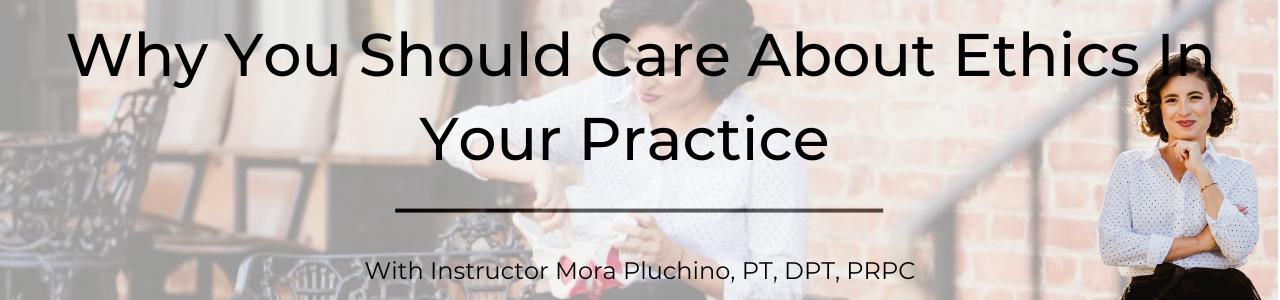
Mora Pluchino, PT, DPT, PRPC (Faculty member, and Sr. TA) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). Mora authored and instructs Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens.
When I used to hear the word “ethics requirement,” I would wrinkle my nose and find the cheapest, quickest course to fulfill my New Jersey requirement. I would sit through it and count down the hours. It was not out of a lack of respect for the continuing educator or the importance of the material. I just felt, no matter how the material was presented it was just dry and did not feel like it applied to my more niched areas of practice.
As I dove deeper into pelvic floor treatment and the pelvic floor community, I realized there was such a need for us to have these conversations on the topic of ethics. A lot of questions posted on social media forums and groups have an underlying ethical component and practitioners are not necessarily aware. The more I researched, the more I realized these topics are so complex and can be very interesting when applied to the daily life of a pelvic health provider
Let’s talk about how you can know if something has an ethical component or concern. There are a variety of tests and measures to assess ethical situations and we review these in the class Ethical Concerns for the Pelvic Health Professional. If you are wondering if some of the clinical questions you have are actually founded in ethics you may find yourself asking questions like the following.
One of my favorite ways to assess an ethical question is by using the Kidder’s Ethical Decision Making Model. The fourth step of this model includes four checkpoints that can be helpful for quick clinical questions. These give us an idea of ways to recognize right versus wrong in scenarios and how we can correct or act accordingly. The four tests proposed by kidder are “The Legal Test,” “The Stench Test,” “The Front Page Test” and “The Mom Test” (Ferrier, 2021). If an ethical concern does not pass one of these tests, it does not have merit as an ethical course of action. If something doesn’t pass these tests, the right versus wrong aspect is a moral temptation and a person has to decide which option they would like to choose. We all have different moral compasses and backgrounds and so each person’s comfort level with these decisions may be different.
If a scenario arises, we start with “The Legal Test.” This is where we think about whether an action (or inaction) is legal or not. This may require some research or consultation if we do not know the answers. “The Stench Test” tests a person’s inner moral intuition. How does it feel with how you have been raised and when referenced against your moral foundation? “The Front Page Test” encourages a person to theorize how they would feel if the ethical situation they are thinking about were to be on the front page of a newspaper. It is a publicity test, do you want that to be how the world sees you, your clinic, your practice, your skills, etc? “The Mom Test” makes us reference all those who have been moral examples or might pass judgment on decisions we make (Ferrier, 2021).
Knowing these tests, look at the scenarios at the end of this blog. Imagine how you might run through the four Kidder Tests clinically. This can be great practice for clinical decision making. Like any skill, the more we practice, the more confident we are in the skill and the easier it is to do the task.
Ultimately with ethical decision making, there is a lot more “grey area” and “it depends” answers than there are clear cut scenarios. We can be much more comfortable with the decisions we make based on how we have examined the information and considered all options and outcomes. One of the positives of this class, Ethical Concerns for the Pelvic Health Professional - January 29, 2023, is having an audience of peers to talk through real clinical concerns and situations to problem solve and get input on things that may be weighing on a provider.
Scenario 1: Your patient comes in and tells you that their partner yells at them on a regular basis and controls how they can spend their money.
- The Legal Test: What are your legal abilities and obligations here?
- The Stench Test: How do you feel about this?
- The Front Page Test: If someone posted the story “Therapist told about XYZ and does ABC” how would you feel?
- The Mom Test: How would your parent/ caregiver feel about your decision on this scenario?
Scenario 2: A patient tells you that their practitioner forced them to have a pelvic examination without explaining the procedure and continued after the patient asked them to stop.
- The Legal Test: Is what this practitioner did legal?
- The Stench Test: What is your gut feeling in this scenario?
- The Front Page Test: If someone wrote a review about your practice and included this story, would it be a positive for your practice?
- The Mom Test: How would your favorite clinical instructor have felt about this situation?
Scenario 3: You have been invited to an affiliate program with a popular medical device company. You have the opportunity to make $15 for every patient care item you can sell in your clinic.
- The Legal Test: Are there any legal implications?
- The Stench Test: How do you feel with a quick “right versus wrong” decision here?
- The Front Page Test: How could you advertise this for your clinic in a way that is positive?
- The Mom Test: If someone posted this situation in a Facebook Pelvic Support Group, what would the response be?
Resource:
Ferrier, Patricia. Applying Kidder's ethical decision making model - in this article, the author uses a model of. Studocu. (2021). Retrieved December 26, 2022, from https://www.studocu.com/en-us/document/florida-institute-of-technology/introduction-to-behavior-analysis/applying-kidders-ethical-decision-making-model/20045486
Ethical Concerns for Pelvic Health Professionals

Course Dates:
January 29, September 16
Price: $175
Experience Level: Beginner
Contact Hours: 6
Description: The purpose of this class is to explore the ethical challenges Pelvic Health Practitioners may experience including consent, managing trauma and abuse, and preventing misconduct. This includes basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges due to the anatomical areas being treated, topics being discussed, and intimacy of sessions
Hello everyone…we hope your 2023 has been peaceful and productive. Dr. Meehan and I are very excited about the upcoming course on Menstruation and Pelvic Health. We’re excited because this is a chance to discuss the Menstrual Experience, an opportunity that is not common in society today. Menstrual Symptoms and anxiety about seeing blood on clothes or furniture can create obstacles to opportunities in education, career advancement, relationships, health care, family, sports, and enjoyment. Society has missed out for too many generations on the contributions of people who have had to miss opportunities to shine due to challenging aspects of their Menstrual Experience.
