Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sitting to standing. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: (1)
- Anterior Tip: Iliococcygeus and pubococcygeus, Sacrococcygeal ligament
- Lateral: Coccygeal muscles that run parallel with the sacrospinous ligament
- Posteriorly: Fibers of gluteus maximus and sacrotuberous ligament
Along with serving as a major attachment site for the above structures it provides support for weight bearing in the seated position and provides structural support for the anus. However, the coccyx is only 10% weight-bearing, so what seems to go wrong that this bone is taking the brunt of the weight-bearing? Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall or an internal trauma like a difficult childbirth (1,2).
In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulted in coccyx pain were from the use of instruments such as forceps delivery or vacuum-assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth (3). Other causes of coccyx pain can be non-traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction (1).
When assessing a patient with coccyx pain, it is also of the utmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retro rectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign and if excision is necessary. Quite often, these masses can be felt as a bulge on rectal examination (4, 5).
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain (1). Special wedge-shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain.
Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx (1). Unique taping methods demonstrated in video by Dr. Abbate can be used as a follow-up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroiliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered. Luckily, conservative treatment is successful in about 90% of cases (1).
Join Lila Abbate in her upcoming Coccydynia and Painful Sitting remote course on December 14th. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
References:
- Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
AUTHOR BIO
Lila Abbate, PT, DPT, OCS, WCS, PRPC

Lila Abbate (she/her) is the Director/Owner of New Dimensions Physical Therapy with locations in Roslyn, Long Island, and the Noho Section of New York City. Dr. Abbate graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release.
She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series and the Pregnancy and Postpartum Rehabilitation courses. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
She is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, and the International Pelvic Pain Society. Dr. Abbate is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.

Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sitting to standing. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: (1)
- Anterior Tip: Iliococcygeus and pubococcygeus, Sacrococcygeal ligament
- Lateral: Coccygeal muscles that run parallel with the sacrospinous ligament
- Posteriorly: Fibers of gluteus maximus and sacrotuberous ligament
Along with serving as a major attachment site for the above structures it provides support for weight bearing in the seated position and provides structural support for the anus. However, the coccyx is only 10% weight-bearing, so what seems to go wrong that this bone is taking the brunt of the weight-bearing? Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall or an internal trauma like a difficult childbirth (1,2).
In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulted in coccyx pain were from the use of instruments such as forceps delivery or vacuum-assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth (3). Other causes of coccyx pain can be non-traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction (1).
When assessing a patient with coccyx pain, it is also of the utmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retro rectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign and if excision is necessary. Quite often, these masses can be felt as a bulge on rectal examination (4, 5).
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain (1). Special wedge-shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain.
Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx (1). Unique taping methods demonstrated in video by Dr. Abbate can be used as a follow-up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroiliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered. Luckily, conservative treatment is successful in about 90% of cases (1).
Join Lila Abbate in her upcoming Coccydynia and Painful Sitting remote course on December 14th. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
References:
- Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
AUTHOR BIO
Lila Abbate, PT, DPT, OCS, WCS, PRPC

Lila Abbate (she/her) is the Director/Owner of New Dimensions Physical Therapy with locations in Roslyn, Long Island, and the Noho Section of New York City. Dr. Abbate graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release.
She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series and the Pregnancy and Postpartum Rehabilitation courses. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
She is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, and the International Pelvic Pain Society. Dr. Abbate is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.

The year was 1998 - my fellow classmates and I converged upon our journey in graduate school to become physical therapists. In our first semester, we shouldered a heavy load of coursework and were memorably immersed in a battle between courses taught by our anatomy and histology professors. Both professors claimed stake to the title of teaching the “most important course in the curriculum.” The connection between anatomy and physical therapy was clear and specific. But there were moments when the connection between histology and physical therapy seemed less relevant and the demands from our histology professor obtuse. The battle between courses played out in both the cadaver lab and the histology slide viewing rooms. My classmates and I found ourselves compelled to pour over both anatomy and histology with focused intensity; the figurative competition became a grind.
We shared in collective moans and groans surrounding the challenge of having a histology professor who thought so highly of cellular structure and function and insisted our appreciation of the topic should equal that of learning anatomy. This professor made exceedingly clear to each of us: “You MUST know what a normal cell looks like to understand basic anatomy and physiology. If you don’t know what normal looks like, then you’ll never know what abnormal looks like.” We studied muscle slides, fibrocartilage slides, hyaline cartilage slides, endothelium slides, neuron slides, bone slides, tendon slides….and on and on and on. We counted mitochondria. We compared normal and abnormal. Over and over again.
Little did I know - our future understanding of health would literally hinge upon such things. Normal and abnormal cellular health. Intra- and Inter-cellular (mis)communication. Inter-cellular barrier integrity. Mitochondrial (dys)function.
In September 2024, Dr. Casey Means shined a spotlight on our country’s health crises by participating in a non-partisan roundtable discussion titled “American Health and Nutrition – a Second Opinion” – elucidating in a national forum the stark reality of the dismal nutrition situation that plagues our country resulting in equally dismal national health statistics. We are all witnesses to this health catastrophe. She also recently published “Good Energy,” a call-to-action she co-authored with her brother Cally Means. In the roundtable discussion and in the book, Dr. Means eloquently describes the driver of all health and disease states - the status of cellular function – and that this is foundationally driven by nutrition or lack thereof. Based on the overwhelming evidence in the literature I’ve read through the years, and compiled to create “Nutrition Perspectives in Pelvic Rehab,” I couldn’t agree with her more.
And I guess this is where I admit our histology professor was on to something.
As rehab professionals, we absolutely care about what cells look like, act like, move like, and feel like. We may not realize it, but cellular health or dysfunction can dictate if our patients have low energy, metabolic dysregulation (diabetes, obesity, fatty liver disease), neurodegenerative diseases like Parkinson’s, Alzheimer’s, dementia & peripheral neuropathy (Qiao et.al., 2024; Sabui et.al., 2022), neurocognitive changes, (Shatalina et.al., 2024) cancer, chronic pain, or even dysregulation of the gut-brain axis (found in conditions such as IBS). Cellular dysfunction is at the foundation of all of these conditions and their sequelae. We also may not realize it, but when we palpate tissue that is painful, inflamed, tense, tight, dyscoordinated, or find joints to be irritated (Seewald et.al. 2023) cellular dysfunction may be making itself manifest. Sarcopenia, muscle degeneration and weakness, also has underpinnings in metabolic and thus cellular dysregulation (Daily &Park, 2022; Xie & Huang, 2024). Chronic systemic inflammation is by definition cellular dysregulation. (Kharrazian, 2022)
And finally, we also may not fully realize the decidedly negative impact our standard American diet has on each and every condition just listed, or more precisely, on our cellular health. Without normal cellular function our bodies will devolve into chaos - otherwise known as disease states.
