Did you know that the food you eat can directly impact the way your brain processes pain and responds to stress? This may seem like a surprising connection, but research has shown that a maladaptive central nervous system (CNS), can be influenced by dietary choices.
A maladaptive CNS is a condition where the brain's ability to regulate sensory input and adapt to changes is compromised, leading to amplified pain perception and other negative symptoms commonly associated with chronic pain conditions. In this article, we'll explore the impact of diet on the development and function of a maladaptive CNS and discuss how making healthy dietary choices can help improve its resilience and overall cognitive abilities. So, buckle up, put down that bag of chips, and get ready to learn how your diet can affect your central nervous system.
The Maladaptive Central Nervous System
A maladaptive CNS exhibits abnormal changes in its function that leads to amplified pain perception, impaired motor control, or other negative symptoms often associated with chronic pain conditions due to its inability to properly regulate sensory input and respond in an adaptive way. A maladaptive CNS can manifest in a variety of manners including chronic pain from central sensitization, poor descending inhibitory control, and decline in neuroplasticity.
Dietary choices can significantly impact the development and function of a maladaptive CNS by altering the way the brain processes sensory information and responds to stimuli. Research has shown that diet and exercise can have profound consequences for increasing the resilience of the CNS to injuries and for maintaining cognitive abilities. Both can influence the capability of the brain to fight disease and react to challenges.
Healthy diets, such as those high in omega-3 fatty acids and curcumin, contained in foods such as salmon and turmeric, can stimulate molecular systems that serve neuronal function and plasticity in the brain and spinal cord and can elevate levels of molecules important for daily brain function, for example, brain-derived neurotrophic factor (BDNF). Conversely, unhealthy diets that consist of high amounts of saturated fats and sugars, as prevalent in “junk food,” do the opposite. A poor diet high in processed foods and low in nutrients can trigger inflammation throughout the body, including in the central nervous system, potentially leading to increased sensitivity to pain and stress.(1)
The Enteric Nervous System
This brings us to the enteric nervous system (ENS), this second brain both stores and produces neurotransmitters, serving as the scaffolding of interplay between the ENS, SNS, and CNS. Healthy brain function and modulation are dependent upon the microbiota’s [gut bugs] activity of the vagus nerve.(2)
Microbial factors, cytokines, and gut hormones can also impact cognition by finding their way to the brain through the gut mucosal system and its local immune system. This impacts not only cognition, but also emotion, mood, stress resilience, recovery, appetite, metabolic balance, interoception, and PAIN.(3) So, by process of logic, the food we eat, or fail to eat, directly impacts the health or dysfunction of this magnificently orchestrated system. One that directly and profoundly impacts our brain, our body, and our being.
In conclusion, it is evident that our dietary choices play a crucial role in the health and function of our central nervous system. By consuming nutrient-rich foods, we can promote the resilience of our CNS and maintain cognitive abilities. On the other hand, a diet filled with processed and unhealthy foods can have detrimental effects on our brain and spinal cord, leading to inflammation and increased sensitivity. It is up to us to make mindful and deliberate choices when it comes to what we eat, as it directly impacts our overall well-being. As the saying goes, "You are what you eat," and this rings true for the health of our CNS.
Learn how to nourish our bodies and minds with wholesome and nourishing foods, and in turn, strengthen the powerhouse that is our central nervous system. As always, the conversation doesn't end here. Let's continue to explore and discuss the impact of diet on our bodies, CNS, and strive towards optimal brain health. Join Megan Pribyl for Nutrition Perspectives for the Pelvic Rehab Therapist to gain vital and clarifying information in her next course scheduled for February 22-23, 2025.
Resources
- Gomez-Pinilla F, Gomez AG. The influence of dietary factors in central nervous system plasticity and injury recovery. PM R. 2011 Jun;3(6 Suppl 1):S111-6. doi: 10.1016/j.pmrj.2011.03.001. PMID: 21703566; PMCID: PMC3258094.
- Turna, J., Grosman Kaplan, K., Anglin, R., & Van Ameringen, M. (2016). "What's Bugging the Gut in OCD?" a Review of the Gut Microbiome in Obsessive-Compulsive Disorder. Depress Anxiety, 33(3), 171-178. doi:10.1002/da.22454
- Lerner, A., Neidhofer, S., & Matthias, T. (2017). The Gut Microbiome Feelings of the Brain: A Perspective for Non-Microbiologists. Microorganisms, 5(4). doi:10.3390/microorganisms5040066
AUTHOR BIO
Megan Pribyl, PT, CMPT, CMTPT/DN, PCES

Megan Pribyl, PT, CMPT, CMTPT/DN, PCES (she/her) is a mastery-level physical therapist at the University of Kansas Health System in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic health, pregnancy, and postpartum rehabilitation – all with integration of health and wellness. She began her PT career in 2000 after graduating from the University of Colorado Health Sciences Center with her Master of Science in Physical Therapy. Prior, she earned her dual degree in Nutrition and Exercise Sciences (B.S. Foods & Nutrition, B.S. Kinesiology) in 1998 from Kansas State University. Later, she obtained her CMPT from the North American Institute of Orthopedic Manual Therapy and became certified in dry needling in 2019. Since 2015, she has been a faculty member of Herman & Wallace Pelvic Rehab Institute and enjoys both teaching and developing content. She created and instructs Nutrition Perspectives for the Pelvic Rehab Therapist offered remotely through Herman & Wallace. She also teaches Pelvic Function – Level 1, Pregnancy Rehabilitation and Postpartum Rehabilitation. She brings many years of experience and insight to all courses. As a content developer, Megan has also contributed to the Herman & Wallace Oncology Series, Pelvic Function Level 2A, as well as the Pelvic Function Series Capstone Course.