Many patients have Menstrual Concerns that they would like to discuss with someone but don’t feel confident or able to engage in these important conversations. Pelvic floor practitioners have a unique opportunity to evaluate their patients’ Menstrual Experience and create an individualized care plan that takes that experience into consideration. We discuss how to initiate conversations with patients on a topic that is surrounded by cultural taboo and stigma, and we discuss biological underpinnings of the normal Menstrual Cycle and of Menstrual Symptoms that so many people experience each month, often hundreds of times in a lifetime
There is a very exciting section of the live course dedicated to understanding the quickly evolving landscape of options to manage Menstrual Flow. We carry out live demonstrations on how much blood is lost on each day of a ‘typical’ period, and we have demonstrations of use, mode of action, and maintenance of wide variety of disposable and reusable products: Liners, Pads, Intra-Labial Pads, Tampons (we discuss absorbency, expansion, and applicators), Cups, Discs, and ever-expanding options in Period Underwear, Period Activewear, Period Sleepwear, Period Swimwear (bikini and 1- piece), and Menstrual Sponges (not recommended). We discuss pros and cons of these collection and absorption method on different days of flow, and we develop a Flow Management plan so each person can confidently engage in the things that are important to them on any day of the month.
This course was designed to promote open discussion of the Menstrual Experience among health care providers so we are confident and prepared to serve as advocates of productive Menstrual Dialogue to re-consider the Menstrual Experience in a more positive light. It is our hope that this course inspires participants to engage in Menstrual Conversations with patients, with people who are important to them, within professional circles, and in social communities to erode Menstrual Stigma and find solutions real practical that reduce barriers to opportunities in education, career advancement, relationships, health care, family, sports, and enjoyment.
We hope to see you soon in the class to take the next important step together on this exciting Menstrual Journey!
Nicholas Gaffga, MD, FAAFP, MPH and Amy Meehan, PT, DPT, MTC
Menstruation and Pelvic Health
Course Dates:
February 25-26
Price: $575
Experience Level: Beginner
Contact Hours: 19
Description: This course is designed for clinicians who want to obtain advanced knowledge and skills to educate patients on non-hormonal, non-surgical, and non-prescription interventions for improving the Menstrual Experience. Developed by Nicholas Gaffga, MD, MPH, FAAFP and presented together with Amy Meehan, PT, DPT, MTC, this course is geared towards the pelvic rehab provider looking to impart Menstrual Interventions that:
- Put control in the hands of people who menstruate to identify and carry out the interventions that are appropriate to them.
- Use a holistic approach and advanced knowledge and familiarity with body and mind.
- Emphasize healthy practices that can positively impact the Menstrual Experience and beyond, in areas such as mental health and chronic diseases.
- Discover root causes of issues, rather than quick fixes, to have benefits that are sustainable across the lifespan.

Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
It has been nearly 8 years since I taught my first in-person rendition of “Nutrition Perspectives for the Pelvic Rehab Therapist” in Seattle, WA through Herman & Wallace – and over a decade since I began writing the course in earnest. Creating and teaching this course has been an honor for me and truly a full-circle opportunity to share my passion for nutrition with other clinicians. The mission of the course is to create a ripple effect from one person to the next. But if there’s anything the last couple of years has taught me, it’s that we still have a long way to travel to reach the destination of fully integrated care centered on the whole person. As a guide, I tap the growing body of literature on nutrition and health to help show us the way.
I recall having taught this course on 11 occasions in-person between June 2015 and October 2019 at gracious site host clinics nationwide. I enjoyed each and every one of these experiences. Since the 2020 pivot to remote format, I have taught Nutrition Perspectives via Zoom 18 times - after we were faced with restrictions on traveling and gathering.
Having taught Nutrition Perspectives in both formats, I’d like to share with you first why I love teaching this course, and second why I love teaching it in its remote format. It truly is a class perfectly suited to this mode of delivery.
First, why I love teaching this course:
It is my passion to share nutrition information with peers in pelvic rehab. Before becoming a PT, I studied nutrition as an undergrad. After becoming a PT, and more specifically a pelvic PT, it became crystal clear that we needed to incorporate the essence of nutritional sciences into pelvic rehab– and even into general clinical practice. Nutrition Perspectives became my answer to the burning and urgent questions I had about how we could blend the worlds of rehabilitation and nutrition. I scoured the literature to find answers – and what I found was astonishing. Paradigm shifting. Compelling.
Early in my career, I would only sporadically encounter patients who would experience what I would now describe as “functional gastro-intestinal disorders with extra-intestinal manifestations”. Fast-forwarding to today, it is rare to see a patient who does not experience any conditions such as GERD, constipation, gas/abdominal pain/bloating/discomfort, anxiety, depression, and complex or chronic pain conditions. Because of this reality, it has become essential for healthcare providers to have a basic working knowledge of functional nutrition. Especially providers in pelvic rehabilitation. Having a working knowledge of these conditions and potential nutritional underpinnings can help us better understand and serve our clients.
Not only does nutrition have significant relevance to our patients – it is relevant to each of us as human beings! But be aware – the realm of nutrition appears chock-full of confusing contradictions. And our patients are now – more than ever – asking us for our thoughts on nutrition-related topics. They’re listening to podcasts. They’re reading social media posts and blogs. They’re watching short video clips to find quick answers to complex questions. And they want to run some of their questions by you – their trusted health professional ally. You want to feel confident and competent in what you’re sharing. My mission is to make evidence-informed information accessible and relevant to you, the practicing clinician so then you can, in turn, share with confidence and competence.

Now, on to why I love teaching this course remotely:
Don’t get me wrong – I love to travel. But imagine traveling alone to new cities -not as a free-spirited adventure solo traveler – but instead as an idealistic instructor who doesn’t want to be without any supplies needed for teaching a course far from home! This translates to a very heavy suitcase filled with visual aids and lab supplies. This humongous check-in bag contains items necessary to conduct the course descriptively – books, empty product containers, glass jars (yes, GLASS), carefully packaged kefir grains, a SCOBY, bowls, spoons, kitchen towels, and those hard-to-find food items that one can’t be certain to find in an unfamiliar city. And a tablecloth. Because when we’re talking about food with guests, presentation is important!
Now imagine navigating travel challenges with said heavy, giant suitcase; chucking it on and off a rental car bus during a cold rainstorm for example.. Imagine pushing it down a carpeted hotel hallway that is so plush, it prohibits the wheels from functioning properly. Imagine repacking in 15 minutes what took 3 hours to initially pack in order to catch a return flight home.