As rehab professionals, we need to know all we can about anatomy, biomechanics, and therapeutic intervention. In my journey, it was the requisite histological training combined with my studies in nutritional sciences that allowed me to see how the “peripheral” topics of nutrition, health, and cellular function intersected in vivid clarity early in my career. This fueled my long-standing passion to share this information with other healthcare providers through the creation of “Nutrition Perspectives.”
This intersection should inform our intention as we steer towards solutions to the overarching American health crisis while helping our clients – one conversation at a time. “Nutrition Perspectives in Pelvic Rehab” (NPPR) provides practical steps to navigate a path forward to improve digestive health, gut health, and overall health. First, we must bravely confront the magnitude and complexity of the problem as we equip ourselves with working knowledge of functional nutrition as shared in NPPR.
Optimizing cellular health can positively influence everything we care about as rehab providers. I might argue in this context – that learning about functional nutrition may be equivalent in importance to anatomy and histology! More fairly – the intersection of anatomy, histology & nutrition will be the foundation upon which the future of health and wellness, and hopefully healthcare will eventually be built.
Nutrition Perspectives in Pelvic Rehab is nearing its 10th anniversary– 10 years of sharing profoundly important nutritional concepts that impact each one of us and the clients we serve. As the body of evidence explodes, the essence of the message within NPPR is unwavering and may just become your “most important course in the curriculum.” Nutrition matters deeply – all the way down to the cellular level.
Come learn the hows and whys in an upcoming offering of Nutrition Perspectives in Pelvic Rehab – available in remote format on the following dates: Dec 7-8, 2024; Feb 22-23, 2025; June 7-8, 2025; Oct 11-12, 2025 & Dec 6-7, 2025.
Resources:
- American Health and Nutrition – A Second Opinion. https://rumble.com/v5fy7bv-american-health-and-nutrition-a-second-opinion.html
- Daily JW, Park S. Sarcopenia Is a Cause and Consequence of Metabolic Dysregulation in Aging Humans: Effects of Gut Dysbiosis, Glucose Dysregulation, Diet and Lifestyle. Cells. 2022 Jan 20;11(3):338. doi: 10.3390/cells11030338. PMID: 35159148; PMCID: PMC8834403.
- Kharrazian D. Functional Medicine Approaches to Neurodegeneration. Phys Med Rehabil Clin N Am. 2022 Aug;33(3):733-743. doi: 10.1016/j.pmr.2022.04.011. PMID: 35989061.
- Means, C; Means, C. Good Energy – the Surprising Connection between Metabolism and Limitless Health. Avery. May 2024.
- Qiao L, Yang G, Wang P, Xu C. The Potential Role of Mitochondria in the Microbiota-Gut-Brain Axis: Implications for Brain Health. Pharmacol Res. 2024 Sep 25:107434. doi: 10.1016/j.phrs.2024.107434. Epub ahead of print. PMID: 39332752.
- Sabui A, Biswas M, Somvanshi PR, Kandagiri P, Gorla M, Mohammed F, Tammineni P. Decreased anterograde transport coupled with sustained retrograde transport contributes to reduced axonal mitochondrial density in tauopathy neurons. Front Mol Neurosci. 2022 Sep 30;15:927195. doi: 10.3389/fnmol.2022.927195. PMID: 36245925; PMCID: PMC9561864.
- Seewald LA, Sabino IG, Montney KL, Delco ML. Synovial fluid mitochondrial DNA concentration reflects the degree of cartilage damage after naturally occurring articular injury. Osteoarthritis Cartilage. 2023 Aug;31(8):1056-1065. doi: 10.1016/j.joca.2023.03.013. Epub 2023 Apr 6. PMID: 37028640; PMCID: PMC10524327.
- Shatalina E, Whitehurst TS, Onwordi EC, Gilbert BJ, Rizzo G, Whittington A, Mansur A, Tsukada H, Marques TR, Natesan S, Rabiner EA, Wall MB, Howes OD. Mitochondrial complex I density is associated with IQ and cognition in cognitively healthy adults: an in vivo [18F]BCPP-EF PET study. EJNMMI Res. 2024 Apr 17;14(1):41. doi: 10.1186/s13550-024-01099-1. PMID: 38632153; PMCID: PMC11024075.
- Xie X, Huang C. Role of the gut-muscle axis in mitochondrial function of aging muscle under different exercise modes. Ageing Res Rev. 2024 Jul;98:102316. doi: 10.1016/j.arr.2024.102316. Epub 2024 May 3. PMID: 38703951.
AUTHOR BIO
Megan Pribyl, PT, CMPT, CMTPT/DN, PCES

Megan Pribyl, PT, CMPT, CMTPT/DN, PCES (she/her) is a mastery-level physical therapist at the University of Kansas Health System in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic health, pregnancy, and postpartum rehabilitation – all with integration of health and wellness. She began her PT career in 2000 after graduating from the University of Colorado Health Sciences Center with her Master of Science in Physical Therapy. Prior, she earned her dual degree in Nutrition and Exercise Sciences (B.S. Foods & Nutrition, B.S. Kinesiology) in 1998 from Kansas State University. Later, she obtained her CMPT from the North American Institute of Orthopedic Manual Therapy and became certified in dry needling in 2019. Since 2015, she has been a faculty member of Herman & Wallace Pelvic Rehab Institute and enjoys both teaching and developing content. She created and instructs Nutrition Perspectives for the Pelvic Rehab Therapist offered remotely through Herman & Wallace. She also teaches Pelvic Function – Level 1, Pregnancy Rehabilitation and Postpartum Rehabilitation. She brings many years of experience and insight to all courses. As a content developer, Megan has also contributed to the Herman & Wallace Oncology Series, Pelvic Function Level 2A, as well as the Pelvic Function Series Capstone Course.