Megan’s longstanding passion for both nutritional sciences and manual therapy culminated in her creating Nutrition Perspectives for the Pelvic Rehab Therapist designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to integrate ancient and traditional practices with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation. Clinicians will come away from this course with both simple and practical integrative tools that can be immediately utilized to help clients and providers alike - along their path of healing.
Megan enjoys her many fulfilling roles as an instructor, clinician, wife, and mom to two active teenagers and owner of two rambunctious golden retrievers. She loves to read, cook, be in the great outdoors, travel, and spend time with her family and friends. She has a passion for both the mountains and the beach, exploring scientific literature, and learning all she can about the power of using nature, nurture, and nutrition to heal and sustain health.

As the holiday season approaches, it’s the perfect time to prioritize what truly matters. Join us March 28-30 at HWConnect in Seattle, WA to discover the power of networking, learning, and growth as we come together to celebrate the gift of connecting to one another. At Herman & Wallace, we believe that connection is the heart and soul of meaningful relationships, personal growth, and professional opportunities.
Networking opportunities throughout the event allow attendees to connect with like-minded individuals, share ideas, and build lasting relationships. Through structured networking sessions, informal social gatherings, and interactive activities, attendees will be able to expand their professional network and form meaningful connections with others in their industry. These networking opportunities are a highlight of HWConnect and create a supportive and collaborative environment where new friendships are formed, and partnerships can be forged.
Keynote speakers and topics include Dawn Sandalcidi, PT, RCMT, BCB-PMD lecturing on the “Development of Continence Through The Lens of The Diaphragm, Ribcage, and Pelvic Floor;” Nancy Norton, RN discussing “The Power of Humor for Pelvic Healers,” and Leticia Nieto, PsyD, LMFT, TEP who will be delving into “Trauma Responsive Care for Those We Work With and for Us.”
Other speakers and topics include:
- Ken McGee, PT, DPT - "5 Lessons from Gender-Affirming Care for All Your Clients"
- Carole High Gross, PT, DPT, PRPC - "Eating Disorders and Disordered Eating: Putting the pieces together and the hope pelvic rehabilitation can provide"
- Dr. Cindy Mosbrucker - "Endometriosis and the Evil Triplets: IC, IBS, and Levator Spasm"
- Ramona C. Horton, MPT, DPT
There is scheduled time in the vendor hall where vendor sponsor CMT will be along with other exhibitors including Intimate Rose, PacificRoots (MedRoots), Shift MD, and SRC Health. You can also opt in to morning yoga, meditation, or other breakout sessions throughout the day. Some of our favorite faculty members will be leading these sessions: Dustienne Miller, Nari Clemons, Brianna Durand, Emily McElrath, and Allison Ariail.
Past attendees have provided glowing reviews of the conference, including:
This holiday season, don't miss the opportunity to gift yourself a ticket to HWConnect. Embrace the importance of networking, learning, and growth with inspiring keynote speakers and valuable sessions. Register today and take the first step towards building lasting connections that will enrich your personal and professional life.
As author Leo Buscaglia once said, "Too often we underestimate the power of a touch, a smile, a kind word, a listening ear, an honest compliment, or the smallest act of caring, all of which have the potential to turn a life around." Make the choice to prioritize connection this holiday season and reap the benefits for years to come. Happy holidays, and we look forward to seeing you at HWConnect!


For decades, the G-spot has captivated attention, sparking debates in science and popular culture. Is it a distinct anatomical structure, a myth, or simply the same region as the 'female prostate'? While opinions differ, the heart of the discussion may be less about anatomy and more about semantics. Let’s explore the evidence and why this debate persists.
The Anatomy of the G-Spot and Female Prostate
The term 'G-spot' was introduced by German gynecologist Ernst Gräfenberg in 1950, describing a sensitive area on the anterior vaginal wall linked to the urethra and its surrounding tissues (near the bladder neck). In 1981, sexologists Beverly Whipple and John D. Perry popularized the term in their book, emphasizing that this area could enhance pleasure for some women. Notably, the G-spot was never claimed to be a single 'magic button' but rather a zone of heightened sensitivity.
Modern research has shifted focus to the female prostate, also known as Skene’s glands, which are located near the urethra. These glands share histological and functional similarities with the male prostate, contributing to urinary health, sexual arousal, and orgasm.
Evolving Perspectives on the Debate
Early Skepticism: In 2001, Terrence Hines dismissed the G-spot as a 'modern gynecologic myth,' citing inconsistent evidence and suggesting its existence was more cultural than anatomical.
Reframing as the Female Prostate: A 2022 review proposed reclassifying Skene’s glands as the female prostate. It argued that sensations attributed to the G-spot may stem from the stimulation of these glands and surrounding tissues.
A Matter of Semantics?
Does the debate boil down to terminology? Gräfenberg’s description of the G-spot and modern studies on the female prostate appear to refer to the same periurethral region. Whether we call it the G-spot or the female prostate, the area has been scientifically linked to pleasure. The controversy seems less about function and more about naming conventions.
Orgasms are Diverse: The vaginal (G-spot) orgasm isn’t the only type of orgasm or pathway to pleasure. Research indicates that approximately 70–80% of women require direct clitoral stimulation to achieve orgasm, as the clitoris contains a high concentration of nerve endings, making it particularly sensitive
Statistics on Female Orgasm:
- 40.9% of women orgasm from both clitoral stimulation and vaginal penetration.
- 35.4% orgasm solely from clitoral stimulation.
- 20.1% orgasm solely from vaginal stimulation.
- 16% report pleasurable sensations from cervical stimulation.
- 3.6% are unable to achieve orgasm.
Final Thoughts
The evidence suggests that the G-spot, as a distinct entity, is less about anatomical uniqueness and more about the interplay of surrounding tissues, including the female prostate. What’s more important than terminology is recognizing and embracing the diversity of orgasmic experiences. Whether clitoral, vaginal, cervical, or a combination, all forms of pleasure are valid and backed by science. Moving forward, let’s focus less on labels and more on understanding and normalizing the spectrum of female sexual health and pleasure.