This was the reality of logistics I eagerly and enthusiastically took on to be able to teach this class. But that giant suitcase couldn’t hold even close to everything I wanted to share, and it actually was a bit cumbersome to manage. Maybe a lot cumbersome. Always plastered with the bright orange “HEAVY” sticker warning – there was a limit to what I could bring along to live course events.
When we first transitioned this course to remote format, it was a quick response to begin offering CEUs when lockdown mode began. The silver lining, we discovered, was that the remote format for this course was in fact – much better than the live event format.
Now, all the necessary supplies are right where I need them to best instruct. Plus, predictable kitchen and lecture spaces create a seamless experience for the participants. Teaching from home has been life-changing as an instructor. I can practice what I preach about nourishing the nervous system and mitigating stress with lifestyle choices. It is nourishing to be able to sleep well at home the nights before I teach. Adequate rest is a superpower that allows me to give my best well-rested self to the participants.
The remote format is not just nourishing to me, but also to the participants who can attend from the comfort of home or familiarity of a clinic. Wherever you are, you can take the course. No airports, no suitcases, nor carpeted hotel hallways. That’s accessibility. That’s getting this information into the hands and minds of providers in locations all around this country and beyond. We need this accessibility if we ever hope to reach our destination of fully integrative care of the whole person – for all.
For these reasons, Nutrition Perspectives for the Pelvic Rehab Therapist will remain in this remote format – even as our lives begin to involve travel and in-person events again. All good things. But I do hope you enjoy taking Nutrition Perspectives as much as I enjoy teaching it. I invite you to join me on the journey toward implementing more integrative care as standard practice. It’s not always an easy road, nor the popular road. And sometimes it feels as hard as dragging a giant, heavy suitcase behind you. But it’s a path worth taking – one that will be fruitful for both you and the clients you serve. Let’s travel it together.
Nutrition Perspectives for the Pelvic Rehab Therapist will be offered quarterly in 2023: January 21-22, June 10-11, September 16-17, and December 2-3.
Nutrition Perspectives for the Pelvic Rehab Therapist

Course Dates:
January 21-22, June 10-11, September 16-17, and December 2-3
Price: $525
Experience Level: Beginner
Contact Hours: 17.75
Description: Participants will be introduced to the latest research in nutrition through immersive lectures and hands-on labs. The course will cover essential digestion concepts, nourishment strategies, and the interconnected nature of physical and emotional health across the lifespan. Further, clinicians will delve into nutritional relevancies in bowel and bladder dysfunction, pelvic health, pain, and healing. Labs throughout include insightful demonstrations and breakout sessions. The course participant will acquire new, readily applicable tools for patient empowerment, engagement, and self-management utilizing presented principles.
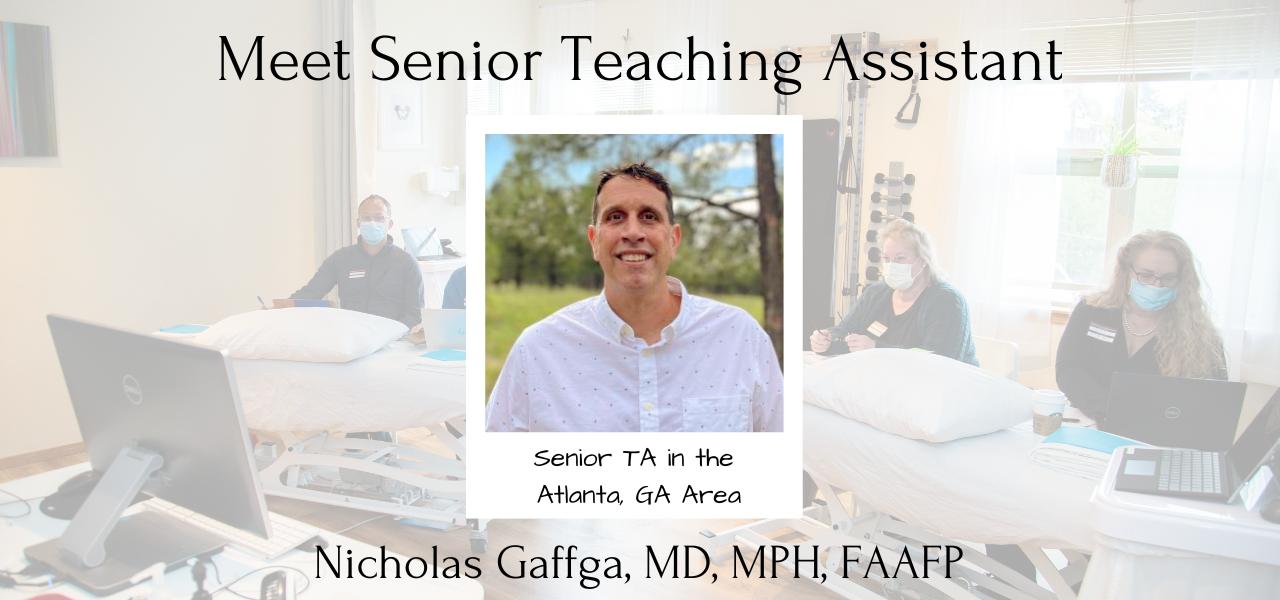
Nicholas Gaffga, MD, MPH, FAAFP sat down with The Pelvic Rehab Report this week to discuss himself and how he came to TA (and teach) for Herman & Wallace. Niko is scheduled to TA next in Birmingham, AL for Pelvic Floor Level 1 scheduled March 4-5 2023, and will be instructing Menstruation and Pelvic Health on February 25-26 2023.
Who are you?
Describe your clinical practice. My name is Niko Gaffga, and I am a family medicine physician seeing patients in Atlanta, GA. Over the 20 years I have been practicing medicine, I have worked in a number of settings: pediatrics, gerontology, emergency room, ICU, HIV prevention in Africa for 4 years, occupational medicine, travel medicine, and obstetrics and gynecology. As I look back over these memories, the area of work where I most feel connected with my patients is women’s health and outpatient gynecology.
How did you get involved in the pelvic rehabilitation field?
My journey in pelvic health physical therapy has been one of the most exciting and rewarding of my career. One day in my clinic I saw a patient who had pelvic pain. When I walked into the room she was crying. Over the next few months, we were able to reduce her IC symptoms considerably with medications and diet modification. And one time when I went into the room to see her, she stood up and smiled and hugged me. This reminded me why I wanted to be a doctor. Along this journey, I realized there were aspects of her experience that I could not address using my training as a physician, so I began investigating other ways to provide more holistic care to my patients. That was when I discovered the world of pelvic floor physical therapy. To understand more, I signed up for PF1. During that 3-day weekend, I saw the power of powerful pelvic floor physical therapy to help patients feel better. Since that time, I have taken all the courses in the Pelvic Floor series, as well as Male Pelvic Floor and three other specialty courses offered at Herman & Wallace. I even overcame my fear and anxiety and signed up to be a teaching assistant. I thought I could never be a TA…but since that time I have been TA 13 times and each time I am grateful for the opportunity to make a difference in other people’s lives. My experience working with pelvic floor practitioners has shown me the power of collaborating among health care professionals with different skills and treatment modalities to offer our patients the most holistic and effective care they can get.