Megan’s longstanding passion for both nutritional sciences and manual therapy culminated in her creating Nutrition Perspectives for the Pelvic Rehab Therapist designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to integrate ancient and traditional practices with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation. Clinicians will come away from this course with both simple and practical integrative tools that can be immediately utilized to help clients and providers alike - along their path of healing.
Megan enjoys her many fulfilling roles as an instructor, clinician, wife, and mom to two active teenagers and owner of two rambunctious golden retrievers. She loves to read, cook, be in the great outdoors, travel, and spend time with her family and friends. She has a passion for both the mountains and the beach, exploring scientific literature, and learning all she can about the power of using nature, nurture, and nutrition to heal and sustain health.
Overall prevalence of pelvic floor dysfunction (PFD) ranges from 14.7%-45% within the athletic population (Culleon-Quinn 2022). Additional evidence supports the incidence of PFD within this population (Culleon-Quinn 2022, Rebullido et al 2021, Rodríguez-López et al 2020, Nygaard & Shaw 2016). The athletic population is disproportionately in need of pelvic health services – but much like the general population, many athletes are not aware of the signs and symptoms of PFD, so they may not know to seek care (Bosch-Donate et al, 2024, Cardoso et al, 2018).
In a recent publication in the International Journal of Sports Physical Therapy, a group of student and faculty researchers investigated a method of screening collegiate athletes for PFD as a component of the DPT students’ project to promote health in their communities. The intent of the study was to identify the incidence of PFD in collegiate athletes, assess for awareness of PFD, and explore psychosocial factors related to PFD in athletes.
Taking place at the DPT students’ university, student-athletes were recruited from multiple sports teams to participate in a generalized pelvic floor screening in two phases. In the first phase, students completed a demographics section as well as the Cozean Pelvic Dysfunction Screening Tool, a ten-item subjective screening tool. Athletes who scored a “3” or greater on the Cozean Pelvic Dysfunction Screening Tool were then invited to participate in the second phase of screening: a simple, external pelvic floor muscle (PFM) function assessment, performed by the researchers. The researchers chose this score due to the 91% specificity indicating possible PFD in individuals who score 3 or greater on the tool. (Cozean, N 2018)
The researchers performed an external PFM function assessment that included palpation of the coccyx over clothing. This external assessment allowed for improved comfort of the athletes as well as improved efficiency in the performance of the assessment. Coccygeal motion palpation was previously found to be valid when performed by clinicians without formal pelvic health training and was correlated with activation patterns shown via real-time ultrasound, demonstrating 94% sensitivity and 79% specificity in identifying PFM activation patterns (Maher & Iberle, 2020).
For the PFM function assessment, the researchers palpated the tip of the coccyx with the athlete in a seated position as described in the original 2020 study. Participants were then instructed to contract, release, and lengthen their pelvic floor muscles while the student researchers palpated the motion of the coccyx. As described in the validity study, student researchers identified whether or not the coccyx moved anteriorly, posteriorly, or not at all to infer the activity of the PFM. If the student researchers were unsure, the faculty research leader, a Board-Certified Women’s Health Clinical Specialist, and a Certified Pelvic Rehabilitation Practitioner were available on-site to confirm findings.
Once the coccygeal motion palpation was completed, the researchers assigned the athletes into one of three classifications of suspected PFM impairment:
- “normal PFM activity” indicating that the coccyx moved posteriorly with PFM lengthening and anteriorly with PFM contraction
- “increased tone/overactive PFM activity” indicating that the coccyx did not move posteriorly during lengthening, but did move anteriorly with contraction
- “decreased tone/underactive PFM activity” indicating that the coccyx moved posteriorly with lengthening, but did not move anteriorly with contraction
The researchers then shared information with the student athletes pertaining specifically to the suspected PFM impairment identified. Athletes were given information about the PFM, general exercises to consider, as well as resources for finding a trained PT if they desired more formal assessment and interventions.
A quarter (24.5%) of participants scored a “3” or greater on the subjective screening tool, with positive correlations with increased age, self-identified female gender, and increased knowledge of PFD. Swimming athletes were also found to have an increased incidence of positive screening scores as compared to other sports. Following coccygeal motion testing, 54% of the participants were identified as demonstrating “decreased tone/underactive PFM activity” and 39% were identified as demonstrating “increased tone/overactive PFM activity”.
Of the 13 athletes who scored positive on the Cozean Pelvic Dysfunction Screening Tool, 12 also demonstrated objective signs of increased or decreased tone of the PFM during coccygeal motion palpation, (92.3%) reinforcing the Cozean tool’s effectiveness as a simple subjective screening tool for PFD. Additionally, coccygeal motion palpation is a simple, non-invasive, objective screening method that can be taught to clinicians who do not have formal training in pelvic health, allowing for screening to be performed efficiently by all clinicians, and addressing a critical barrier to receiving care.
The results of this study highlight that PFD is often present in physically fit individuals who are competitive athletes. Additionally, 69% of the athlete participants presenting with suspected PFD reported feelings of embarrassment, anxiety, worry, or annoyance with regard to their symptoms, and 62% reported feelings of frustration. 69% of the athletes presenting with suspected PFD reported feeling as though PFD had an effect on athletic performance and 77% reported that PFD had an impact on their personal life. These qualitative findings illustrate that beyond the physical impact of PFD, there is a psychosocial impact as well. By implementing a PFD screening process for athletes, clinicians without formal pelvic health training can help identify athletes who may be experiencing PFD and serve as the initial point of contact to help athletes function better, both on and off the playing field.
By performing screening with a subjective screening tool and an external pelvic floor muscle assessment, the researchers were able to identify athletes demonstrating subjective and objective characteristics of PFD efficiently, while also emphasizing participant comfort. Taking this innovative approach to PFM assessment, it is much more feasible to integrate pelvic floor screening into a standard sports screening performed by a general physical therapist or athletic trainer. Once identified, those professionals can facilitate referral to a physical therapist with pelvic health training for more thorough assessment and treatment. This would allow more athletes with PFD to receive access to care and could have implications for both athletic performance as well as quality of life.
Interested in learning more? Come and see this group speak at APTA’s Combined Sections Meeting in 2025 where they’ll present an educational session about the study and discuss the implementation of this screening process to help ensure that athletes with PFD are identified sooner and receive access to care efficiently.
