginoplasty or neovaginoplasty may also benefit from pessary use for maintaining the patency of the canal5.
Traditionally in the United States, pessaries have been placed by medical professionals rather than rehabilitation professionals (although some PTs at the Veteran Affairs were involved in fitting pessaries under the guidance of urogynecologists). In 2021, the American Physical Therapy Association’s Academy of Pelvic Health convened a Pessary Task Force to look at the feasibility of physical therapists fitting and managing pessaries. In 2022, the Academy of Pelvic Health released its position statement to include pessary fitting and management in the scope of practice of pelvic health physical therapists in the United States and its five territories. By the end of 2022, the Academy of Pelvic Health hosted its first pessary fitting course. Several more courses have been offered since then.
If you are looking to include pessary fitting and management in your clinical toolkit, first check with your state physical therapy board to ensure that it is permitted where you practice. If your state does allow pessary fitting, select a class that ideally includes both didactic and lab-based coursework. Be aware that most will require a pelvic health fundamentals class with internal examination as a prerequisite. Once you have passed your pessary class, it will be important to maintain solid connections with advanced clinicians (i.e., trusted urogynecologists and gynecologists) who you can coordinate with on more complex cases, such as those that present with vaginal dermatoses or genitourinary syndrome of menopause.
Physical therapists specialize in showing clients how to tend and support their bodies. Active participation in pessary fitting and management is a way to help the nearly 40% of people with vaginal canals who are expected to develop pelvic organ prolapse7.
Note: The author does not currently know of any occupational therapists fitting pessaries in the United States, but they hope that this becomes a part of OT scope in the future.
References
- Shah SM, Sultan AH, Thakar R. The history and evolution of pessaries for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(2):170-175.
- Jin C, Yan H, Shang Y, et al. Real-world clinical effectiveness of nonsurgical treatments for female with POP-Q stage II cystocele: a retrospective analysis of therapeutic efficacy. Transl Androl Urol. 2024;13(4):483-492.
- Petter Rodrigues M, Bérubé MÈ, Charette M, McLean L. Conservative interventions for female exercise-induced urinary incontinence: a systematic review. BJU Int. Published online July 23, 2024.
- Nemeth Z, Vida P, Markovic P, Gubas P, Kovacs K, Farkas B. Long-term self-management of vaginal cube pessaries can improve sexual life in patients with pelvic organ prolapse, results from a secondary analysis. Int Urogynecol J. Published online August 5, 2024.
- Mensah V, Christianson MS, Yates M, Tobler K, Kolp LA. Novel use of a pessary to maintain vaginal patency following vaginoplasty or neovaginoplasty for mullerian anomalies or agenesis. Fertility and Sterility. 2013;99(3):S37.
- Wang B, Chen Y, Zhu X, et al. Global burden and trends of pelvic organ prolapse associated with aging women: An observational trend study from 1990 to 2019. Front Public Health. 2022;10:975829.
AUTHOR BIO
Ken McGee, PT, DPT
 Ken McGee, PT, DPT, (they/he) is a queer transmasculine pelvic health physical therapist based in Seattle. Their mission is to bring greater awareness to the pelvic health needs of the LGBTQIA2S community. They enjoy mentoring other rehabilitation professionals to better care for people of all genders.
Ken McGee, PT, DPT, (they/he) is a queer transmasculine pelvic health physical therapist based in Seattle. Their mission is to bring greater awareness to the pelvic health needs of the LGBTQIA2S community. They enjoy mentoring other rehabilitation professionals to better care for people of all genders.
Ken received their Doctor of Physical Therapy from the University of Washington in 2014 and their board certification as a Women’s Health Clinic Specialist (WCS) in 2018. Ken has lectured nationally and internationally on birth tears. Their practice, B3 Physical Therapy and Wellness, centers on transgender and perinatal rehabilitation. Ken also provides peer bodyfeeding support and doula care.
As musculoskeletal specialists, we are adept at identifying postural dysfunction. I often explain to patients how their ribcage might shift posteriorly relative to the plumb line and how gravity can amplify forces on specific structures. To help patients understand the difference between their habitual non-optimal posture and a more optimally aligned posture, many occupational and physical therapists use the IPA’s Vertical Compression Test (VCT). This test effectively demonstrates how improved alignment facilitates better weight transfer through the base of support. Sometimes this test reproduces back or pelvic pain which allows the patient to understand how their posture might be a contributing factor to them not feeling their best. In addition to the VCT, I incorporate Mountain Pose as an additional kinesthetic tool for postural retraining.
 Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
At our follow-up visit, the client noted an increase in her postural awareness. She was surprised by how frequently she noticed her pelvic floor gripping in a state of overactivity. She also reported enhanced awareness during her standing yoga postures in class. Grounding down through the feet, cued as imagining the soles of the feet getting magnetically drawn into the floor, can be a useful verbal cue to assist with letting go of unnecessary gripping. The experience of achieving embodied optimal alignment has given her greater self-efficacy, and she’s successfully translated this improved postural awareness into her daily life. Self-awareness and empowerment are central goals in my physical therapy practice, and integrating yoga into this process makes my clinical work even more fulfilling.
To learn more, join Dustienne in her remote course Yoga for Pelvic Pain this September 14-15! This course discusses a variety of pelvic conditions including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Dustienne also describes the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge in this course.
Author Bio:
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for Radio City Christmas Spectacular. She is an assistant professor of musical theater and jazz dance at the Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.