What patient population do you find most rewarding in treating and why?
The most interesting and rewarding aspect of my work is helping patients improve their Menstrual Experience. Menstrual Forums can be difficult to find, but they create opportunities to share knowledge and understanding of the Menstrual Experience to increase Menstrual Optimism, Menstrual Confidence, and ultimately, Menstrual Pride. I have been working for 7 years to create a course that empowers pelvic health practitioners to open a Menstrual Forum with patients to help them better understand and improve their Menstrual Experience. It is a humbling, fascinating, and rewarding experience to walk with someone on a Menstrual Journey.
If you could get a message out to physical therapists about pelvic rehab what would it be?
If there are issues that as a rehab practitioner you are having trouble helping your patients with, explore referring them to a pelvic floor therapist who can help the patient in a whole different way.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
There is a simple scenario that profoundly changed how I see my patients. Physicians carrying out gynecological procedures are trained to sit at the foot of the bed to get the best field of view and to be able to carry out procedures on the patient. However, pelvic floor physical therapists usually sit next to the patient for ergonomics and also to be able to detect pain or anxiety on the face of the patient with each procedure that is carried out. This simple change in perspective invited me to be more aware of the effect that the visit is having on the patient and be more mindful of how they experience the encounter.
What do you find is the most useful resource for your practice?
My most useful resource is the ability to communicate with a variety of health professionals who have
What is in store for you in the future as a clinician?
My dream is to work in outpatient gynecology in close collaboration with a pelvic floor physical therapist to provide holistic health care for our patients.
What books or articles have impacted you as a clinician?
The Female Pelvis (Bandine Calais-Germain) for its beautiful informative illustrations that make pelvic anatomy and physiology come to life; In the Flo (Alisa Vitti) and The Rumi Collection (Kabir Helminski) for their new perspective on life; Period Repair Manual (Lara Briden); and The Fifth Vital Sign (Lisa Hendrickson-Jack) for their informative and proactive approach to understanding and improving the Menstrual Experience.
What has been your favorite Herman & Wallace Course and why?
Pelvic Floor Level 1 was life-changing for me because it introduced me to a whole new field of care and a whole different way of seeing patients. Herman & Wallace has been welcoming to me, as a physician and as a male, into a world where I could have potentially felt like an outsider. Thank you.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
In the past 3 years, I have worked with 14 different Herman & Wallace instructors as a participant and as TA. I have learned many lessons, but the one that has helped me the most is the encouragement to follow my dreams and to be the best I can be, even if the road seems difficult or unorthodox. There is a world out there waiting to be created.
What do you love about assisting at courses?
Being a TA at Herman & Wallace courses is the highlight of my month. I literally look at my calendar each day to see how soon it will be until the class starts. I love being a part of other people’s journey to learn more about pelvic floor physical therapy, I love helping people find their way in their careers, I love sharing the things that I am passionate about, I love sharing a physician’s perspective, and most of all I love seeing the light bulb turn on in someone’s eyes when they have visualized something in a new and exciting way.
What is your message to course participants who are just starting their journey?
If pelvic floor therapy is a field that you are curious about or find interesting and you feel a calling for, I encourage you to invest time and energy to learn more about it. Your professional options and your ability to help people will only be limited by what you can imagine.
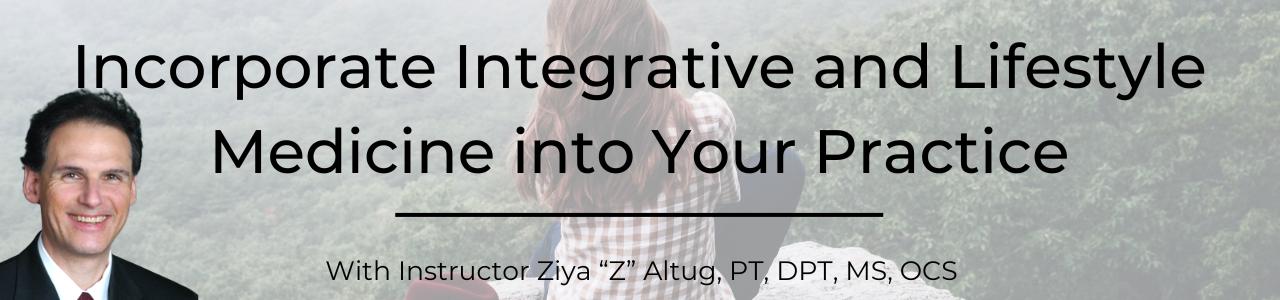
Ziya Altug, PT, DPT, MS, OCS is a board-certified doctor of physical therapy with 32 years of clinical experience treating musculoskeletal injuries. Z currently provides outpatient physical therapy in the home setting in Los Angeles, California, and serves as a continuing education instructor. He received his Bachelor of Science in Physical Therapy at the University of Pittsburgh in 1989, a Master of Science in Sport and Exercise Studies in 1985, a Bachelor of Science in Physical Education in 1983 from West Virginia University, and a Doctor of Physical Therapy from the College of St. Scholastica in 2015. Z is a long-standing member of the American Physical Therapy Association and a member of the American College of Lifestyle Medicine. He has attended workshops in yoga, tai chi, qigong, Pilates, Feldenkrais Method, and the Alexander Technique.
Dr. Altug is the author of the books Integrative Healing: Developing Wellness in the Mind and Body (2018), The Anti-Aging Fitness Prescription (2006), and Manual of Clinical Exercise Testing, Prescription, and Rehabilitation (1993). In 2020, he published the chapter Exercise, Dance, Tai Chi, Pilates, and Alexander Technique in The Handbook of Wellness Medicine. In 2021, he published the article Lifestyle Medicine for Chronic Lower Back Pain: An Evidence-Based Approach in the American Journal of Lifestyle Medicine. Z joins the H&W faculty and is presenting his personally curated course Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management. This week he sat down with The Pelvic Rehab Report to discuss his course.
What made you want to create this course?