You can read the published research article, "Screening for Incidence and Effect of Pelvic Floor Dysfunction in College-Aged Athletes," here: https://ijspt.org/screening-for-incidence-and-effect-of-pelvic-floor-dysfunction-in-college-aged-athletes/.
AUTHOR BIO
Ashlie Crewe Campitella, PT, DPT, WCS, PRPC
 Dr. Ashlie Crewe Campitella earned her Bachelor of Psychology and Doctorate of Physical Therapy at Gannon University prior to beginning her pelvic health training. She is a board-certified women’s health clinical specialist (WCS) and has her certification as a pelvic health practitioner (PRPC) through the Herman and Wallace Pelvic Rehabilitation Institute.
Dr. Ashlie Crewe Campitella earned her Bachelor of Psychology and Doctorate of Physical Therapy at Gannon University prior to beginning her pelvic health training. She is a board-certified women’s health clinical specialist (WCS) and has her certification as a pelvic health practitioner (PRPC) through the Herman and Wallace Pelvic Rehabilitation Institute.
Ashlie has developed pelvic health continuing education that is comprehensive and inclusive of all genders through the Institute of Advanced Musculoskeletal Treatments, where she is now a lead instructor. She also serves as the Pelvic Health Development Program Coordinator for Upstream Rehabilitation Institute. Additionally, Ashlie is a member of the International Pelvic Pain Society, and the Global Pelvic Health Alliance and serves as an adjunct faculty member at Lebanon Valley College, as well as on the medical advisory board for the Lichen Sclerosus Support Network. She remains in clinical practice in Harrisburg, Pennsylvania, treating patients of all ages and genders with pelvic health complaints, with a special focus on implementing a pain neuroscience and trauma-informed approach to pelvic health treatment.

Boundaries, Self-Care, and Meditation Part 1 and Boundaries, Self-Care and Meditation Part 2, scheduled for November 23, are instructed by Nari Clemons, PT, PRPC and Jenna Ross, MSPT, BCB-PMD, PRPC.
Women are often socialized to be these kinds of words: sweet, likable, giving, generous, helpful, and accommodating. If that bend of conditioning is particularly strong, it shapes our relationships and our career choices. We often choose a career that makes us feel like we are being sweet, helpful, and generous. These traits serve others around us well, and they may increase our likability with others. We begin to see our likability as how much we embody these traits, and we can see our worth to others and ourselves as how much we show up in this one-dimensional way to others.
Taken to an extreme, this starts to look like being uber-available for patients calling them on our own time, emailing from home, running over in sessions to give the patient everything they could possibly get from a session, adding in hours to accommodate a patient, writing our notes during our lunchtime, and finding that resource for our patient by searching the web for an hour.
“Tis better to give than receive” or “giving them the shirt off our back” may be mantras we use or grew up with. But is it really true? Is giving more than we receive actually sustainable as a model? And if you give someone the shirt off your back, what would you wear? So many of the models we are raised to see as virtuous are actually rooted in martyrdom and are the hallmarks of poor boundaries.
When we hyper-inflate the “likable” characteristics of ourselves, it is often because we are deeply afraid of being seen as selfish, unlikable, or worst of all, a bi#ch. But why? We make these traits shadows…the traits to deny in ourselves and go to extreme lengths to hide from ourselves and others. Maybe instead, these are the very traits that can help us to understand where we need to set a boundary, rest, or realize we really don’t want to say yes to that added demand.
They can remind us of our energy limits and draw lines that help us have more room for joy, fun, and self-care. If we could honor these shadow traits as helpful protectors of ourselves, we could consider our happiness and balance equally as important as our patients’ happiness and balance. We could find ways to leave work on time to make it to that fun dance class, and we could empower our patients to have greater self-sufficiency. Often, when we are conflicted or tired, we can do well to ask ourselves, “What would a selfish bi#ch do?” The answer is usually what our being needs for balance, but we are too afraid to embrace our shadow to acknowledge our deeper needs and wants.
By ridding ourselves of the need to be seen as syrupy sweet (and utterly drained) and by embracing self-care that may look harsh or selfish to others, we can empower ourselves to have better boundaries. This can also help our patients as we model balanced caregiving, without self-sacrifice. By embracing and honoring these important traits of self-care, self-protection, and acknowledging our needs, we set the stage for less burnout and more healthy relationships in life. So, next time you are overwhelmed by the number of obligations you have or the time you are bleeding energy for others, ask yourself “What would my selfish bi#ch do?” And, if you manage to hear and honor her, high-five yourself as you strut to better self-care and integrated self-love.
Enter the course I co-wrote and teach with Jenna Ross - Boundaries, Self-Care, and Meditation Part 2. This course was born out of our own personal and professional struggles and our journey to having a life and a practice that we love and can sustain. This class provides a safe space to facilitate deep, personal, and professional transformation through evidence-based information and practices. Join us in Boundaries, Self-Care, and Meditation Part 2 on November 23 to learn new strategies to address both oneself and one's patients with a mind, body, and spirit approach.
AUTHOR BIO
Nari Clemons, PT, PRPC

Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment, as well as Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jen Vande Vegte, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jen Vandevegte. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari’s passions include teaching students how to use their hands more receptively and precisely for advanced manual therapy skills while keeping it simple enough to feel successful. She also is an advocate for therapists learning how to feel well and thrive as they care for others, which is a skill that can be developed. “Basically, I love helping therapists learn to help themselves and others more while having a lot of fun doing it”. Nari lives in Portland Oregon, where she runs a local study/mentoring group and has a private practice, Portland Pelvic Therapy. Her interests include meditation, working out, nature, and being constantly humbled from raising her three amazing teenagers!
Discover Inclusive Care for Gender and Sexual Minorities in this interview with Brianna Durand, an expert in inclusive care for gender and sexual minorities. In this insightful video, Durand discusses the importance of tailored and compassionate healthcare for individuals who identify as LGBTQ+.
Gain valuable insights as Durand shares her extensive knowledge on the unique challenges faced by these communities and how to provide comprehensive and inclusive care. With a focus on creating safe and welcoming spaces for all individuals, this video provides valuable information for healthcare professionals and anyone looking to support the LGBTQ+ community.