Join Tara Sullivan in her upcoming remote course, Sexual Medicine in Pelvic Rehab, on January 18-29, 2025 if you are interested in learning more about hymen myths, squirting, G-spot, prostate gland, sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post prostatectomy; as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus.
References:
The statistics provided on female orgasm are derived from various studies, primarily published in The Journal of Sexual Medicine. Below are the references for these statistics:
- "40.9% of women orgasm from both clitoral stimulation and vaginal penetration" and "35.4% orgasm solely from clitoral stimulation"
These figures are from a study published in The Journal of Sexual Medicine, which examined women's orgasmic experiences through self-reported surveys:- Herbenick, D., Reece, M., Sanders, S. A., Dodge, B., & Fortenberry, J. D. (2010). Women's Experiences with Vaginal Penetration and Its Association with Orgasm and Sexual Pleasure: Findings from a Nationally Representative Sample of Women in the United States. The Journal of Sexual Medicine, 7(Suppl 5), 324–333. DOI: 10.1111/j.1743-6109.2010.01814.x
- "20.1% orgasm solely from vaginal stimulation"
This statistic comes from the same study, which highlighted how a subset of women can achieve orgasm through vaginal stimulation alone but noted variability based on anatomy and personal preferences. - "16% report pleasurable sensations from cervical stimulation"
This finding comes from a 2023 study published in The Journal of Sexual Medicine, which focused on sensations related to cervical stimulation:- Schubach, L. A., et al. (2023). Cervical Sensitivity and Orgasm: Self-Reported Experiences from an Online Survey. The Journal of Sexual Medicine, 20(1), 49–59. DOI: 10.1093/jsm/jqac115
- "3.6% are unable to achieve orgasm"
This figure is derived from population-level studies on sexual dysfunction and orgasm prevalence:- Kingsberg, S. A., et al. (2019). Orgasmic Dysfunction in Women: Epidemiology and Treatment Outcomes.Obstetrics and Gynecology International Journal, 27(6), 10–17.
AUTHOR BIO:
Tara Sullivan, PT, DPT, PRPC, WCS, IF
 Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage, anatomy, and physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara Sullivan, PT, PRPC, WCS, IF (she/her) started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage, anatomy, and physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara established the pelvic health program at HonorHealth in Scottsdale and expanded the practice to 12 locations across the valley. She continues treating patients with her hands-on individualized approach, taking the time to listen and educate them, empowering them to return to a healthy and improved quality of life. Dr. Tara has developed and taught several pelvic health courses and lectures at local universities in Arizona including Northern Arizona University, Franklin Pierce University, and Midwestern University. In 2019, she joined the faculty team at Herman and Wallace teaching continuing education courses for rehab therapists and other health care providers interested in the pelvic health specialty, including a course she authored-Sexual Medicine in Pelvic Rehab, and co-author of Pain Science for the Chronic Pelvic Pain Population. Dr. Tara is very passionate about creating awareness of Pelvic Floor Dysfunction and launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
In March 2024, Dr. Tara left HonorHealth and founded her company Mind to Body Healing (M2B) to continue spreading awareness on pelvic health, mentor other healthcare providers, and incorporate sexual counseling into her pelvic floor physical therapy practice. She has partnered with Co-Owner, Dr. Kylee Austin, PT.
Rehabilitation providers experience ethical conflicts every day, whether they realize it or not. Just today, I was cruising through social media on my lunch break and saw a post (edited for autonomy) that posed an ethical concern, potentially without its author even knowing. We’ll refer back to this post throughout the blog so please read:
“We have a patient at my clinic whose partner called and scheduled the appointment for the patient. My colleague did the evaluation this morning and said the partner answered all questions for the patient. The partner was inquiring about decreasing posterior pelvic floor tension for anal sex. The therapist found it strange that the partner was answering all the questions for the patient. At this time, I'm really wondering if the partner is forcing the patient to come to pelvic floor therapy and participate. How would you all handle this situation?”
You know this stopped my scroll immediately. Yes, it is a patient care question. However, this situation also brings up so many other intricacies that we encounter as pelvic health providers. I gave my reply and then read others, and this experience made me glad that Herman and Wallace offered three ethics classes talking about ethics for pelvic floor therapists to attend and be able to collaborate on issues just like the one above.
There are many ways that people like to work through ethical situations and scenarios and the ethics series with H&W usually uses the RIPS model, but just to add some new perspective, today we are going to look at the above scenario through the lens of The Critical Dialogue Method.
Delaney et al. (2024) state “Clinical ethicists bring moral reasoning to bear on concrete and complex clinical ethical problems by undertaking ethical deliberation in collaboration with others.” Their article dives into 7 steps of facilitation of such discussions among clinicians. This model is intended to help clinicians identify issues, clarify, and guide them as needed. It also acknowledges that not all ethical problem-solving is linear, chronological, or top-down.
Step One is “setting the scene.”
This is known as an opening statement. This alerts a provider’s peers about the details of the inquiry and allows those participating to be fully present to give their input. As therapists like to do, we should be working to create a safe space for the provider with the questions. In the scenario above, that post was step one as it set the scene for what the therapist had concerns about.
Step two is “listening actively and without interruption.”
This is where therapists get to put all of their experience in being active listeners with patients to the test. Keep in mind these steps don’t need to be linear so listening and replying with questions that show a person was actively listening is important. In our example, we’ve all joined a social media location to collaborate and share clinical questions, thus tacitly agreeing to be active listeners.
Step three is “gathering information and perspectives.”
This is when those active listening skills come in. When it's a social media post, this might be the comments section or even DMs! In our scenario above, therapists were great at sympathizing, empathizing, clarifying, and giving their perspective. They said things like “I’m seeing the red flags you are” and “I’ve had that happen to me and here is what happened…” Someone even kindly took the partner’s side asking if maybe they were a medical provider and that was an explanation for the potentially problematic controlling behavior. Here are some examples of statements or questions that showed a therapist was actively listening.