My father was a physician specializing in internal medicine. He specialized in treating conditions such as tuberculosis, chronic obstructive pulmonary disease (COPD), and asthma. Starting in elementary school, I remember discussing with my Dad the importance of nutrition, sleep, stress control, and sustainable activity in healing. Of course, as a ten-year-old, I played with his stethoscope and reflex hammer for hours! My father used “lifestyle medicine” principles to help his patients recover. My Mom introduced me to the benefits of aromatherapy for relaxation. She used to wash our clothes with lavender-scented soaps, and there was lavender-scented potpourri throughout our house. My mother used to say the lavender was to “keep the wolves away so the sheep can sleep.” She also taught me how to prepare and cook healthful meals in high school. Now, I have a fascination with culinary medicine. I am very grateful for all of these childhood experiences.
Before entering PT school, I majored in physical education and exercise science. After I graduated from PT school, I wanted to use my interest in wellness, health, fitness, and self-care strategies to help patients heal and recover. Recently, I have followed the American College of Lifestyle Medicine research and webinars to gain additional knowledge. Currently, I treat patients in their homes and teach continuing education courses in integrative and lifestyle medicine.
What need does your course fill in the field of pelvic rehabilitation?
This course provides practical tools to help clinicians manage pain. For example, my course will cover research, resources, and labs to create clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, and expressive and art-based therapies. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis, and self-massage. All of these strategies may be helpful for clinicians specializing in pelvic rehabilitation.
Who, what demographic, would benefit from your course?
Rehabilitation providers of any experience level would benefit from taking this course.
What patient population do you find most rewarding in treating and why?
I currently focus on orthopedics and geriatrics. I especially enjoy working with older patients in their homes and designing creative home exercise programs they can use to stay healthy.
What do you find is the most useful resource for your practice?
I enjoy using resources from the following organizations:
- American College of Lifestyle Medicine
- American College of Sports Medicine
- International Association for the Study of Pain
What books or articles have impacted you as a clinician?
I enjoyed reading the following three books to expand my knowledge of lifestyle medicine and integrative medicine:
- Lifestyle Medicine by James Rippe
- Lifestyle Medicine Handbook by Beth Frates and colleagues
- Lifestyle Medicine by Garry Egger and colleagues
What is your message to course participants who are just starting their journey?
I recommend all clinicians collaborate with professionals outside their own profession. For example, I recommend physical therapists work with the following:
- Acupuncturists, massage therapists, registered dietitians
- Practitioners in yoga, Pilates, qigong, tai chi, Alexander Technique, Feldenkrais Method
- Specialists in expressive therapies such as dance, music, art, drama, poetry, and play.
Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management

Course Dates:
January 21, 2023
Price: $125
Experience Level: Beginner
Contact Hours: 4.5
Description: This course was written and developed by Ziya “Z” Altug, PT, DPT, MS, OCS, a board-certified doctor of physical therapy with 32 years of experience in treating musculoskeletal conditions, Brief lectures on the research and resources and labs will cover a toolbox approach for creating clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, expressive and art-based therapies, and the impact of nature on health. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis, and self-massage.
Janet Drake Whalen, PT, DPT sat down with The Pelvic Rehab Report this week to discuss herself and how she came to TA for Herman & Wallace. Janet is scheduled to TA next at the Doylestown PA for Pelvic Floor Level 1 scheduled January 7-8 2023.
Hi Janet, can you tell us a little bit about yourself and your clinical practice?
I am a physical therapist with 36 years of experience who has spent 34 years of my career in women’s health physical therapy. Over my career, I have been an advocate and continue to promote abdominal and pelvic health for all. My career led me to become a Lamaze-educated childbirth educator, certified neuroscience practitioner, women’s health coach, and professional yoga therapist. My clinical practice now is in a hospital setting where I am educating outpatient therapy staff, healthcare providers, and physicians on pelvic health. I am heading the start of a 4th-trimester program and a sexual health program.
What has your educational journey as a pelvic rehab therapist looked like, and how did you get involved in the pelvic rehabilitation field?
My educational journey started after an unplanned cesarean birth of my first son 34 years ago. In 1988 resources for women after delivery was scarce. I started looking into education and found a course taught by a nurse, Jo Laycock, from England. I attended her course sitting with nurses to learn about incontinence. My first women's health physical therapy courses were through the OB/GYN section of the APTA taught by Elizabeth Noble, Holly Herman, Kathy Wallace, Jill Boissonnault, and Marla Bookout. When Holly Herman and Kathy Wallace started their own education company, I started to attend courses through Herman & Wallace. After my vaginal birth after the Cesarean of my second son in 1990, I studied and earned my Lamaze International Childbirth Educator certification. I taught Lamaze for 9 years and continue with my certification. I started as a teaching assistant with Herman & Wallace approximately 15 years ago.
What patient population do you find most rewarding in treating and why?
This is a difficult question for me, although I would have to say that pregnancy and postpartum was my initial passion. Sexual health and whole-body wellness have been my passion for the past 12 years. I enjoy the interdisciplinary approach to sexual dysfunctions and continuing to learn more every year from patients and fellow clinicians.
If you could get a message out to physical therapists about pelvic rehab what would it be?
Every patient has a pelvis with organs and muscles. If you are treating spine and hip patients, you are affecting the pelvic floor muscles and the pelvic floor muscles are affecting your patients’ symptoms. External treatment can be as effective as internal treatment - so take a pelvic health course, you and your patients will benefit!
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
I've had so many amazing instructors and colleagues over the years. From my therapeutic pain specialty certification to Louis Gifford’s work on what patients really what to know: 4 questions...
- What is wrong with me?
- How long will it take?
- What can I (the patient) do for it?
- What can you (the healthcare provider) do for it?
Also, listen to your patient's story. Meet your patients where they are and ask them open-ended questions.
What do you find is the most useful resource for your practice?
Besides a hi-low table, my ears and my heart.
What is in store for you in the future as a clinician?
To educate as many clinicians and therapists as possible to be ready to hand over the baton in five to seven years. A successful 4th-trimester program and sexual health program at the hospital I am currently employed.
What books or articles have impacted you as a clinician?
This is another tough question for me I have a library of books. But I will say that a textbook that I always have on hand is Anatomy Trains by Tom Myers. Research articles that provide a consensus of terminology and classifications with algorithms that are great to discuss with other clinicians.
What has been your favorite Herman & Wallace Course and why?
Pelvic Floor 3 (now Pelvic Floor Capstone) with Holly Herman piqued my interest in sexual health. Since that time all the visceral and myofascial courses with Ramona Horton have shaped and deepened my practice.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
One lesson that has stayed from Nari Clemens is how important it is to take care of yourself. Another from Ramona Horton regarding hands-on treatment is that you are having a conversation with the brain/nervous system.
What do you love about assisting at courses?
What I love about assisting at courses is meeting all the physical therapists from different stages of their careers with an interest in pelvic health. Their energy excites me and reminds me how wonderful our profession is.
What is your message to course participants who are just starting their journey?