Are you looking to improve your knowledge and understanding of inclusive care for the LGBTQ+ community? Look no further! Our remote course on Inclusive Care for Gender and Sexual Minorities is here to guide you through the most important principles and best practices in providing compassionate and equitable care for individuals of all gender identities and sexual orientations.
Led by industry expert, Brianna Durand, this comprehensive course will cover topics such as terminology, cultural competency, and the unique healthcare needs of gender and sexual minorities. By the end of the course, you will have the tools and resources to confidently offer inclusive and affirming care to all patients, regardless of their gender or sexual identity.
Don't miss this opportunity to learn from one of the top leaders in inclusive healthcare. Enroll now in the December 9th Inclusive Care for Gender and Sexual Minorities Course and take the first step towards becoming a more inclusive healthcare provider.

As a healthcare professional, staying informed about ethical and legal responsibilities is not just a requirement, but a crucial aspect of providing the best care for your patients. I instruct a remote course that tackles these difficult issues - my course, Ethical Considerations from a Legal Lens is a comprehensive remote course taking place on November 17, 2024, that will delve into these important topics from the perspective of the pelvic health rehabilitation field.
Why does this topic matter?
Navigating the complex legal and ethical landscape can be challenging for healthcare providers, particularly in specialized areas like pelvic rehabilitation or even more niche subsets within pelvic health. This course is designed to help practitioners gain a deeper understanding of ethical decision-making while helping a provider feel more legal compliance to safeguard the patient’s well-being and the integrity of a provider’s practice.
During this course, you’ll interactively explore key concepts including:
- Patient confidentiality and informed consent in sensitive treatments like pelvic health
- Legal obligations that impact your practice and decision-making process
- Practical case studies to strengthen ethical problem-solving skills
- Strategies to reduce legal risks while delivering high-quality care
Whether you’re a physical therapist, occupational therapist, or another healthcare provider working in pelvic health, this course is an excellent opportunity to sharpen your ethical compass and protect your practice from potential legal pitfalls.
Who Should Attend?
This course is designed for all pelvic health professionals who want to:
- Refresh their understanding of ethical standards
- Stay updated on legal obligations
- Ensure compliance with state and federal regulations
- Strengthen their ethical decision-making skills
Whether you're new to the field or a seasoned professional, this course offers valuable insights that will enhance your ability to care for patients ethically and legally. This class offers a “think tank” of your peers to help problem-solve real-time ethical or legal issues you may be experiencing in your practice.
With evolving legal and ethical complexities, staying educated is key to practicing responsibly and avoiding potential issues. Join us on November 17 for this impactful course that will empower you with the tools to uphold ethical excellence in pelvic health.
Ready to take your practice to the next level?
Register today and ensure you’re prepared to navigate the ethical and legal challenges in your profession.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much she has not treated since beginning this journey and she is always happy to further her education to better help her patients meet their goals.
She strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, She opened her own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.
At Herman & Wallace, we’re committed to providing practitioners with the knowledge and skills they need to offer the best care possible. We’ve heard your feedback regarding the lack of familiarity with rectal balloon catheters, and we’re excited to announce a new remote course: Anorectal Balloon Catheters: Introduction and Practical Application.
Course Overview
This short but comprehensive course offers 5.5 contact hours dedicated to the essential aspects of using rectal balloon catheters in treating patients experiencing defecatory dysfunction. It is designed for those who have completed Pelvic Function Level 1.
While this course will be conducted remotely, participants are required to register with another clinician to facilitate hands-on lab practice.
Learning Objectives
Participants will explore a range of topics, including:
- Understanding Anatomy and Physiology: Gain insights into the relevant anatomy and pathophysiology associated with defecatory conditions.
- Assessment Techniques: Learn how to assess sensation in the anal canal related to defecation using balloon catheters.
- Treatment Planning: Develop appropriate treatment plans for patients with hypersensitivity and hyposensitivity affecting defecation.
- Indications and Contraindications: Understand when balloon training is appropriate and explore in-depth treatment guidelines.
- Data Interpretation: Learn how to interpret assessment data gathered during balloon catheter evaluations and formulate effective treatment strategies.
Join Us
Anorectal Balloon Catheters: Introduction and Practical Application is perfect for practitioners eager to enhance their skill set in managing defecatory dysfunction through advanced techniques. We invite you to join senior faculty Allison Arial on December 14th for this enriching educational opportunity.
Don’t miss the chance to expand your expertise and improve your clinical practice. Register now and be part of a course designed to elevate the standard of care for your patients!
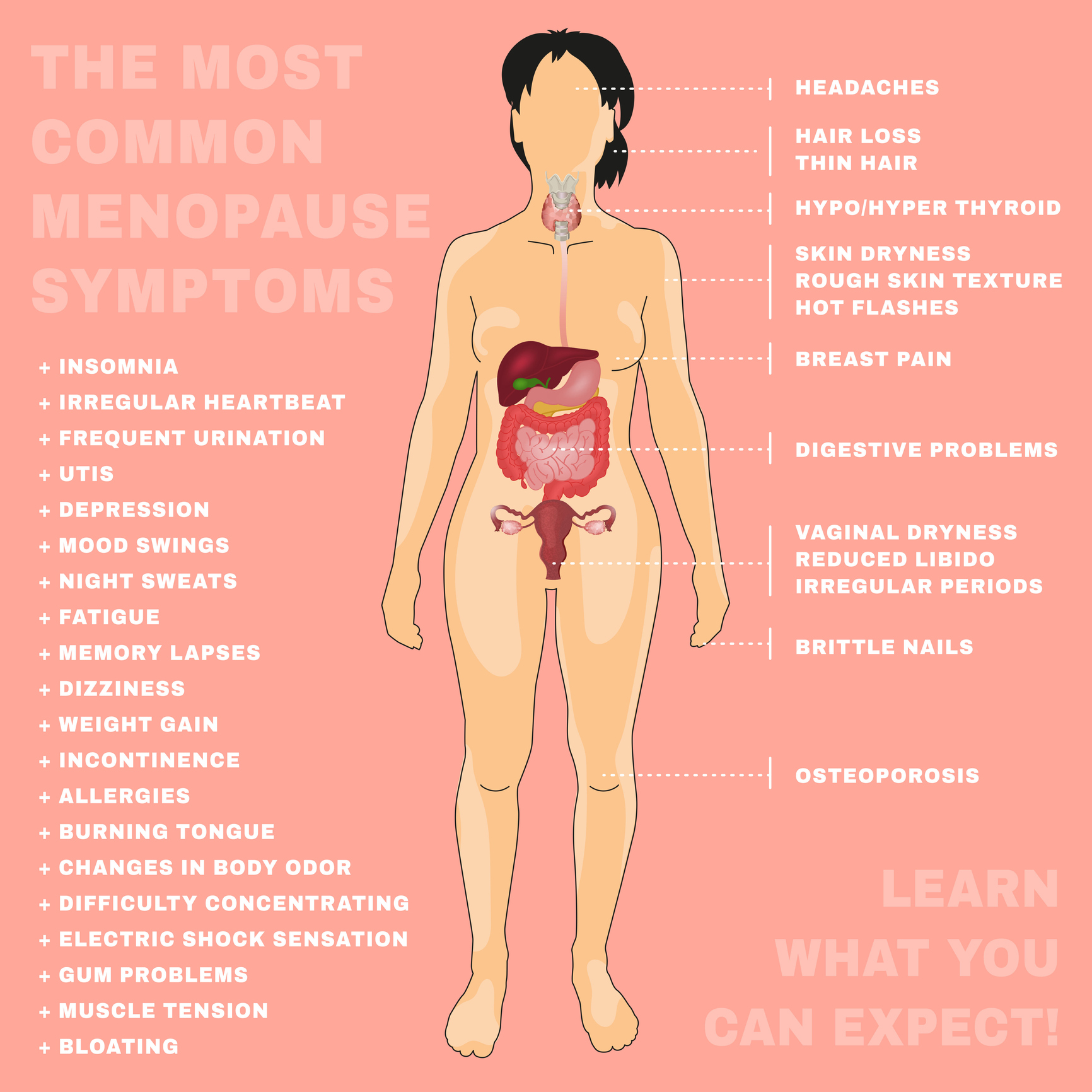