- What I heard you say is….
- The way you described it, what seems to have happened is…
- I’m hearing that there is some (insert emotion here - confusion, uncertainty, apprehension)....
- Can you tell us more about….
- Can you explain what you meant when you said…
(Adapted from Delaney et al., 2024)
Step four entails "closing in on the ethical question(s).”
This helps move the situation from what has been ethically feeling problematic to what can be done to resolve the issue. In this scenario, I think we can think of a few ethical questions. Some that come to mind are below:
- Is a partner allowed to make their spouse attend a therapy session potentially against their will?
- Is a spouse entitled to privacy with only their therapist if they would like this?
- Is a therapist able to intervene if they suspect abuse is occurring?
- If abuse is suspected, what next steps should be taken?
Step five is about “identifying ways of responding.”
This allows the conversation to move from “What is wrong” to “How do we resolve this?” The first part of this is exploring all of the “possible and available courses of action (Delany et al., 2024).” In this case, we’re thinking about what options are on the table, and what is reasonable while also considering the “what ifs” and things that have already been tried. In our scenario, a variety of solutions were provided to the questioning clinicians.
- Separate the couple in order to let the patient speak about their needs without pressure from the spouse.
- Provide privacy with a closed door and noise machine.
- Address the patient’s goals, reviewing them privately with the patient’s permission, to ensure they align with what their partner may have said previously.
- Check in with the patient’s referring provider to see if they have any concerns about abuse.
Step six involves “identifying and weighing the ethical pros and cons of each possible response.”
In our above scenario, we have a variety of potential pros and cons. We could offend, embarrass, or potentially lose a client by making a false allegation. We could deny a shy, anxious, or scared patient their emotional support human. We could be robbing a partner who feels guilt or worry over possibly causing their partner pain the ability to help correct it. We could also be helping a patient leave an abusive relationship or avoid having to perform an activity they don’t want to. We could be preventing domestic violence or any type of abuse. There is a spectrum, and we can create many scenarios along the way.
Step seven, the last step, is “ethically justified outcomes.”
This means that all of the previous steps have been completed (not necessarily sequentially or singularly) and then an ethically appropriate action is selected. As the RIPS model teaches us, there are many different situations and so some ethical scenarios will be very simple with just one answer, while others may be a dilemma being two potentially right answers, while others may be a whole lot of “it depends” and “I’m not sure!” In our case above, the consensus was that we definitely needed more information in order to make an informed decision on the next course of action!
If you were intrigued by taking a clinical question like this and trying to come up with a “good” solution, you may enjoy taking Ethical Concerns for Pelvic Health Professionals to sharpen, or just use, your ethical and clinical decision-making skills! The next course event is scheduled for January 19th, 2025.
Reference:
- Delany C, Feldman S, Kameniar B, et al. Critical dialogue method of ethics consultation: making clinical ethics facilitation visible and accessible. Journal of Medical Ethics. Published Online First: 08 July 2024. doi: 10.1136/jme-2024-109927 https://jme.bmj.com/content/early/2024/10/24/jme-2024-109927
Constipation, which includes rectal evacuation disorders, slow transit constipation, and IBS to name a few is one of the most common gastrointestinal disorders worldwide (1,2). The complexity of constipation and its impact on a person’s health and quality of life is often misunderstood and common treatment strategies such as diet, exercise, hydration, and stress management can be an oversimplification of what is necessary to effectively manage the disorder (1). From a rehabilitation lens, it is pivotal to prioritize the function of the nervous system when developing a treatment strategy for constipation, considering the nervous system is the central control mechanism of all functions and processes in the human body.
Dry needling, specifically, dry needling with electrical stimulation, is one of the most impactful tools we have in rehabilitation to improve the health and function of the nervous system. Dry needling has evolved from a procedure that utilizes a monofilament needle to deliver mechanical input into “trigger points” in muscle tissue to include the use of a monofilament needle for the delivery of electrical stimulation, which is often described as percutaneous electrical stimulation or neuromodulation. The use of electrical stimulation with dry needling can have a profound effect on improving the healing capacity of tissues and the overall functional recovery of the human body primarily due to the impact it has on the nervous system. Therefore, we must have a sound understanding of the neuroanatomy and physiology of any region of the body and the associated dysfunction to effectively develop and implement a treatment plan.
The gastrointestinal system is considered the most complicated system in our body in terms of the number of structures involved in function and regulation and the enormity of neurons that innervate the gastrointestinal tract, and it is yet to be fully understood (3). The enteric nervous system, which is commonly considered the third branch of the autonomic nervous system, is at the center of regulatory control of the gastrointestinal (GI) tract and precisely coordinates the function of GI neurons, glial cells, macrophages, interstitial cells, and enteroendocrine cells which drives gut motility and secretions (3). It is interesting to note that the sophistication of the enteric nervous system allows the GI tract to be able to function independently of any neural inputs from the central nervous system (3,4). However, normal physiologic functioning of the GI tract is influenced by bidirectional neuronal connections between the enteric and central nervous systems which is known as the “brain-gut-axis” (3).
Embedded in the walls of the GI tract are the myenteric and submucosal plexuses of the enteric nervous system, which innervate the GI tract and uniquely provide both excitatory and inhibitory motor neurons (4). The myenteric plexus lies between the longitudinal and circular muscle layers of the GI tract and coordinates smooth muscle movements or gut propulsions (“motility”) while the submucosal plexus is found within the connective tissues of the submucosa and regulates secretion, absorption, and blood flow in the GI tract (3,4).
The sympathetic and parasympathetic nervous systems influence the function of the GI tract primarily through integrated neuronal activity with the enteric nervous system versus direct innervation to the wall of the gut, with the exception of blood vessels and sphincters which receive direct sympathetic innervation (3).