If you're just starting your journey, hold on! There is a lot to learn, to practice, to share, and to educate others. You are going to influence so many people’s lives.
Tara Sullivan, PT, DPT, PRPC, WCS, IF sat down with Holly Tanner and The Pelvic Rehab Report to discuss her course, Sexual Medicine in Pelvic Rehab. Tara started in the healthcare field as a massage therapist, practicing for over ten years including three years of teaching massage and anatomy, and physiology. Tara has specialized exclusively in Pelvic Floor Dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012.
Hi Tara, can you introduce yourself and tell us a little bit about your background?
Sure! So I’m Tara. I’ve been a pelvic health rehab therapist for about 10 years now. I started right out of PT school and I got a job at a local hospital where they were looking to grow and build the pelvic rehab program. So of course, I found Herman & Wallace and started taking all of the classes there that I could and just kept learning over the years. Now the program is expanded across the valley, we have nine different locations, and it’s been very successful and fulfilling. It’s my passion.
Recently, I would say the past four to five years of my career, I’ve started getting more into sexual dysfunctions. I was always into pelvic floor dysfunction in general - bowel, bladder, sexual dysfunction, and chronic pelvic pain, but I didn’t get specifically into the sexual medicine side of it until recently. I did the fellowship with ISSWSH that really pulled all of that information together with what I’ve learned through the years.
Can you explain what ISSWSH is and how that combined with the knowledge base that you already had?
I feel like ISSWSH for me, where I came full circle. I finally was like “I get it.” ISSWSH is the International Society for the Study of Women’s Sexual Health and it’s all the gurus like Dr. Goldstein, Rachel Rubin, and Susan Kellogg that have been around forever doing the research on sexual medicine. I started attending their conferences, became a faculty member, and presented at their annual fall meeting here in Scottsdale. Then I ended up doing their fellowship. Every year I would attend the conference, but it took a couple of years for all of that knowledge to soak in and for me to be able to really apply it. For example, that patient with that sticky discharge, maybe that is lichen planus – that’s the kind of medical side that you don’t necessarily learn in physical therapy school.
That for me just really helped my differential diagnosis which means that you can get the patient’s care faster. Get them to that resolution faster because you are working with a team of people and we all have our roles. As PTs and rehab practitioners, we have the time to sit with our patients. We are so blessed to have an hour, and the medical doctors don’t, for us to really take that time to figure out the patient’s history and what they’ve been through, and what could be the cause of it. We have the time to be the detective and help them get the care they need. Whether it’s with us, or in conjunction with something else. My goal is to never tell someone that I can’t help them because it’s not muscular.
How has this knowledge helped you in your collaboration with other practitioners in your practice?
I feel like this knowledge was the missing link for me. It brings it all together for the patient. So the patients come here and the urologist says “that’s not my area,” and then the gynecologist says “that’s not my area.” Then they come to you and you’re like “it’s kind of my area, but I can’t prescribe the medication that you need.”
My practice got so much better, just in the sense of the overall quality of care, when I was able to develop those relationships with the doctors. I could pick up the phone and say “Hey, that patient that you sent me – I think they have vestibulodynia, and I think it’s from their long-term use of oral contraceptive pills. I think that they might benefit from some local estrogen testosterone cream.” They would say, I don’t know about that, and I’d respond “let me send you some articles. Let me tell you what I’ve learned.”
Now I can just pick up the phone or send them a text asking them to prescribe so and so. It really helped bridge that gap. The doctors now will say “Ok. I know something’s going on, but I don’t know if it’s muscular or tissue. I don’t have that training, what do you think?” So it’s just been such a collaboration, it’s been so great. Then I’ll go the reverse of that and watch them do a surgery, watch them do a procedure.
For our patients, we need to take that time and work with the physicians and develop that relationship with them, because it’s easy to pass it off as “that’s not my job.” Especially the vestibule! The gynecologist goes right through it and looks into the vaginal canal and then the urologist is like I’m going to look at the urethra but I’m not looking around it, let me just stick that scope in. This knowledge and ability to use differential diagnosis, for me just brings it all together.
Does your course have an online, pre-recorded portion as well as a live component?
Yes. There are about nine lab videos on manual techniques because everyone wants to know what to do. For me, it’s more about what you know. What can you identify and differentiate with the differential diagnosis. Then we have about two hours of just the basic lectures on general pain and overactivity of the pelvic floor so that we can spend our time in the live lecture getting into the very specific conditions that we as PTs are, not necessarily diagnosing, but recognizing and sending for further care. That’s really where I wanted this class to fill the gap between the urologist, the gynecologist, and the PT.
Is your course primarily vulvo-vaginal conditions or are there some penile, scrotal, or other conditions?
It is both male and female dysfunctions, and I have a few transgender cases. I don’t personally treat the transgender population very often so I only have a couple of examples of that. I have a lot of examples where I’m trying to get practitioners to recognize the problem by what the patient is saying and their history, and how to funnel this into their differential diagnosis. Case studies include different types of vestibulodynia and causes, all the different skin conditions…and it’s not necessarily something that they didn’t learn in one of the Pelvic Floor Series courses, but I wanted one class where they could just talk about all the sexual dysfunctions and get into some of the ones that we don’t see as often but are present.
We also talk about PGAD (persistent genital arousal disorder), and with male dysfunctions, we talk about spontaneous ejaculation and urethral discharge, post finasteride syndrome. All of these things that you might not see every day, but when you see them you’ll recognize them so that you can help patients talk to the doctor and get the proper care. There are a lot of random, not as obvious, conditions that are not as prevalent. Then there are the common conditions that we see every single day like lichens.
What is the biggest takeaway that practitioners have who come into your class?
It is really being able to access and effectively use differential diagnosis. A lot of practitioners in the course are like “I always wondered what that was.” I have a ton of pictures that I share, and I’m like, I know have seen this before. I think a lot of it is the differential diagnosis. The feedback that I get from every class is “I feel like I can go to the clinic on Monday and apply what I learned.” “I’m going to go buy a q-tip and start doing a q-tip test because now I know what to do with that information.” They feel that confidence of really being able to apply it, talk to the patient, talk to the doctors, and figure out that meaningfulness.

Sexual Medicine in Pelvic Rehab
Course Dates:
January 14-15, 2023
May 13-14, 2023
September 23-24, 2023
Price: $450
Experience Level: Beginner
Contact Hours: 15
Description: This two-day course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, squirting, G-spot, prostate gland, sexual response cycles, hormone influence on sexual function; the anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function, and specific dysfunction treated by physical therapy in detail. Including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, and post-prostatectomy, as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD), and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Course Reviews:
- The instructor offered excellent examples of what can be seen in the patient population and advised good treatment plans to help. She was very thorough in answering questions and very well-informed on all topics presented in this class. I was so thankful to learn more about the hormone component of pelvic floor rehab, as I feel that this is greatly lacking in the Midwest -- we still live on the idea that hormones and HRT are BAD! Looks like I will be doing some heavy marketing soon with research articles! Thank you so much for all of this information!