According to the International Menopause Society, “The purpose of the day is to raise awareness of menopause and the support options available for improving health and well-being.” While we have come a long way in bringing this issue into the spotlight, I still encounter patients on a daily basis who are unaware of what this transition can mean to their long-term health and quality of life. Some do not discuss their symptoms with their physician, and others, despite sharing their symptoms with their doctor, often leave the visit with “just live with it” as the recommended course of care due to fear of breast cancer (Barber and Charles 2023).
I have been teaching my menopause course, Menopause Transitions and Pelvic Rehab, for almost three years. A common question raised by participants during the course is whether discussing hormonal treatment options is outside the scope of pelvic rehabilitation. While I understand the concern, I do have some thoughts I would like you to consider. To elaborate, let me share a recent clinical experience I had when evaluating a patient for an orthopedic pathology.
This patient was a cis-female patient in her late 40s who presented to the clinic for mid-back pain. She had an extensive medical history of auto-immune conditions and work-related injury. She had been hospitalized due to her diagnosis and had lost a substantial amount of weight. As with any therapy evaluation, I asked how she was sleeping.
 What she reported isn’t atypical for many of my patients. She was having pain that was disrupting her sleep patterns. She also reported hot flashes that were waking her up frequently in the night. She would go on walks occasionally but was not exercising regularly due to fatigue. Her food intake consisted of several servings of vegetables and fruit but was lacking in protein. On further discussion, she reported not having a period for a little over a year. She had misgivings about hormones due to breast cancer risk and wasn’t sure it was an option for her.
What she reported isn’t atypical for many of my patients. She was having pain that was disrupting her sleep patterns. She also reported hot flashes that were waking her up frequently in the night. She would go on walks occasionally but was not exercising regularly due to fatigue. Her food intake consisted of several servings of vegetables and fruit but was lacking in protein. On further discussion, she reported not having a period for a little over a year. She had misgivings about hormones due to breast cancer risk and wasn’t sure it was an option for her.
I was able to explain the background behind the Women’s Health Initiative and how this research was misinterpreted in the media and among many in the healthcare community regarding the safety of hormone therapy (Bluming and Tavris 2018). I explained estrogen is approved for the treatment of hot flashes and prevention of osteoporosis by The Menopause Society (position statement 2022). I also discussed the current recommendations of weight training from the Center for Disease Control of two days a week. We strategized goals for implementing this into her plan as she progressed in her exercise ability. I highlighted how the ability to process protein diminishes as she ages (Bauer et. al, 2013) requiring diligence to ensure adequate amounts in her diet.
On her next visit, she reported meeting with her obstetrics and gynecology doctor. She was given the option of hormone therapy and had started on a daily regimen. Her sleeping had improved, and she was feeling more like herself. She was making an effort to get protein at every meal, and while she was still not exercising consistently, she was hoping to start soon.
This patient was at high risk for osteoporosis due to her substantial weight loss and low BMI (Xiang et. al, 2017). Her sleep was being impacted by her hot flashes. Lack of sleep has been shown to increase the risk of cancer, heart disease, and neurodegenerative disease (Garborino et.al, 2021). It can also affect our patient’s ability to cope with stress and pain. How is someone supposed to heal if they can’t sleep? If I had not known about approved hormonal medications for the symptoms the patient was experiencing – I would not have been able to explain this option to the patient.
As pelvic health therapists, prescribing medications is certainly outside our scope. However, if we aren’t aware of their indications, how are our patients supposed to know their options? We are often the health care provider in whom they spend the most time and thus our patients often report symptoms to us that they haven’t shared with their doctor.
That is not to say that patients do not talk to their doctors about menopause. Many patients do actually report their symptoms to their physician; however, studies have found that these physicians often have not received the proper education on the menopause transition and are not always aware of when to prescribe hormone therapy (Kling et. al, 2019). We can provide referrals to specialists who DO have that knowledge so patients can know their options and make decisions together with an informed provider.
We can help to bridge the knowledge gap by knowing risks, benefits, and treatment options, not for prescription of medication, but as a conduit of information to give our patients options to discuss with their providers. This can allow for symptom management, improving quality of life, and in some instances prevention of fracture.
The more healthcare clinicians that have a basic understanding of menopausal symptoms and treatments, the more patients can be made aware of the options available to them. This allows for a dialogue to occur between physician and patient. Certainly, this is only a small piece of the treatment puzzle. There are many more important aspects of treatment including building muscle, sleep hygiene, stress management, and nutrition, which do fall within our scope.