Sympathetic inputs to the GI tract regulate secretion and motility and parasympathetic inputs to the distal colon are important for colonic motility and defecation (3).
The function of the somatic nervous system innervating key structures involved with defecation should be equally prioritized to comprehensively evaluate factors contributing to constipation. This may include spinal nerves from the thoracolumbar and sacral vertebral segments, the iliohypogastric and ilioinguinal nerves, the pudendal nerve, the levator ani nerve, and even the phrenic nerve if we are considering the innervation and function of the diaphragm and the importance of breathing mechanics and control of intraabdominal pressure during voiding.
From a treatment perspective, the most impactful window of access to modulate activity in the gastrointestinal tract using dry needling with electrical stimulation is targeting spinal nerves and associated peripheral nerves and their target organs (primarily muscle tissue) that converge with our autonomic nervous system innervating the gut (5). Additionally, electrical stimulation applied directly over the involved target tissue in the GI tract can help facilitate changes in GI function because the enteric nervous system is embedded in the wall of the GI lumen. The rationale for the use of neuromodulation to impact the function of the gastrointestinal tract is that our system is a bioelectric system, therefore, the application of electrical stimulation can have a profound impact on neuromuscular function which is interrelated with neurovascular, neuroimmune function, neuroinflammatory function, neuroendocrine function and so on (5, 6, 7). There is even evidence that electrical stimulation can impact the concentration of bacterial populations in the GI tract which can influence the overall function of the gut. Lastly, ongoing dysfunction in gastrointestinal tissue or any visceral tissue can create neuromotor dysfunction in associated somatic tissues that may include pain, tissue sensitization, abnormal muscle tone, and abnormal motor control strategies which can be effectively and efficiently treated with dry needling and electrical stimulation.
In conclusion, dry needling with electrical stimulation is one the best tools used in conjunction with traditional rehabilitation strategies to create meaningful, sustainable improvements in the function of the human body. If you want to learn more about the implementation of dry needling into your practice as it relates to constipation or gastrointestinal disorders, join us on an upcoming course!
Dry Needling and Pelvic Health: Foundational Concepts and Techniques
Dry Needling and Pelvic Health 2: Advanced Concepts and Neuromodulation
Dry Needling and Pelvic Health: Pregnancy and Postpartum Considerations
References
- Forootan M, Bagheri N, Darvishi M. Chronic constipation: A review of literature. Medicine (Baltimore). 2018;97(20):e10631. doi:10.1097/MD.0000000000010631
- Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. 2018;209(2):86-91. doi:10.5694/mja18.00241
- Sharkey KA, Mawe GM. The enteric nervous system. Physiol Rev. 2023;103(2):1487-1564. doi:10.1152/physrev.00018.2022
- Spencer NJ, Hu H. Enteric nervous system: sensory transduction, neural circuits and gastrointestinal motility. Nat Rev Gastroenterol Hepatol. 2020;17(6):338-351. doi:10.1038/s41575-020-0271-2
- Larauche M, Wang Y, Wang PM, et al. The effect of colonic tissue electrical stimulation and celiac branch of the abdominal vagus nerve neuromodulation on colonic motility in anesthetized pigs. Neurogastroenterol Motil. 2020;32(11):e13925. doi:10.1111/nmo.13925
- Zhang C, Chen T, Fan M, et al. Electroacupuncture improves gastrointestinal motility through a central-cholinergic pathway-mediated GDNF releasing from intestinal glial cells to protect intestinal neurons in Parkinson's disease rats. Neurotherapeutics. 2024;21(4):e00369.
- Jacobson A, Yang D, Vella M, Chiu IM. The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes. Mucosal Immunol. 2021;14(3):555-565. doi:10.1038/s41385-020-00368-1
AUTHOR BIO:
Tina Anderson, MS PT
 Tina Anderson (she/her) received her Master of Science in Physical Therapy in 2001 from Grand Valley State University located in Grand Rapids, Michigan. She graduated from Michigan State University in 1996 with a Bachelor of Science in Kinesiology. Tina specializes in treating patients with complex neuromusculoskeletal dysfunction including dysfunctions of the pelvic floor. Tina earned her dry-needling certification in 2006 and has been teaching dry-needling nationwide since 2008. Tina was integral in pioneering dry-needling techniques for the pelvic floor and surrounding neuroanatomical structures. She currently owns and operates a private physical therapy practice in Aspen, Colorado. Tina and her family, including their new “fur” child Beatrice, love living and playing in the Rocky Mountains!
Tina Anderson (she/her) received her Master of Science in Physical Therapy in 2001 from Grand Valley State University located in Grand Rapids, Michigan. She graduated from Michigan State University in 1996 with a Bachelor of Science in Kinesiology. Tina specializes in treating patients with complex neuromusculoskeletal dysfunction including dysfunctions of the pelvic floor. Tina earned her dry-needling certification in 2006 and has been teaching dry-needling nationwide since 2008. Tina was integral in pioneering dry-needling techniques for the pelvic floor and surrounding neuroanatomical structures. She currently owns and operates a private physical therapy practice in Aspen, Colorado. Tina and her family, including their new “fur” child Beatrice, love living and playing in the Rocky Mountains!