- Various topics only glossed over in other courses were covered in detail to meet the various levels of knowledge of all students in the class. On top of this, new and useful material was also introduced and explained very well.
- Tara gave practical tips for us to start using in clinical practice and her notes to her lecture were KEY!

Erica Vitek, MOT, OTR, BCB-PMD, PRPC has attended extensive post-graduate rehabilitation education in the area of Parkinson disease and exercise. She is certified in LSVT (Lee Silverman Voice Treatment) BIG and is a trained PWR! (Parkinson Wellness Recovery) provider, both focusing on intensive, amplitude, and neuroplasticity-based exercise programs for people with Parkinson disease. You can learn more about this topic in Erica's remote course, Parkinson Disease and Pelvic Rehabilitation.
Does the person with Parkinson disease sense where to contract their pelvic floor and the level of contraction they need to overcome the strength of the urge they experience? The sensorimotor deficit that we can visually observe as degradation in movement amplitude in the limb motor system, for example shuffling steps and micrographia, is also suspect in the pelvic floor. Also, consider the lengthening of the pelvic floor that must occur for emptying the bowels. Adequate descent amplitude of the pelvic floor and proper coordination with the abdomen to do so may also not be sensed. Further, strengthening of the pelvic floor is an effective technique for improved sexual health functioning, but may also be challenged by impaired sensorimotor feedback. Treatment of this sensorimotor mismatch in the pelvic floor in a person with Parkinson disease requires specialized expertise and feedback from an OT or PT who treats pelvic floor dysfunction and understands how the neurodegeneration affects their abilities.
When most people think about people with Parkinson disease, they think about stooped posture, shuffling gait, slow and rigid movement, balance difficulties, and tremoring. Often these motor symptoms are the main target of pharmacological treatments with neurologists and many experience positive functional gains. Non-motor symptoms, however, can be more disabling than motor symptoms and have significant adverse effects on the quality of life in people with Parkinson disease.
The pharmacologic management of non-motor autonomic dysfunction, including urinary, bowel, and sexual health impairments, is often ineffective, not supported by adequate research, or causes intolerable side effects for people with Parkinson disease. In a recent article titled “Update on Treatments for Nonmotor Symptoms of Parkinson’s Disease – An Evidence-Based Medicine Review.” Seppi, K, et al., 2019, the authors state this about the use of a pharmacological treatment approach - “Before attempting any treatment for lower urinary tract symptoms, urinary tract infections, prostate disease in men, and pelvic floor disease in women should be ruled out.” It is rare to see a mention of the pelvic floor within the literature that addresses helping people with Parkinson disease.
Pelvic rehabilitation specialists have a unique opportunity to step in and help these individuals improve their quality of life and many neurologists are unaware of the benefits our services could provide for their patients. Please join me in an exciting dive into understanding the physiology of how Parkinson disease affects a person’s pelvic health and develop your skills to effectively assess and develop treatment plans to change the life of these individuals.
Here is a sneak peek acronym into some of the teaching strategies discussed in Parkinson Disease and Pelvic Rehabilitation!
- P - Pacing
- A - Amplitude training
- R - Reinforcement feedback loop
- K - Kinesthetic training
- I - Internal cue restoration training
- N - Neuroplasticity training principles
- S - Sensorimotor retraining
- O - Occupation & goal-directed task training
- N - New skill restoration

Parkinson Disease and Pelvic Rehabilitation
Course Date:
January 27-28, 2023
Price: $300
Experience Level: Beginner
Contact Hours: 10
Description: This course introduces basic neuroanatomy with a detailed overview of pelvic neurophysiology in preparation for an extensive in-depth look at pelvic health treatment options for Parkinson disease. Pelvic floor external and internal neuro-musculoskeletal assessment considerations will be instructed with the understanding that participants have prior experience in pelvic health coursework or pelvic health patient treatment experience.
Preparatory lectures about Parkinson disease will help develop a clear understanding of the neurophysiology of the disease to establish an equal foundation between experienced practitioners and those who have never worked with this patient demographic. Live course lectures deep-dive into characteristic pelvic health conditions that people with Parkinson's disease may face, discuss multiple assessment and treatment planning options, and will also discuss applications for TENS in the neurologic population.
Course Reviews:
- Erica was a phenomenal instructor. She is very passionate and it showed throughout the session. The information she provided was very evidence-based and filled in the gaps for many other types of patients besides patients with Parkinson's. Would highly recommend this class even for learning about treating pelvic floor patients with neurological disorders.
- Erica is a skilled, interesting instructor. Her passion for this topic came through in her teaching style. She enhanced the course with her passion and delivery.
- I learned a great deal about Parkinson's and really felt that the course was worthwhile and valuable. I am very appreciative of the fact that she created a course about this specific topic as there is a large need.
- This was an awesome class. Erica is an incredible teacher! I can't wait to use what I learned this weekend in the clinic to help my patients!
Faculty member, and Sr. TA, Mora Pluchino, PT, DPT, PRPC is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). Mora authored and instructs Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens.
- "I want to start my own practice but I'm not sure if I need to hire a lawyer to help!"
- "I have a problematic patient that I want to discontinue seeing, but don't want to be guilty of abandonment of care."
- "I am so confused by the types of clinical insurance that I am required to have!"
- "I want to hire an employee and include a non-compete clause in their employment contract!"
- "I want to start my own cash-based practice and need help with this process!"
- "I plan to market my practice for THIS population, is it legal to exclude THAT group of people?"
With the end of 2022 approaching, now is the perfect time to take a pelvic health-focused ethics class. For many states, licensed professionals have to fulfill an ethics continuing education requirement, including physical therapists, occupational therapists, mental health, and many other healthcare providers.
I started writing this series a year ago. I struggled to find a class to meet my biannual ethics requirement for New Jersey that was related to my practice in pelvic health. I soon realized that as a pelvic health provider and educator, the most popular questions that come up for practitioners, secondary only to specific treatment interventions, are ethical in nature.
- "Is ________ ok?"
- "What happens if ________ happens?"
- "Can a patient sue me for ______?"
- "How do I do ________ legally?"
Providers want to know that they are providing services that are legal and ethical. Even if you have never considered yourself as being overly concerned with the topic of ethics, you have probably had these thoughts. That was certainly the case for me! The further I fell down the rabbit hole of ethics, the more I realized it affects our day-to-day clinical life minute by minute. Ethics is the study of right versus wrong and how we make those personal qualifying decisions. So this covers everything from cleaning procedures, scheduling, patient care, and more!