In honor of World Menopause Day, let’s celebrate by raising awareness for our patients in regard to this change, and what can be done as they navigate through this transitional time. Join me on November 2-3, 2024 in Menopause Transitions and Pelvic Rehab to be a part of the conversation.
References:
- The 2022 hormone therapy position statement of The North American Menopause Society. Menopause, 2022. 29(7): p. 767-794.
- Barber, K. and A. Charles, Barriers to Accessing Effective Treatment and Support for Menopausal Symptoms: A Qualitative Study Capturing the Behaviors, Beliefs and Experiences of Key Stakeholders. Patient Prefer Adherence, 2023. 17: p. 2971-2980.
- Bauer, J., et al., Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc, 2013. 14(8): p. 542-59.
- Bluming, A.Z.T.C., Estrogen Matters. 2018, 1290 Avenue of the Americans, New York, NY 10104: Little, Brown Spark. 310.
- Garbarino, S., et al., Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol, 2021. 4(1): p. 1304.
- Kling, J.M., et al., Menopause Management Knowledge in Postgraduate Family Medicine, Internal Medicine, and Obstetrics and Gynecology Residents: A Cross-Sectional Survey. Mayo Clin Proc, 2019. 94(2): p. 242-253.
- Xiang, B.Y., et al., Body mass index and the risk of low bone mass-related fractures in women compared with men: A PRISMA-compliant meta-analysis of prospective cohort studies. Medicine (Baltimore), 2017. 96(12): p. e5290.
AUTHOR BIO
Christine Stewart, PT, CMPT
Christine Stewart, PT, CMPT (she/her) graduated from Kansas State University in 1992 and pursued her master’s degree in physical therapy from the University of Kansas Medical Center graduating in 1994. She began her career specializing in orthopedics and manual therapy then became interested in women’s health after the birth of her second child.
Christine developed her pelvic health practice in a local hospital with a focus on urinary incontinence and prolapse. She left the practice in 2010 to work at Olathe Health to further focus on pelvic rehabilitation for all genders and obtain her CMPT from the North American Institute of Manual Therapy. She completed Diane Lee’s Integrated Systems Model education series in 2018. Her passion is empowering patients through education and treatment options for the betterment of their health throughout their lifespan. She enjoys speaking to physicians and to community-based organizations on pelvic health physical therapy.

While you may be reading this thinking, ‘I don’t know anyone who is Intersex,’ or ‘I’ve never treated a patient who is Intersex’ you might be surprised to find that 1.7% to 4% of people are Intersex, according to Zeeman and Aranda (2020) in their 2020 article A Systematic Review of the Health and Healthcare Inequalities for People with Intersex Variance.
According to Haghighat, et. al (2023) in their article Intersex people's perspectives on affirming healthcare practices: A qualitative study, “Intersex people have variations in their sex characteristics that do not exclusively fall within binary definitions of male and female.” These variations can be chromosomal, hormonal, gonadal, or anatomical (Cochetti, Monro, Vecchietti, & Yeadon-Lee [2020] and Haghighat, et. al [2023]).
Intersex folx are often seen by multiple healthcare providers throughout their lifetime, including pelvic rehab practitioners. However, one thing that most don’t know, is that historically; Intersex folx have been very mistreated and pathologized by healthcare workers. Many Intersex folx have been given non-medically necessary and non-consensual surgical procedures and hormone treatments over the years; and unfortunately, some of these practices are still occurring around the world even today. Intersex folx have also been treated by providers with inaccurate education and inadequate training needed to provide care to Intersex populations, leaving many patients who are Intersex being the ones who educate their own medical providers about their variations and healthcare needs. Tiffany Jones (2018) also mentions in her article Intersex Studies: A Systematic Review of International Health Literature that even language in the medical literature is inaccurate and inadequate when describing Intersex populations (Jones, 2018).
This maltreatment and poor education on the healthcare providers' part, as well as dissemination of inaccurate and pathologizing medical information; can lead to copious trauma for patients and a lack of trust in healthcare workers and healthcare systems. In Haghighat, et. al.’s article, they state that “depathologization of intersex variations and comprehensive teachings of intersex history and medical care must be incorporated into medical curricula to mitigate experiences of medical trauma and to relieve the burden placed on patients to be their own medical experts and advocates. Systemic change is needed for the normalization and demedicalization of intersex variations and for the medical empowerment of the intersex community.”
In my course Intersex Patients: Rehab and Inclusive Care, next scheduled for November 16, 2024, healthcare providers will learn about the healthcare needs that are unique to Intersex folx and about how to provide trauma-informed, evidence-based evaluations, treatments, and plans of care for patients who are Intersex. Students will also learn how to provide Intersex-Affirming Healthcare and how to be better allies in healthcare and in life to Intersex folx so that we can help put a stop to these non-medically necessary and non-consensual medical procedures, empower patients who are Intersex to have a say in their healthcare practices, to help stop the pathologization and further marginalization of Intersex people, and to educate other people (not just healthcare providers) about how to be allies to Intersex folx everywhere.
Resources:
- Intersex Studies: A Systematic Review of International Health Literature. Jones, T. (2018). Intersex Studies: A Systematic Review of International Health Literature. Sage Open, 8(2).https://doi.org/10.1177/2158244017745577
- Intersex people's perspectives on affirming healthcare practices: A qualitative study. Darius Haghighat, Tala Berro, Lillian Torrey Sosa, Kayla Horowitz, Bria Brown-King, Kimberly Zayhowski. Intersex people's perspectives on affirming healthcare practices: A qualitative study. Social Science & Medicine, Vol 329, 2023 116047, ISSN 0277-9536, https://doi.org/10.1016/j.socscimed.2023.116047.
- A Systematic Review of the Health and Healthcare Inequalities for People with Intersex Variance. Zeeman L, Aranda K. A Systematic Review of the Health and Healthcare Inequalities for People with Intersex Variance. Int J Environ Res Public Health. 2020 Sep 8;17(18):6533. doi: 10.3390/ijerph17186533. PMID: 32911732; PMCID: PMC7559554.
- https://www.tandfonline.com/doi/full/10.1080/13691058.2020.1825815#abstract/. Cochetti, D., Munro, S., Vecchietti, V., & Yeadon-Lee, T. (2020, November 25). 500-515. doi: 10.1080/13691058.