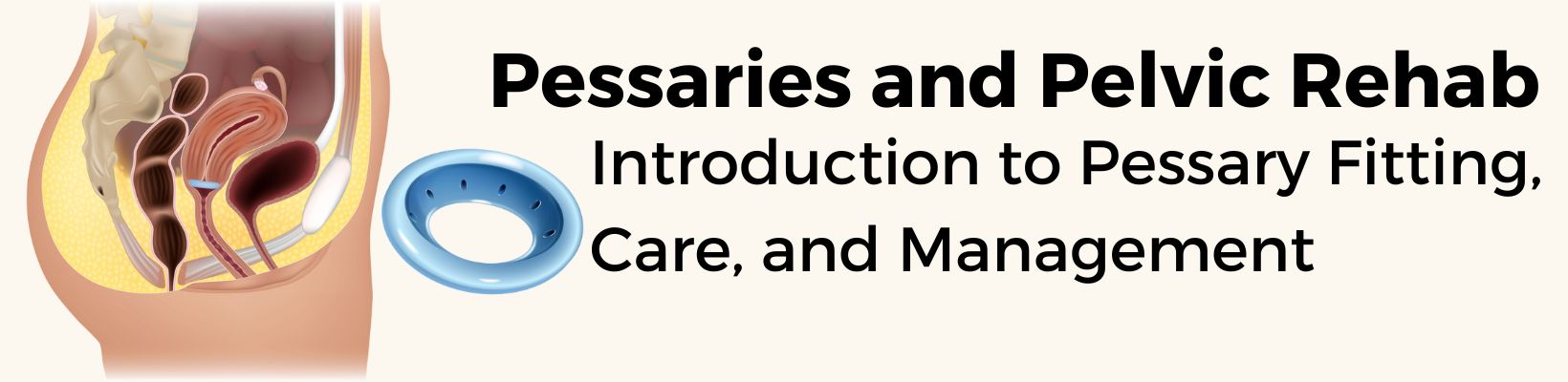
Pessaries and Pelvic Rehab includes 6 hours of pre-course video lectures that cover relevant pelvic anatomy, types of prolapse, indications and contraindications for prolapse, and medical-legal considerations for pessary fitting. The in-person portion will include labs on advanced POP assessment and assessment of vaginal dimensions, as well as provide participants the opportunity to fit various pessary types under the supervision of an instructor.
This two-day in-person course is targeted to pelvic therapists who are interested in adding pessary fitting to their clinical practice and have completed Pelvic Function Level 1 and Level 2B.
Attendees will:
- -Identify Which Patients to Refer to medical providers for pessary assessment and fitting
-Learn Indications and Contraindications for pessary fitting
-Assess Perineal and Vaginal Dimensions to determine pessary choices and fitting
-Perform a Pessary Fitting for 4 types of pessaries including ring, dish, donut, and cube
-Screen for Complications of pessary fitting and use
-Create Plans of Care that consider lifespan issues, the role of hormones, and other pelvic functions including, but not limited to, bowel, bladder, and sexual health.
Pessaries and Pelvic Rehab is perfect for practitioners eager to add pessary fitting to their clinical practice. Look for this course to be scheduled for 2025!

If you haven’t registered yet then consider this your personal invitation to join us at HWConnect 2025 in beautiful Seattle, Washington. Take advantage of this golden opportunity to network, learn, and expand your toolkit. The conference will be here before you realize it – and tickets are limited! PLUS, if you register now, you can reserve your room at a special discounted rate.
FRIDAY SPEAKER LINEUP
 Ramona Horton, MPT, DPT - "The Do Not Miss List: What many pelvic rehab therapists overlook"
Ramona Horton, MPT, DPT - "The Do Not Miss List: What many pelvic rehab therapists overlook"
Ramona Horton, MPT, DPT developed and instructs the visceral and fascial mobilization courses for HW and frequently presents at local, national, and international venues – including International Pelvic Pain Society, CSM and HWConnect- on topics relating to women’s health, pelvic floor dysfunction, and manual therapy.
KEYNOTE SPEAKER
 Dawn Sandalcidi PT, RCMT, BCB-PMD - “Development of Continence Through The Lens of The Diaphragm, Ribcage, and Pelvic Floor.”
Dawn Sandalcidi PT, RCMT, BCB-PMD - “Development of Continence Through The Lens of The Diaphragm, Ribcage, and Pelvic Floor.”
Dawn Sandalcidi PT, RCMT, BCB-PMD is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. Dawn has spoken at the World Physical Therapy Conference about pediatric pelvic floor dysfunction and incontinence, has been published in the Journals of Urologic Nursing and Section of Women’s Health. In 2018, Dawn was awarded the Elizabeth Noble Award by the American Physical Therapy Association Section on Women's Health for providing Extraordinary and Exemplary Service to the Field of Physical Therapy for Children.
SATURDAY SPEAKER LINEUP
 Ken McGee, PT, DPT - "Five Lessons from Gender-Affirming Care for All Your Clients"
Ken McGee, PT, DPT - "Five Lessons from Gender-Affirming Care for All Your Clients"
Ken McGee, PT, DPT (they/he) is a white, queer transmasculine physical therapist. They have helped hundreds of people overcome conditions related to gender affirmation and pregnancy. Ken has lectured nationally and internationally on conditions related to gender affirmation and birth tears. Their practice, B3 Physical Therapy, centers on transgender and perinatal rehabilitation.
 Dr. Cindy Mossbrucker - "Endometriosis and the Evil Triplets: IC, IBS, and Levator Spasm"
Dr. Cindy Mossbrucker - "Endometriosis and the Evil Triplets: IC, IBS, and Levator Spasm"
Dr. Cindy Mosbrucker is a nationally recognized expert in minimally invasive excision of endometriosis, as well as the diagnosis and treatment of pelvic pain in women. Dr. Mosbrucker is a sought-after resource for women with pelvic pain from all causes, including pudendal neuralgia, levator spasm, hip impingement and labral tears, and interstitial cystitis.
KEYNOTE SPEAKER
 Nancy Norton, RN - “The Power of Humor for Pelvic Healers.”
Nancy Norton, RN - “The Power of Humor for Pelvic Healers.”
Nancy Norton, RN is a Registered Nurse and comedian and has been featured on A&E, Netflix, Amazon Prime, and tours nationally - headlining clubs, festivals, conferences, and events - performing both standup comedy and delivering keynote presentations. Nancy has also toured internationally on several USO tours entertaining the troops in Europe, Asia, Iceland, and the Pacific. Nancy also hosts a weekly Podcast called "Tromedy", aimed at helping to transmute trauma responses with comedy.