Practitioners want to know that they will not be open to any legal action for the care and services provided. This usually requires more awareness and knowledge than just purchasing an annual liability insurance policy. Each provider and clinical environment has their own ethos, policies, and procedures, but there are also larger existing rules and laws to help guide providers to provide the best possible care.
In Ethical Concerns for the Pelvic Health Professional, we discuss the basics of doing no harm to our patients, obtaining informed consent, and decision-making based on different ethical models. The goal here is to send you to work immediately following this class feeling more confident in ethical labeling and decision-making. This class is a more global and essential look at the concept of ethics as applied to pelvic health.
The sole purpose of Ethical Considerations from a Legal Lens is to explore the ethical challenges pelvic health practitioners may experience from a health law perspective. This course is for any pelvic health professional looking to build skills for ethical evaluation, problem-solving, and derivation of solutions with a specific focus on legalities and related concepts.
This series of ethics-related classes is meant to build your clinical character and problem-solving abilities in what feels like "sticky" situations and help to guide you to clinical and business decisions that make you feel comfortable at the end of a work day.
To sweeten up this class series, each offering has an expert join the discussion on certain topics and case studies, to offer additional perspectives and points of view to the discussion.
I am looking forward to having an open discussion about the ethical and legal considerations for our profession at the next offered class on December 10th, 2022!
Ethical Considerations from a Legal Lens
Course Dates:
December 10, 2022
June 3, 2023
November 12, 2023
Price: $175
Experience Level: Beginner
Contact Hours: 6
Description: This one-day remote course covers ethical considerations from a legal lens for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day-to-day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges, and the legalities of pelvic health can add further complications for patient care, business, and clinical practice decisions.
The purpose of this class is to explore the ethical challenges Pelvic Health Practitioners may experience from a health law perspective. This course is for any Pelvic Health Professional looking to build skills for ethical evaluation, problem-solving, and derivation of solutions with a specific focus on the legalities and related concepts. Prior to the live aspect of this course, participants will be asked to review the ethical framework and definitions via pre-recorded lecture and take Core Values Self Assessment. Live instruction will review applicable health laws and legal terms that converge with the pelvic health world. This will be followed by case study discussion in small groups, followed by a large group discussion with input from the instructor and a legal expert/ educator. The remainder of this course is meant to be a guided discussion through the legal and ethical struggles of the pelvic health practitioner.
Ethical Concerns for Pelvic Health Professionals - Remote Course
Course Dates:
January 29, 2023
September 16,2023
Price: $175
Experience Level: Beginner
Contact Hours: 6
Description: This course is for any Pelvic Health Professional looking to build skills for ethical evaluation, problem-solving, and derivation of solutions, and explores the ethical challenges practitioners may experience including consent, managing trauma and abuse, and preventing misconduct. Prior to the live aspect of this course, participants will be asked to review the ethical framework and definitions via pre-recorded lecture and take Core Values Self Assessment. Live instruction will review the ways in which patients and practitioners can be vulnerable in the pelvic health treatment setting and how to address this. This will be followed by case study discussion in small groups, followed by large group discussion with input from the instructor and an ethics expert/ educator. The remainder of this course is meant to be a guided discussion through the ethical struggles of the pelvic health practitioner
Aparna Rajagopal, PT, Mhs, PRPC, and Leeann Taptich, PT, DPT are the authors and instructors of the Breathing and the Diaphragm remote course. Aparna and Leeann bring a wealth of experience to this course.
Aparna: About 10-plus years ago I had a patient who had a large para esophageal hernia which had been surgically repaired. She had been referred to therapy because of general debility and weakness and she couldn't do endurance-based things like gardening or walking for long periods of time. She was in her mid-sixties. She had seen 2 or 3 therapists and they couldn’t figure things out. She had the same complaint that she couldn’t breathe and every time she said she couldn’t breathe the therapist would obviously refer her back to the doctor who would run cardiac tests, and all kinds of other tests and say she was cleared from a medical standpoint and then send her back to therapy. So in this process, the patient came to me and one of the first things she said was that she had difficulty taking in a breath of air -that she felt like she couldn’t expand - not that she couldn’t breathe.
Based on that complaint, I started my assessment. I started looking at the thoracic spine and found that she actually couldn’t expand from the rib cage at all because of her surgery to fix her large para esophageal hernia. One of the things we know about para esophageal hernias is also that it can be associated with increased intraabdominal pressure - related to things like chronic severe constipation, chronic cough, etc. She got better. She healed, and I realized that this was something that patients needed. In the process of treating her, my interest in breathing and the diaphragm developed.
Leeann: I started at Henry Ford Health Systems, where Aparna and I currently work together, about 7 years ago. Around that time, Aparna did a one-hour lecture on dysfunctional breathing and breathing to help us understand the mechanics of the pelvic floor and the abdominals, and the diaphragm. I’ve always looked for my missing link in my treatment, specifically in my lumbar/low back pain patients. The lecture was a lightbulb moment for me, and it made sense to me. What I used to focus on at that time was Transverse Abdominis engagement and it didn't always work for all patients.
I call Aparna my missing link. So, it started off with the one-hour lecture that she delivered. Then we collaborated and worked on developing a four-hour course on the same topic that ended up with eight hours worth of content because of how much great research there was available about the topic. Gradually the four-hour class transitioned into what we have now - a full weekend course. It’s a great mash-up of ortho and pelvic floor approaches for both of us and has really helped both of us treat our patients better from both a pelvic standpoint and an orthopedic standpoint.
Aparna: We work together. We are able to treat patients jointly, bringing in the diaphragm/breathing aspect, incorporating the sports and manual training that Leeann has and the pelvic knowledge that I have. We are able to tie everything together and treat our patients in a very holistic way.
Leeann: My big thing is that we try to incorporate more of the regional interdependence model. When patients come in with symptoms in an area, we look above, below, and beyond to see how the whole system is functioning together. We like to see how the body moves as a whole instead of focusing on just one part of it. That’s where most of our treatment is derived from and how we work together.
Breathing and the Diaphragm - Remote Course

Course Dates:
November 19-20
January 21-22, 2023
Price: $450
Experience Level: Beginner
Contact Hours: 14
Description: This remote course is designed to expand the participant's knowledge of the diaphragm and breathing mechanics. Through multiple lectures and detailed labs, participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi-component system that works together. Optimal function of the diaphragm and breathing patterns are key to a healthy pelvic floor, a normal functioning core, and postural stability. Evidence-based methods to assess the diaphragm and breathing mechanics are presented along with easy-to-apply practical intervention strategies.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. The assessment concepts and treatment techniques can easily be integrated into a therapist's current evaluation and intervention strategies.