- Gain foundational knowledge. Not everyone with a healthcare degree arrived there by way of being a biology major. Accordingly, many people in the health field are simply unaware of how many wonderful people in this world exist outside the XY and XX binary. Did you know there are also people with just one X chromosome per cell? Some people are even XXYY or XXY! Also, some people may have chromosomes that fit binary expectations; however, they have generic variations that result in different bodily responses to sex hormones. This might, for example, lead to someone with XY chromosomes presenting with testes in the abdomen while also having breasts and a vulva. By taking this course, you will be able to appreciate the wide range of what it means to be a human. One of my all-time favorite podcast series, Gonads by RadioLab, is a great starting point for engaging with these concepts prior to the course: https://radiolab.org/series/radiolab-presents-gonads/
- Connect with your clients better. After taking this class, I learned new ways to bring up the topic of what it means to be intersex and how that relates to pelvic rehabilitation. I went from not being aware of any of my current clients being intersex, to finding out two were intersex within a few days of completing this course! This class will help you to build better rapport with all of your clients, whether they are intersex or not.
- Get practical tips on making your practice more inclusive. One of the big takeaways for me from this course was how to update my intake forms. I had already accounted for gender differences on my documents, but not sex differences. Through this course, I got great suggestions, such as including an organ inventory, rather than simply the three choices of male/female/intersex. The organ inventory is a great example of making a form more inclusive because I would want to know if a non-intersex (also called endosex) cisgender man didn't have, for instance, testicles just as much as I'd want to be prepared to support an intersex client with variations in anatomical structures. Here is a link to ideas for making your forms more intersex-friendly: https://www.queeringmedicine.com/resources/intake-form-guidance-for-providers.
AUTHOR BIO:
Molly O’Brien-Horn, PT DPT, CLT

Molly O’Brien-Horn graduated from Rutgers School of Biomedical & Health Sciences (formerly the University of Medicine & Dentistry of New Jersey) with her Doctor of Physical Therapy degree. She is a Pelvic Health Physical Therapist, a Certified Lymphedema Therapist, and an LSVT BIG Parkinson’s Disease Certified Therapist. She is also a sex counselor, a trained childbirth doula, and a trained postpartum doula. Molly is a member of the American Physical Therapy Association Academy of Pelvic Health Physical Therapy and is also a Teaching Assistant with the Herman & Wallace Pelvic Rehabilitation Institute.
Molly is passionate about providing accessible healthcare to pelvic health patients of all age ranges, all gender-identities, all sexualities, all body variations, and all ability levels. She also has experience in a variety of physical therapy settings over the years including pediatric and adult oncology, school-based pediatrics, inpatient and intensive care unit hospital-based settings, skilled nursing facilities, outpatient and sports-based orthopedics, and wound care.

HWConnect is scheduled for March 28-30, 2025 in Seattle Washington. HWConnect tickets include all speakers, breakout sessions, labs, mixers, vendor hall time, and reception.
HWConnect 2025 has announced our keynote speakers for the March 28-30, 2025 event, and you do NOT want to miss them.
HWConnect opens on Friday, March 28, 2025, and will culminate that evening with Keynote Speaker, Dawn Sandalcidi, PT, RCMT, BCB-PMD. If you are a pediatric therapist then you should be familiar with Dawn, who is the trailblazer and leading expert in the field of pediatric pelvic floor disorders. This keynote will be a deep dive into the “Development of Continence Through The Lens of The Diaphragm, Ribcage, and Pelvic Floor.”
A little about Dr. Sandalcidi. She is a national and international speaker, a faculty instructor at the Herman & Wallace Pelvic Rehab Institute, and runs an online teaching and mentoring platform for parents and professionals. In 2017, Dawn spoke at the World Physical Therapy Conference in South Africa about pediatric pelvic floor dysfunction and incontinence. In 2018, Dawn was awarded the Elizabeth Noble Award by the American Physical Therapy Association Section on Women's Health for providing Extraordinary and Exemplary Service to the Field of Physical Therapy for Children. She has also been published in the Journals of Urologic Nursing and Section of Women’s Health.
Next, let’s move on to Saturday. HW is excited to announce that Nancy Norton, RN will be headlining the event as our Saturday Keynote Speaker. Not only is Nancy a registered nurse and comedian, but she also has a talent for intuitively reading the room which we will experience first-hand with her keynote address, “The Power of Humor for Pelvic Healers.”
You may be familiar with Nancy already as she has been featured on A&E, Netflix, Amazon Prime, tours nationally, and has a weekly Podcast called "Tromedy" that is aimed at helping to transmute trauma responses with comedy. Buckle up for hilarious storytelling mixed with standup punchlines rooted in real-life experiences like growing up in a dysfunctional Ozark family and working in Healthcare.
HWConnect closes on Sunday with our final esteemed Keynote Speaker, Leticia Nieto, Psy.D., LMFT. Leticia is a leadership coach, psychotherapist, and educator specializing in liberation and equity, cultural responsiveness, motivational patterning, and evolutionary creativity. Dr. Nieto will be channeling her experience in activism, scholarship, and consulting work to speak on “Working Well: Trauma Responsive Care for Those We Work With and for Us.”
Dr. Nieto is internationally recognized for her expertise in addressing social justice concerns from a developmental ecological perspective including orienting to systemic transformation, survivance, song and poetry, relational repair, joy, radical rest, intersectional coalition, and reparative and restorative justice. Her 2010 book, Beyond Inclusion, Beyond Empowerment: A Developmental Strategy to Liberate Everyone, is an accessible analysis of the dynamics of oppression and supremacy that offers readers ways to develop skills to promote social justice.
All three Keynote Speakers are at the top of their field, and we can’t wait to hear what they have to say! Make sure you seize this opportunity to be inspired and connect with the experts.
If you haven’t registered yet then consider this your personal invitation to join us at HWConnect 2025 in beautiful Seattle, Washington. Take advantage of this golden opportunity to network, learn, and expand your toolkit. The conference will be here before you realize it – and tickets are limited! PLUS, if you register now, you can reserve your room at a special discounted rate.
📲 Get more information! https://www.hermanwallace.com/connect-2025
🛎 Register to attend! https://hermanwallace.com/hwconnect-2025