SUNDAY SPEAKER LINEUP
 Carole High Gross, PT, DPT, PRPC - "Eating Disorders and Disordered Eating: Putting the Pieces Together, and the Hope Pelvic Rehabilitation Can Provide"
Carole High Gross, PT, DPT, PRPC - "Eating Disorders and Disordered Eating: Putting the Pieces Together, and the Hope Pelvic Rehabilitation Can Provide"
Carole High Gross, PT, MS, DPT, PRPC serves on the APTA Pelvic Workgroup of the Ehlers-Danlos International Consortium. Carole has a special interest in working with individuals living with eating disorders, hypermobility, and throughout the pregnancy and postpartum journey.
KEYNOTE SPEAKER
 Leticia Nieto, PsyD, LMFT, TEP - “Working Well: Trauma Responsive Care for Those We Work With and for Us.”
Leticia Nieto, PsyD, LMFT, TEP - “Working Well: Trauma Responsive Care for Those We Work With and for Us.”
Leticia Nieto, PsyD, LMFT, TEP is a leadership coach, psychotherapist, and educator specializing in liberation and equity, cultural responsiveness, motivational patterning, and evolutionary creativity. Dr. Nieto is internationally recognized for her expertise in addressing social justice concerns from a developmental ecological perspective including orienting to systemic transformation, survivance, song and poetry, relational repair, joy, radical rest, intersectional coalition, and reparative and restorative justice. Her 2010 book, Beyond Inclusion, Beyond Empowerment: A Developmental Strategy to Liberate Everyone, is an accessible analysis of the dynamics of oppression and supremacy that offers readers ways to develop skills to promote social justice.
Discounted Hotel Rooms Available Until January 1, 2025
HWConnect 2025 will take place entirely at the Hilton Seattle Airport & Conference Center in Seattle, WA, and we would love for you to stay at the hotel for ease of attending all sessions and social events and have secured a room block and special pricing for conference attendees starting at $167.
The hotel is accessible from the Seattle-Tacoma Airport by walling across the skybridge by the SeaTac light rail station, making it very convenient for those flying in or attending from the greater Seattle area. We Look Forward to Seeing You at HWConnect!
HWConnect 2025 is scheduled for March 28-30, 2025 in Seattle Washington.
When it comes to treating defecatory disorders, particularly fecal incontinence and chronic constipation, innovation can be a game changer. Enter rectal balloon catheters—a tool that, despite initial discomforting imagery, offers significant benefits for patients struggling with these conditions.
At first glance, the thought of a balloon being inserted into the anus may provoke apprehension. However, it's essential to understand that the size of these balloons is smaller than that of an average bowel movement, making their use far more manageable than one might expect. The primary role of these catheters is to provide sensory retraining in the anal canal, an aspect of treatment that is otherwise challenging to achieve.
Numerous studies have highlighted the effectiveness of rectal balloon catheters. For instance, research by Bright et al. in 2005 showed that when patients squeeze to retain a balloon, it effectively mimics the physiology of defecation. This process aids in improving maximal anal squeeze pressures, a vital aspect of bowel control.
As the study states, “External anal sphincter contraction is difficult for some patients to perform on request. With traction on a balloon catheter, anal squeeze pressures improved in most patients. This indicates that many patients perform maximal anal squeeze pressures better once that muscle group has been tested in a more normal physiological function.”
This revelation underscores the potential of balloon catheters in not only retraining muscle function but also in enhancing patient confidence during bowel movements.
The key to success with rectal balloon catheters lies in careful patient selection. Not every patient will benefit from this approach, but for those who do, the results can be transformative. Many have reported significant improvements in their ability to manage symptoms and regain control over their bowel functions.
Are you still feeling apprehensive about integrating balloon catheters into your practice?
It’s understandable. Take a course to build your confidence and learn how to use this remarkable clinical tool. In Anorectal Balloons: Introduction and Practical Applications you will learn the research that supports the use of balloon catheters, as well as evaluation and treatment techniques using anorectal balloons. You will participate in a lab to ensure proper handling. Anorectal Balloons: Introduction and Practical Applications is an online course lasting 5.5 hours. Join me on December 14 to learn more about anorectal balloon catheters so that you can add this tool to your clinical repertoire.
Rectal balloon catheters may initially seem daunting, but they represent an essential advancement in the treatment of defecatory disorders. With the right training and patient selection, you can add this remarkable clinical tool to your repertoire and make a profound difference in your patients' lives.
Resources:
Bright T, Kapoor R, Voyvodich F, Schloithe A, Wattchow D. The use of a balloon catheter to improve evaluation in anorectal manometry. Colorectal Dis. 2005 Jan;7(1):4-7. doi: 10.1111/j.1463-1318.2004.00698.x. PMID: 15606577.
AUTHOR BIO:
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman & Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.
Prostate cancer remains one of the most commonly diagnosed cancers among men, yet the pathway to effective screening can be fraught with confusion and uncertainty. With varying recommendations from different health organizations and a multitude of testing options available, patients often find themselves unsure about when and how to pursue screening. Two of the screening methods often recommended are the Prostate-Specific Antigen (PSA) test and MRI.
Prostate-Specific Antigen (PSA) Testing
Screening for prostate cancer has been confusing for some patients in terms of what is recommended. Prostate-Specific Antigen (PSA) is used by some providers, but some patients are unsure when to proceed with testing. The US Preventative Services Task CDC recommends that the use of PSA screening between in men aged 55 to 69 should be an individual choice, however, it should not be performed in men over the age of 70. Other websites recommend having a discussion for screening between individuals and their medical provider, which may include PSA testing, starting at 50, earlier if there is a risk present.
Some of the issues for screening for prostate cancer with PSA include false positives that require additional testing and biopsy, overdiagnosis, and overtreatment. The treatment for prostate cancer has a lot of side effects including urinary incontinence, erectile dysfunction, and bowel issues. This is concerning when quality of life can be greatly influenced by these side effects.
MRI
With improved technology, MRI is emerging as a nice screening tool for prostate cancer. MRI has shown promising results. MRI does identify cancer before it is too advanced. It also is decreasing the number of patients that are diagnosed with clinically insignificant cancer, which means fewer patients are being overtreated. According to Hugosoon et al in 2024, using MRI to decide if a biopsy should be performed “eliminated more than half of diagnoses of clinically insignificant prostate cancer,” while the risk of being diagnosed at an incurable stage was “very low.”1 The use of MRI is more than for diagnosis at the pre-biopsy stage but is progressing to screening, active surveillance, clinical staging, and detection of recurrent disease. 2 Artificial intelligence (AI) based algorithms are being explored for the use of detecting and characterizing prostate cancer on an MRI. These are showing promising results as well, particularly with decreasing false positives.3
As the landscape of prostate cancer screening evolves, it is crucial for patients and healthcare providers alike to remain informed and engaged in discussions about the best approaches to diagnosis and treatment. The decision to undergo screening should not be taken lightly; it requires a thorough understanding of the benefits and risks associated with various testing methods, including PSA testing and the promising role of MRI.
In an era where technology, including artificial intelligence, is reshaping how we approach cancer detection, it’s imperative to remain proactive and adaptable. By prioritizing education and open communication, we can ensure that the journey through prostate cancer screening and treatment is navigated with confidence and clarity.
Join us in Oncology of the Pelvic Floor Level 1 (OPF1) to receive an introduction to oncology of the pelvic floor, or Oncology of the Pelvic Floor Level 2A (OPF2A) for a deeper understanding of prostate cancer and empower yourself or your patients with the knowledge needed for informed health choices. In OPF1, we address issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis while in OPF2A, we cover topics of prostate cancer, testicular and penile cancers, as well as colorectal and anal cancers. You will learn the latest diagnostic testing for each type of cancer as well as medical treatment and how that treatment can influence our patients’ bodies. Hands-on treatment techniques that can be used in the rehabilitation process are learned. Join us to learn more about prostate cancer and more!
Oncology of the Pelvic Floor Level 1 is next offered January 11-12, 2025.
Oncology of the Pelvic Floor Level 2A is next offered March 8-9, 2025.
Resources
- Hugosson J, Godtman RA, Wallstrom J, et al. (2024). Results after four years of screening for prostate cancer with PSA and MRI. New England Journal of Medicine. 391; 1083-1095.
- Trecarten S, Sunnapwar AG, Clarke GD, Liss MA. (2024). Chapter Three- Prostate MRI for the detection of clinically significant prostate cancer: update and future directions. Advances in Cancer Research. Vol 161. 71-118.
- Roubiere O, Jaouen T, Baseilhac P, et al. (2023). Artificial intelligence algorithms aimed at characterizing or detecting prostate cancer on MRI: How accurate are they when tested on independent cohorts?- A systematic review. Diagnostic and Interventional Imaging. Vol 104 (5): 221-234.
AUTHOR BIO:
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman & Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.

In 2024, the Journal of Women’s and Pelvic Health Physical Therapy published an article on stress urinary incontinence (SUI) and parous runners. It specifically looked at functional lower extremity strength along with running mechanics. The study had 22 participants who performed functional strength tests, including a 30-second single-leg sit-to-stand test and a 10-minute treadmill run with a cadence assessment, and also filled out SUI questionnaires. The higher questionnaire scores had a positive correlation between increased ground contact times and slower cadences.
There was no correlation between the 30-second single-limb sit-to-stand test and higher SUI questionnaire scores. However, multiple other studies referenced in this article have shown increased SUI with decreased hip external rotation and abduction strength compared to those without SUI. The 30-second single-limb sit-to-stand test has not been validated as a good measure of hip strength at this time.
In the remote course The Runner and Pelvic Health by Leeann Taptich and Aparna Rajagopal, they will discuss running mechanics, faults of running including ground reaction forces, contact times, and cadence along with functional strength assessments that can be performed for parous female runners with reported SUI. Please join them on December 14, 2024 for this course.
Reference:
Ron NJ, Dolbinski SC, Hodonicky EG, Middlebrook DO, Olmstead SR, Olsen SL, Ron ED. Hollman JH. Associations between running mechanics, functional lower extremity strength, and stress urinary incontinence in parous female runners. Journal of Women’s & Pelvic Health Physical Therapy. 2024; 48(3): 147-153.
AUTHOR BIO:
Leeann Taptich DPT, SCS, MTC
 Leeann Taptich (she/her) has been a physical therapist since 2006. She graduated with a BS in Kinesiology from Michigan State University and a Doctorate of Physical Therapy from the University of St Augustine. In 2009, she earned her Manual Therapy from the University is St Augustine and her board certification as a Sports Certified Specialist in 2018.
Leeann Taptich (she/her) has been a physical therapist since 2006. She graduated with a BS in Kinesiology from Michigan State University and a Doctorate of Physical Therapy from the University of St Augustine. In 2009, she earned her Manual Therapy from the University is St Augustine and her board certification as a Sports Certified Specialist in 2018.
Leeann leads the Sports Physical Therapy team at Henry Ford Macomb Hospital in Michigan where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete. With her combination of credentials and her exposure to pelvic health, she is able to use a very eclectic but complete approach in her treatment of orthopedic and sports patients. With the hospital system, she is involved with the community promoting health and wellness at local running competitions and events.
Leeann is passionate about educating and teaching and has assisted in teaching multiple courses at the local State University PT department. She is co-chair of the continuing education committee at her hospital where she writes and develops courses. Leeann lives in the metro Detroit area with her husband and 2 children. She enjoys hiking, traveling, and watching football.